Aspergillus species US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Aspergillus species. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Aspergillus species US Medical PG Question 1: A 69-year-old man with metastatic colon cancer is brought to the emergency department because of shortness of breath, fever, chills, and a productive cough with streaks of blood for the past 5 days. He has a history of emphysema. The patient does not have abdominal pain or headache. He receives chemotherapy with 5-fluorouracil, leucovorin, and oxaliplatin every 6 weeks; his last cycle was 3 weeks ago. His temperature is 38.3°C (101°F), pulse is 112/min, and blood pressure is 100/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 83%. A few scattered inspiratory crackles are heard over the right lung. His mucous membranes are dry. Cardiac examination is normal. Laboratory studies show:
Hemoglobin 9.3 mg/dL
Leukocyte count 700/mm3
Segmented neutrophils 68%
Lymphocytes 25%
Eosinophils 4%
Monocytes 3%
Platelet count 104,000/mm3
Serum
Glucose 75 mg/dL
Urea nitrogen 41 mg/dL
Creatinine 2.1 mg/dL
Galactomannan antigen Positive
Which of the following is the most appropriate initial pharmacotherapy?
- A. Ceftriaxone and azithromycin
- B. Rifampin, isoniazid, pyrazinamide, and ethambutol
- C. Ceftazidime and levofloxacin
- D. Piperacillin-tazobactam
- E. Voriconazole (Correct Answer)
Aspergillus species Explanation: ***Voriconazole***
- The patient has **neutropenic fever** (leukocyte count 700/mm3, recent chemotherapy) with pulmonary symptoms and a positive **galactomannan antigen**, which is highly suggestive of **invasive aspergillosis**.
- **Voriconazole** is the recommended first-line agent for the treatment of **invasive aspergillosis**.
*Ceftriaxone and azithromycin*
- This combination is typically used for **community-acquired pneumonia**, targeting common bacterial pathogens like *Streptococcus pneumoniae* and atypical bacteria.
- It does not cover **fungal infections** like aspergillosis, nor does it provide broad-spectrum gram-negative coverage suitable for neutropenic fever.
*Rifampin, isoniazid, pyrazinamide, and ethambutol*
- This four-drug regimen is the standard treatment for **active tuberculosis**.
- There is no clinical or laboratory evidence (e.g., acid-fast bacilli smear, cultures) to suggest tuberculosis in this patient.
*Ceftazidime and levofloxacin*
- **Ceftazidime** is a third-generation cephalosporin with good gram-negative coverage, including *Pseudomonas*, which might be considered in neutropenic fever. However, it lacks adequate gram-positive coverage.
- **Levofloxacin** is a fluoroquinolone that provides broad-spectrum coverage, but this combination still misses the likely fungal pathogen and is not ideal for initial empiric therapy in severe neutropenic fever.
*Piperacillin-tazobactam*
- **Piperacillin-tazobactam** is a broad-spectrum antibiotic with good coverage against both gram-positive and gram-negative bacteria, including *Pseudomonas aeruginosa*, making it a common choice for **empiric therapy in neutropenic fever**.
- However, it does not cover **fungal infections**, which are strongly indicated by the positive **galactomannan antigen** in this immunocompromised patient.
Aspergillus species US Medical PG Question 2: A 7-year-old boy with a history of cystic fibrosis is brought to the physician for evaluation of recurrent episodes of productive cough, wheezing, and shortness of breath over the past month. Physical examination shows coarse crackles and expiratory wheezing over both lung fields. Serum studies show elevated levels of IgE and eosinophilia. A CT scan of the lungs shows centrally dilated bronchi with thickened walls and peripheral airspace consolidation. Antibiotic therapy is initiated. One week later, the patient continues to show deterioration in lung function. A sputum culture is most likely to grow which of the following?
- A. Monomorphic, septate hyphae that branch at acute angles (Correct Answer)
- B. Monomorphic, broad, nonseptate hyphae that branch at wide angles
- C. Dimorphic, broad-based budding yeast
- D. Dimorphic, cigar-shaped budding yeast
- E. Monomorphic, narrow budding encapsulated yeast
Aspergillus species Explanation: **Monomorphic, septate hyphae that branch at acute angles**
- The patient's presentation with **cystic fibrosis (CF)**, recurrent respiratory symptoms, CT findings of **central bronchiectasis**, elevated **IgE**, and **eosinophilia** strongly points towards **allergic bronchopulmonary aspergillosis (ABPA)**.
