Cryptococcus neoformans/gattii US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cryptococcus neoformans/gattii. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cryptococcus neoformans/gattii US Medical PG Question 1: You are taking care of a patient with renal failure secondary to anti-fungal therapy. The patient is a 66-year-old male being treated for cryptococcal meningitis. This drug has a variety of known side effects including acute febrile reactions to infusions, anemia, hypokalemia and hypomagnesemia. What is the mechanism of action of this drug?
- A. Inhibition of squalene epoxidase
- B. Binding of the 50S subunit
- C. Pore formation secondary to ergosterol binding (Correct Answer)
- D. Disruption of microtubule formation
- E. Inhibition of 1,3-beta-glucan synthase
Cryptococcus neoformans/gattii Explanation: ***Pore formation secondary to ergosterol binding***
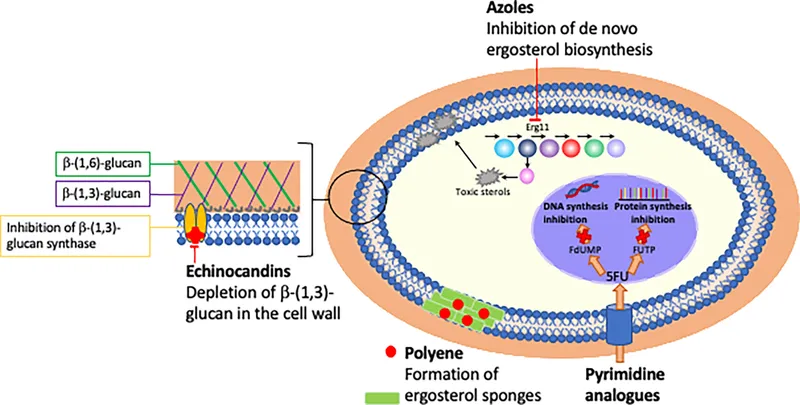
- This describes the mechanism of action of **amphotericin B**, the antifungal agent used for cryptococcal meningitis.
- Amphotericin B binds to **ergosterol** in the fungal cell membrane, leading to the formation of pores, disruption of membrane integrity, and ultimately cell death.
- The side effects described—**nephrotoxicity with renal failure, hypokalemia, and hypomagnesemia**—are classic adverse effects of amphotericin B due to its effect on renal tubular cells and electrolyte wasting.
*Inhibition of squalene epoxidase*
- This is the mechanism of action for **terbinafine**, an antifungal primarily used for dermatophyte infections (e.g., onychomycosis), not systemic infections like cryptococcal meningitis.
- Terbinafine inhibits ergosterol synthesis at an earlier step but does not cause the severe nephrotoxicity and electrolyte disturbances described.
*Binding of the 50S subunit*
- This mechanism of action is characteristic of **macrolide antibiotics** like azithromycin or clarithromycin, which are antibacterial agents, not antifungals.
- These drugs inhibit bacterial protein synthesis and are ineffective against fungal infections.
*Disruption of microtubule formation*
- This is the mechanism of action for **griseofulvin**, an antifungal drug used for dermatophyte infections of the skin, hair, and nails.
- Griseofulvin interferes with fungal cell division and is not used for life-threatening systemic infections like cryptococcal meningitis.
*Inhibition of 1,3-beta-glucan synthase*
- This mechanism is associated with **echinocandins** (e.g., caspofungin, micafungin), which inhibit fungal cell wall synthesis.
- While echinocandins are used for some systemic fungal infections (particularly Candida and Aspergillus), they do not typically cause the severe renal failure and electrolyte disturbances characteristic of amphotericin B.
