Mucormycoses US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Mucormycoses. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Mucormycoses US Medical PG Question 1: A 19-year-old man with a history of type 1 diabetes presents to the emergency department for the evaluation of a blood glucose level of 492 mg/dL. Laboratory examination revealed a serum bicarbonate level of 13 mEq/L, serum sodium level of 122 mEq/L, and ketonuria. Arterial blood gas demonstrated a pH of 6.9. He is admitted to the hospital and given bicarbonate and then started on an insulin drip and intravenous fluid. Seven hours later when his nurse is making rounds, he is confused and complaining of a severe headache. Repeat sodium levels are unchanged, although his glucose level has improved. His vital signs include a temperature of 36.6°C (98.0°F), pulse 50/min, respiratory rate 13/min and irregular, and blood pressure 177/95 mm Hg. What other examination findings would be expected in this patient?
- A. Hypoglycemia
- B. Pupillary constriction
- C. Papilledema (Correct Answer)
- D. Pancreatitis
- E. Peripheral edema
Mucormycoses Explanation: ***Papilledema***
- This patient's symptoms (confusion, severe headache, bradycardia, irregular respiration, hypertension) following treatment for **diabetic ketoacidosis (DKA)** are highly suggestive of **cerebral edema**.
- **Papilledema** is a retinal finding resulting from increased intracranial pressure (ICP), which is a characteristic sign of cerebral edema.
*Hypoglycemia*
- While the patient's glucose level has improved, it is not described as being low enough to cause hypoglycemia, and the symptoms are more consistent with **increased ICP**.
- Symptoms of hypoglycemia (e.g., tremors, sweating, hunger, anxiety) are different from the patient's current presentation of confusion and severe headache.
*Pupillary constriction*
- **Pupillary constriction** (miosis) is typically not associated with cerebral edema; instead, **pupillary dilation** (mydriasis) can occur with severe increase in ICP due to uncal herniation.
- The combination of bradycardia, irregular respiration, and hypertension (Cushing's triad) is indicative of increased ICP, which would likely cause pupillary changes related to brainstem compression.
*Pancreatitis*
- Pancreatitis is a known complication of DKA, but it typically presents with **severe abdominal pain**, nausea, and vomiting, rather than cerebral symptoms.
- Although the patient had DKA, the current neurological symptoms point directly to an intracranial process rather than an abdominal issue.
*Peripheral edema*
- **Peripheral edema** results from fluid accumulation in peripheral tissues and is not a direct consequence or expected finding in cerebral edema.
- While fluid administration can cause some peripheral fluid retention, it typically does not lead to the acute neurological deterioration seen in this patient.
Mucormycoses US Medical PG Question 2: An investigator is studying growth patterns of various fungal pathogens. Incubation of an isolated fungus at 25°C shows branching hyphae with rosettes of conidia under light microscopy. After incubation at 37°C, microscopic examination of the same organism instead shows smooth, white colonies with rounded, elongated cells. Infection with the investigated pathogen is most likely to cause which of the following conditions?
- A. Pityriasis versicolor
- B. Candidiasis
- C. Cryptococcosis
- D. Sporotrichosis (Correct Answer)
- E. Coccidioidomycosis
Mucormycoses Explanation: ***Sporotrichosis***
- The description of a fungal pathogen exhibiting **thermal dimorphism** (different forms at 25°C and 37°C) is characteristic of **Sporothrix schenckii**.
- At 25°C, it typically grows as **mold with branching hyphae and conidia in rosettes**, and at 37°C, it grows as **yeast-like cells (cigar-shaped bodies in tissue)**, which can appear rounded and elongated.
*Pityriasis versicolor*
- Caused by **Malassezia globosa**, which is a **lipophilic yeast** and does not exhibit thermal dimorphism described here.
- Characterized by **hypo- or hyperpigmented skin patches**, not deep tissue infection with dimorphic growth.
*Candidiasis*
- Caused by **Candida species**, which are **opportunistic yeasts** that can form pseudohyphae and true hyphae but do not display the specific dimorphism with rosettes of conidia at 25°C.