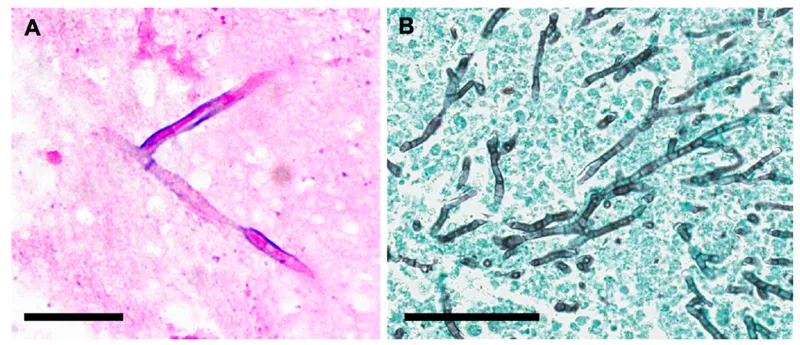
- *Aspergillus fumigatus*, the causative agent of ABPA, is characterized microscopically by **monomorphic, septate hyphae that branch at acute angles**.
*Monomorphic, broad, nonseptate hyphae that branch at wide angles*
- This describes organisms like *Rhizopus* or *Mucor*, which cause **mucormycosis**.
- Mucormycosis typically affects immunocompromised individuals (e.g., diabetics, neutropenic patients) and presents as aggressive rhinocerebral or pulmonary infections, not ABPA.
*Dimorphic, broad-based budding yeast*
- This morphology is characteristic of *Blastomyces dermatitidis*, which causes **blastomycosis**.
- Blastomycosis is an endemic fungal infection often presenting with pulmonary symptoms, but it does not cause central bronchiectasis, elevated IgE, or eosinophilia in the context of CF.
*Dimorphic, cigar-shaped budding yeast*
- This morphology describes *Sporothrix schenckii*, which causes **sporotrichosis**.
- Sporotrichosis typically presents as a chronic ulcerative skin disease (rose gardener's disease) or, less commonly, pulmonary disease, but is not associated with ABPA.
*Monomorphic, narrow budding encapsulated yeast*
- This morphology is characteristic of *Cryptococcus neoformans*, which causes **cryptococcosis**.
- Cryptococcosis commonly affects immunocompromised individuals, causing meningoencephalitis or pulmonary disease, but its presentation is distinct from ABPA, lacking the allergic and bronchiectatic features described.
Aspergillus species US Medical PG Question 3: A 50-year-old HIV-positive male presents to the ER with a two-day history of fever and hemoptysis. Chest radiograph shows a fibrocavitary lesion in the right middle lobe. Biopsy of the afflicted area demonstrates septate hyphae that branch at acute angles. Which of the following is the most likely causal organism?
- A. Mycobacterium tuberculosis
- B. Pneumocystis jirovecii
- C. Aspergillus fumigatus (Correct Answer)
- D. Candida albicans
- E. Mucor species
Aspergillus species Explanation: ***Aspergillus fumigatus***
- The combination of **fever**, **hemoptysis**, a **fibrocavitary lesion** in an **HIV-positive** patient, and the presence of **septate hyphae branching at acute angles** on biopsy are classic findings for invasive **aspergillosis**.
- **Aspergillus** specifically targets individuals with compromised immune systems, and the pathological description of the hyphae is highly characteristic of this fungus.
*Mycobacterium tuberculosis*
- While **Mycobacterium tuberculosis** can cause **fever**, **hemoptysis**, and **cavitary lesions** in HIV-positive patients, the microscopic description of **septate hyphae branching at acute angles** is not consistent with bacterial infection.
- Tuberculosis is characterized by **acid-fast bacilli** and granulomatous inflammation, not fungal hyphae.
*Mucor species*
- **Mucor** (along with Rhizopus) causes **mucormycosis**, an invasive fungal infection that can affect immunocompromised patients and present with pulmonary involvement and cavitary lesions.