Cryptococcus neoformans/gattii US Medical PG Question 2: A 44-year-old man comes to the physician because of a 3-week history of productive cough, fever, and lethargy. He also has several skin lesions over his body. His symptoms began 3 weeks after he returned from a camping trip in Kentucky. Three years ago, he underwent kidney transplantation for polycystic kidney disease. Current medications include sirolimus and prednisone. His temperature is 38°C (100.4°F). Diffuse crackles are heard over the lung fields. There are 4 white, verrucous skin patches over his chest and upper limbs. A photomicrograph of a skin biopsy specimen from one of the lesions is shown. Which of the following is the most likely diagnosis?
- A. Coccidioidomycosis
- B. Mucormycosis
- C. Blastomycosis (Correct Answer)
- D. Cryptococcosis
- E. Histoplasmosis
Cryptococcus neoformans/gattii Explanation: ***Blastomycosis***
- The patient's history of **camping in Kentucky**, along with the presence of **pulmonary symptoms** (productive cough, fever, crackles) and **verrucous skin lesions**, are classic for blastomycosis.
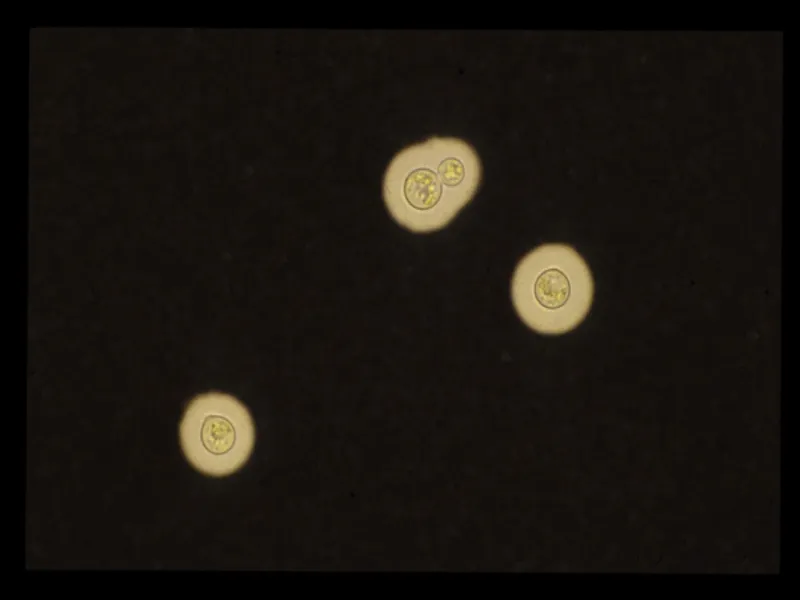
- The photomicrograph showing **broad-based budding yeast** is pathognomonic for *Blastomyces dermatitidis*.
*Coccidioidomycosis*
- This is typical in the **Southwestern United States and parts of Mexico**, not Kentucky.
- Microscopic examination would reveal **spherules containing endospores**, which are not seen in the provided image.
*Mucormycosis*
- This infection is characterized by **irregular, broad, non-septate hyphae** with **wide-angle branching**, often invading blood vessels, leading to tissue necrosis.
- It primarily affects immunocompromised patients but typically presents as **rhinocerebral** or **pulmonary infection**, less commonly with verrucous skin lesions of this type.
*Cryptococcosis*
- Primarily affects the **lungs and central nervous system**, especially in immunocompromised individuals.
