HPV-associated cancers US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for HPV-associated cancers. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
HPV-associated cancers US Medical PG Question 1: A 38-year-old woman makes an appointment with her family physician for a routine check-up after being away due to travel for 1 year. She recently had a screening Pap smear, which was negative for malignancy. Her past medical history is significant for a Pap smear 2 years ago that reported a low-grade squamous intraepithelial lesion (LSIL). A subsequent colposcopy diagnosed high-grade cervical intraepithelial neoplasia (CIN2). The patient is surprised by the differences in her diagnostic tests. You explain to her the basis for the difference and reassure her. With this in mind, which of the following HPV serotypes is most likely to be present in the patient?
- A. HPV 33
- B. HPV 16 (Correct Answer)
- C. HPV 6
- D. HPV 31
- E. HPV 18
HPV-associated cancers Explanation: ***HPV 16***
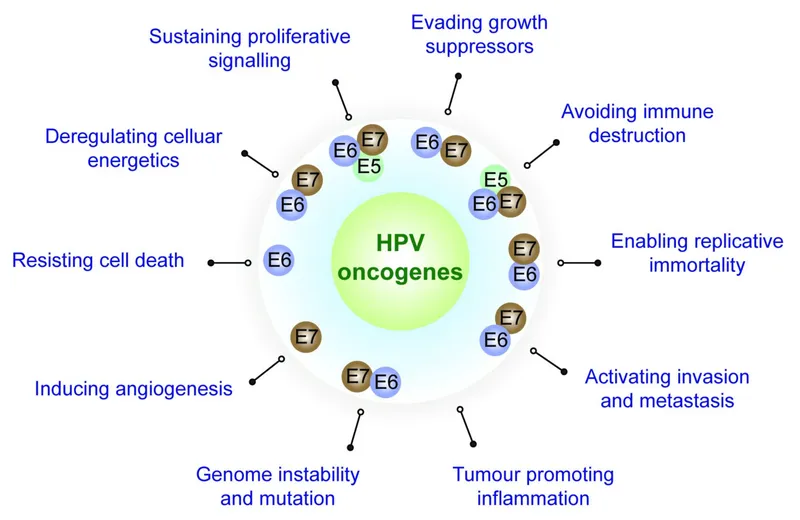
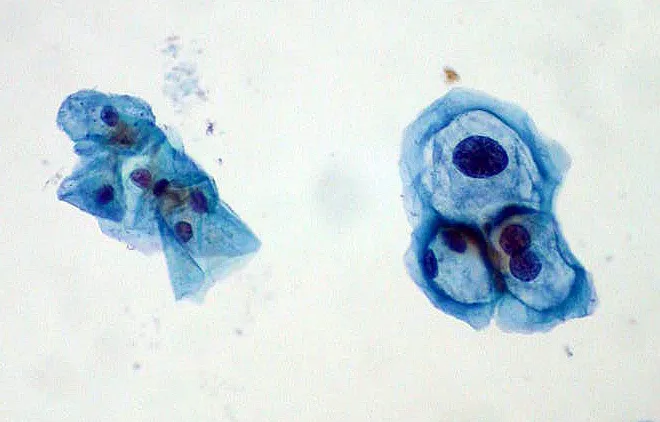
- HPV 16 is the most common **high-risk HPV serotype**, responsible for approximately 50-60% of all **cervical cancers** and a high percentage of **high-grade cervical intraepithelial neoplasia (CIN2/3)**. The progression from LSIL to CIN2 in this patient suggests infection with a high-risk type, making HPV 16 the most likely candidate.
- Given the patient's history of CIN2, a lesion of high-grade dysplasia, it is highly probable that she is infected with one of the most oncogenic HPV types, of which HPV 16 is paramount in prevalence.
*HPV 33*
- HPV 33 is a **high-risk HPV type** but is less prevalent than HPV 16 and 18 in causing cervical lesions. While it can cause CIN2, it is not the *most likely* serotype.
- It accounts for a smaller proportion of cervical cancers and high-grade dysplasias compared to HPV 16.
*HPV 6*
- HPV 6 is a **low-risk HPV type** primarily associated with **genital warts (condyloma acuminata)** and **low-grade squamous intraepithelial lesions (LSIL)** that typically do not progress to CIN2 or cervical cancer.
- Its presence would be inconsistent with the development of CIN2, as low-risk types are rarely implicated in high-grade dysplasia or malignancy.
*HPV 31*
- HPV 31 is another **high-risk HPV type** capable of causing **CIN2** and cervical cancer. However, it is less common than HPV 16.
