Therapeutic approaches targeting oncogenic viruses US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Therapeutic approaches targeting oncogenic viruses. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Therapeutic approaches targeting oncogenic viruses US Medical PG Question 1: A research team develops a new monoclonal antibody checkpoint inhibitor for advanced melanoma that has shown promise in animal studies as well as high efficacy and low toxicity in early phase human clinical trials. The research team would now like to compare this drug to existing standard of care immunotherapy for advanced melanoma. The research team decides to conduct a non-randomized study where the novel drug will be offered to patients who are deemed to be at risk for toxicity with the current standard of care immunotherapy, while patients without such risk factors will receive the standard treatment. Which of the following best describes the level of evidence that this study can offer?
- A. Level 1
- B. Level 3 (Correct Answer)
- C. Level 5
- D. Level 4
- E. Level 2
Therapeutic approaches targeting oncogenic viruses Explanation: ***Level 3***
- A **non-randomized controlled trial** like the one described, where patient assignment to treatment groups is based on specific characteristics (risk of toxicity), falls into Level 3 evidence.
- This level typically includes **non-randomized controlled trials** and **well-designed cohort studies** with comparison groups, which are prone to selection bias and confounding.
- The study compares two treatments but lacks randomization, making it Level 3 evidence.
*Level 1*
- Level 1 evidence is the **highest level of evidence**, derived from **systematic reviews and meta-analyses** of multiple well-designed randomized controlled trials or large, high-quality randomized controlled trials.
- The described study is explicitly stated as non-randomized, ruling out Level 1.
*Level 2*
- Level 2 evidence involves at least one **well-designed randomized controlled trial** (RCT) or **systematic reviews** of randomized trials.
- The current study is *non-randomized*, which means it cannot be classified as Level 2 evidence, as randomization is a key criterion for this level.
*Level 4*
- Level 4 evidence includes **case series**, **case-control studies**, and **poorly designed cohort or case-control studies**.
- While the study is non-randomized, it is a controlled comparative trial rather than a case series or retrospective case-control study, placing it at Level 3.
*Level 5*
- Level 5 evidence is the **lowest level of evidence**, typically consisting of **expert opinion** without explicit critical appraisal, or based on physiology, bench research, or animal studies.
- While the drug was initially tested in animal studies, the current human comparative study offers a higher level of evidence than expert opinion or preclinical data.
Therapeutic approaches targeting oncogenic viruses US Medical PG Question 2: A 60-year-old man comes to the physician’s office with jaundice. Liver ultrasound reveals a shrunken liver and biopsy reveals cirrhosis. Hepatitis serologies are below:
Anti-HAV: negative
HBsAg: negative
HBsAb: positive
HBeAg: negative
Anti-HBe: negative
Anti-HBc: negative
Anti-HCV: positive
The hepatitis C viral load is 1,000,000 copies/mL. The patient is started on an antiviral regimen including sofosbuvir. What is the mechanism of action of this drug?