- However, mucormycosis is characterized by **non-septate (aseptate) hyphae branching at right (90-degree) angles**, not septate hyphae at acute angles, making it distinguishable from Aspergillus.
*Pneumocystis jirovecii*
- **Pneumocystis jirovecii** is a common cause of pneumonia in HIV-positive patients, typically presenting as **diffuse interstitial infiltrates** rather than cavitary lesions.
- Microscopic examination would reveal **cysts** and **trophozoites**, not septate hyphae, making it inconsistent with the biopsy findings.
*Candida albicans*
- While **Candida albicans** can cause infections in immunocompromised individuals, it typically presents as **oral thrush**, esophagitis, or disseminated candidiasis.
- Pulmonary involvement is less common and usually manifests as **pneumonitis** rather than cavitary lesions, and its hyphae are typically **pseudohyphae** or budding yeasts, not septate hyphae branching at acute angles.
Aspergillus species US Medical PG Question 4: A 47-year-old alcoholic man presents to the office for a 72-hour history of intense right hemithorax pain. He also complains of fever, chills, and sweating that started 10 days ago, as well as persistent coughing with abundant malodorous sputum. Chest radiography shows a round consolidation with air-fluid levels in the middle third of the right hemithorax. Sputum samples for a direct exam, culture, and acid-fast bacilli (AFB) are sent. What is the correct diagnosis?
- A. Bronchopulmonary sequestration
- B. Bronchiectasis
- C. Tuberculosis
- D. Lung cancer
- E. Lung abscess (Correct Answer)
Aspergillus species Explanation: ***Lung abscess***
- The combination of **fever, chills, sweating, persistent coughing with malodorous sputum**, and a **round consolidation with air-fluid levels** on chest radiography in an alcoholic patient is highly indicative of a lung abscess.
- Alcoholism is a significant risk factor due to aspiration, leading to polymicrobial infections and subsequent tissue necrosis and cavitation.
*Bronchopulmonary sequestration*
- This is a rare congenital malformation where a portion of lung tissue is not connected to the tracheobronchial tree and receives its blood supply from the systemic circulation.
- It typically presents as a **mass lesion** on imaging, often without acute signs of infection like fever and malodorous sputum, unless it becomes secondarily infected.
*Bronchiectasis*
- Characterized by **irreversible dilation of the bronchi** resulting from chronic inflammation and infection, leading to chronic cough and sputum production.
- While it can cause chronic cough and sputum, the acute presentation with a distinct **round consolidation with air-fluid levels** points more specifically to an abscess.
*Tuberculosis*
- While tuberculosis can cause **fever, cough, and cavitary lesions** which might appear as air-fluid levels, the **malodorous sputum** is less typical, and the acute onset (72-hour intense pain after 10 days of symptoms) is more consistent with a pyogenic bacterial infection.
- Furthermore, a round consolidation with air-fluid levels without other classic features of TB (e.g., upper lobe predominance, Ghon complex) makes it less likely given the other findings.
*Lung cancer*
- Lung cancer can present as a **mass or consolidation** on imaging, and patients may experience cough, weight loss, and fatigue.
- However, the rapid onset of **fever, chills, malodorous sputum, and air-fluid levels** strongly suggests an infectious process with cavitation rather than an uncomplicated malignancy.
Aspergillus species US Medical PG Question 5: A 31-year-old female undergoing treatment for leukemia is found to have a frontal lobe abscess accompanied by paranasal swelling. She additionally complains of headache, facial pain, and nasal discharge. Biopsy of the infected tissue would most likely reveal which of the following?
- A. Yeast with pseudohyphae
- B. Septate hyphae
- C. Irregular non-septate hyphae (Correct Answer)
- D. Spherules containing endospores
- E. Budding yeast with a narrow base
Aspergillus species Explanation: ***Irregular non-septate hyphae***
- The clinical presentation of a **leukemic patient** with a **frontal lobe abscess** and **paranasal swelling**, along with headache, facial pain, and nasal discharge, strongly suggests **mucormycosis**.
- Mucormycosis is characterized by **broad, ribbon-like, irregular non-septate hyphae** with **right-angle branching** on tissue biopsy, making this the most likely finding.
