Filarial nematodes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Filarial nematodes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
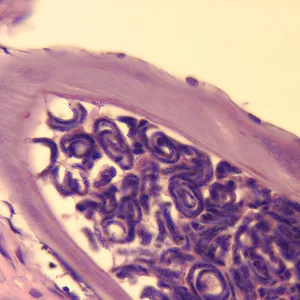
Filarial nematodes US Medical PG Question 1: A 7-year-old girl is brought to the physician by her mother because of a 4-week history of irritability, diarrhea, and a 2.2-kg (5-lb) weight loss that was preceded by a dry cough. The family returned from a vacation to Indonesia 2 months ago. Her vital signs are within normal limits. Abdominal examination shows mild tenderness with no guarding or rebound and increased bowel sounds. Her leukocyte count is 9,200/mm3 with 20% eosinophils. A photomicrograph of a wet stool mount is shown. Which of the following is the most appropriate pharmacotherapy?
- A. Diethylcarbamazine
- B. Metronidazole
- C. Albendazole (Correct Answer)
- D. Praziquantel
- E. Doxycycline
Filarial nematodes Explanation: ***Albendazole***
- The image shows a **hookworm egg**, characterized by its thin shell and developing larva inside; clinical features like **eosinophilia**, diarrhea, weight loss, and travel to an endemic area (Indonesia) are consistent with hookworm infection.
- **Albendazole** is the drug of choice for treating hookworm infections and other intestinal nematode infections.
*Diethylcarbamazine*
- This drug is primarily used for treating **lymphatic filariasis** (e.g., Wuchereria bancrofti, Brugia malayi) and **Loiasis** (African eye worm).
- It is not effective against hookworm infections.
*Metronidazole*
- **Metronidazole** is an antimicrobial agent effective against certain parasitic infections like **Giardia**, **Entamoeba histolytica**, and bacterial vaginosis.
- It is not indicated for the treatment of hookworm infections.
*Praziquantel*
- **Praziquantel** is an anthelminthic drug primarily used to treat infections caused by **flukes** (e.g., Schistosoma species) and **tapeworms** (e.g., Taenia species).
- It is not effective against hookworm infections.
*Doxycycline*
- **Doxycycline** is a tetracycline antibiotic with broad-spectrum activity against various bacterial infections and is also used in the treatment of some parasitic infections like **malaria prophylaxis** and **filariasis** (due to activity against Wolbachia endosymbionts).
- It is not a primary treatment for hookworm infections.
Filarial nematodes US Medical PG Question 2: A 39-year-old man presents to his primary care physician with a high fever, cough, and malaise. One week ago, he returned from a vacation to Hawaii where he went waterskiing with his family. Three days before presentation, he started experiencing intermittent abdominal pain, which was followed by flu-like symptoms, itchiness in his eyes, and photosensitivity. On presentation, his temperature is 103°F (39.4°C), blood pressure is 114/72 mmHg, pulse is 105/min, and respirations are 18/min. Physical exam reveals conjunctivitis and mild jaundice. Which of the following treatments could be used to treat this patient's condition?
- A. Ganciclovir
- B. Metronidazole
- C. Doxycycline (Correct Answer)
- D. Vancomycin
- E. Azithromycin
Filarial nematodes Explanation: ***Doxycycline***
- The patient's symptoms (fever, cough, malaise, abdominal pain, **conjunctival suffusion** presenting as conjunctivitis, jaundice) after waterskiing in Hawaii are highly suggestive of **leptospirosis**, an infection caused by *Leptospira* bacteria.
- **Doxycycline** is the recommended treatment for mild to moderate leptospirosis, while severe cases (Weil's disease with jaundice) may require intravenous penicillin G or ceftriaxone.
- The biphasic illness pattern and water exposure history are classic features of this spirochete infection.
*Ganciclovir*
- **Ganciclovir** is an antiviral medication primarily used to treat **cytomegalovirus (CMV)** infections, especially in immunocompromised patients.
- The clinical picture presented does not align with typical CMV infection, which is often asymptomatic or causes mono-like symptoms without the water exposure history.