- A. Inhibits reverse transcriptase
- B. Inhibits integrase
- C. Inhibits synthesis of DNA-dependent DNA polymerase
- D. Inhibits RNA-dependent RNA polymerase (Correct Answer)
- E. Inhibits hepatitis C protease
Therapeutic approaches targeting oncogenic viruses Explanation: ***Inhibits RNA-dependent RNA polymerase***
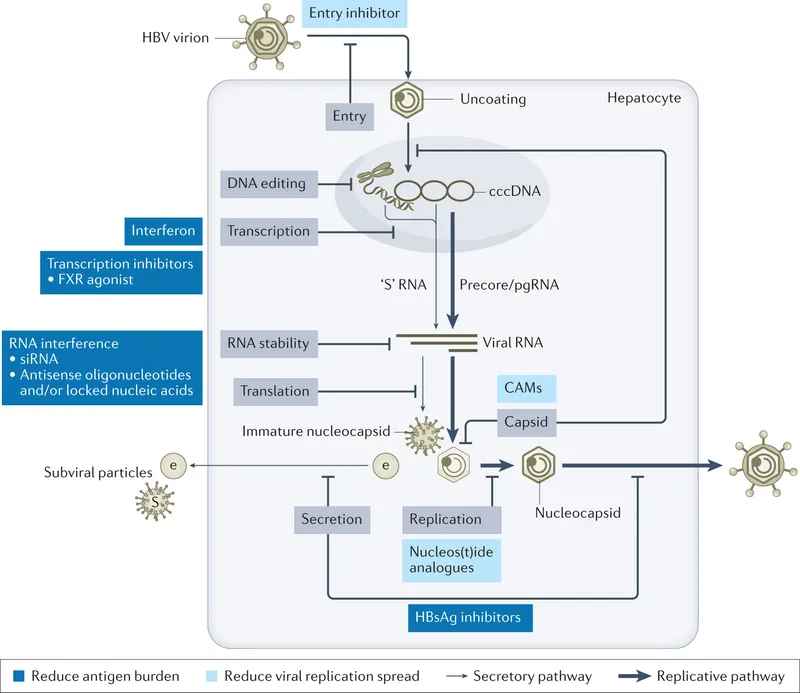
- Sofosbuvir is a **nucleotide analog** that targets the **HCV RNA-dependent RNA polymerase (NS5B)**, essential for viral replication.
- By inhibiting NS5B, it acts as a **chain terminator**, preventing the synthesis of new viral RNA strands.
*Inhibits reverse transcriptase*
- This mechanism is characteristic of drugs used to treat **HIV infection**, as reverse transcriptase is an enzyme found in retroviruses.
- Hepatitis C virus (HCV) is an **RNA virus** that replicates via an RNA intermediate, not DNA, and thus does not utilize reverse transcriptase.
*Inhibits integrase*
- Integrase inhibitors are a class of drugs primarily used in the treatment of **HIV infection**, preventing the viral DNA from integrating into the host genome.
- HCV replication does not involve an integration step into the host DNA, making this mechanism irrelevant for HCV treatment.
*Inhibits synthesis of DNA-dependent DNA polymerase*
- Inhibition of DNA-dependent DNA polymerase primarily targets organisms that replicate their DNA, such as **herpesviruses** or host cell processes.
- HCV is an RNA virus and does not synthesize or rely on a DNA-dependent DNA polymerase for its replication cycle.
*Inhibits hepatitis C protease*
- While **protease inhibitors (e.g., -previr drugs)** are an important class of anti-HCV drugs, sofosbuvir specifically targets the viral **RNA polymerase (NS5B)**.
- Protease inhibitors block the **NS3/4A protease**, which is responsible for cleaving the large HCV polyprotein into functional proteins.
Therapeutic approaches targeting oncogenic viruses US Medical PG Question 3: During an experiment, the immunophenotypes of different cells in a sample are determined. The cells are labeled with fluorescent antibodies specific to surface proteins, and a laser is then focused on the samples. The intensity of fluorescence created by the laser beam is then plotted on a scatter plot. The result shows most of the cells in the sample to be positive for CD8 surface protein. Which of the following cell types is most likely represented in this sample?