*Yeast with pseudohyphae*
- This morphology is characteristic of **Candida species**, which can cause opportunistic infections but typically manifest as candidemia, esophagitis, or vulvovaginitis in immunocompromised patients, not usually a frontal lobe abscess with paranasal involvement.
- While Candida can cause severe systemic infections, the specific combination of a frontal lobe abscess and paranasal swelling points away from Candida as the primary cause in this context.
*Septate hyphae*
- **Septate hyphae** are typical of **Aspergillus species**, which can cause invasive aspergillosis, including sinopulmonary infections and CNS involvement in immunocompromised hosts.
- However, Aspergillus hyphae are typically **narrow (3-6 µm)** with **acute-angle (45-degree) branching**, differentiating them from the broad, irregular hyphae seen in mucormycosis.
*Spherules containing endospores*
- This morphology is characteristic of **Coccidioides immitis**, the causative agent of coccidioidomycosis.
- Coccidioidomycosis is geographically restricted to endemic areas (e.g., southwestern US) and typically presents with pulmonary symptoms, disseminated disease, or meningitis, which does not fit the described paranasal and frontal lobe presentation.
*Budding yeast with a narrow base*
- This morphology is characteristic of **Cryptococcus neoformans**, an encapsulated yeast that commonly causes **meningitis** and **pneumonia** in immunocompromised individuals.
- While Cryptococcus can cause CNS infections, the presence of paranasal swelling and the specific description of a frontal lobe abscess make mucormycosis a more fitting diagnosis.
Aspergillus species US Medical PG Question 6: A 28-year-old woman with a past history of type 1 diabetes presents to your office with a 2-week history of vaginal itching and soreness accompanied by a white, clumpy vaginal discharge which she says resembles cheese curds. Her last HbA1c from a month ago was 7.8%, and her last cervical cytology from 10 months ago was reported as normal. She has a blood pressure of 118/76 mmHg, respiratory rate of 14/min, and heart rate of 74/min. Pelvic examination reveals multiple small erythematous lesions in the inguinal and perineal area, vulvar erythema, and excoriations. Inspection demonstrates a normal cervix and a white, adherent, thick, non-malodorous vaginal discharge. Which of the following is most likely to be present in a saline wet mount from the vaginal discharge of this patient?
- A. Clue cells on saline smear
- B. Gram-negative diplococci
- C. Hyphae (Correct Answer)
- D. Motile flagellates
- E. Multinucleated giant cells
Aspergillus species Explanation: ***Hyphae***
- The patient's symptoms of **vaginal itching**, soreness, and a **white, clumpy discharge resembling cheese curds** are classic for **vulvovaginal candidiasis** (yeast infection).
- A **saline wet mount** in such cases typically reveals **hyphae** and **budding yeast forms** of *Candida albicans*.
*Clue cells on saline smear*
- **Clue cells** are characteristic of **bacterial vaginosis**, which is typically associated with a **thin, grayish discharge** and a **fishy odor** (amine odor), neither of which are described here.
- The discharge in this patient is described as **thick and non-malodorous**, which is inconsistent with bacterial vaginosis.
*Gram-negative diplococci*
- **Gram-negative diplococci** are the hallmark of **gonorrhea**, caused by *Neisseria gonorrhoeae*.
- Gonorrhea often presents with **purulent discharge** and cervical inflammation, or it can be asymptomatic; it does not typically cause the **clumpy discharge** and intense itching seen in this patient.
*Motile flagellates*
- **Motile flagellates** are characteristic of **trichomoniasis**, caused by *Trichomonas vaginalis*.
- This infection usually presents with a **frothy, yellow-green discharge**, a **fishy odor**, and cervical petechiae (strawberry cervix), which are not a feature of this patient's presentation.
*Multinucleated giant cells*
- **Multinucleated giant cells** are indicative of **herpes simplex virus (HSV) infection**, particularly when found on a **Tzanck smear** of a lesion.
- While the patient has erythematous lesions, the primary complaint of **vaginal discharge** and itching points away from herpes as the main cause of the discharge.
