HPV vaccination and screening US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for HPV vaccination and screening. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
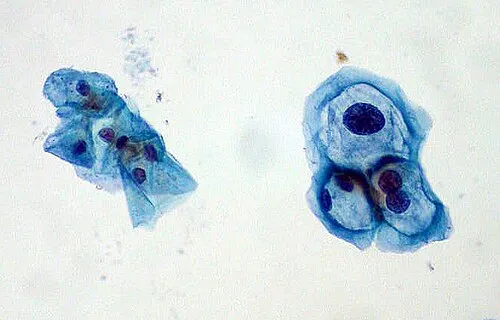
HPV vaccination and screening US Medical PG Question 1: A 38-year-old woman makes an appointment with her family physician for a routine check-up after being away due to travel for 1 year. She recently had a screening Pap smear, which was negative for malignancy. Her past medical history is significant for a Pap smear 2 years ago that reported a low-grade squamous intraepithelial lesion (LSIL). A subsequent colposcopy diagnosed high-grade cervical intraepithelial neoplasia (CIN2). The patient is surprised by the differences in her diagnostic tests. You explain to her the basis for the difference and reassure her. With this in mind, which of the following HPV serotypes is most likely to be present in the patient?
- A. HPV 33
- B. HPV 16 (Correct Answer)
- C. HPV 6
- D. HPV 31
- E. HPV 18
HPV vaccination and screening Explanation: ***HPV 16***
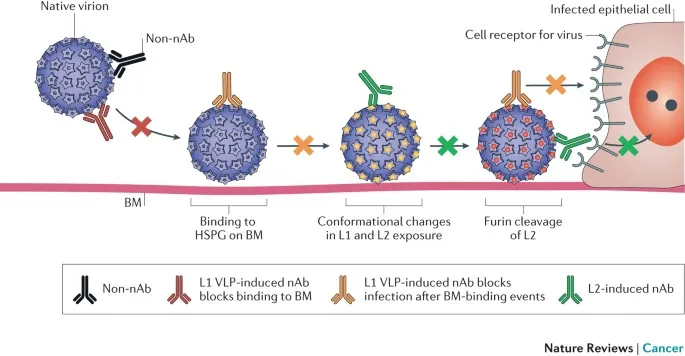
- HPV 16 is the most common **high-risk HPV serotype**, responsible for approximately 50-60% of all **cervical cancers** and a high percentage of **high-grade cervical intraepithelial neoplasia (CIN2/3)**. The progression from LSIL to CIN2 in this patient suggests infection with a high-risk type, making HPV 16 the most likely candidate.
- Given the patient's history of CIN2, a lesion of high-grade dysplasia, it is highly probable that she is infected with one of the most oncogenic HPV types, of which HPV 16 is paramount in prevalence.
*HPV 33*
- HPV 33 is a **high-risk HPV type** but is less prevalent than HPV 16 and 18 in causing cervical lesions. While it can cause CIN2, it is not the *most likely* serotype.
- It accounts for a smaller proportion of cervical cancers and high-grade dysplasias compared to HPV 16.
*HPV 6*
- HPV 6 is a **low-risk HPV type** primarily associated with **genital warts (condyloma acuminata)** and **low-grade squamous intraepithelial lesions (LSIL)** that typically do not progress to CIN2 or cervical cancer.
- Its presence would be inconsistent with the development of CIN2, as low-risk types are rarely implicated in high-grade dysplasia or malignancy.
*HPV 31*
- HPV 31 is another **high-risk HPV type** capable of causing **CIN2** and cervical cancer. However, it is less common than HPV 16.
- While plausible, HPV 16 remains statistically the most probable cause of CIN2.
*HPV 18*
- HPV 18 is a **high-risk HPV type** and is the second most common cause of **cervical cancer**, particularly **adenocarcinoma**. It is also associated with high-grade squamous lesions.
- While HPV 18 is a strong contender for high-grade lesions like CIN2, HPV 16 is still more frequently implicated in squamous cell carcinoma precursors.