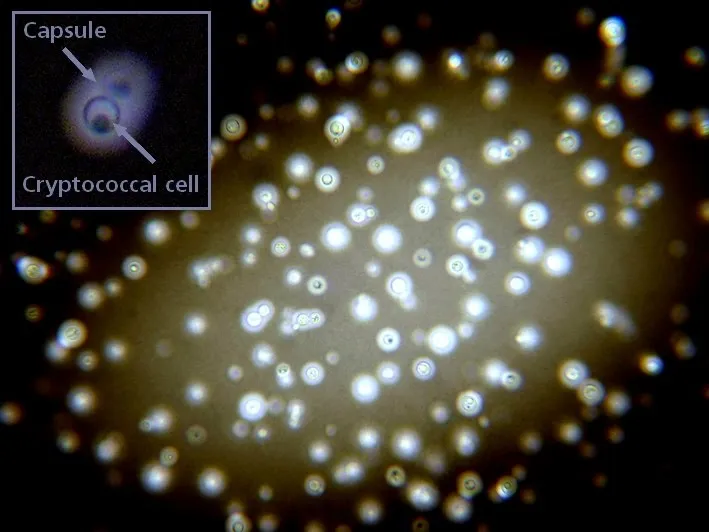
- Microscopy typically shows **encapsulated yeast** cells, which would be visible with India ink stain, and are not represented by the broad-based budding in the image.
*Histoplasmosis*
- Prevalent in the **Ohio and Mississippi River Valleys**, which includes Kentucky, and is often associated with **bird or bat droppings**.
- On microscopy, it presents as **small intracellular yeast** within macrophages, which is morphologically distinct from the large, broad-based budding yeast shown.
Cryptococcus neoformans/gattii US Medical PG Question 3: A 25-year-old man with no significant past medical history is brought in by ambulance after a witnessed seizure at home. On physical exam, temperature is 102.3 deg F (39.1 deg C), blood pressure is 90/62 mmHg, pulse is 118/min, and respirations are 25/min. He is unable to touch his chin to his chest and spontaneously flexes his hips with passive neck flexion. Appropriate empiric treatment is begun. CT head is unremarkable, and a lumbar puncture sample is obtained. Gram stain of the cerebrospinal fluid (CSF) reveals gram-positive diplococci. Which of the following would you expect to see on CSF studies?
- A. Elevated opening pressure, elevated protein, normal glucose
- B. Normal opening pressure, normal protein, normal glucose
- C. Elevated opening pressure, elevated protein, elevated glucose
- D. Normal opening pressure, elevated protein, normal glucose
- E. Elevated opening pressure, elevated protein, low glucose (Correct Answer)
Cryptococcus neoformans/gattii Explanation: ***Elevated opening pressure, elevated protein, low glucose***
- **Bacterial meningitis** typically presents with an **elevated opening pressure** due to inflammation and increased intracranial pressure.
- The inflammatory response leads to increased vascular permeability, causing **elevated protein** in the CSF and **low glucose** due to bacterial consumption.
*Elevated opening pressure, elevated protein, normal glucose*
- While **elevated opening pressure** and **elevated protein** can be seen in inflammatory conditions, **normal CSF glucose** is more characteristic of viral meningitis or non-infectious inflammatory conditions, not bacterial.
- In bacterial meningitis, bacteria metabolize glucose, leading to a **decreased CSF glucose level**.
*Normal opening pressure, normal protein, normal glucose*
- This profile is typical for a **normal CSF study** or certain chronic neurological conditions, not acute bacterial meningitis.
- The patient's severe symptoms, including fever, seizure, and meningismus, contradict a normal CSF profile.
*Elevated opening pressure, elevated protein, elevated glucose*
- While **elevated opening pressure** and **elevated protein** can occur, **elevated CSF glucose** is inconsistent with any common form of meningitis.
- An elevated CSF glucose is rare and would suggest systemic hyperglycemia without impaired glucose transport into the CSF.
*Normal opening pressure, elevated protein, normal glucose*
- A **normal opening pressure** would be unusual in a patient with bacterial meningitis, given the inflammation and potential for increased intracranial pressure.
- While **elevated protein** and **normal glucose** can occur in certain conditions (e.g., Guillain-Barré syndrome), it does not fit the clinical picture of acute bacterial meningitis with fever and meningismus.