- A. Mature cytotoxic T lymphocytes (Correct Answer)
- B. Activated regulatory T lymphocytes
- C. Inactive B lymphocytes
- D. Dendritic cells
- E. Mature helper T lymphocytes
Therapeutic approaches targeting oncogenic viruses Explanation: ***Mature cytotoxic T lymphocytes***
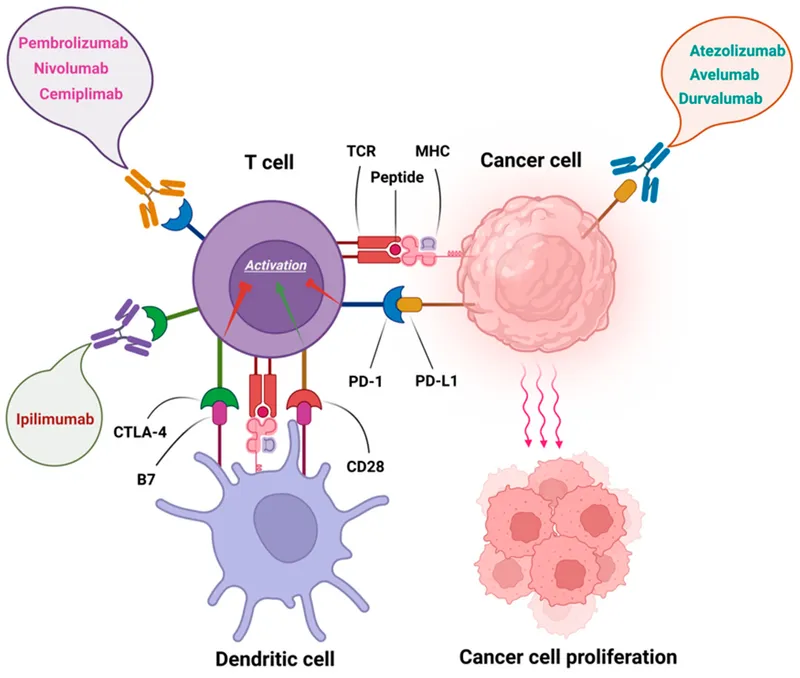
- **CD8** is a characteristic surface marker for **cytotoxic T lymphocytes**, indicating their immune function in directly killing infected or cancerous cells.
- The "mature" designation implies they have fully developed and are ready to exert their effector functions.
*Activated regulatory T lymphocytes*
- **Regulatory T lymphocytes** are typically identified by the expression of **CD4** and **CD25**, along with the intracellular transcription factor **FOXP3**, not CD8.
- Their primary role is immune suppression, not direct cytotoxicity.
*Inactive B lymphocytes*
- **B lymphocytes** are characterized by the expression of **CD19**, **CD20**, and surface immunoglobulins, which are distinct from the CD8 marker.
- Their main function is antibody production.
*Dendritic cells*
- **Dendritic cells** are primarily **antigen-presenting cells** and are identified by markers such as **CD11c** and **MHC class II molecules**, not CD8.
- While some rare subsets of dendritic cells can express CD8α, it is not their predominant or defining marker.
*Mature helper T lymphocytes*
- **Helper T lymphocytes** are defined by the expression of **CD4** and play a crucial role in coordinating the immune response.
- They do not express CD8, which is characteristic of cytotoxic T cells.
Therapeutic approaches targeting oncogenic viruses US Medical PG Question 4: A group of scientists is conducting an experiment on the human cells involved in the immune response. They genetically modify B cells so they do not express the cluster of differentiation 21 (CD21) on their cell surfaces. The pathogenesis of which of the following organisms would most likely be affected by this genetic modification?
- A. Human papillomavirus
- B. Human immunodeficiency virus (HIV)
- C. Parvovirus B19
- D. Epstein-Barr virus (EBV) (Correct Answer)
- E. Measles virus
Therapeutic approaches targeting oncogenic viruses Explanation: ***Epstein-Barr virus (EBV)***
- EBV primarily infects B cells by binding to **CD21**, also known as the **C3d receptor** or CR2.
- Absence of CD21 would prevent EBV from entering B cells, thereby disrupting its **pathogenesis** and replication cycle.