- Infections range from superficial mucocutaneous to systemic, but the fungal morphology described does not fit.
*Cryptococcosis*
- Caused by **Cryptococcus neoformans** or **Cryptococcus gattii**, which are **encapsulated yeasts** and do not exhibit dimorphism (mold at 25°C, yeast at 37°C).
- Primarily causes **meningoencephalitis** or pulmonary disease, and is identified by its capsule and yeast form.
*Coccidioidomycosis*
- Caused by **Coccidioides immitis** or **Coccidioides posadasii**, which are **thermally dimorphic fungi**, but their morphology differs from the description.
- At 25°C, they grow as molds with **arthroconidia**, and at 37°C, they form **spherules containing endospores** in tissue, not smooth, white colonies with rounded, elongated cells.
Mucormycoses US Medical PG Question 3: A 27-year-old diabetic male rushes to the emergency department after finding his blood glucose level to be 492 mg/dL which is reconfirmed in the ED. He currently does not have any complaints except for a mild colicky abdominal pain. His temperature is 37°C (98.6°F), respirations are 15/min, pulse is 67/min, and blood pressure is 122/88 mm Hg. Blood is drawn for labs the result of which is given below:
Serum:
pH 7.0
pCO2 32 mm Hg
HCO3- 15.2 mEq/L
Sodium 122 mEq/L
Potassium 4.8 mEq/L
Urinalysis is positive for ketone bodies. He is admitted to the hospital and given intravenous bicarbonate and then started on an insulin drip and normal saline. 7 hours later, he is found to be confused and complaining of a severe headache. His temperature is 37°C (98.6°F), pulse is 50/min, respirations are 13/min and irregular, and blood pressure is 137/95 mm Hg. What other examination findings would be expected in this patient?
- A. Pancreatitis
- B. Pupillary constriction
- C. Hypoglycemia
- D. Peripheral edema
- E. Papilledema (Correct Answer)
Mucormycoses Explanation: ***Papilledema***
- The patient's presentation with **confusion**, **severe headache**, **bradycardia**, **irregular respirations**, and **elevated blood pressure** (Cushing's triad) 7 hours after treatment for **diabetic ketoacidosis (DKA)** suggests increased intracranial pressure due to **cerebral edema**.
- **Papilledema** is a key ophthalmoscopic finding in significant cerebral edema, resulting from increased intracranial pressure transmitted to the optic nerve sheath.
*Pancreatitis*
- Pancreatitis can cause abdominal pain and may be associated with DKA, but the acute neurological deterioration with signs of increased intracranial pressure after initial treatment points away from pancreatitis as the primary expected finding at this stage.
- While initial mild colicky abdominal pain could suggest pancreatitis, the late-onset confusion, headache, and vital sign changes following DKA treatment are not characteristic of pancreatitis, but rather of a severe neurological complication.
*Pupillary constriction*
- **Pupillary constriction** (miosis) can be associated with opioid overdose, pontine lesions, or certain medications, but it is not a direct or expected finding in cerebral edema causing increased intracranial pressure.
- In cerebral edema, pupils are more likely to be dilated or unequal, especially if there is uncal herniation.
*Hypoglycemia*
- While **hypoglycemia** can occur with insulin therapy, leading to confusion and neurological symptoms, the patient's blood pressure is elevated and heart rate is low (bradycardia), which are not typical signs of hypoglycemia.
- Hypoglycemia usually presents with sympathetic activation (tachycardia, diaphoresis) before progressing to bradycardia in severe cases, but the associated hypertension and irregular breathing pattern are more indicative of increased intracranial pressure.
*Peripheral edema*
- **Peripheral edema** is swelling in the extremities and is generally due to fluid overload, heart failure, kidney disease, or liver disease.
- While fluid administration during DKA treatment could potentially lead to some fluid retention, it does not explain the acute neurological deterioration, headache, and vital sign changes (Cushing's triad) seen in this patient, which are far more characteristic of cerebral edema.