Cryptococcus neoformans/gattii US Medical PG Question 4: A previously healthy 17-year-old boy is brought to the emergency department because of fever, nausea, and myalgia for the past day. His temperature is 39.5°C (103.1°F), pulse is 112/min, and blood pressure is 77/55 mm Hg. Physical examination shows scattered petechiae over the anterior chest and abdomen. Blood culture grows an organism on Thayer-Martin agar. Which of the following virulence factors of the causal organism is most likely responsible for the high mortality rate associated with it?
- A. Immunoglobulin A protease
- B. Lipooligosaccharide (Correct Answer)
- C. Toxic shock syndrome toxin-1
- D. Lipoteichoic acid
- E. Erythrogenic exotoxin A
Cryptococcus neoformans/gattii Explanation: ***Lipooligosaccharide***
- The patient's presentation with **fever**, **hypotension**, and **petechiae**, along with a positive blood culture on Thayer-Martin agar, points to **meningococcemia** caused by *Neisseria meningitidis*.
- **Lipooligosaccharide (LOS)** acts as an **endotoxin**, triggering an excessive inflammatory response that leads to widespread vascular damage, **capillary leakage**, and **septic shock**, accounting for the high mortality.
*Immunoglobulin A protease*
- While *N. meningitidis* produces **IgA protease** to cleave secretory IgA and evade host defenses on mucosal surfaces, this factor is primarily involved in colonization and initial invasion rather than the systemic severity and mortality of septic shock.
- Its role is to help the bacteria **adhere and penetrate** host mucous membranes, but it does not directly cause the shock and petechiae seen in this severe presentation.
*Toxic shock syndrome toxin-1*
- **Toxic shock syndrome toxin-1 (TSST-1)** is a **superantigen** produced by *Staphylococcus aureus* that causes **toxic shock syndrome**, which can present with fever, rash, and hypotension.
- However, the organism grown on **Thayer-Martin agar** is characteristic of *Neisseria meningitidis*, not *Staphylococcus aureus*.
*Lipoteichoic acid*
- **Lipoteichoic acid** is a major component of the cell wall of **Gram-positive bacteria**, acting as a potent proinflammatory molecule and contributing to septic shock in those infections.
- *Neisseria meningitidis* is a **Gram-negative bacterium**, and therefore does not possess lipoteichoic acid.
*Erythrogenic exotoxin A*
- **Erythrogenic exotoxin A** is primarily produced by ***Streptococcus pyogenes*** and is responsible for the characteristic rash of **scarlet fever**.
- While *S. pyogenes* can cause invasive infections, the clinical picture and the specific growth on **Thayer-Martin agar** are not consistent with streptococcal infection.
Cryptococcus neoformans/gattii US Medical PG Question 5: A 26-year-old female with AIDS (CD4 count: 47) presents to the emergency department in severe pain. She states that over the past week she has been fatigued and has had a progressively worse headache and fever. These symptoms have failed to remit leading her to seek care in the ED. A lumbar puncture is performed which demonstrates an opening pressure of 285 mm H2O, increased lymphocytes, elevated protein, and decreased glucose. The emergency physician subsequently initiates treatment with IV amphotericin B and PO flucytosine. What additional treatment in the acute setting may be warranted in this patient?
- A. Serial lumbar punctures (Correct Answer)
- B. Fluconazole
- C. Mannitol
- D. Chloramphenicol
- E. Acetazolamide
Cryptococcus neoformans/gattii Explanation: **Serial lumbar punctures**
- The elevated opening pressure (285 mm H2O) indicates **increased intracranial pressure (ICP)**, which is common in cryptococcal meningitis and can be life-threatening.
- Serial lumbar punctures can help to **reduce ICP** and relieve symptoms, improving outcomes in patients with cryptococcal meningitis.
*Fluconazole*
- Fluconazole is used for **maintenance therapy** to prevent relapse after the acute phase of cryptococcal meningitis has been controlled.
- It is generally **not recommended for initial acute treatment** in severe cases due to its fungistatic nature, making it less effective than the combination of amphotericin B and flucytosine.