*Metronidazole*
- **Metronidazole** is an antibiotic effective against **anaerobic bacteria** and certain parasites (e.g., *Giardia*, *Trichomonas*).
- It is not indicated for the treatment of leptospirosis, which is caused by a spirochete requiring tetracyclines or beta-lactams.
*Vancomycin*
- **Vancomycin** is an antibiotic used for treating serious infections caused by **Gram-positive bacteria**, particularly **methicillin-resistant *Staphylococcus aureus* (MRSA)** or *Clostridioides difficile*.
- It is not effective against *Leptospira* species, which are spirochetes.
*Azithromycin*
- **Azithromycin** is a macrolide antibiotic effective against a range of bacterial infections, including **atypical pneumonia** and some sexually transmitted infections.
- While azithromycin has some activity against leptospirosis, **doxycycline** or penicillin-based antibiotics are strongly preferred as first-line treatment with better evidence base.
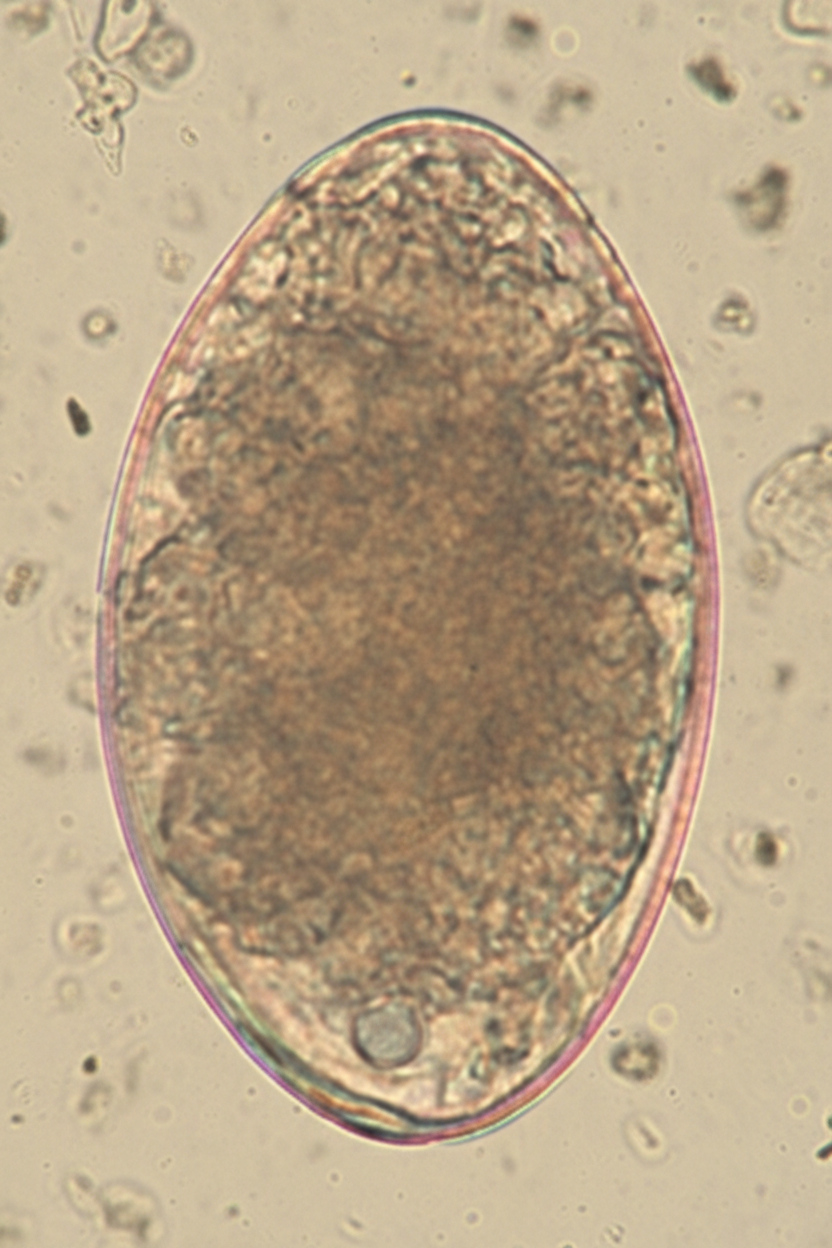
Filarial nematodes US Medical PG Question 3: A 40-year-old woman presents to clinic with multiple complaints. She complains of swelling around her eyes (Image A) and generalized weakness. A complete blood count reveals eosinophilia. She recently returned from a trip to Asia where she reports having eaten street food, including pork. If this patient's disease is explained by a parasite that causes inflammation of skeletal muscle, what would be the appropriate treatment?
