Dermatophytes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Dermatophytes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Dermatophytes US Medical PG Question 1: A 10-year-old girl presents to the clinic, with her mother, complaining of a circular, itchy rash on her scalp for the past 3 weeks. Her mother is also worried about her hair loss. The girl has a past medical history significant for asthma. She needs to use her albuterol inhaler once per week on average. Her blood pressure is 112/70 mm Hg; the heart rate is 104/min; the respiratory rate is 20/min, and the temperature is 37.0°C (98.6°F). On exam, the patient is alert and interactive. Her lungs are clear on bilateral auscultation. On palpation, a tender posterior cervical node is present on the right side. Examination of the head is shown in the image. Which of the following is the best treatment option for the patient?
- A. Subcutaneous triamcinolone
- B. Topical betamethasone
- C. Ketoconazole shampoo
- D. Oral terbinafine (Correct Answer)
- E. Oral doxycycline
Dermatophytes Explanation: ***Oral terbinafine***
- The patient's clinical presentation with an **itchy, circular rash** and **hair loss** on the scalp, along with a **tender posterior cervical node**, is highly suggestive of **tinea capitis**.
- **Oral antifungals** like terbinafine are the **first-line treatment** for tinea capitis because topical agents cannot effectively penetrate the hair shaft where the fungus resides.
*Subcutaneous triamcinolone*
- Triamcinolone is a **corticosteroid** and is used to treat inflammatory conditions, not fungal infections.
- While it might reduce swelling or itching temporarily, it would **not eradicate the underlying fungal infection** and could potentially worsen it.
*Topical betamethasone*
- Betamethasone is a **topical corticosteroid** which might reduce inflammation and itchiness.
- However, topical antifungals and steroids are **ineffective for tinea capitis** as they do not reach the fungal elements within the hair follicles.
*Ketoconazole shampoo*
- While ketoconazole is an antifungal, **shampoo formulations** are generally **not sufficient** to treat tinea capitis on their own.
- They can be used as an **adjunct** to oral therapy to reduce shedding of fungal spores and prevent spread but cannot cure the infection effectively.
*Oral doxycycline*
- Doxycycline is an **antibiotic** primarily used to treat bacterial infections, and some inflammatory skin conditions such as acne or rosacea.
- It has **no antifungal properties** and would be completely ineffective against tinea capitis.
Dermatophytes US Medical PG Question 2: A 23-year-old woman comes to the physician because of a 5-month history of a pruritic rash on the bilateral upper extremities. She has no history of serious illness and takes no medications. A skin biopsy of the rash shows intraepidermal accumulation of edematous fluid and widening of intercellular spaces between keratinocytes. Which of the following is the most likely diagnosis?
- A. Dermatitis herpetiformis
- B. Eczematous dermatitis (Correct Answer)
- C. Acanthosis nigricans
- D. Lichen planus
- E. Psoriasis vulgaris
Dermatophytes Explanation: ***Eczematous dermatitis***
- The biopsy findings of **intraepidermal edema** and **widening of intercellular spaces between keratinocytes (spongiosis)** are classic histopathologic features of eczematous dermatitis.
- The clinical presentation of a **pruritic rash** on the upper extremities further supports this diagnosis, as eczema is characterized by itching and inflammation.
*Dermatitis herpetiformis*
- This condition is characterized by **subepidermal vesicles** and **neutrophilic infiltrates** in the dermal papillae, with IgA deposition, which differs from the findings described.
- It is strongly associated with **celiac disease** and presents with intensely pruritic, grouped papules and vesicles, predominantly on extensor surfaces.
*Acanthosis nigricans*
- Histologically, acanthosis nigricans shows **papillomatosis** and **hyperkeratosis**, with epidermal thickening, rather than intraepidermal edema or spongiosis.
- Clinically, it presents as **hyperpigmented, velvety plaques** in intertriginous areas, not a generalized pruritic rash.
*Lichen planus*
- Biopsy of lichen planus would reveal a **band-like lymphocytic infiltrate** at the dermoepidermal junction, **sawtooth rete ridges**, and **Civatte bodies**.
- Clinically, it often presents with **pruritic, polygonal, purple, planar papules and plaques** (the 6 Ps), which is not consistent with the described rash.
*Psoriasis vulgaris*
- Histopathologically, psoriasis is characterized by **acanthosis**, **parakeratosis**, **Munro microabscesses**, and **dilated blood vessels** in the dermal papillae.