HPV vaccination and screening US Medical PG Question 2: A 58-year-old woman presents to the physician for a routine gynecological visit. She denies any acute issues and remarks that she has not been sexually active for the past year. Her last Pap test was negative for any abnormal cytology. A pelvic examination and Pap test is performed at the current visit with no remarkable findings. Which of the following approaches to cervical cancer screening is most appropriate for this patient?
- A. Colposcopy in 3 years
- B. Pap test and HPV test in 5 years (Correct Answer)
- C. Pap test only in 5 years
- D. Discontinue screening until the patient becomes sexually active
- E. Colposcopy at the current visit to verify Pap test results
HPV vaccination and screening Explanation: ***Pap test and HPV test in 5 years***
- For women aged 30-65, **co-testing with both a Pap test and HPV test every 5 years** is the preferred screening interval if both results are normal.
- This patient, at 58 years old, falls within this age range, and her prior normal Pap tests along with a normal current one, support a 5-year interval for co-testing.
*Colposcopy in 3 years*
- **Colposcopy** is a diagnostic procedure performed to further evaluate abnormal Pap test results, not a routine screening method.
- Doing a colposcopy in 3 years would be an overly aggressive approach given her history of normal screenings.
*Pap test only in 5 years*
- While a Pap test alone every 3 years is an acceptable screening option, **co-testing with HPV every 5 years** is generally preferred due to its higher sensitivity for detecting precancerous lesions.
- Omitting the HPV test would reduce the effectiveness of the screening strategy in detecting cervical cancer early.
*Discontinue screening until the patient becomes sexually active*
- **Sexual activity** is a risk factor for HPV infection, but cervical cancer screening guidelines do not link its discontinuation to a lack of sexual activity.
- Women over 65 years old with a history of adequate negative screenings may discontinue screening, but this patient is 58 and does not meet that criterion yet.
*Colposcopy at the current visit to verify Pap test results*
- A **colposcopy** is indicated for **abnormal Pap test results**, which this patient does not have.
- Performing a colposcopy in the absence of abnormal findings is unnecessary and not part of routine screening.
HPV vaccination and screening US Medical PG Question 3: A 27-year-old female presents to her OB/GYN for a check-up. During her visit, a pelvic exam and Pap smear are performed. The patient does not have any past medical issues and has had routine gynecologic care with normal pap smears every 3 years since age 21. The results of the Pap smear demonstrate atypical squamous cells of undetermined significance (ASCUS). Which of the following is the next best step in the management of this patient?
- A. Repeat Pap smear in 1 year
- B. Perform colposcopy
- C. Perform an HPV DNA test (Correct Answer)
- D. Perform a Loop Electrosurgical Excision Procedure (LEEP)
- E. Repeat Pap smear in 3 years
HPV vaccination and screening Explanation: ***Perform an HPV DNA test***
- For women aged 25-29 with an **ASCUS Pap smear result**, the recommended next step is to perform an **HPV DNA test** to triage the finding.
- If the HPV test is positive, a colposcopy is indicated. If negative, routine screening can resume.
*Repeat Pap smear in 1 year*
- This approach is typically recommended for adolescents (age < 21) with an ASCUS result or for women aged 21-24 if HPV testing is not available.
- For women aged 25-29, **HPV testing** is preferred to determine the need for colposcopy.
*Perform colposcopy*
- **Colposcopy** is indicated if the HPV DNA test is positive following an ASCUS result in women 25-29, or for persistent ASCUS or low-grade squamous intraepithelial lesion (LSIL) results in younger women.
- It is not the immediate next step for ASCUS in this age group without prior HPV status.
*Perform a Loop Electrosurgical Excision Procedure (LEEP)*
- **LEEP** is a treatment for high-grade cervical dysplasia (HSIL) or recurrent/persistent LSIL, not a diagnostic step for initial ASCUS.
- Performing a LEEP based solely on an **ASCUS result** would be overly aggressive and may lead to unnecessary complications.
*Repeat Pap smear in 3 years*
- **Repeating a Pap smear in 3 years** is the recommendation for women with a normal Pap smear and negative HPV test, or for those who had an ASCUS/LSIL result with negative HPV testing and subsequent normal screening.
- It is not appropriate for an initial ASCUS finding in a 27-year-old.