*Mannitol*
- Mannitol is an **osmotic diuretic** sometimes used to acutely *reduce* ICP in cases of cerebral edema.
- While effective in some situations, it is **not the primary treatment for increased ICP** in cryptococcal meningitis, where repeated LPs are preferred to remove infected CSF and directly reduce pressure.
*Chloramphenicol*
- Chloramphenicol is an **antibiotic** primarily used to treat bacterial infections, not fungal infections.
- It has **no role in the treatment of fungal meningitis** caused by *Cryptococcus neoformans*.
*Acetazolamide*
- Acetazolamide is a **carbonic anhydrase inhibitor** that can reduce CSF production, thereby *reducing* ICP.
- While it can be used in some cases of elevated ICP, routine use in cryptococcal meningitis is **not standard practice**, and serial LPs are generally the preferred method for managing dangerously high ICP in this context due to their immediate efficacy.
Cryptococcus neoformans/gattii US Medical PG Question 6: A 34-year-old woman presents with confusion, drowsiness, and headache. The patient’s husband says her symptoms began 2 days ago and have progressively worsened with an acute deterioration of her mental status 2 hours ago. The patient describes the headaches as severe, localized to the frontal and periorbital regions, and worse in the morning. Review of symptoms is significant for a mild, low-grade fever, fatigue, and nausea for the past week. Past medical history is significant for HIV infection for which she is not currently receiving therapy. Her CD4+ T cell count last month was 250/mm3. The blood pressure is 140/85 mm Hg, the pulse rate is 90/min, and the temperature is 37.7°C (100.0°F). On physical examination, the patient is conscious but drowsy. Papilledema is present. No pain is elicited with extension of the leg at the knee joint. The remainder of the physical examination is negative. Laboratory findings, including panculture, are ordered. A noncontrast CT scan of the head is negative and is followed by a lumbar puncture. CSF analysis is significant for:
Opening pressure 250 mm H2O (70-180 mm H2O)
Glucose 30 mg/dL (40-70 mg/dL)
Protein 100 mg/dL (<40 mg/dL)
Cell count 20/mm3 (0-5/mm3)
Which of the following additional findings would most likely be found in this patient?
- A. Gram-positive diplococci are present on microscopy
- B. CSF shows a positive acid-fast bacillus stain
- C. Multiple ring-enhancing lesions are seen on a CT scan
- D. CSF shows gram negative diplococci
- E. CSF India ink stain shows encapsulated yeast cells (Correct Answer)
Cryptococcus neoformans/gattii Explanation: ***CSF India ink stain shows encapsulated yeast cells***
- The patient's presentation with **subacute meningitis symptoms** (headache, confusion, low-grade fever) in the setting of **untreated HIV infection** with a low CD4+ count (250/mm3) strongly suggests an opportunistic infection.
- The CSF findings of **elevated opening pressure**, **low glucose**, **high protein**, and **moderate pleocytosis** are classic for **cryptococcal meningitis**, for which the India ink stain is diagnostic for encapsulated yeast cells.
*Gram-positive diplococci are present on microscopy*
- This finding suggests **bacterial meningitis**, specifically caused by organisms like *Streptococcus pneumoniae*.
- While bacterial meningitis presents acutely with severe symptoms, the **subacute course** and moderate pleocytosis are less typical, and the patient's immune status points towards an opportunistic infection.
*CSF shows a positive acid-fast bacillus stain*
- A positive **acid-fast bacillus (AFB) stain** in CSF would indicate **tuberculous meningitis**.
- While tuberculous meningitis can present subacutely with similar CSF findings in HIV patients, it typically involves a more significant lymphocytic pleocytosis and a more pronounced chronic course than suggested by the acute worsening.
*Multiple ring-enhancing lesions are seen on a CT scan*
- **Multiple ring-enhancing lesions** on CT or MRI are characteristic of **Toxoplasma encephalopathy** or **CNS lymphoma** in HIV-positive patients.