Aspergillus species US Medical PG Question 7: A 58-year-old man presents with a high-grade fever, throbbing left-sided headache, vision loss, and left orbital pain. He says that his symptoms started acutely 2 days ago with painful left-sided mid-facial swelling and a rash, which progressively worsened. Today, he woke up with complete vision loss in his left eye. His past medical history is significant for type 2 diabetes mellitus, diagnosed 5 years ago. He was started on an oral hypoglycemic agent which he discontinued after a year. His temperature is 38.9°C (102.0°F), blood pressure is 120/80 mm Hg, pulse is 120/min, and respiratory rate is 20/min. On examination, there is purulent discharge from the left eye and swelling of the left half of his face including the orbit. Oral examination reveals extensive necrosis of the palate with a black necrotic eschar and purulent discharge. Ophthalmic examination is significant for left-sided ptosis, proptosis, and an absence of the pupillary light reflex. Laboratory findings are significant for a blood glucose level of 388 mg/dL and a white blood cell count of 19,000 cells/mm³. Urinary ketone bodies are positive. Fungal elements are found on a KOH mount of the discharge. Which of the following statements best describes the organism responsible for this patient’s condition?
- A. It appears as a narrow-based budding yeast with a thick capsule
- B. Histopathological examination shows non-septate branching hyphae (Correct Answer)
- C. It produces conidiospores
- D. It has budding and filamentous forms
- E. Histopathological examination shows acute angle branching hyphae
Aspergillus species Explanation: ***Histopathological examination shows non-septate branching hyphae***
- The patient's presentation with **diabetic ketoacidosis**, orbital pain, vision loss, facial swelling, necrotic palatal eschar, and high fever strongly suggests **mucormycosis**, a severe fungal infection.
- Mucormycosis is caused by fungi belonging to **Mucorales order** (e.g., *Rhizopus*, *Mucor*, *Lichtheimia*), which are characterized by **broad, ribbon-like, non-septate hyphae with irregular, wide-angle branching**.
*It appears as a narrow-based budding yeast with a thick capsule*
- This description is characteristic of **Cryptococcus neoformans**, which causes cryptococcosis, often presenting with meningoencephalitis and lung involvement.
- The clinical picture and *KOH mount* findings in this patient are inconsistent with cryptococcosis.
*It produces conidiospores*
- **Conidiospores are asexual spores** produced by many fungi, including *Aspergillus* and *Penicillium*, but this is a general characteristic and not specific enough to definitively identify the pathogen responsible for mucormycosis.
- The *histopathological features* (non-septate hyphae) are the key identifier in mucormycosis.
*It has budding and filamentous forms*
- This description generally refers to **dimorphic fungi** (e.g., *Histoplasma*, *Blastomyces*, *Coccidioides*), which exhibit yeast forms in tissue and mold forms in culture.
- Mucorales are typically **molds** in both environments and are not considered dimorphic, nor do they commonly present with budding forms.
*Histopathological examination shows acute angle branching hyphae*
- This morphological description is characteristic of **Aspergillus species**, which cause aspergillosis, another opportunistic fungal infection.
- *Aspergillus* hyphae are typically **septate** and branch at acute angles (around 45 degrees), unlike the broad, non-septate, wide-angle branching hyphae of Mucorales.
Aspergillus species US Medical PG Question 8: A 16-year-old girl presents to her physician with itching, soreness, and irritation in the vulvar region. She reports that these episodes have occurred 6–7 times a year since the age of 5. She used to treat these symptoms with topical ketoconazole cream, but this time it failed to help. She also has had several episodes of oral candidiasis in the past. She is not sexually active and does not take any medication. Her vital signs are as follows: the blood pressure is 115/80 mm Hg, the heart rate is 78/min, the respiratory rate is 15/min, and the temperature is 35.5°C (97.7°F). Examination shows vulvovaginal erythema with cottage cheese-like plaques and an intact hymen. Wet mount microscopy is positive for yeast. Along with a swab culture, the physician orders a dihydrorhodamine test and myeloperoxidase staining for a suspected primary immunodeficiency. The dihydrorhodamine test is positive, and the myeloperoxidase staining reveals diminished staining. Which of the following best describes this patient's condition?
- A. The patient is likely to have another immune impairment besides the one for which she was tested. (Correct Answer)
- B. The patient should receive prophylactic courses of wide spectrum antibiotics to prevent infections.