- While plausible, HPV 16 remains statistically the most probable cause of CIN2.
*HPV 18*
- HPV 18 is a **high-risk HPV type** and is the second most common cause of **cervical cancer**, particularly **adenocarcinoma**. It is also associated with high-grade squamous lesions.
- While HPV 18 is a strong contender for high-grade lesions like CIN2, HPV 16 is still more frequently implicated in squamous cell carcinoma precursors.
HPV-associated cancers US Medical PG Question 2: A 41-year-old man with HIV comes to the physician because of rectal bleeding and itching for 2 weeks. During this period, he has also had pain with defecation. Four months ago, he was diagnosed with anogenital warts that were treated with cryotherapy. Over the past year, he has been sexually active with 3 male partners. He uses condoms inconsistently. Current medications are zidovudine, emtricitabine, and efavirenz. Digital rectal examination and anoscopy show an exophytic mass on the anal margin that is protruding into the anal canal. The mass is tender to palpation and bleeds easily on contact. Laboratory studies show a leukocyte count of 7,600/mm3 and a CD4+ T-lymphocyte count of 410/mm3 (N ≥ 500). A biopsy specimen of the lesion shows a well-differentiated squamous cell carcinoma. Which of the following cellular processes was most likely involved in the pathogenesis of this patient's malignancy?
- A. Activation of c-myc gene
- B. Inactivation of TP53 gene (Correct Answer)
- C. Activation of TAX gene
- D. Inactivation of VHL gene
- E. Inactivation of WT1 gene
HPV-associated cancers Explanation: ***Inactivation of TP53 gene***
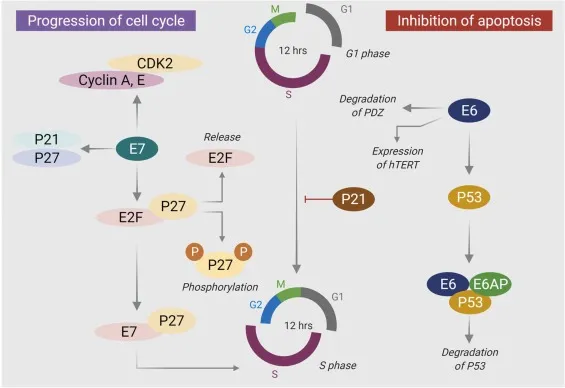
- This patient's **squamous cell carcinoma** (SCC) of the anus is strongly associated with **human papillomavirus (HPV) infection**, which is common in HIV-positive sexually active men. HPV oncoproteins, particularly E6, promote the degradation of the **TP53 tumor suppressor protein**.
- Inactivating mutations or degradation of **TP53** remove a critical checkpoint in the cell cycle, allowing cells with DNA damage to proliferate uncontrollably and contributing to carcinogenesis.
*Activation of c-myc gene*
- The **c-myc proto-oncogene** is involved in cell proliferation, differentiation, and apoptosis, and its activation is commonly seen in lymphomas (e.g., Burkitt lymphoma) and other cancers.
- While *c-myc* activation can contribute to various malignancies, it is not the **primary molecular mechanism** linked to HPV-associated anal squamous cell carcinoma.
*Activation of TAX gene*
- The **TAX gene** is a transforming gene of **human T-cell lymphotropic virus type 1 (HTLV-1)**, responsible for T-cell leukemia/lymphoma.
- This patient's presentation with anal squamous cell carcinoma, rather than a hematologic malignancy, makes HTLV-1 and TAX gene activation an unlikely cause.
*Inactivation of VHL gene*
- The **VHL (Von Hippel-Lindau) gene** is a tumor suppressor gene whose inactivation is strongly associated with **renal cell carcinoma** (clear cell type) and other tumors like pheochromocytoma and hemangioblastoma.
- Inactivation of **VHL** is not a primary mechanism in the development of anal squamous cell carcinoma.
*Inactivation of WT1 gene*
- The **WT1 (Wilms tumor 1) gene** is a tumor suppressor gene primarily associated with **Wilms tumor**, a kidney cancer that typically affects children.
- Inactivation of **WT1** is not a known pathogenic mechanism for anal squamous cell carcinoma in adults.
HPV-associated cancers US Medical PG Question 3: A 25-year-old woman presents for STI screening. She reports consistent condom use with her partner. Which of the following STIs is least effectively prevented by proper condom use?