- While these are common HIV-related CNS complications, the patient's primary presentation points to **meningitis** (inflammation of meninges with CSF abnormalities) rather than focal brain lesions without meningeal involvement.
*CSF shows gram negative diplococci*
- **Gram-negative diplococci** in CSF suggest **meningococcal meningitis** (*Neisseria meningitidis*).
- This typically presents as an **acute, severe bacterial meningitis** with rapid deterioration, usually in immunocompetent individuals or specific outbreaks, which doesn't align with the subacute onset and specific CSF profile for cryptococcus.
Cryptococcus neoformans/gattii US Medical PG Question 7: A 48-year-old man with HIV comes to the physician because of skin lesions over his face and neck for 2 weeks. They are not itchy or painful. He does not have fever or a sore throat. He was treated for candidal esophagitis 3 months ago. He is sexually active with his wife, who knows of his condition, and uses condoms consistently. He is currently receiving triple antiretroviral therapy with lamivudine, abacavir, and efavirenz. He is 175 cm (5 ft 9 in) tall and weighs 58 kg (128 lb); BMI is 18.8 kg/m2. Examination shows multiple skin colored papules over his face and neck with a dimpled center. Cervical lymphadenopathy is present. The remainder of the examination is unremarkable. His hemoglobin concentration is 12.1 g/dL, leukocyte count is 4,900/mm3, and platelet count is 143,000/mm3; serum studies and urinalysis show no abnormalities. CD4+ T-lymphocyte count is 312/mm3 (normal ≥ 500). Which of the following is the most likely cause of this patient's findings?
- A. Poxvirus (Correct Answer)
- B. A herpesvirus
- C. Papillomavirus
- D. Coccidioides
- E. Bartonella
Cryptococcus neoformans/gattii Explanation: ***Poxvirus***
- The description of **skin-colored papules with a dimpled (umbilicated) center** is highly characteristic of **molluscum contagiosum**, which is caused by a poxvirus. This condition is common in immunocompromised individuals, such as those with HIV.
- The patient's **HIV-positive status** and **CD4+ count of 312/mm³** indicate immunocompromise, making him susceptible to severe or widespread molluscum contagiosum, often seen on the face and neck.
*A herpesvirus*
- Herpes simplex virus typically causes **painful, clustered vesicles** on an erythematous base, often with recurrent outbreaks; this presentation does not match the described painless, umbilicated papules.
- Varicella-zoster virus (another herpesvirus) causes chickenpox or shingles, presenting as **vesicles and crusts in a dermatomal pattern** (shingles) or diffuse rash (chickenpox), which is inconsistent with this patient's lesions.
*Papillomavirus*
- Human papillomavirus (HPV) causes **warts**, which are typically rough, hyperkeratotic papules or nodules, lacking the characteristic central umbilication seen in this patient.
- While common in immunocompromised individuals, HPV lesions usually present differently and are not described as skin-colored with a dimpled center.
*Coccidioides*
- **Coccidioidomycosis** is a fungal infection that can cause various skin manifestations, including **erythema nodosum**, **erythema multiforme**, or subcutaneous nodules, but not the distinct umbilicated papules characteristic of molluscum contagiosum.
- Systemic symptoms like fever, cough, and fatigue are common in disseminated coccidioidomycosis, and while skin lesions can occur, they do not typically present as solitary or multiple umbilicated papules.
*Bartonella*
- *Bartonella* infections, particularly *Bartonella henselae* (cat scratch disease) or *Bartonella quintana* (bacillary angiomatosis), typically present as **reddish-purple vascular lesions** (angiomatous papules or nodules) or localized lymphadenopathy.
- The lesions described are skin-colored and umbilicated, not vascular, making *Bartonella* an unlikely cause.