Mucormycoses US Medical PG Question 4: A 26-year-old female with AIDS (CD4 count: 47) presents to the emergency department in severe pain. She states that over the past week she has been fatigued and has had a progressively worse headache and fever. These symptoms have failed to remit leading her to seek care in the ED. A lumbar puncture is performed which demonstrates an opening pressure of 285 mm H2O, increased lymphocytes, elevated protein, and decreased glucose. The emergency physician subsequently initiates treatment with IV amphotericin B and PO flucytosine. What additional treatment in the acute setting may be warranted in this patient?
- A. Serial lumbar punctures (Correct Answer)
- B. Fluconazole
- C. Mannitol
- D. Chloramphenicol
- E. Acetazolamide
Mucormycoses Explanation: **Serial lumbar punctures**
- The elevated opening pressure (285 mm H2O) indicates **increased intracranial pressure (ICP)**, which is common in cryptococcal meningitis and can be life-threatening.
- Serial lumbar punctures can help to **reduce ICP** and relieve symptoms, improving outcomes in patients with cryptococcal meningitis.
*Fluconazole*
- Fluconazole is used for **maintenance therapy** to prevent relapse after the acute phase of cryptococcal meningitis has been controlled.
- It is generally **not recommended for initial acute treatment** in severe cases due to its fungistatic nature, making it less effective than the combination of amphotericin B and flucytosine.
*Mannitol*
- Mannitol is an **osmotic diuretic** sometimes used to acutely *reduce* ICP in cases of cerebral edema.
- While effective in some situations, it is **not the primary treatment for increased ICP** in cryptococcal meningitis, where repeated LPs are preferred to remove infected CSF and directly reduce pressure.
*Chloramphenicol*
- Chloramphenicol is an **antibiotic** primarily used to treat bacterial infections, not fungal infections.
- It has **no role in the treatment of fungal meningitis** caused by *Cryptococcus neoformans*.
*Acetazolamide*
- Acetazolamide is a **carbonic anhydrase inhibitor** that can reduce CSF production, thereby *reducing* ICP.
- While it can be used in some cases of elevated ICP, routine use in cryptococcal meningitis is **not standard practice**, and serial LPs are generally the preferred method for managing dangerously high ICP in this context due to their immediate efficacy.
Mucormycoses US Medical PG Question 5: A 47-year-old woman presents with blurry vision for the past 2 weeks. She says that symptoms onset gradually and have progressively worsened. She works as a secretary in a law firm, and now her vision is hampering her work. Past medical history is significant for psoriasis, diagnosed 7 years ago, managed with topical corticosteroids. Her blood pressure is 120/60 mm Hg, respiratory rate is 17/min, and pulse is 70/min. Her BMI is 28 kg/m2. Physical examination is unremarkable. Laboratory findings are significant for the following:
RBC count 4.4 x 1012/L
WBC count 5.0 x 109/L
Hematocrit 44%
Fasting plasma glucose 250 mg/dL
Hemoglobin A1C 7.8%
Which of the following would be the most likely cause of death in this patient?
- A. Rhinocerebral mucormycosis
- B. Coma
- C. Peripheral neuropathy
- D. Myocardial infarction (Correct Answer)
- E. Renal failure
Mucormycoses Explanation: ***Myocardial infarction***
- The patient's elevated **fasting plasma glucose** (250 mg/dL) and **HbA1C** (7.8%) indicate **uncontrolled diabetes mellitus**. Her **BMI of 28** kg/m2 points to **overweight/obesity**, another risk factor for cardiovascular disease.
- **Cardiovascular disease**, including **myocardial infarction**, is the leading cause of death in patients with diabetes due to accelerated atherosclerosis.
*Rhinocerebral mucormycosis*
- This is an **opportunistic fungal infection** typically seen in severely immunocompromised patients, particularly those with uncontrolled diabetes and ketoacidosis.
- While diabetes is a risk factor, the patient does not present with characteristic symptoms such as **facial pain**, **black nasal discharge**, or widespread immunosuppression.
*Coma*
- **Diabetic coma** can result from extreme hyperglycemia (**hyperosmolar hyperglycemic state**) or severe hypoglycemia.
- While the patient has hyperglycemia, her blood pressure, respiratory rate, and pulse are stable, and the physical examination is unremarkable, suggesting she is not in immediate danger of diabetic coma.