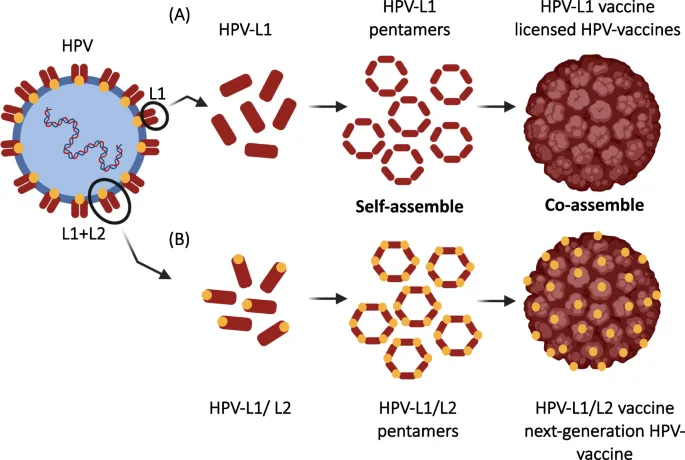
*Human papillomavirus*
- HPV primarily infects **epithelial cells** and uses entry receptors other than CD21, such as alpha-6 integrins and heparan sulfate proteoglycans.
- Its pathogenesis is not directly dependent on B cell CD21 expression.
*Human immunodeficiency virus (HIV)*
- HIV primarily infects **CD4+ T cells and macrophages** by binding to CD4 and chemokine co-receptors (CCR5 or CXCR4).
- CD21 on B cells is not a primary receptor for HIV entry or infection.
*Parvovirus B19*
- Parvovirus B19 primarily targets **erythroid progenitor cells** by binding to the **P antigen** (globoside) on their surface.
- Its infection pathway does not involve CD21 on B cells.
*Measles virus*
- Measles virus primarily uses **CD150 (SLAM)** as its receptor on immune cells (including B cells and T cells) and nectin-4 on epithelial cells.
- While B cells can be infected, CD21 is not the primary receptor for measles virus entry.
Therapeutic approaches targeting oncogenic viruses US Medical PG Question 5: A 1-year-old girl is brought to the physician for a well-child examination. She has no history of serious illness. She receives a vaccine in which a polysaccharide is conjugated to a carrier protein. Which of the following pathogens is the most likely target of this vaccine?
- A. Hepatitis A virus
- B. Varicella zoster virus
- C. Streptococcus pneumoniae (Correct Answer)
- D. Bordetella pertussis
- E. Clostridium tetani
Therapeutic approaches targeting oncogenic viruses Explanation: ***Streptococcus pneumoniae***
- This pathogen is a common cause of **pneumonia**, **otitis media**, and **meningitis** in young children. The **pneumococcal conjugate vaccine (PCV)** targets *Streptococcus pneumoniae*'s polysaccharide capsule by conjugating it to a carrier protein.
- Conjugating the polysaccharide to a protein carrier allows for a **T-cell-dependent immune response**, which is crucial for eliciting a robust and long-lasting antibody response in infants and young children, whose immune systems are not yet mature enough to respond effectively to unconjugated polysaccharide antigens.
*Hepatitis A virus*
- The vaccine for **Hepatitis A virus** is an **inactivated vaccine** containing whole killed virus particles, not a polysaccharide conjugated to a carrier protein.
- It is typically given to children to prevent **Hepatitis A infection**, which causes liver inflammation.
*Varicella zoster virus*
- The **varicella vaccine** for **Varicella zoster virus** is a **live, attenuated vaccine**, meaning it contains a weakened form of the live virus.
- This vaccine aims to prevent **chickenpox** and is not a polysaccharide-protein conjugate vaccine.
*Bordetella pertussis*
- The vaccine for **Bordetella pertussis** (whooping cough) is part of the **DTaP vaccine** and is an **acellular vaccine**, containing purified components of the bacterium.
- These components are primarily **toxoids** (inactivated toxins) or other bacterial proteins, not polysaccharides.
*Clostridium tetani*
- The vaccine for **Clostridium tetani** is a **toxoid vaccine**, meaning it contains an inactivated form of the **tetanus toxin**.
- This is part of the **DTaP vaccine** and works by stimulating an immune response against the toxin, not bacterial polysaccharides.