- A. Praziquantel
- B. Niridazole
- C. Albendazole or mebendazole (Correct Answer)
- D. Ivermectin
- E. Diethylcarbamazine
Filarial nematodes Explanation: ***Albendazole or mebendazole***
- The clinical presentation (periorbital edema, myalgia/weakness, eosinophilia, recent travel to Asia with consumption of pork) strongly suggests **trichinellosis**, caused by *Trichinella spiralis*.
- **Albendazole** or **mebendazole** (both benzimidazole anthelmintics) are the drugs of choice for treating trichinellosis by killing adult worms in the intestine and larvae in muscle tissue.
- Treatment is most effective when started early in the course of infection.
*Praziquantel*
- This agent is primarily used to treat infections caused by **trematodes** (flukes) and **cestodes** (tapeworms), such as schistosomiasis and taeniasis.
- It is **not effective** against *Trichinella spiralis*.
*Niridazole*
- Niridazole is an **older antischistosomal drug** that is now rarely used due to significant side effects.
- It has **no activity** against *Trichinella spiralis*.
*Ivermectin*
- Ivermectin is effective against various **nematodes**, including *Onchocerca volvulus* (river blindness) and *Strongyloides stercoralis*.
- While it has some activity against *Trichinella*, it is generally considered less effective than benzimidazoles and **not the first-line treatment** for trichinellosis.
*Diethylcarbamazine*
- This medication is primarily used to treat **lymphatic filariasis** (*Wuchereria bancrofti*, *Brugia malayi*) and **loiasis** (*Loa loa*).
- It is **not effective** against *Trichinella spiralis* infection.
Filarial nematodes US Medical PG Question 4: A 32-year-old woman presents to your office with abdominal pain and bloating over the last month. She also complains of intermittent, copious, non-bloody diarrhea over the same time. Last month, she had a cough that has since improved but has not completely resolved. She has no sick contacts and has not left the country recently. She denies any myalgias, itching, or rashes. Physical and laboratory evaluations are unremarkable. Examination of her stool reveals the causative organism. This organism is most likely transmitted to the human host through which of the following routes?
- A. Insect bite
- B. Penetration of skin (Correct Answer)
- C. Sexual contact
- D. Inhalation
- E. Animal bite
Filarial nematodes Explanation: ***Penetration of skin***
- The symptoms of **abdominal pain**, **bloating**, **intermittent copious non-bloody diarrhea**, and a recent **cough** are highly suggestive of a **hookworm infection**.
- Hookworm larvae (filariform larvae) primarily penetrate the skin, usually through bare feet, as their mode of entry into the human host.
*Insect bite*
- Although some parasitic infections are transmitted by insect bites (e.g., malaria, Chagas disease), hookworms are not transmitted this way.
- **Insect-borne diseases** typically present with different clinical manifestations or geographical associations.
*Sexual contact*
- **Sexually transmitted infections** involve direct contact of mucous membranes or body fluids during sexual activity.
- Hookworm infection transmission through sexual contact is not a recognized route.
*Inhalation*
- **Inhalation** is a route of transmission for respiratory pathogens (e.g., influenza, tuberculosis) or certain fungal infections, but not for hookworms.
- While hookworm larvae migrate through the lungs, the initial infection pathway is not via inhalation.
*Animal bite*
- **Animal bites** transmit diseases like rabies or certain bacterial infections, but not parasitic hookworms.