- Clinically, it manifests as **erythematous plaques with silvery scales**, typically on extensor surfaces, distinguishing it from a generalized pruritic rash with spongiosis.
Dermatophytes US Medical PG Question 3: A 28-year-old homeless male with a past medical history significant for asthma comes to your clinic complaining of a chronic rash on his scalp and feet. He describes the rash as “dry and flaky,” and reports it has been present for at least a year. He was using a new dandruff shampoo he got over the counter, with little improvement. The patient reports it is extremely itchy at night, to the point that he can't sleep. On exam, you note a scaly patch of alopecia, enlarged lymph glands along the posterior aspect of his neck, and fine scaling in between his toes and on the heel and sides of his foot. His temperature is 99°F (37°C), blood pressure is 118/78 mmHg, and pulse is 81/min. Which of the following is the most accurate test for the suspected diagnosis?
- A. KOH preparation of scalp scraping (Correct Answer)
- B. Wood's lamp
- C. Skin biopsy with histopathological examination
- D. CBC and total serum IgE
- E. Culture on Sabouraud dextrose agar
Dermatophytes Explanation: ***KOH preparation of scalp scraping***
- The patient's presentation with **chronic, itchy, scaly scalp rash** (alopecia and enlarged lymph glands) and **fungal-like rash on feet** (scaling between toes, heel, and sides) strongly suggests a dermatophyte infection (**tinea capitis** and **tinea pedis**).
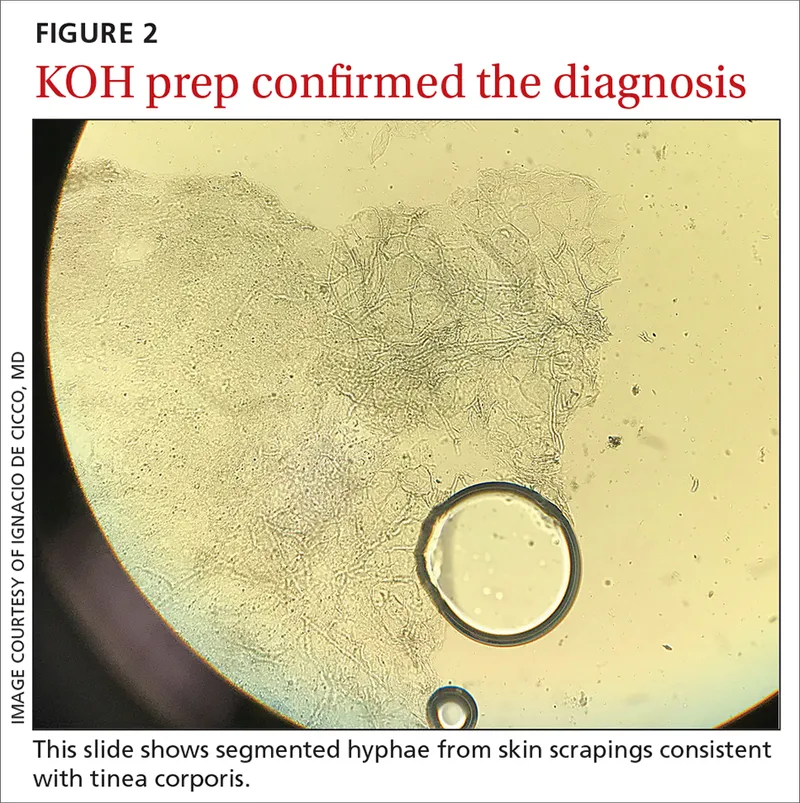
- A **KOH preparation** allows for direct visualization of **fungal hyphae and spores**, confirming the presence of a fungal infection quickly and accurately.
- This is the **most accurate rapid diagnostic test** for dermatophyte infections.
*Wood's lamp*
- A Wood's lamp is useful for certain types of **tinea capitis** (e.g., those caused by *Microsporum* species) that **fluoresce**, but it is not accurate for all dermatophyte infections (e.g., *Trichophyton* species do not fluoresce).
- It is a screening tool but **not a definitive diagnostic test** for all fungal infections, as it doesn't confirm the presence of fungi directly.
*Skin biopsy with histopathological examination*
- While a **skin biopsy** can identify fungal elements on histopathology (especially with PAS stain), it is **invasive, expensive, and unnecessary** for a straightforward clinical presentation of dermatophyte infection.