Cryptococcus neoformans/gattii US Medical PG Question 8: A 47-year-old woman comes to the physician because of a 3-day history of fever, fatigue, loss of appetite, cough, and chest pain. Physical examination shows diffuse inspiratory crackles over the left lung field. An x-ray of the chest shows hilar lymphadenopathy and well-defined nodules with central calcifications. Urine studies show the presence of a polysaccharide antigen. A biopsy specimen of the lung shows cells with basophilic, crescent-shaped nuclei and pericellular halos located within macrophages. This patient's history is most likely to show which of the following?
- A. Visit to Arizona desert
- B. Recent trip to Brazil
- C. Previous mycobacterial infection
- D. Exposure to bat droppings (Correct Answer)
- E. Treatment with inhaled glucocorticoids
Cryptococcus neoformans/gattii Explanation: ***Exposure to bat droppings***
- The clinical presentation, including fever, cough, chest pain, **hilar lymphadenopathy**, **nodules with central calcifications**, and **intracellular encapsulated yeasts** in macrophages, is classic for **histoplasmosis**.
- **Histoplasma capsulatum** is endemic to the Ohio and Mississippi River valleys and is transmitted through inhalation of spores from soil contaminated with **bat or bird droppings**.
*Visit to Arizona desert*
- Exposure in the **Arizona desert** is associated with **coccidioidomycosis** (Valley Fever), which presents with similar pulmonary symptoms but is caused by Coccidioides immitis/posadasii, characterized by **spherules** containing endospores.
- While it can cause hilar lymphadenopathy and nodules, the characteristic intracellular budding yeasts within macrophages and the polysaccharide antigen in urine point away from coccidioidomycosis.
*Recent trip to Brazil*
- A trip to **Brazil** might suggest diseases like **Paracoccidioidomycosis**, which presents with chronic mucocutaneous or disseminated lesions, or various tropical infections, but is not typically characterized by the specific pulmonary and microscopic findings described here.
- The histopathological findings of **intracellular yeasts with pericellular halos** (consistent with Histoplasma) would not be the primary finding for paracoccidioidomycosis, which generally shows characteristic **"pilot wheel"** or multiple budding yeasts.
*Previous mycobacterial infection*
- A previous **mycobacterial infection** would lead to tuberculosis, characterized by **acid-fast bacilli** and granulomas with **caseating necrosis**, which is different from the described intracellular yeasts and polysaccharide antigen.
- While tuberculosis can cause hilar lymphadenopathy and pulmonary nodules, the given microscopic description of cells with basophilic nuclei and pericellular halos within macrophages does not fit Mycobacterium tuberculosis.
*Treatment with inhaled glucocorticoids*
- Inhaled glucocorticoids are used to treat conditions like asthma or COPD and, while prolonged use can rarely predispose to **opportunistic fungal infections** (e.g., aspergillosis, candidiasis), they are not a cause of this specific clinical presentation or the microbiological findings of histoplasmosis.
- The use of inhaled steroids would not explain the geographic exposure, hilar lymphadenopathy, or the specific appearance of the fungal elements within macrophages described.
Cryptococcus neoformans/gattii US Medical PG Question 9: A 46-year-old woman presents to her primary care physician with complaints of increasing left upper quadrant discomfort. She has a known history of type 1 Gaucher disease. On physical examination, her spleen is palpable 8 cm below the costal margin. Routine laboratory work reveals severe pancytopenia. After consultation with the patient on the risks of her condition, the patient decides to undergo a splenectomy. Which of the following is more likely to occur as a consequence of splenectomy in this patient?
- A. Thrombocytopenia
- B. Leukopenia
- C. Pneumococcal septicemia (Correct Answer)
- D. Staphylococcal septicemia
- E. Anemia
Cryptococcus neoformans/gattii Explanation: ***Pneumococcal septicemia***
- Patients who undergo splenectomy are at significantly increased risk of **overwhelming post-splenectomy infection (OPSI)**, particularly from **encapsulated bacteria** like *Streptococcus pneumoniae*.