*Peripheral neuropathy*
- **Diabetic peripheral neuropathy** is a common long-term complication of diabetes, causing symptoms like numbness, tingling, and pain, mainly in the extremities.
- While likely present with long-standing uncontrolled diabetes, it is generally **not a direct cause of death** but rather contributes to morbidity and risk of secondary complications like foot ulcers and infections.
*Renal failure*
- **Diabetic nephropathy** is a major microvascular complication of diabetes leading to **chronic kidney disease** and potentially end-stage renal failure.
- While possible in the long term, there are no specific direct indicators of severe or advanced renal failure in her current presentation such as elevated creatinine or signs of fluid overload; cardiovascular events pose a more immediate and common fatal risk in uncontrolled diabetes.
Mucormycoses US Medical PG Question 6: A 19-year-old woman presents to the emergency department with complaints of blurry vision and headaches that started 2 days ago. She reports that she has been experiencing some facial pain, but she thought it was related to her toothache. She is also worried about a black spot that is increasing in size on her face over the last month. She expresses concerns about her frequency of urination. Recently, she had a runny nose and cough that resolved spontaneously. The patient was diagnosed with type 1 diabetes mellitus at 13 years of age. She is a non-smoker and drinks beer occasionally. Her blood pressure is 122/98 mm Hg and temperature is 37.2°C (98.9°F). The physical examination is normal with the exception of a black necrotic eschar lateral to the right nasal ala. She lost 2.7 kg (6 lb) since her last visit, which was 6 months ago. A routine urinalysis at the office is positive for glucose and ketones. What is the most likely cause of the patient’s symptoms?
- A. Bacillus anthracis
- B. Mucormycosis (Correct Answer)
- C. Clostridium difficile
- D. Histoplasma capsulatum
- E. Aspergillus fumigatus
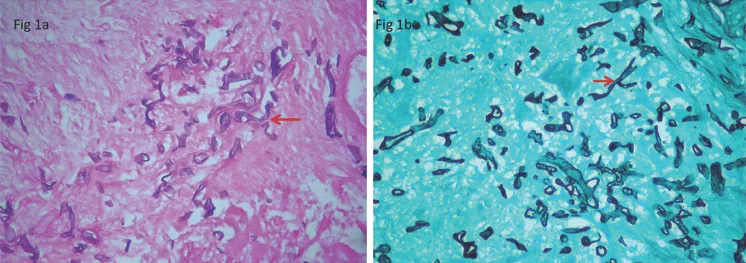
Mucormycoses Explanation: ***Mucormycosis***
- This patient, with uncontrolled **Type 1 diabetes** (indicated by frequent urination, weight loss, and glucose/ketones in urine), is at high risk for **mucormycosis**, an opportunistic fungal infection.
- The presence of a **black necrotic eschar** on the face, coupled with eye symptoms (blurry vision) and facial pain, is highly characteristic of **rhino-orbital-cerebral mucormycosis**, which often originates in the sinuses.
*Bacillus anthracis*
- **Cutaneous anthrax** would present as a painless ulcer with a black eschar, but it typically occurs in individuals exposed to infected animals or animal products and is not associated with diabetes or the rhinocerebral symptoms described.
- Systemic symptoms like blurry vision, headaches, and polyuria are not typical for cutaneous anthrax.
*Clostridium difficile*
- This bacterium primarily causes **gastrointestinal infections**, leading to diarrhea, abdominal pain, and fever.
- There are no symptoms described that suggest a *C. difficile* infection, and it does not cause facial eschars or rhino-orbital symptoms.
*Histoplasma capsulatum*
- **Histoplasmosis** is a fungal infection typically acquired by inhaling spores, often found in bird or bat droppings, mainly affecting the lungs.
- While it can disseminate in immunocompromised individuals, causing mucocutaneous lesions, it typically doesn't present with a rapid-onset facial eschar or the specific rhino-orbital symptoms seen here.
*Aspergillus fumigatus*
- Although **invasive aspergillosis** can occur in immunocompromised patients, including those with diabetes, it more commonly affects the lungs (e.g., aspergilloma, chronic pulmonary aspergillosis).