- Biopsy is typically reserved for cases where the diagnosis is unclear or when malignancy or other inflammatory conditions need to be ruled out.
*CBC and total serum IgE*
- A **CBC (complete blood count)** and **total serum IgE** would be helpful in diagnosing allergic conditions or parasitic infections, but are not direct diagnostic tools for fungal infections.
- While asthma (an allergic condition) is in the patient's history, the rash description is more consistent with a **fungal etiology** rather than an allergic one alone.
*Culture on Sabouraud dextrose agar*
- **Fungal culture** on Sabouraud dextrose agar is a confirmatory test that identifies the specific species of dermatophyte and can guide treatment if initial therapies fail.
- However, it takes **2-4 weeks** for results, making it less practical for initial diagnosis compared to a **KOH preparation**, which provides rapid results within minutes.
Dermatophytes US Medical PG Question 4: An 18-year-old man presents to the office, complaining of an itchy patch on his torso that appeared one week ago. The patient is on the college wrestling team and is concerned he will not be able to compete if it gets infected. He has no significant medical history, and his vital signs are within normal limits. On examination, there is an erythematous, scaly plaque with central clearing at approximately the level of rib 6 on the left side of his torso. What diagnostic test would be most appropriate at this time?
- A. Eaton agar
- B. Wood’s lamp examination
- C. Thayer-Martin agar
- D. Sabouraud agar
- E. KOH preparation (Correct Answer)
Dermatophytes Explanation: ***KOH preparation***
- A **KOH (potassium hydroxide) preparation** is the most appropriate initial diagnostic test for suspected **dermatophytosis** (ringworm), a common fungal infection often seen in wrestlers due to skin-to-skin contact.
- The KOH dissolves keratin and cellular debris, allowing for easier visualization of **fungal hyphae** and **spores** under a microscope, confirming the diagnosis.
*Eaton agar*
- **Eaton agar** is a specialized culture medium used for isolating and growing **Mycoplasma pneumoniae**, a bacterium that causes respiratory infections.
- It is not used for diagnosing fungal skin infections.
*Wood’s lamp examination*
- A **Wood's lamp examination** uses ultraviolet light to detect certain dermatophytes (like *Microsporum canis*), which may fluoresce
- However, many common dermatophytes, such as *Trichophyton rubrum*, do not fluoresce, making KOH preparation a more universally effective initial diagnostic tool.
*Thayer-Martin agar*
- **Thayer-Martin agar** is a selective culture medium primarily used for isolating and growing **Neisseria gonorrhoeae** and **Neisseria meningitidis**, bacteria responsible for sexually transmitted infections and meningitis, respectively.
- It is not indicated for diagnosing fungal skin infections.
*Sabouraud agar*
- **Sabouraud agar** is a recognized culture medium specifically designed for the isolation and identification of **fungi**, including dermatophytes.
- While useful for confirmation and species identification, a **KOH preparation** is a quicker and more immediate diagnostic test to confirm the presence of fungal elements in the clinic.
Dermatophytes US Medical PG Question 5: A 15-year-old boy is brought to the physician with an ongoing pruritic rash for 1 week. The rash is on his right forearm (refer to the image). He has not had a similar rash in the past. He has no history of allergies, and he is not taking any medications. He frequently enjoys gardening in their backyard. They have no household pets. The physical examination reveals no other abnormalities. Given the most likely diagnosis, which of the following is the most appropriate treatment of the condition described in this case?
- A. Topical salicylic acid
- B. Oral terbinafine
- C. Topical hydrocortisone
- D. Topical clotrimazole (Correct Answer)
- E. Oral acitretin
Dermatophytes Explanation: ***Topical clotrimazole***
- This patient's symptoms (pruritic rash, gardening hobby) are highly suggestive of **tinea corporis** (ringworm), a **fungal infection** often acquired from contact with infected soil or plants.
- **Topical imidazole antifungals** like clotrimazole are the first-line treatment for localized tinea corporis.
*Oral terbinafine*
- Oral antifungals like terbinafine are reserved for **widespread, severe, or recalcitrant fungal infections**, or involvement of the hair/nails (tinea capitis or onychomycosis).
- Given the localized nature of the rash on the forearm and no previous history, a topical agent is generally sufficient.
*Topical salicylic acid*
- Salicylic acid is a **keratolytic agent** used to treat conditions with thickened or scaly skin, such as **acne, psoriasis, or warts**.