HPV vaccination and screening US Medical PG Question 4: A 19-year-old woman presents for a sports physical. She says she feels healthy and has no concerns. Past medical history is significant for depression and seasonal allergies. Current medications are fluoxetine and oral estrogen/progesterone contraceptive pills. Family history is significant for a sister with polycystic ovarian syndrome (PCOS). The patient denies current or past use of alcohol, recreational drugs, or smoking. She reports that she has been on oral birth control pills since age 14 and uses condoms inconsistently. No history of STDs. She is sexually active with her current boyfriend, who was treated for chlamydia 2 years ago. She received and completed the HPV vaccination series starting at age 11. Her vital signs include: temperature 36.8°C (98.2°F), pulse 97/min, respiratory rate 16/min, blood pressure 120/75 mm Hg. Physical examination is unremarkable. Which of the following are the recommended guidelines for cervical cancer screening for this patient at this time?
- A. Cytology (pap smear) and HPV DNA co-testing every 3 years
- B. Cytology (pap smear) every 3 years
- C. Cytology (pap smear) annually
- D. Cytology (pap smear) and HPV DNA co-testing every 5 years
- E. No cervical cancer screening is indicated at this time (Correct Answer)
HPV vaccination and screening Explanation: ***No cervical cancer screening is indicated at this time***
- Current guidelines recommend initiating **cervical cancer screening** at age 21, regardless of sexual activity initiation.
- The patient is 19 years old, therefore, screening is not yet indicated per standard recommendations.
*Cytology (pap smear) and HPV DNA co-testing every 3 years*
- This option is incorrect because **co-testing** with cytology and HPV DNA is generally recommended for women aged 30-65 years, not for women under 21.
- While cytology every 3 years is a recommendation for women 21-29, co-testing is not the primary recommendation in this age group, and the patient is below the screening age.
*Cytology (pap smear) every 3 years*
- This screening interval is recommended for women aged 21-29 years, but the patient is currently 19 years old.
- Initiating screening earlier than 21 years is not recommended due to the high incidence of **transient HPV infections** and low risk of cervical cancer in younger individuals.
*Cytology (pap smear) annually*
- **Annual Pap smears** are no longer recommended for routine screening; guidelines have shifted to longer intervals due to the slow progression of cervical cancer and high rates of HPV clearance.
- Even if screening were indicated, annual cytology is not the current recommendation for any age group, especially not for a 19-year-old.
*Cytology (pap smear) and HPV DNA co-testing every 5 years*
- This screening strategy (**co-testing every 5 years**) is recommended for women aged 30-65 years.
- This patient is only 19 years old, making this recommendation inappropriate for her age.
HPV vaccination and screening US Medical PG Question 5: A 12-year-old girl presents to her primary care physician for a well-child visit. She has a history of asthma and uses her inhaler 1-2 times per week when she exercises. She does not smoke and is not currently sexually active; however, she does have a boyfriend. She lives with her mother in an apartment and is doing well in school. Her temperature is 97.6°F (36.4°C), blood pressure is 124/75 mmHg, pulse is 80/min, respirations are 12/min, and oxygen saturation is 98% on room air. Physical exam is notable for a healthy young girl with no findings. Which of the following is most appropriate for this patient at this time?
- A. Pelvic examination
- B. Serum lipids and cholesterol
- C. HPV vaccine (Correct Answer)
- D. Hypertension screening
- E. Human papilloma virus PCR
HPV vaccination and screening Explanation: ***HPV vaccine***
- The **HPV vaccine** is recommended for all adolescents, typically starting at **age 11 or 12**, to prevent HPV-related cancers and genital warts.
- While she may not be currently sexually active, the vaccine is most effective when administered **before exposure** to the virus.
*Pelvic examination*
- A **pelvic examination** is not routinely recommended for a 12-year-old girl during a well-child visit unless there are specific symptoms or concerns.
- The patient has no complaints indicating the need for such an invasive procedure.
*Serum lipids and cholesterol*
- **Lipid screening** is typically recommended for adolescents with risk factors like a family history of early cardiovascular disease or dyslipidemia, or for all adolescents sometime between ages 9 and 11 and again between 17 and 21.