- Hookworm infection does not result from direct contact with an animal's saliva or puncture wound.
Filarial nematodes US Medical PG Question 5: An otherwise healthy 39-year-old woman presents to her primary care provider because of right-leg swelling, which started 4 months ago following travel to Kenya. The swelling has been slowly progressive and interferes with daily tasks. She denies smoking or alcohol use. Family history is irrelevant. Vital signs include: temperature 38.1°C (100.5°F), blood pressure 115/72 mm Hg, and pulse 99/min. Physical examination reveals non-pitting edema of the entire right leg. The overlying skin is rough, thick and indurated. The left leg is normal in size and shape. Which of the following is the most likely cause of this patient condition?
- A. Obstruction of lymphatic channels (Correct Answer)
- B. Hypoalbuminemia
- C. Lymphatic hypoplasia
- D. Venous thromboembolism
- E. Persistent elevation of venous pressures
Filarial nematodes Explanation: ***Obstruction of lymphatic channels***
- The patient's history of travel to **Kenya**, along with **progressive, non-pitting edema** of the entire right leg and **rough, thick, indurated skin**, strongly suggests **filariasis**, a parasitic infection that obstructs lymphatic channels.
- **Obstruction of lymphatic channels** leads to **lymphedema**, which characteristically presents with the described symptoms and skin changes (e.g., **elephantiasis**).
*Hypoalbuminemia*
- **Hypoalbuminemia** typically causes **generalized, pitting edema** due to decreased plasma oncotic pressure, not localized, non-pitting edema in a single limb.
- There are no clinical signs to suggest **hepatic** or **renal dysfunction** that would cause significant hypoalbuminemia.
*Lymphatic hypoplasia*
- **Lymphatic hypoplasia** (primary lymphedema) is usually congenital or develops in early life and would not typically manifest acutely after travel in a 39-year-old.
- While it causes lymphedema, the travel history points to an acquired cause rather than a congenital defect.
*Venous thromboembolism*
- **Venous thromboembolism** (DVT) typically presents with acute onset of **painful, edematous** limb, often with **pitting edema**, and can be associated with warmth and erythema.
- The **slowly progressive** nature of the swelling over 4 months and **non-pitting edema** are less consistent with acute DVT.
*Persistent elevation of venous pressures*
- **Persistent elevation of venous pressures** (e.g., chronic venous insufficiency) leads to **pitting edema**, skin discoloration (**hyperpigmentation**), and **ulcerations**, not the rough, thick, indurated skin seen in this case.
- This condition is also typically associated with factors like prolonged standing or obesity, which are not mentioned here.
Filarial nematodes US Medical PG Question 6: A 16-year-old boy is brought to the physician by his host parents for evaluation of a progressively pruritic rash over his shoulders and buttocks for the past 6 months. He recently came to the United States from Nigeria to attend a year of high school. He reports that it has been increasingly difficult for him to read the whiteboard during classes. Physical examination shows symmetrically distributed papules 4–8 mm in diameter, excoriation marks, and patchy hyperpigmentation over his shoulders, waist, and buttocks. There is nontender inguinal lymphadenopathy and several firm, nontender subcutaneous nodules along the right iliac crest. Six skin snip biopsies are taken from the pelvic girdle, buttocks, and thigh, and are then incubated in saline. After 24 hours, microscopic examination shows motile microfilariae. Which of the following is the most likely diagnosis?
- A. Cysticercosis
- B. Onchocerciasis (Correct Answer)
- C. Lymphatic filariasis
- D. Cutaneous larva migrans
- E. Trichuriasis
Filarial nematodes Explanation: ***Onchocerciasis***
- The presentation of **pruritic rash with papules**, **subcutaneous nodules** (onchocercomas), and **visual difficulties** (river blindness) in an individual from an endemic area (Nigeria) is classic for **onchocerciasis**.
- The presence of **motile microfilariae in skin snips** after saline incubation is a diagnostic hallmark of this condition, caused by *Onchocerca volvulus*.