- The spleen plays a crucial role in filtering encapsulated bacteria and producing opsonizing antibodies, and its removal compromises this immune function.
*Thrombocytopenia*
- **Thrombocytopenia** is typically a symptom *before* splenectomy in Gaucher disease due to hypersplenism.
- After splenectomy, the platelet count often **increases**, not decreases, due to the removal of the organ that sequesters platelets and destroys them.
*Leukopenia*
- **Leukopenia** (specifically neutropenia) is a pre-existing condition in severe Gaucher disease due to hypersplenism and bone marrow involvement.
- Post-splenectomy, the white blood cell count, particularly neutrophils, generally **increases** as the sequestration and destruction in the spleen are eliminated.
*Staphylococcal septicemia*
- While *Staphylococcus* can cause serious infections, it is **not the primary pathogen** associated with OPSI in asplenic patients.
- Encapsulated bacteria like *Streptococcus pneumoniae* are the most common and dangerous cause of post-splenectomy sepsis.
*Anemia*
- **Anemia** is a common finding in Gaucher disease due to hypersplenism and bone marrow infiltration.
- Splenectomy typically **improves** anemia by removing the site of red blood cell destruction and reducing abnormal cytokine production that inhibits erythropoiesis.
Cryptococcus neoformans/gattii US Medical PG Question 10: A 36-year-old woman with HIV comes to the physician because of a 3-day history of pain and watery discharge in her left eye. She also has blurry vision and noticed that she is more sensitive to light. Her right eye is asymptomatic. She had an episode of shingles 7 years ago. She was diagnosed with HIV 5 years ago. She admits that she takes her medication inconsistently. She wears contact lenses. Current medications include abacavir, lamivudine, efavirenz, and a nutritional supplement. Her temperature is 37°C (98.6°F), pulse is 89/min, and blood pressure is 110/70 mm Hg. Examination shows conjunctival injection of the left eye. Visual acuity is 20/20 in the right eye and 20/80 in the left eye. Extraocular movements are normal. Her CD4+ T-lymphocyte count is 90/mm3. A photograph of the left eye after fluorescein administration is shown. Which of the following is the most likely diagnosis?
- A. Pseudomonas keratitis
- B. Fusarium keratitis
- C. Neurotrophic keratopathy
- D. Herpes simplex keratitis (Correct Answer)
- E. Herpes zoster keratitis
Cryptococcus neoformans/gattii Explanation: ***Herpes simplex keratitis***
- The fluorescein staining shows a **dendritic ulcer**, which is **pathognomonic** for herpes simplex keratitis.
- The patient's **immunosuppressed state** due to HIV with a low CD4+ count (90/mm3) makes her susceptible to opportunistic viral infections like HSV.
*Pseudomonas keratitis*
- Often seen in **contact lens wearers**, but it typically presents with a rapidly progressive, painful, circumferential stromal infiltrate, and often a **hypopyon**, which are not described.
- The classic dendritic pattern on fluorescein staining is not characteristic of bacterial keratitis.
*Fusarium keratitis*
- This is a **fungal infection** often associated with contact lens use, especially after corneal trauma involving vegetable matter.
- It presents with feathery, elevated infiltrates and satellite lesions, which differ from the dendritic pattern seen.
*Neurotrophic keratopathy*
- This condition results from **corneal denervation**, leading to impaired epithelial healing.
- While it can cause persistent epithelial defects, it typically appears as an oval or irregular epithelial defect without the distinct dendritic branching pattern.
*Herpes zoster keratitis*
- While caused by a herpesvirus (VZV), it typically presents with a characteristic **pseudodendrite** (not true dendrite) that stains poorly with fluorescein and is associated with a **rash in the V1 dermatome**.
- The patient's history of shingles 7 years ago is less relevant than the current classic dendritic pattern for HSV.
More Cryptococcus neoformans/gattii US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.