- A. Chlamydia
- B. Gonorrhea
- C. HIV
- D. HPV (Correct Answer)
- E. Hepatitis B
HPV-associated cancers Explanation: ***HPV***
- **Human Papillomavirus** is primarily transmitted through skin-to-skin contact, making it difficult to prevent even with consistent condom use [1].
- Condoms may not cover all infected skin areas, allowing for transmission from areas like the **scrotum** or **perineum** [1].
*Chlamydia*
- **Chlamydia trachomatis** is a bacterial infection primarily transmitted through **genital fluid exchange**, which is largely prevented by condoms.
- Consistent and correct condom use significantly reduces the risk of transmission.
*Gonorrhea*
- **Neisseria gonorrhoeae** is a bacterial infection transmitted through **mucous membrane contact** and **genital fluids**, effectively blocked by condoms.
- Condoms serve as a reliable barrier against the transmission of this bacterium.
*HIV*
- **Human Immunodeficiency Virus** is transmitted through **bodily fluids** including semen and vaginal fluid; condoms are highly effective in preventing this exchange.
- When used correctly and consistently, condoms are a critical tool in preventing HIV transmission.
*Hepatitis B*
- **Hepatitis B virus (HBV)** is transmitted through **blood** and **bodily fluids**, including sexual contact.
- Condoms provide a significant physical barrier against the exchange of these fluids, thus reducing transmission risk.
HPV-associated cancers US Medical PG Question 4: A public health campaign increases vaccination rates against human papillomaviruses 16 and 18. Increased vaccination rates would have which of the following effects on the Papanicolaou test?
- A. Decreased true positive rate
- B. Decreased positive predictive value (Correct Answer)
- C. Decreased negative predictive value
- D. Increased positive likelihood ratio
- E. Increased true negative rate
HPV-associated cancers Explanation: ***Decreased positive predictive value***
- An increase in vaccination rates against **HPV 16 and 18** will reduce the **prevalence of cervical dysplasia and cancer** caused by these types.
- With fewer true cases in the population, a Papanicolaou (Pap) test is more likely to yield a **false positive result** when it tests positive, thus decreasing its **positive predictive value**.
- **PPV = TP/(TP+FP)** - when disease prevalence decreases, the number of true positives decreases while false positives remain relatively stable, reducing the overall PPV.
*Decreased true positive rate*
- The **true positive rate (sensitivity)** of the Pap test refers to its ability to correctly identify individuals with the disease (cervical dysplasia/cancer).
- While the overall number of true positives will decrease due to reduced disease prevalence, the inherent ability of the test to detect existing disease (i.e., its sensitivity) is **not directly affected by vaccination rates**.
- Sensitivity is an intrinsic test property: **Sensitivity = TP/(TP+FN)**.
*Decreased negative predictive value*
- The **negative predictive value** is the probability that a person with a negative test result truly does not have the disease.
- As the prevalence of the disease decreases due to vaccination, the probability of a negative test being truly negative actually **increases**, leading to an **increased negative predictive value**.
- **NPV = TN/(TN+FN)** - lower prevalence means fewer false negatives relative to true negatives.
*Increased positive likelihood ratio*
- The **positive likelihood ratio** describes how much more likely a positive test result is in someone with the disease compared to someone without the disease and is derived from sensitivity and specificity.
- **LR+ = Sensitivity/(1-Specificity)** - vaccination reduces disease prevalence but does not inherently change the **diagnostic accuracy** (sensitivity and specificity) of the Pap test, so the likelihood ratio remains unchanged.
*Increased true negative rate*
- The **true negative rate (specificity)** of the Pap test refers to its ability to correctly identify individuals who do not have the disease.
- While the overall number of true negatives will increase (because there are fewer cases to begin with), the inherent ability of the test to correctly identify healthy individuals (i.e., its specificity) is **not directly affected by the change in disease prevalence**.
- Specificity is an intrinsic test property: **Specificity = TN/(TN+FP)**.
HPV-associated cancers US Medical PG Question 5: A 55-year-old postmenopausal woman comes to the physician for a screening Pap smear. She has no history of serious illness. Her last Pap smear was 10 years ago and showed no abnormalities. She has smoked one-half pack of cigarettes daily for 20 years and drinks 3 bottles of wine per week. She is sexually active with multiple male partners and uses condoms inconsistently. Her paternal grandmother had ovarian cancer and her maternal aunt had breast cancer. Pelvic examination shows multiple red, fleshy polypoid masses on the anterior vaginal wall. A biopsy is obtained and histology shows large cells with abundant clear cytoplasm. Which of the following is the most significant risk factor for this diagnosis?