- While it can cause sinusitis and, rarely, cutaneous lesions, the rapid progression to a **black necrotic eschar** in the context of uncontrolled diabetes points more strongly towards mucormycosis.
Mucormycoses US Medical PG Question 7: A 58-year-old man presents with a high-grade fever, throbbing left-sided headache, vision loss, and left orbital pain. He says that his symptoms started acutely 2 days ago with painful left-sided mid-facial swelling and a rash, which progressively worsened. Today, he woke up with complete vision loss in his left eye. His past medical history is significant for type 2 diabetes mellitus, diagnosed 5 years ago. He was started on an oral hypoglycemic agent which he discontinued after a year. His temperature is 38.9°C (102.0°F), blood pressure is 120/80 mm Hg, pulse is 120/min, and respiratory rate is 20/min. On examination, there is purulent discharge from the left eye and swelling of the left half of his face including the orbit. Oral examination reveals extensive necrosis of the palate with a black necrotic eschar and purulent discharge. Ophthalmic examination is significant for left-sided ptosis, proptosis, and an absence of the pupillary light reflex. Laboratory findings are significant for a blood glucose level of 388 mg/dL and a white blood cell count of 19,000 cells/mm³. Urinary ketone bodies are positive. Fungal elements are found on a KOH mount of the discharge. Which of the following statements best describes the organism responsible for this patient’s condition?
- A. It appears as a narrow-based budding yeast with a thick capsule
- B. Histopathological examination shows non-septate branching hyphae (Correct Answer)
- C. It produces conidiospores
- D. It has budding and filamentous forms
- E. Histopathological examination shows acute angle branching hyphae
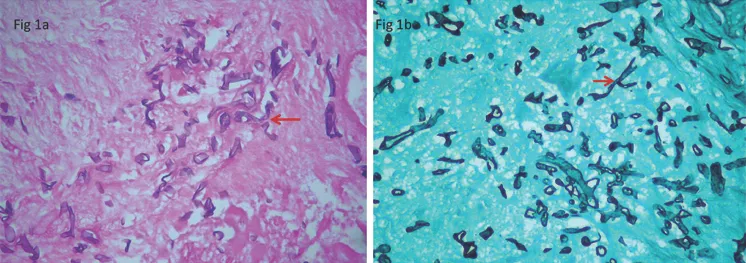
Mucormycoses Explanation: ***Histopathological examination shows non-septate branching hyphae***
- The patient's presentation with **diabetic ketoacidosis**, orbital pain, vision loss, facial swelling, necrotic palatal eschar, and high fever strongly suggests **mucormycosis**, a severe fungal infection.
- Mucormycosis is caused by fungi belonging to **Mucorales order** (e.g., *Rhizopus*, *Mucor*, *Lichtheimia*), which are characterized by **broad, ribbon-like, non-septate hyphae with irregular, wide-angle branching**.
*It appears as a narrow-based budding yeast with a thick capsule*
- This description is characteristic of **Cryptococcus neoformans**, which causes cryptococcosis, often presenting with meningoencephalitis and lung involvement.
- The clinical picture and *KOH mount* findings in this patient are inconsistent with cryptococcosis.
*It produces conidiospores*
- **Conidiospores are asexual spores** produced by many fungi, including *Aspergillus* and *Penicillium*, but this is a general characteristic and not specific enough to definitively identify the pathogen responsible for mucormycosis.
- The *histopathological features* (non-septate hyphae) are the key identifier in mucormycosis.
*It has budding and filamentous forms*
- This description generally refers to **dimorphic fungi** (e.g., *Histoplasma*, *Blastomyces*, *Coccidioides*), which exhibit yeast forms in tissue and mold forms in culture.
- Mucorales are typically **molds** in both environments and are not considered dimorphic, nor do they commonly present with budding forms.
*Histopathological examination shows acute angle branching hyphae*
- This morphological description is characteristic of **Aspergillus species**, which cause aspergillosis, another opportunistic fungal infection.