- This patient does not present with any specific risk factors that would warrant immediate screening at this age, and it is not the most appropriate *initial* intervention.
*Hypertension screening*
- **Blood pressure** is already routinely measured at well-child visits, as indicated by the patient's vitals (124/75 mmHg). This is part of the standard physical exam, not a separate intervention to be chosen.
- While her blood pressure is at the higher end for her age, further evaluation would come after initial screening, which has already occurred.
*Human papilloma virus PCR*
- **HPV PCR testing** is used for screening for cervical cancer in adults (typically women age 25 and older) or for diagnostic evaluation of HPV-related lesions.
- This test is not indicated for routine screening in a 12-year-old girl, as it does not prevent HPV and is not a part of adolescent preventive care.
HPV vaccination and screening US Medical PG Question 6: A 16-year-old male is brought to the clinic by his mother for the complaints of fever, nonproductive cough, fatigue, lack of appetite, and sore throat for the past 2 months. Several other students at his high school have had similar symptoms. Physical exam shows a whitish membrane in his oropharynx, bilateral enlarged cervical lymphadenopathy, and mild splenomegaly. Which of the following tests is most likely to diagnose his condition?
- A. Monospot test (Correct Answer)
- B. Enzyme-linked immunosorbent assay
- C. Throat culture
- D. Urine culture
- E. Chest X-ray
HPV vaccination and screening Explanation: ***Monospot test***
- The Monospot test detects **heterophile antibodies**, which are commonly produced during an acute Epstein-Barr virus (EBV) infection, the cause of **infectious mononucleosis**.
- The patient's symptoms (fever, fatigue, nonproductive cough, sore throat, cervical lymphadenopathy, splenomegaly) and the epidemiological context (several other students with similar symptoms) are highly suggestive of **infectious mononucleosis**.
*Enzyme-linked immunosorbent assay (ELISA)*
- While ELISA can detect antibodies to various pathogens, including EBV-specific antigens, the **Monospot test** is the more common and rapid initial diagnostic tool for infectious mononucleosis.
- ELISA for EBV-specific antibodies (e.g., VCA-IgM, VCA-IgG) might be used if the Monospot test is negative but clinical suspicion remains high, especially in younger children or atypical presentations.
*Throat culture*
- A throat culture is used to identify bacterial infections, such as **Streptococcus pyogenes** (strep throat).
- Although the patient has a sore throat and a whitish membrane, his other systemic symptoms (fatigue, splenomegaly, lack of appetite for 2 months) are not typical for a bacterial pharyngitis which usually responds to antibiotics. A **nonproductive cough** also makes bacterial pharyngitis less likely.
*Urine culture*
- A urine culture is used to diagnose **urinary tract infections**.
- The patient's symptoms are not indicative of a urinary tract infection.
*Chest X-ray*
- A chest X-ray is used to evaluate the lungs for conditions such as **pneumonia**, **bronchitis**, or other respiratory pathologies.
- While the patient has a nonproductive cough, the predominant systemic symptoms (fever, fatigue, lymphadenopathy, splenomegaly) point towards a systemic viral infection rather than primarily a lung issue that would be definitively diagnosed by a chest X-ray.
HPV vaccination and screening US Medical PG Question 7: A 55-year-old Caucasian male presents for a routine colonoscopy. A polyp is found in the patient's transverse colon and is found to be cancerous on histological evaluation. Upon examination, it is found that these cancerous cells have decreased MHC class I expression on their surface. Which immune system cell is most capable of killing these tumor cells?
- A. Cytotoxic T-cells
- B. B-cells
- C. Macrophages
- D. Natural killer cells (Correct Answer)
- E. Eosinophils
HPV vaccination and screening Explanation: ***Natural killer cells***
- **Natural killer (NK) cells** are specialized lymphocytes that identify and kill cells with **decreased or absent MHC class I expression**, a common feature of tumor cells and virus-infected cells.
- They provide a rapid, non-specific immune response without prior sensitization.
*Cytotoxic T-cells*
- **Cytotoxic T-cells (CTLs)** recognize and kill target cells by binding to specific **antigens presented by MHC class I molecules**.