*Cysticercosis*
- This condition is caused by the larval stage of *Taenia solium* and typically presents with **calcified lesions** in the muscle and brain (neurocysticercosis), which can lead to seizures.
- It does not typically cause the generalized pruritic rash, subcutaneous nodules, or ocular symptoms described, nor would **motile microfilariae** be found in skin snips.
*Lymphatic filariasis*
- Caused by *Wuchereria bancrofti* or *Brugia malayi*, this disease is characterized by **lymphedema** and **hydrocele**, eventually leading to **elephantiasis**.
- While it involves filarial worms and can cause lymphadenopathy, it does not typically manifest with the described rash, vision problems, or **subcutaneous nodules** (onchocercomas).
*Cutaneous larva migrans*
- This condition, caused by hookworm larvae (e.g., *Ancylostoma braziliense*), presents as a **serpiginous, intensely pruritic eruption** where the larvae migrate under the skin.
- It does not cause subcutaneous nodules, generalized papular rash, or ocular involvement, and skin snips would not show **microfilariae**.
*Trichuriasis*
- Caused by the **whipworm** (*Trichuris trichiura*), this is an intestinal nematode infection that can lead to **abdominal pain**, **diarrhea**, **rectal prolapse**, and **anemia**.
- It does not present with skin lesions, subcutaneous nodules, or visual impairment, and diagnosis is typically made by finding **ova in stool samples**, not microfilariae in skin snips.
Filarial nematodes US Medical PG Question 7: A previously healthy 48-year-old man comes to the physician because of a 2-week history of a nonpruritic rash on his right forearm. The rash began as pustules and progressed to form nodules and ulcers. He works as a gardener. Physical examination shows right axillary lymphadenopathy and the findings in the photograph. Which of the following is the most likely causal organism?
- A. Bartonella henselae
- B. Sporothrix schenckii (Correct Answer)
- C. Pasteurella multocida
- D. Blastomyces dermatitidis
- E. Pseudomonas aeruginosa
Filarial nematodes Explanation: ***Sporothrix schenckii***
- The patient's occupation as a **gardener** and the description of a rash progressing from **pustules to nodules and ulcers**, associated with **axillary lymphadenopathy** along a lymphatic chain, are classic findings of **sporotrichosis** (rose gardener's disease), caused by *Sporothrix schenckii*.
- This fungus is found in soil and on plants, and infection typically occurs via **traumatic inoculation** (e.g., thorn prick).
*Bartonella henselae*
- This bacterium causes **cat-scratch disease**, characterized by a papule or pustule at the inoculation site and regional lymphadenopathy.
- While it causes lymphadenopathy, the skin lesions typically do not progress to the chronic **ulcerative and nodular pattern along lymphatic drainage** seen here, and there's no history of cat exposure.
*Pasteurella multocida*
- *Pasteurella multocida* is a common cause of **wound infections after animal bites or scratches**, particularly from cats and dogs.
- Infections typically manifest as rapid onset of **erythema, swelling, and pain** at the bite site, often with cellulitis, rather than the described pustular-to-nodular-to-ulcerative progression along lymphatic channels.
*Blastomyces dermatitidis*
- *Blastomyces dermatitidis* causes **blastomycosis**, a systemic fungal infection that can present with cutaneous lesions, often **papules, pustules, or ulcers**, but these are typically associated with **pulmonary involvement** and occur after inhalation of spores, not directly from skin inoculation with lymphatic spread in a gardener.
- The skin lesions of blastomycosis are often described as **verrucous** with sharply demarcated borders.
*Pseudomonas aeruginosa*
- *Pseudomonas aeruginosa* can cause various skin infections, especially in immunocompromised individuals, those with burns, or associated with water exposure (e.g., **"hot tub folliculitis"**).
- While it can cause pustules, it does not typically produce the **lymphocutaneous spread** of nodules and ulcers observed in this patient's presentation.