- *Aspergillus* hyphae are typically **septate** and branch at acute angles (around 45 degrees), unlike the broad, non-septate, wide-angle branching hyphae of Mucorales.
Mucormycoses US Medical PG Question 8: A 50-year-old HIV-positive male presents to the ER with a two-day history of fever and hemoptysis. Chest radiograph shows a fibrocavitary lesion in the right middle lobe. Biopsy of the afflicted area demonstrates septate hyphae that branch at acute angles. Which of the following is the most likely causal organism?
- A. Mycobacterium tuberculosis
- B. Pneumocystis jirovecii
- C. Aspergillus fumigatus (Correct Answer)
- D. Candida albicans
- E. Mucor species
Mucormycoses Explanation: ***Aspergillus fumigatus***
- The combination of **fever**, **hemoptysis**, a **fibrocavitary lesion** in an **HIV-positive** patient, and the presence of **septate hyphae branching at acute angles** on biopsy are classic findings for invasive **aspergillosis**.
- **Aspergillus** specifically targets individuals with compromised immune systems, and the pathological description of the hyphae is highly characteristic of this fungus.
*Mycobacterium tuberculosis*
- While **Mycobacterium tuberculosis** can cause **fever**, **hemoptysis**, and **cavitary lesions** in HIV-positive patients, the microscopic description of **septate hyphae branching at acute angles** is not consistent with bacterial infection.
- Tuberculosis is characterized by **acid-fast bacilli** and granulomatous inflammation, not fungal hyphae.
*Mucor species*
- **Mucor** (along with Rhizopus) causes **mucormycosis**, an invasive fungal infection that can affect immunocompromised patients and present with pulmonary involvement and cavitary lesions.
- However, mucormycosis is characterized by **non-septate (aseptate) hyphae branching at right (90-degree) angles**, not septate hyphae at acute angles, making it distinguishable from Aspergillus.
*Pneumocystis jirovecii*
- **Pneumocystis jirovecii** is a common cause of pneumonia in HIV-positive patients, typically presenting as **diffuse interstitial infiltrates** rather than cavitary lesions.
- Microscopic examination would reveal **cysts** and **trophozoites**, not septate hyphae, making it inconsistent with the biopsy findings.
*Candida albicans*
- While **Candida albicans** can cause infections in immunocompromised individuals, it typically presents as **oral thrush**, esophagitis, or disseminated candidiasis.
- Pulmonary involvement is less common and usually manifests as **pneumonitis** rather than cavitary lesions, and its hyphae are typically **pseudohyphae** or budding yeasts, not septate hyphae branching at acute angles.
Mucormycoses US Medical PG Question 9: A 26-year-old man with HIV and a recent CD4+ count of 800 presents to his PCP with fever, cough, and dyspnea. He notes that he recently lost his job as a construction worker and has not been able to afford his HAART medication. His temperature is 102.6°F (39.2°C), pulse is 75/min, respirations are 24/min, and blood pressure is 135/92 mmHg. Physical exam reveals a tachypneic patient with scattered crackles in both lungs, and labs show a CD4+ count of 145 and an elevated LDH. The chest radiography is notable for bilateral diffuse interstitial infiltrates. For definitive diagnosis, the physician obtains a sputum sample. Which stain should he use to visualize the most likely responsible organism?
- A. Periodic acid schiff stain
- B. Silver stain (Correct Answer)
- C. Ziehl-Neelsen stain
- D. India ink stain
- E. Carbol fuchsin stain
Mucormycoses Explanation: ***Silver stain***
- The patient's presentation with **fever, cough, dyspnea, bilateral diffuse interstitial infiltrates**, and a **CD4+ count of 145** (indicating severe immunosuppression) is highly suggestive of ***Pneumocystis jirovecii*** **pneumonia (PCP)**, formerly known as ***Pneumocystis carinii***.
- ***Pneumocystis jirovecii*** **cysts** and **trophozoites** are best visualized using **silver-based stains** (e.g., Gomori methenamine silver stain) which stain the fungal cell walls dark brown or black.
*Periodic acid schiff stain*
- **PAS stain** is used to identify **glycogen, mucus, and fungal elements** like those of *Candida* or *Aspergillus*, by staining polysaccharides a magenta color.