Therapeutic approaches targeting oncogenic viruses US Medical PG Question 6: A 45-year-old man with HIV comes to the physician because of multiple lesions on his chest and lower extremities. The lesions have progressively increased in size and are not painful or pruritic. Current medications include abacavir, dolutegravir, and lamivudine. A photograph of the lesions is shown. His CD4+ T-lymphocyte count is 450/mm3 (normal ≥ 500/mm3). A skin biopsy shows multiple spindle-shaped cells and lymphocytic infiltrate. Which of the following is the most appropriate pharmacotherapy?
- A. Ganciclovir
- B. Amphotericin B
- C. Alpha-interferon (Correct Answer)
- D. Doxycycline
- E. Nitazoxanide
Therapeutic approaches targeting oncogenic viruses Explanation: ***Alpha-interferon***
- This patient's presentation with **multiple skin lesions** in the setting of **HIV infection** and a **CD4+ count of 450/mm3** is highly suggestive of **Kaposi's sarcoma (KS)**. The biopsy findings of **spindle-shaped cells** and **lymphocytic infiltrate** further support this diagnosis. Though chemotherapy regimens are common for widespread KS, **alpha-interferon** is an appropriate treatment for **localized or less aggressive KS**, especially given his relatively preserved immune status (CD4+ count).
- Alpha-interferon exerts **antineoplastic effects** by inhibiting cell proliferation and stimulating host immune responses against tumor cells, making it suitable for managing KS.
*Ganciclovir*
- **Ganciclovir** is an antiviral agent primarily used for the treatment of **cytomegalovirus (CMV) infections**, such as retinitis or colitis, especially in immunocompromised patients.
- The patient's symptoms are not consistent with CMV disease, and the biopsy findings point away from a viral infection typically treated by ganciclovir.
*Amphotericin B*
- **Amphotericin B** is a broad-spectrum antifungal medication used to treat severe, **invasive fungal infections** like candidiasis, aspergillosis, or cryptococcosis.
- The clinical presentation and biopsy results (spindle cells, lymphocytic infiltrate) do not indicate a fungal etiology.
*Doxycycline*
- **Doxycycline** is a tetracycline antibiotic with broad antibacterial activity, used for infections like Lyme disease, chlamydia, or acne. It also has anti-inflammatory properties but is not a primary treatment for Kaposi's sarcoma.
- While some research explores its potential in KS due to its anti-angiogenic properties, it is not considered first-line pharmacotherapy for established Kaposi's sarcoma at this stage.
*Nitazoxanide*
- **Nitazoxanide** is an antiparasitic medication used to treat certain parasitic infections, such as cryptosporidiosis and giardiasis.
- The patient's symptoms and biopsy findings are not indicative of a parasitic infection.
Therapeutic approaches targeting oncogenic viruses US Medical PG Question 7: A parent presents to her pediatrician requesting information about immunizations for her newborn. The pediatrician explains about basic principles of immunization, types of vaccines, possible adverse effects, and the immunization schedule. Regarding how immunizations work, the pediatrician explains that there are mainly 2 types of vaccines. The first type of vaccine provides stronger and more lasting immunity as it induces both cellular and humoral immune responses. The second type of vaccine produces mainly a humoral response only, and its overall efficacy is less as compared to the first type. Which of the following vaccines belongs to the first type of vaccine that the pediatrician is talking about?
- A. Hepatitis A vaccine
- B. Polio vaccine (Salk)
- C. Yellow fever vaccine (Correct Answer)
- D. Rabies vaccine
- E. Hepatitis B vaccine
Therapeutic approaches targeting oncogenic viruses Explanation: ***Yellow fever vaccine***
- The Yellow fever vaccine is a **live-attenuated vaccine**, which mimics natural infection and effectively stimulates both **cellular and humoral immune responses**, leading to strong and long-lasting immunity.
- Live-attenuated vaccines contain a weakened form of the pathogen, allowing for replication within the host and robust immune system activation.
*Hepatitis A vaccine*
- The Hepatitis A vaccine is an **inactivated vaccine**, which primarily induces a **humoral (antibody-mediated) immune response**.
- Inactivated vaccines generally do not stimulate a strong cellular immune response and often require booster doses to maintain protective immunity.