- C. The patient’s phagocytes are unable to generate an oxidative burst to kill intracellular bacteria.
- D. The patient is susceptible to all mycotic infections.
- E. The patient’s phagocytes can only perform extracellular killing.
Aspergillus species Explanation: ***The patient is likely to have another immune impairment besides the one for which she was tested.***
- The **positive dihydrorhodamine (DHR) test** indicates that the patient's phagocytes are capable of producing an **oxidative burst**, effectively ruling out **Chronic Granulomatous Disease (CGD)**.
- The **diminished myeloperoxidase (MPO) staining** suggests **Myeloperoxidase Deficiency**, which is usually asymptomatic in most patients but can predispose to recurrent Candida infections, especially in diabetics.
- However, **MPO deficiency alone does not explain** the severity and frequency of this patient's recurrent **oral and vulvovaginal candidiasis** starting from age 5, suggesting an additional immune defect.
- The pattern of chronic mucocutaneous candidiasis suggests a defect in **T-cell immunity** or the **CARD9 pathway**, which is crucial for antifungal responses against *Candida* species.
- Therefore, the patient likely has a **combined immunodeficiency**: MPO deficiency (detected) plus another defect affecting cell-mediated immunity or antifungal responses (not yet tested for).
*The patient should receive prophylactic courses of wide spectrum antibiotics to prevent infections.*
- The **positive DHR test** indicates normal oxidative burst, meaning the patient is not primarily susceptible to catalase-positive bacterial infections that would require prophylactic antibiotics (unlike in CGD).
- The recurrent infections are **fungal** (Candida), not bacterial, so broad-spectrum antibiotics would not be the appropriate prophylactic treatment.
- Appropriate management would include **antifungal prophylaxis** (e.g., fluconazole) and further investigation for T-cell defects.
*The patient's phagocytes are unable to generate an oxidative burst to kill intracellular bacteria.*
- This statement is **directly contradicted** by the **positive DHR test**, which demonstrates that phagocytes *are* capable of generating an oxidative burst.
- Inability to generate an oxidative burst is the hallmark of **Chronic Granulomatous Disease (CGD)**, where the DHR test would be **negative** (abnormal).
- In CGD, patients present with recurrent catalase-positive bacterial infections (Staphylococcus, Serratia, Nocardia) and invasive fungal infections (Aspergillus), not primarily mucocutaneous candidiasis.
*The patient is susceptible to all mycotic infections.*
- While the patient has **recurrent candidiasis**, there is no evidence of susceptibility to a broad range of other fungal pathogens (e.g., Aspergillus, Cryptococcus, Histoplasma).
- The specific pattern of **chronic mucocutaneous candidiasis** suggests a targeted defect in anti-Candida immunity (T-cell or CARD9 deficiency), rather than global susceptibility to all fungi.
- Susceptibility to all mycotic infections would be seen in severe combined immunodeficiencies (SCID) or advanced HIV/AIDS, which would present with multiple opportunistic infections.
*The patient's phagocytes can only perform extracellular killing.*
- This statement is **incorrect** because phagocytes (neutrophils and macrophages) primarily perform **intracellular killing** after engulfing pathogens through phagocytosis.
- The **positive DHR test** confirms intact oxidative burst, which is essential for **intracellular killing** of phagocytosed organisms.
- MPO deficiency affects the efficiency of intracellular killing (as MPO enhances the microbicidal activity of hydrogen peroxide), but phagocytes still retain other intracellular killing mechanisms (lysozyme, defensins, proteases).
Aspergillus species US Medical PG Question 9: A 27-year-old male who works on an organic farm is diagnosed with infection by N. americanus, a helminthic parasite. Eosinophils require which antibody isotype to destroy these parasites via antibody-dependent cellular cytotoxicity?
- A. IgE (Correct Answer)
- B. IgA
- C. IgG
- D. IgM
- E. IgD
Aspergillus species Explanation: ***IgE***
- **IgE** antibodies are crucial in the immune response against helminthic parasites, including *N. americanus*, by sensitizing **mast cells** and **eosinophils**.
- When **IgE** binds to the surface of parasites, the **Fc receptor** on eosinophils recognizes the Fc portion of IgE, leading to the release of cytotoxic granules that destroy the parasite (antibody-dependent cellular cytotoxicity).