- It does not have primary antifungal properties and would not be effective against tinea corporis.
*Topical hydrocortisone*
- Hydrocortisone is a **low-potency topical corticosteroid** used to reduce inflammation and itching in conditions like **eczema or contact dermatitis**.
- While it may temporarily relieve itching, it can **worsen fungal infections** by suppressing the local immune response, making it inappropriate for tinea.
*Oral acitretin*
- Acitretin is a **retinoid medication** primarily used to treat **severe psoriasis** and other keratinization disorders.
- It has no role in the direct treatment of fungal infections like tinea corporis.
Dermatophytes US Medical PG Question 6: A 48-year-old man comes to the physician because of a hypopigmented skin lesion on his finger. He first noticed it 4 weeks ago after cutting his finger with a knife while preparing food. He did not feel the cut. For the past week, he has also had fever, fatigue, and malaise. He has not traveled outside the country since he immigrated from India to join his family in the United States 2 years ago. His temperature is 38.7°C (101.7°F). Physical examination shows a small, healing laceration on the dorsal aspect of the left index finger and an overlying well-defined, hypopigmented macule with raised borders. Sensation to pinprick and light touch is decreased over this area. Which of the following is the most likely causal pathogen of this patient's condition?
- A. Epidermophyton floccosum
- B. Mycobacterium leprae (Correct Answer)
- C. Malassezia furfur
- D. Pseudomonas aeruginosa
- E. Leishmania donovani
Dermatophytes Explanation: ***Mycobacterium leprae***
- The patient's history of immigration from **India**, a country endemic for leprosy, coupled with the **hypopigmented, anesthetic skin lesion** with raised borders, is classic for **leprosy** (Hansen's disease).
- The diminished sensation to pinprick and light touch in the affected area points to **nerve involvement**, a hallmark of *Mycobacterium leprae* infection.
*Epidermophyton floccosum*
- This fungus primarily causes **tinea infections** (ringworm), such as athlete's foot and jock itch.
- While it can cause skin lesions, they are typically **erythematous** and scaly, not hypopigmented with sensory loss.
*Malassezia furfur*
- This yeast is responsible for **tinea versicolor**, characterized by **hypopigmented or hyperpigmented patches** that typically scale.
- However, it does not cause **nerve damage** or accompanying sensory loss, and systemic symptoms like fever and malaise are not typical.
*Pseudomonas aeruginosa*
- This bacterium can cause various opportunistic infections, including skin infections like **ecthyma gangrenosum** or **folliculitis** in immunocompromised patients.
- *Pseudomonas* infections are usually painful, often associated with a characteristic **grape-like odor**, and do not typically present with chronic, anesthetic, hypopigmented lesions.
*Leishmania donovani*
- This parasite causes **visceral leishmaniasis** (kala-azar), which presents with fever, weight loss, hepatosplenomegaly, and **hyperpigmentation of the skin** (darkening), not hypopigmentation.
- It does not cause localized anesthetic skin lesions like those described in the patient.
Dermatophytes US Medical PG Question 7: A 17-year-old boy comes to the physician because of a nonpruritic rash on his chest for 1 week. He returned from a trip to Puerto Rico 10 days ago. He started using a new laundry detergent after returning. He has type 1 diabetes mellitus controlled with insulin. His mother has Hashimoto thyroiditis, and his sister has severe facial acne. Examination of the skin shows multiple, nontender, round, hypopigmented macules on the chest and trunk. There is fine scaling when the lesions are scraped with a spatula. Which of the following is the most likely underlying mechanism of this patient's symptoms?
- A. Increased sebum production
- B. Infection with Trichophyton rubrum
- C. Increased growth of Malassezia globosa (Correct Answer)
- D. Antigen uptake by Langerhans cells
- E. Autoimmune destruction of melanocytes
Dermatophytes Explanation: ***Increased growth of Malassezia globosa***
- The clinical presentation of **hypopigmented macules with fine scaling** on the chest and trunk, especially in a young male who recently traveled to a tropical climate (Puerto Rico), is highly characteristic of **tinea versicolor**.
- Tinea versicolor is caused by an overgrowth of **Malassezia species** (primarily *M. globosa*), a commensal yeast that thrives in warm, humid conditions and is often associated with oily skin, leading to dyspigmentation and scaling due to interference with melanin production.