- Since these cancer cells have **decreased MHC class I expression**, CTLs would be less effective at recognizing and killing them.
*B-cells*
- **B-cells** are primarily involved in humoral immunity, producing **antibodies** that can neutralize pathogens or mark cells for destruction.
- They do not directly kill target cells, and their activation typically requires specific antigen recognition, often with T-cell help.
*Macrophages*
- **Macrophages** are phagocytic cells that engulf and digest cellular debris, pathogens, and some tumor cells.
- While they can kill tumor cells, their primary mechanism involves **phagocytosis** or antigen presentation, not direct cytotoxicity based on MHC I expression levels.
*Eosinophils*
- **Eosinophils** are granulocytes primarily involved in the defense against **parasitic infections** and in allergic reactions.
- They are not a primary defense mechanism against tumor cells, especially not based on MHC class I expression.
HPV vaccination and screening US Medical PG Question 8: A 28-year-old male with a history of HIV infection is found to have a CD4+ T lymphocyte count of 68 cells per microliter. As a consequence of his HIV infection, this patient is at increased risk of malignancy due to which of the following?
- A. Pneumocystis jiroveci
- B. Actinomyces israelii
- C. Helicobacter pylori
- D. HHV-6
- E. Epstein-Barr Virus (EBV) (Correct Answer)
HPV vaccination and screening Explanation: ***Epstein-Barr Virus (EBV)***
- **EBV** is a major cause of **AIDS-related malignancies**, particularly **B-cell lymphomas** including **non-Hodgkin lymphoma (NHL)** and **primary CNS lymphoma**, which are common in patients with CD4 counts below 100 cells/µL.
- The severe immunosuppression in **HIV/AIDS** allows for unchecked **EBV-driven lymphoproliferative disorders** due to impaired T-cell surveillance of EBV-infected B cells.
- Among the options listed, **EBV** is the only **oncogenic virus** and represents a significant cause of morbidity in advanced AIDS patients.
- **Note:** While HHV-8 (KSHV) causing Kaposi's sarcoma is also a major AIDS-related malignancy, it is not among the listed options.
*Pneumocystis jiroveci*
- **Pneumocystis jiroveci pneumonia (PCP)** is a common opportunistic **fungal infection** in HIV patients with CD4 < 200 cells/µL, causing severe respiratory illness.
- **PCP** is not oncogenic and does not increase malignancy risk; it causes acute infection, not cellular transformation.
*Actinomyces israelii*
- **Actinomyces israelii** is a gram-positive **bacterium** causing **actinomycosis**, a chronic suppurative infection with abscess formation and sinus tracts.
- While it can cause opportunistic infections in immunocompromised patients, it is **not oncogenic** and not associated with malignancy risk.
*Helicobacter pylori*
- **H. pylori** is a bacterium associated with **gastric adenocarcinoma** and **gastric MALT lymphoma** in the general population through chronic gastric inflammation.
- However, in the context of advanced HIV/AIDS with CD4 < 100, the predominant malignancy risk is from **oncogenic viruses** (EBV, HHV-8), not gastric pathology from **H. pylori**.
- **H. pylori** is not typically considered an AIDS-defining or AIDS-related malignancy.
*HHV-6*
- **Human Herpesvirus 6 (HHV-6)** causes roseola infantum in children and can reactivate in immunocompromised patients, potentially causing encephalitis or pneumonitis.
- **HHV-6** is **not established as oncogenic** and lacks strong evidence linking it to malignancy in HIV patients, unlike **EBV** (lymphomas) or **HHV-8** (Kaposi's sarcoma).
HPV vaccination and screening US Medical PG Question 9: A scientist is researching the long term effects of the hepatitis viruses on hepatic tissue. She finds that certain strains are oncogenic and increase the risk of hepatocellular carcinoma. However, they appear to do so via different mechanisms. Which of the following answer choices correctly pairs the hepatitis virus with the correct oncogenic process?