*Polio vaccine (Salk)*
- The Salk polio vaccine is an **inactivated polio vaccine (IPV)**, meaning it contains killed viral particles.
- As an inactivated vaccine, it mainly elicits a **humoral immune response** producing circulating antibodies but less mucosal or cellular immunity.
*Rabies vaccine*
- The Rabies vaccine is an **inactivated vaccine** given after exposure or for pre-exposure prophylaxis.
- It primarily induces a **humoral antibody response** rather than a strong cellular immune response.
*Hepatitis B vaccine*
- The Hepatitis B vaccine is a **recombinant vaccine**, containing only a portion of the viral antigen (HBsAg).
- This type of vaccine primarily stimulates a **humoral immune response** leading to antibody production, which is effective but does not typically induce a strong cellular response like live vaccines.
Therapeutic approaches targeting oncogenic viruses US Medical PG Question 8: A 5-year-old boy is brought to the emergency room by his parents due to worsening cough, fever, and difficulty breathing in the past 2 days. Physical exam reveals a barking cough and use of accessory muscles for breathing. After a full clinical workup, he is diagnosed with an upper respiratory infection caused by a parainfluenza virus. Which of the following findings in the clinical workup of this patient supported the diagnosis?
- A. Triad of nasal discharge, conjunctivitis, and spots on the buccal mucosa
- B. Inflammation and swelling of the parotid glands and testes
- C. Photophobia, hypersalivation, and dysphagia
- D. Postauricular lymphadenopathy and rash starting on the face
- E. Chest radiograph showing narrowing of upper trachea and subglottis (Correct Answer)
Therapeutic approaches targeting oncogenic viruses Explanation: ***Chest radiograph showing narrowing of upper trachea and subglottis***
- This finding, often described as a **"steeple sign,"** is characteristic of **croup**, which is most commonly caused by parainfluenza virus and presents with **barking cough** and **stridor**.
- The narrow airway in the **subglottic region** explains the patient's difficulty breathing and use of accessory muscles.
*Triad of nasal discharge, conjunctivitis, and spots on the buccal mucosa*
- This constellation of symptoms, particularly **Koplik spots** on the buccal mucosa, is pathognomonic for **measles**, not parainfluenza virus infection.
- Measles is associated with a distinct rash that is not mentioned as a primary symptom here.
*Inflammation and swelling of the parotid glands and testes*
- This description is characteristic of **mumps**, a viral infection primarily affecting the **parotid glands** and sometimes leading to **orchitis** in males.
- Mumps does not typically present with the respiratory symptoms and barking cough described.
*Photophobia, hypersalivation, and dysphagia*
- These symptoms are highly suggestive of **rabies**, a severe viral infection of the central nervous system.
- Rabies is transmitted via animal bites and presents with neurological rather than primary respiratory symptoms.
*Postauricular lymphadenopathy and rash starting on the face*
- This clinical picture is typical of **rubella (German measles)**, characterized by a **maculopapular rash** that begins on the face and spreads downwards, often with postauricular lymph node enlargement.
- Rubella does not typically cause the severe respiratory distress and barking cough seen in this patient.
Therapeutic approaches targeting oncogenic viruses US Medical PG Question 9: A 16-year-old male is brought to the clinic by his mother for the complaints of fever, nonproductive cough, fatigue, lack of appetite, and sore throat for the past 2 months. Several other students at his high school have had similar symptoms. Physical exam shows a whitish membrane in his oropharynx, bilateral enlarged cervical lymphadenopathy, and mild splenomegaly. Which of the following tests is most likely to diagnose his condition?
- A. Monospot test (Correct Answer)
- B. Enzyme-linked immunosorbent assay
- C. Throat culture
- D. Urine culture
- E. Chest X-ray
Therapeutic approaches targeting oncogenic viruses Explanation: ***Monospot test***
- The Monospot test detects **heterophile antibodies**, which are commonly produced during an acute Epstein-Barr virus (EBV) infection, the cause of **infectious mononucleosis**.