*IgA*
- **IgA** is primarily found in **mucosal secretions** and plays a role in defending against pathogens at mucosal surfaces, but it is not the primary isotype involved in eosinophil-mediated **ADCC** against helminths.
- While IgA can bind to some immune cells, its main function is to **neutralize toxins** and prevent microbial adhesion at mucosal sites.
*IgG*
- **IgG** is the most abundant antibody in serum and is involved in various immune functions, including **opsonization**, **neutralization**, and **complement activation**.
- Although IgG can mediate ADCC by **NK cells** and **macrophages**, it is not the primary isotype for eosinophil-mediated killing of helminths, which is dominated by IgE.
*IgM*
- **IgM** is typically the first antibody produced during a primary immune response and is very effective at **activating the complement system**.
- Its large pentameric structure also limits its diffusion into tissues, and it does not play a direct role in eosinophil-mediated ADCC against helminthic parasites.
*IgD*
- **IgD** primarily functions as a **B cell receptor** on naive B lymphocytes, signaling for their activation and differentiation.
- It is present in very low concentrations in serum and its role in host defense against parasites or in ADCC is negligible.
Aspergillus species US Medical PG Question 10: A 3-month-old girl is brought to the emergency department because of a 2-day history of progressive difficulty breathing and a dry cough. Five weeks ago, she was diagnosed with diffuse hemangiomas involving the intrathoracic cavity and started treatment with prednisolone. She appears uncomfortable and in moderate respiratory distress. Her temperature is 38°C (100.4°F), pulse is 150/min, respirations are 50/min, and blood pressure is 88/50 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 87%. Oral examination shows a white plaque covering the tongue that bleeds when scraped. Chest examination shows subcostal and intercostal retractions. Scattered fine crackles and rhonchi are heard throughout both lung fields. Laboratory studies show a leukocyte count of 21,000/mm3 and an increased serum beta-D-glucan concentration. An x-ray of the chest shows symmetrical, diffuse interstitial infiltrates. Which of the following is most likely to confirm the diagnosis?
- A. Tuberculin skin test
- B. Urine antigen test
- C. CT scan of the chest
- D. Bronchoalveolar lavage (Correct Answer)
- E. DNA test for CFTR mutation
Aspergillus species Explanation: ***Bronchoalveolar lavage***
- The patient, an infant on **prednisolone** (immunosuppression) with **diffuse interstitial infiltrates**, **uncomfortable appearance**, **respiratory distress**, and **oral thrush (white plaque that bleeds when scraped)**, points to **Pneumocystis pneumonia (PCP)**.
- **Bronchoalveolar lavage (BAL)** is the gold standard for diagnosing PCP by identifying **Pneumocystis jirovecii cysts** or **trophozoites** using special stains (e.g., Giemsa, methenamine silver).
*Tuberculin skin test*
- The **tuberculin skin test** is used to diagnose **tuberculosis**, which typically presents with **granulomas** and **cavitary lesions** on chest X-ray, not diffuse interstitial infiltrates.
- While tuberculosis can cause respiratory symptoms, the presence of oral thrush and immunosuppression suggests an opportunistic fungal infection like PCP rather than TB.
*Urine antigen test*
- A **urine antigen test** is commonly used for diagnosing **Legionnaires' disease** or **pneumococcal pneumonia** in adults, and is not applicable for PCP.
- It does not detect *Pneumocystis jirovecii*, which is the suspected pathogen in this immunosuppressed infant.
*CT scan of the chest*
- A **CT scan of the chest** would show **diffuse ground-glass opacities** characteristic of PCP but is a **radiological finding**, not a definitive diagnostic test for the pathogen itself.
- While it can further characterize the pulmonary findings, it cannot identify the causative organism, which is crucial for targeted treatment.
*DNA test for CFTR mutation*
- A **DNA test for CFTR mutation** is used to diagnose **cystic fibrosis**, a genetic disorder affecting mucus production, and is not relevant in this acute presentation of respiratory distress and immunosuppression.
- Cystic fibrosis typically presents with recurrent respiratory infections, pancreatic insufficiency, and failure to thrive, not primarily with opportunistic infections like PCP.
More Aspergillus species US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.