- While it can stain some fungal organisms, it is **not the primary or most effective stain** for *Pneumocystis jirovecii*.
*Ziehl-Neelsen stain*
- The **Ziehl-Neelsen stain** (also known as acid-fast stain) is used to identify **acid-fast bacilli**, such as *Mycobacterium tuberculosis* or *Nocardia*.
- Although **tuberculosis** is common in HIV patients, the clinical presentation and CXR findings (diffuse interstitial infiltrates rather than cavitary lesions or granulomas) **do not strongly suggest tuberculosis** as the primary diagnosis here.
*India ink stain*
- The **India ink stain** is primarily used to visualize the **capsule of *Cryptococcus neoformans*** in cerebrospinal fluid or other body fluids, appearing as a halo around the yeast cells.
- This patient's symptoms are respiratory, and the likely pathogen is *Pneumocystis*, making India ink stain **inappropriate** for this suspected diagnosis.
*Carbol fuchsin stain*
- **Carbol fuchsin stain** is a component of the **acid-fast staining** procedure (like Ziehl-Neelsen), used as the primary stain to identify acid-fast organisms.
- As with Ziehl-Neelsen, this stain is for **mycobacteria** and would **not effectively visualize** ***Pneumocystis jirovecii***.
Mucormycoses US Medical PG Question 10: A 7-year-old boy with a history of cystic fibrosis is brought to the physician for evaluation of recurrent episodes of productive cough, wheezing, and shortness of breath over the past month. Physical examination shows coarse crackles and expiratory wheezing over both lung fields. Serum studies show elevated levels of IgE and eosinophilia. A CT scan of the lungs shows centrally dilated bronchi with thickened walls and peripheral airspace consolidation. Antibiotic therapy is initiated. One week later, the patient continues to show deterioration in lung function. A sputum culture is most likely to grow which of the following?
- A. Monomorphic, septate hyphae that branch at acute angles (Correct Answer)
- B. Monomorphic, broad, nonseptate hyphae that branch at wide angles
- C. Dimorphic, broad-based budding yeast
- D. Dimorphic, cigar-shaped budding yeast
- E. Monomorphic, narrow budding encapsulated yeast
Mucormycoses Explanation: **Monomorphic, septate hyphae that branch at acute angles**
- The patient's presentation with **cystic fibrosis (CF)**, recurrent respiratory symptoms, CT findings of **central bronchiectasis**, elevated **IgE**, and **eosinophilia** strongly points towards **allergic bronchopulmonary aspergillosis (ABPA)**.
- *Aspergillus fumigatus*, the causative agent of ABPA, is characterized microscopically by **monomorphic, septate hyphae that branch at acute angles**.
*Monomorphic, broad, nonseptate hyphae that branch at wide angles*
- This describes organisms like *Rhizopus* or *Mucor*, which cause **mucormycosis**.
- Mucormycosis typically affects immunocompromised individuals (e.g., diabetics, neutropenic patients) and presents as aggressive rhinocerebral or pulmonary infections, not ABPA.
*Dimorphic, broad-based budding yeast*
- This morphology is characteristic of *Blastomyces dermatitidis*, which causes **blastomycosis**.
- Blastomycosis is an endemic fungal infection often presenting with pulmonary symptoms, but it does not cause central bronchiectasis, elevated IgE, or eosinophilia in the context of CF.
*Dimorphic, cigar-shaped budding yeast*
- This morphology describes *Sporothrix schenckii*, which causes **sporotrichosis**.
- Sporotrichosis typically presents as a chronic ulcerative skin disease (rose gardener's disease) or, less commonly, pulmonary disease, but is not associated with ABPA.
*Monomorphic, narrow budding encapsulated yeast*
- This morphology is characteristic of *Cryptococcus neoformans*, which causes **cryptococcosis**.
- Cryptococcosis commonly affects immunocompromised individuals, causing meningoencephalitis or pulmonary disease, but its presentation is distinct from ABPA, lacking the allergic and bronchiectatic features described.
More Mucormycoses US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.