Filarial nematodes US Medical PG Question 8: A 29-year-old internal medicine resident presents to the emergency department with complaints of fevers, diarrhea, abdominal pain, and skin rash for 2 days. He feels fatigued and has lost his appetite. On further questioning, he says that he returned from his missionary trip to Brazil last week. He is excited as he talks about his trip. Besides a worthy clinical experience, he also enjoyed local outdoor activities, like swimming and rafting. His past medical history is insignificant. The blood pressure is 120/70 mm Hg, the pulse is 100/min, and the temperature is 38.3°C (100.9°F). On examination, there is a rash on the legs. The rest of the examination is normal. Which of the following organisms is most likely responsible for this patient’s condition?
- A. Schistosoma mansoni (Correct Answer)
- B. Schistosoma haematobium
- C. Vibrio cholerae
- D. Onchocerca volvulus
- E. Schistosoma japonicum
Filarial nematodes Explanation: ***Schistosoma mansoni***
- The patient's symptoms (fevers, diarrhea, abdominal pain, rash, fatigue) after swimming and rafting in Brazil are classic for **acute schistosomiasis (Katayama fever)**, and *Schistosoma mansoni* is endemic to South America, including Brazil, affecting the **gastrointestinal tract**.
- The rash on the legs is consistent with the entry points of **cercariae** through the skin, and the systemic symptoms develop as the adult worms mature and lay eggs.
*Schistosoma haematobium*
- This species primarily causes **urinary schistosomiasis**, with symptoms like **hematuria**, dysuria, and bladder wall calcification.
- It is prevalent in Africa and the Middle East, not typically associated with Brazil.
*Vibrio cholerae*
- *Vibrio cholerae* causes severe, watery **diarrhea** (rice-water stools) and rapid **dehydration**, usually without a prominent rash or prolonged systemic symptoms like fatigue and fever as the primary presentation.
- While diarrhea is present, the array of other symptoms and the exposure history do not align with cholera.
*Onchocerca volvulus*
- This parasite causes **onchocerciasis (river blindness)**, transmitted by blackflies, and primarily manifests as **dermatitis**, subcutaneous nodules, and significant eye disease leading to blindness.
- It does not typically cause acute febrile illness with prominent gastrointestinal symptoms like those described.
*Schistosoma japonicum*
- *Schistosoma japonicum* is found in East Asia (e.g., China, Philippines), not South America, and primarily affects the **gastrointestinal tract** and liver, similar to *S. mansoni*.
- The geographical exposure to Brazil makes *S. mansoni* the most likely cause, despite similar clinical features to *S. japonicum*.
Filarial nematodes US Medical PG Question 9: A 19-year-old woman presents to the emergency department with complaints of blurry vision and headaches that started 2 days ago. She reports that she has been experiencing some facial pain, but she thought it was related to her toothache. She is also worried about a black spot that is increasing in size on her face over the last month. She expresses concerns about her frequency of urination. Recently, she had a runny nose and cough that resolved spontaneously. The patient was diagnosed with type 1 diabetes mellitus at 13 years of age. She is a non-smoker and drinks beer occasionally. Her blood pressure is 122/98 mm Hg and temperature is 37.2°C (98.9°F). The physical examination is normal with the exception of a black necrotic eschar lateral to the right nasal ala. She lost 2.7 kg (6 lb) since her last visit, which was 6 months ago. A routine urinalysis at the office is positive for glucose and ketones. What is the most likely cause of the patient’s symptoms?
- A. Bacillus anthracis
- B. Mucormycosis (Correct Answer)
- C. Clostridium difficile
- D. Histoplasma capsulatum
- E. Aspergillus fumigatus
Filarial nematodes Explanation: ***Mucormycosis***
- This patient, with uncontrolled **Type 1 diabetes** (indicated by frequent urination, weight loss, and glucose/ketones in urine), is at high risk for **mucormycosis**, an opportunistic fungal infection.
- The presence of a **black necrotic eschar** on the face, coupled with eye symptoms (blurry vision) and facial pain, is highly characteristic of **rhino-orbital-cerebral mucormycosis**, which often originates in the sinuses.
*Bacillus anthracis*
- **Cutaneous anthrax** would present as a painless ulcer with a black eschar, but it typically occurs in individuals exposed to infected animals or animal products and is not associated with diabetes or the rhinocerebral symptoms described.