- The patient's symptoms (fever, fatigue, nonproductive cough, sore throat, cervical lymphadenopathy, splenomegaly) and the epidemiological context (several other students with similar symptoms) are highly suggestive of **infectious mononucleosis**.
*Enzyme-linked immunosorbent assay (ELISA)*
- While ELISA can detect antibodies to various pathogens, including EBV-specific antigens, the **Monospot test** is the more common and rapid initial diagnostic tool for infectious mononucleosis.
- ELISA for EBV-specific antibodies (e.g., VCA-IgM, VCA-IgG) might be used if the Monospot test is negative but clinical suspicion remains high, especially in younger children or atypical presentations.
*Throat culture*
- A throat culture is used to identify bacterial infections, such as **Streptococcus pyogenes** (strep throat).
- Although the patient has a sore throat and a whitish membrane, his other systemic symptoms (fatigue, splenomegaly, lack of appetite for 2 months) are not typical for a bacterial pharyngitis which usually responds to antibiotics. A **nonproductive cough** also makes bacterial pharyngitis less likely.
*Urine culture*
- A urine culture is used to diagnose **urinary tract infections**.
- The patient's symptoms are not indicative of a urinary tract infection.
*Chest X-ray*
- A chest X-ray is used to evaluate the lungs for conditions such as **pneumonia**, **bronchitis**, or other respiratory pathologies.
- While the patient has a nonproductive cough, the predominant systemic symptoms (fever, fatigue, lymphadenopathy, splenomegaly) point towards a systemic viral infection rather than primarily a lung issue that would be definitively diagnosed by a chest X-ray.
Therapeutic approaches targeting oncogenic viruses US Medical PG Question 10: A 5-year-old African American female has experienced recurrent respiratory infections. To determine how well her cell-mediated immunity is performing, a Candida skin injection is administered. After 48 hours, there is no evidence of induration at the injection site. Of the following cell types, which one would normally mediate this type of immune reaction?
- A. Plasma cells
- B. Fibroblasts
- C. T-cells (Correct Answer)
- D. Mast cells
- E. Basophils
Therapeutic approaches targeting oncogenic viruses Explanation: ***T-cells***
- The **Candida skin injection** tests for **delayed-type hypersensitivity (DTH)**, also known as **Type IV hypersensitivity**, which is a classic example of **cell-mediated immunity**.
- **CD4+ Th1 helper T-cells** are the primary mediators of DTH responses. Upon re-exposure to Candida antigens, these memory T-cells release **IFN-γ and other cytokines** that recruit and activate **macrophages**, causing **induration** at the injection site within **48-72 hours**.
- The absence of induration in this patient suggests **impaired cell-mediated immunity**, which explains her recurrent infections.
*Plasma cells*
- **Plasma cells** are responsible for producing and secreting **antibodies**, which are part of the **humoral immune response** (Type II and III hypersensitivity), not cell-mediated immunity.
- While antibodies can play a role in fighting infections, they do not mediate the DTH reaction observed in a skin test.
*Fibroblasts*
- **Fibroblasts** are connective tissue cells involved in wound healing and structural support in tissues, producing **collagen** and other extracellular matrix components.
- They do not directly participate in the initiation or mediation of immune responses like cell-mediated hypersensitivity.
*Mast cells*
- **Mast cells** are primarily involved in **allergic reactions** and defense against parasites through the release of **histamine** and other inflammatory mediators.
- They mediate **immediate-type hypersensitivity reactions (Type I)**, which occur within minutes, not the delayed-type hypersensitivity response tested by a Candida skin injection that peaks at 48-72 hours.
*Basophils*
- **Basophils** are granulocytes that release **histamine** and other mediators, similar to mast cells, and are involved in **allergic reactions** and **parasitic infections**.
- Like mast cells, they primarily contribute to **Type I immediate hypersensitivity**, not the cell-mediated response of DTH.
More Therapeutic approaches targeting oncogenic viruses US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.