*Increased sebum production*
- While increased sebum production can contribute to a favorable environment for fungal growth, it is the underlying mechanism for conditions like **acne vulgaris** and **seborrheic dermatitis**, which present differently (e.g., comedones, inflammatory papules, erythema, greasy scales).
- This patient's rash is specifically described as hypopigmented macules with fine scaling, not inflammatory papules or pustules typical of acne, nor the greasy scales of seborrheic dermatitis.
*Infection with Trichophyton rubrum*
- **Trichophyton rubrum** is a dermatophyte commonly responsible for **tinea corporis** (ringworm of the body), **tinea pedis** (athlete's foot), and **tinea cruris** (jock itch), which typically present as **erythematous, annular, itchy lesions with raised borders**.
- The rash described here (hypopigmented, nonpruritic macules) does not fit the typical presentation of dermatophyte infections caused by *Trichophyton rubrum*.
*Antigen uptake by Langerhans cells*
- **Antigen uptake by Langerhans cells** is a crucial step in the pathogenesis of **allergic contact dermatitis**, where the skin reacts to an external allergen after sensitization, mediated by a **Type IV hypersensitivity reaction**.
- While the patient used a new laundry detergent, the rash's appearance (**hypopigmented macules with fine scaling**) is incongruent with contact dermatitis, which usually presents as an **erythematous, pruritic, vesicular, or eczematous rash** in the contact area.
*Autoimmune destruction of melanocytes*
- **Autoimmune destruction of melanocytes** is the underlying mechanism for **vitiligo**, an autoimmune condition characterized by **well-demarcated, completely depigmented patches** of skin.
- The lesions in this patient are described as **hypopigmented** (reduced pigmentation), not completely depigmented, and show **fine scaling**, which is not a feature of vitiligo.
Dermatophytes US Medical PG Question 8: You are seeing an otherwise healthy 66-year-old male in clinic who is complaining of localized back pain and a new rash. On physical exam, his vital signs are within normal limits. You note a vesicular rash restricted to the upper left side of his back. In order to confirm your suspected diagnosis, you perform a diagnostic test. What would you expect to find on the diagnostic test that was performed?
- A. Gram negative bacilli
- B. Branching pseudohyphae
- C. Pear shaped motile cells
- D. Multinucleated giant cells (Correct Answer)
- E. Gram positive cocci
Dermatophytes Explanation: ***Multinucleated giant cells***
- The patient's presentation of a **unilateral, vesicular rash** in an older adult, along with localized back pain, is highly suggestive of **herpes zoster (shingles)**.
- A Tzanck smear, a common diagnostic test for vesicular lesions, would reveal **multinucleated giant cells** and **intranuclear inclusions**, characteristic cytopathic effects of herpesviruses like VZV.
*Gram negative bacilli*
- This finding would suggest a **bacterial infection**, typically not associated with vesicular rashes like shingles.
- Gram-negative bacilli are often implicated in conditions such as **urinary tract infections** or **sepsis**, not dermatological viral infections.
*Branching pseudohyphae*
- This microscopic feature is characteristic of **fungal infections**, specifically **Candida species**, which present as a candidiasis rash, not a dermatomal vesicular rash.
- Fungal rashes are typically erythematous and can be pruritic but do not usually form discrete vesicles in a dermatomal distribution.
*Pear shaped motile cells*
- This describes **Trichomonas vaginalis**, a parasite causing sexually transmitted infections, primarily **vaginitis** or **urethritis**.
- This finding would be completely unrelated to a vesicular skin rash or the suspected diagnosis of shingles.
*Gram positive cocci*
- This finding is indicative of a **bacterial infection**, such as those caused by **Staphylococcus aureus** or **Streptococcus pyogenes**.
- While these bacteria can cause skin infections (e.g., impetigo, cellulitis), they do not produce the classic unilateral vesicular rash of shingles and would not involve multinucleated giant cells on microscopy.
Dermatophytes US Medical PG Question 9: A 50-year-old HIV-positive male presents to the ER with a two-day history of fever and hemoptysis. Chest radiograph shows a fibrocavitary lesion in the right middle lobe. Biopsy of the afflicted area demonstrates septate hyphae that branch at acute angles. Which of the following is the most likely causal organism?
- A. Mycobacterium tuberculosis
- B. Pneumocystis jirovecii
- C. Aspergillus fumigatus (Correct Answer)
- D. Candida albicans
- E. Mucor species
Dermatophytes Explanation: ***Aspergillus fumigatus***
- The combination of **fever**, **hemoptysis**, a **fibrocavitary lesion** in an **HIV-positive** patient, and the presence of **septate hyphae branching at acute angles** on biopsy are classic findings for invasive **aspergillosis**.