- Systemic symptoms like blurry vision, headaches, and polyuria are not typical for cutaneous anthrax.
*Clostridium difficile*
- This bacterium primarily causes **gastrointestinal infections**, leading to diarrhea, abdominal pain, and fever.
- There are no symptoms described that suggest a *C. difficile* infection, and it does not cause facial eschars or rhino-orbital symptoms.
*Histoplasma capsulatum*
- **Histoplasmosis** is a fungal infection typically acquired by inhaling spores, often found in bird or bat droppings, mainly affecting the lungs.
- While it can disseminate in immunocompromised individuals, causing mucocutaneous lesions, it typically doesn't present with a rapid-onset facial eschar or the specific rhino-orbital symptoms seen here.
*Aspergillus fumigatus*
- Although **invasive aspergillosis** can occur in immunocompromised patients, including those with diabetes, it more commonly affects the lungs (e.g., aspergilloma, chronic pulmonary aspergillosis).
- While it can cause sinusitis and, rarely, cutaneous lesions, the rapid progression to a **black necrotic eschar** in the context of uncontrolled diabetes points more strongly towards mucormycosis.
Filarial nematodes US Medical PG Question 10: A 75-year-old man who underwent a bilateral lung transplant 11 months ago presented to the emergency room with fevers and chills. After the transplant procedure, he was immediately placed on immunosuppressive treatment; however, for unknown reasons he stopped taking the prophylactically-prescribed voriconazole (a triazole antifungal medication used for the treatment and prevention of invasive fungal infections). Upon presentation to the emergency room, the patient was hypoxemic. Imaging revealed pulmonary nodules, which prompted a transbronchial biopsy for further evaluation. The results were negative for acute organ rejection, adenovirus, cytomegalovirus, and acid-fast bacilli. Slides stained with hematoxylin and eosin (H&E) were also prepared, as presented on the upper panel of the accompanying picture, which revealed large round structures. The specimen was sent to the microbiology laboratory for fungal culture, which resulted in the growth of a fuzzy mold on Sabouraud agar (selective medium for the isolation of fungi) at 30.0°C (86.0°F). A lactophenol cotton blue preparation revealed the organism shown on the lower panel of the accompanying picture. What organism has infected this patient?
- A. Blastomyces dermatitidis
- B. Malbranchea species
- C. Cryptococcus neoformans
- D. Coccidioides species (Correct Answer)
- E. Histoplasma capsulatum
Filarial nematodes Explanation: ***Coccidioides species***
- The imaging showing **pulmonary nodules**, the biopsy revealing **large round structures** (spherules), and growth of a **fuzzy mold** on Sabouraud agar in an **immunosuppressed patient** are highly characteristic of Coccidioides infection.
- The **transplant recipient** is at high risk for opportunistic fungal infections, and the visual evidence from the biopsy (spherules) is pathognomonic for **coccidioidomycosis**.
*Blastomyces dermatitidis*
- While it causes **pulmonary disease** and can present with pulmonary nodules, its characteristic microscopic appearance in tissue would be **broad-based budding yeasts**, which is distinct from the large round structures (spherules) seen in the image.
- Blastomyces grows as a mold at room temperature but converts to a yeast form in tissue.
*Malbranchea species*
- **Malbranchea** is a saprophytic fungus and is **not typically considered a human pathogen**, especially in the context of invasive pulmonary disease with specific histological findings like spherules.
- It would not match the clinical presentation or the histological findings described.
*Cryptococcus neoformans*
- **Cryptococcus neoformans** typically presents as **encapsulated yeast cells** in tissue, often associated with a prominent capsule visualized with India ink stain, and primarily causes meningitis in immunocompromised individuals.
- It does not form the large round spherules seen in the biopsy.
*Histoplasma capsulatum*
- **Histoplasma capsulatum** is a **dimorphic fungus** that presents as small, budding yeasts within macrophages in tissue samples, which is a different morphology than the large round structures described.
- While it can cause pulmonary nodules, the specific histological findings do not align.
More Filarial nematodes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.