- A. Hepatitis A virus - chronic inflammation
- B. Hepatitis C virus - chronic inflammation
- C. Hepatitis E virus - integration of viral DNA into host hepatocyte genome
- D. Hepatitis B virus - integration of viral DNA into host hepatocyte genome (Correct Answer)
- E. Hepatitis A virus - integration of viral DNA into host hepatocyte genome
HPV vaccination and screening Explanation: ***Hepatitis B virus - integration of viral DNA into host hepatocyte genome***
- **Hepatitis B virus (HBV)** is a **DNA virus** that can integrate its genetic material into the host hepatocyte genome, leading to genomic instability and promoting oncogenesis.
- This integration, along with chronic inflammation and the production of viral regulatory proteins, contributes significantly to the development of **hepatocellular carcinoma (HCC)**.
*Hepatitis A virus - chronic inflammation*
- **Hepatitis A virus (HAV)** is an **RNA virus** that causes **acute hepatitis** but does not lead to chronic infection or chronic inflammation.
- Due to its acute and self-limiting nature, HAV is **not associated with hepatocellular carcinoma**.
*Hepatitis C virus - integration of viral DNA into host hepatocyte genome*
- **Hepatitis C virus (HCV)** is an **RNA virus** and therefore does not integrate its DNA into the host genome (as it has no DNA phase).
- HCV causes HCC primarily through **chronic inflammation**, **fibrosis**, and **cirrhosis**, not DNA integration.
*Hepatitis E virus - integration of viral DNA into host hepatocyte genome*
- **Hepatitis E virus (HEV)** is an **RNA virus** that typically causes acute, self-limiting hepatitis and does not integrate its genetic material into the host genome.
- While HEV can cause chronic infection in immunocompromised individuals, it is **not generally recognized as an oncogenic virus** leading to HCC.
*Hepatitis A virus - integration of viral DNA into host hepatocyte genome*
- **Hepatitis A virus (HAV)** is an **RNA virus**, meaning it does not have a DNA stage and therefore cannot integrate DNA into the host genome.
- HAV causes **acute, self-limiting infections** and is definitively **not associated with hepatocellular carcinoma**.
HPV vaccination and screening US Medical PG Question 10: A 48-year-old man comes to the physician because of a skin lesion on his nose and in his mouth. The lesions have been gradually increasing in size and are not painful or pruritic. Two months ago, he was treated for esophageal candidiasis. Physical examination shows one pinkish-brown papule on the right wing of the nose and two similar nodular lesions on the hard palate and buccal mucosa. A biopsy of one of the lesions shows spindle-shaped endothelial cells and infiltration of lymphocytes, plasma cells, and macrophages. Which of the following is the most likely causal organism of this patient's condition?
- A. Mycobacterium avium complex
- B. Epstein-Barr virus
- C. Polyomavirus
- D. Human herpes virus 8 (Correct Answer)
- E. Poxvirus
HPV vaccination and screening Explanation: ***Human herpes virus 8***
- The presence of **pinkish-brown papules/nodules** on the skin and oral mucosa, along with a history of esophageal candidiasis (which suggests an **immunocompromised state**), is highly indicative of **Kaposi's sarcoma**.
- **Biopsy findings** of spindle-shaped endothelial cells and inflammatory infiltrate are characteristic features of Kaposi's sarcoma, which is caused by HHV-8.
*Mycobacterium avium complex*
- This infection usually presents with **systemic symptoms** like fever, night sweats, weight loss, and adenopathy, or gastrointestinal symptoms, rather than localized skin and oral lesions.
- Granulomas, not spindle cell lesions, would be expected on **biopsy**.
*Epstein-Barr virus*
- EBV is associated with various lymphoproliferative disorders and lymphomas, as well as **oral hairy leukoplakia** in immunocompromised patients.
- It does not typically cause the **vascular, nodular lesions** described here.
*Polyomavirus*
- Polyomaviruses (e.g., JC virus, BK virus) are associated with **progressive multifocal leukoencephalopathy** and **nephropathy** in immunocompromised patients.
- They do not cause these specific types of **skin and oral lesions**.
*Poxvirus*
- Poxviruses (e.g., molluscum contagiosum) cause **umbilicated papules** or extensive skin lesions but are not associated with the **vascular spindle cell proliferation** seen in Kaposi's sarcoma.
- The lesions caused by poxviruses have a different **histological appearance**.
More HPV vaccination and screening US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.