- **Aspergillus** specifically targets individuals with compromised immune systems, and the pathological description of the hyphae is highly characteristic of this fungus.
*Mycobacterium tuberculosis*
- While **Mycobacterium tuberculosis** can cause **fever**, **hemoptysis**, and **cavitary lesions** in HIV-positive patients, the microscopic description of **septate hyphae branching at acute angles** is not consistent with bacterial infection.
- Tuberculosis is characterized by **acid-fast bacilli** and granulomatous inflammation, not fungal hyphae.
*Mucor species*
- **Mucor** (along with Rhizopus) causes **mucormycosis**, an invasive fungal infection that can affect immunocompromised patients and present with pulmonary involvement and cavitary lesions.
- However, mucormycosis is characterized by **non-septate (aseptate) hyphae branching at right (90-degree) angles**, not septate hyphae at acute angles, making it distinguishable from Aspergillus.
*Pneumocystis jirovecii*
- **Pneumocystis jirovecii** is a common cause of pneumonia in HIV-positive patients, typically presenting as **diffuse interstitial infiltrates** rather than cavitary lesions.
- Microscopic examination would reveal **cysts** and **trophozoites**, not septate hyphae, making it inconsistent with the biopsy findings.
*Candida albicans*
- While **Candida albicans** can cause infections in immunocompromised individuals, it typically presents as **oral thrush**, esophagitis, or disseminated candidiasis.
- Pulmonary involvement is less common and usually manifests as **pneumonitis** rather than cavitary lesions, and its hyphae are typically **pseudohyphae** or budding yeasts, not septate hyphae branching at acute angles.
Dermatophytes US Medical PG Question 10: A 28-year-old woman with a past history of type 1 diabetes presents to your office with a 2-week history of vaginal itching and soreness accompanied by a white, clumpy vaginal discharge which she says resembles cheese curds. Her last HbA1c from a month ago was 7.8%, and her last cervical cytology from 10 months ago was reported as normal. She has a blood pressure of 118/76 mmHg, respiratory rate of 14/min, and heart rate of 74/min. Pelvic examination reveals multiple small erythematous lesions in the inguinal and perineal area, vulvar erythema, and excoriations. Inspection demonstrates a normal cervix and a white, adherent, thick, non-malodorous vaginal discharge. Which of the following is most likely to be present in a saline wet mount from the vaginal discharge of this patient?
- A. Clue cells on saline smear
- B. Gram-negative diplococci
- C. Hyphae (Correct Answer)
- D. Motile flagellates
- E. Multinucleated giant cells
Dermatophytes Explanation: ***Hyphae***
- The patient's symptoms of **vaginal itching**, soreness, and a **white, clumpy discharge resembling cheese curds** are classic for **vulvovaginal candidiasis** (yeast infection).
- A **saline wet mount** in such cases typically reveals **hyphae** and **budding yeast forms** of *Candida albicans*.
*Clue cells on saline smear*
- **Clue cells** are characteristic of **bacterial vaginosis**, which is typically associated with a **thin, grayish discharge** and a **fishy odor** (amine odor), neither of which are described here.
- The discharge in this patient is described as **thick and non-malodorous**, which is inconsistent with bacterial vaginosis.
*Gram-negative diplococci*
- **Gram-negative diplococci** are the hallmark of **gonorrhea**, caused by *Neisseria gonorrhoeae*.
- Gonorrhea often presents with **purulent discharge** and cervical inflammation, or it can be asymptomatic; it does not typically cause the **clumpy discharge** and intense itching seen in this patient.
*Motile flagellates*
- **Motile flagellates** are characteristic of **trichomoniasis**, caused by *Trichomonas vaginalis*.
- This infection usually presents with a **frothy, yellow-green discharge**, a **fishy odor**, and cervical petechiae (strawberry cervix), which are not a feature of this patient's presentation.
*Multinucleated giant cells*
- **Multinucleated giant cells** are indicative of **herpes simplex virus (HSV) infection**, particularly when found on a **Tzanck smear** of a lesion.
- While the patient has erythematous lesions, the primary complaint of **vaginal discharge** and itching points away from herpes as the main cause of the discharge.
More Dermatophytes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.