- A. Family history of breast and ovarian cancer
- B. Human papillomavirus infection
- C. Alcohol consumption
- D. Diethylstilbestrol exposure in utero (Correct Answer)
- E. Cigarette smoking
HPV-associated cancers Explanation: ***Diethylstilbestrol exposure in utero***
- The patient's presentation with **clear cell carcinoma of the vagina**, characterized by **red, fleshy polypoid masses** and **large cells with abundant clear cytoplasm**, is highly suggestive of this diagnosis.
- **In utero exposure to diethylstilbestrol (DES)** is a classic and significant risk factor for the development of clear cell adenocarcinoma of the vagina and cervix.
*Family history of breast and ovarian cancer*
- While a family history of breast and ovarian cancer may indicate an increased risk for other gynecological cancers (e.g., BRCA mutations), it is **not directly linked** to clear cell adenocarcinoma of the vagina.
- This family history points more towards **hereditary breast and ovarian cancer syndromes**, not the specific pathology described.
*Human papillomavirus infection*
- **HPV infection** is a major risk factor for most cases of **squamous cell carcinoma of the vagina and cervix**, and also increases the risk of adenocarcinoma of the cervix.
- However, HPV is **not a primary risk factor for clear cell adenocarcinoma of the vagina**, which has a distinct etiology.
*Alcohol consumption*
- While excessive **alcohol consumption** can be associated with an increased risk of certain cancers, it is **not a specific or significant risk factor** for clear cell adenocarcinoma of the vagina.
- It generally contributes to a broad range of cancers rather than specific rare forms.
*Cigarette smoking*
- **Cigarette smoking** is a well-established risk factor for **squamous cell carcinoma of the cervix and vagina**, among other cancers.
- However, it is **not a recognized significant risk factor** for the development of **clear cell adenocarcinoma of the vagina**.
HPV-associated cancers US Medical PG Question 6: A 40-year-old male presents to his primary care physician for a regularly scheduled check-up. Physical examination reveals nontender cervical lymphadenopathy. A biopsy of the lymph node reveals aggregates of follicular architecture, and cytogenic analysis shows a t(14;18) translocation. The protein most likely responsible for the patient’s condition does which of the following:
- A. Regulates passage through the cell cycle
- B. Activates DNA repair proteins
- C. Regulates cell growth through signal transduction
- D. Inhibits apoptosis (Correct Answer)
- E. Provides mitotic cytoskeleton
HPV-associated cancers Explanation: ***Inhibits apoptosis***
- The t(14;18) translocation is characteristic of **follicular lymphoma** and leads to the overexpression of the **BCL-2 protein**.
- **BCL-2** is an anti-apoptotic protein that prevents programmed cell death, allowing abnormal cells to accumulate.
*Regulates passage through the cell cycle*
- Proteins involved in **cell cycle regulation** (e.g., p53, Rb) control progression through different phases, but BCL-2's primary role is in cell survival, not direct cell cycle progression.
- Dysregulation of cell cycle proteins is seen in many cancers, but the specific BCL-2 translocation primarily affects apoptosis.
*Activates DNA repair proteins*
- **DNA repair proteins** (e.g., ATM, BRCA1/2) are crucial for maintaining genomic integrity and correcting DNA damage.
- While important in cancer development, their activation is not the direct function of the BCL-2 protein overexpressed due to the t(14;18) translocation.
*Regulates cell growth through signal transduction*
- **Signal transduction pathways** often involve growth factors and their receptors (e.g., RTKs) that regulate cell proliferation and differentiation.
- While BCL-2 indirectly impacts cell numbers by preventing apoptosis, its direct role is not in initiating or participating in growth-promoting signal transduction cascades.
*Provides mitotic cytoskeleton*
- The **mitotic cytoskeleton**, composed of microtubules, is essential for chromosome segregation during cell division.
- Proteins like tubulin are the primary components, and BCL-2 has no direct role in forming or organizing these structures.
HPV-associated cancers US Medical PG Question 7: A 57-year-old man presents to the office with complaints of perianal pain during defecation and perineal heaviness for 1 month. He also complains of discharge around his anus, and bright red bleeding during defecation. The patient provides a history of having a sexual relationship with other men without using any methods of protection. The physical examination demonstrates edematous verrucous anal folds that are of hard consistency and painful to the touch. A proctosigmoidoscopy reveals an anal canal ulcer with well defined, indurated borders on a white background. A biopsy is taken and the results are pending. What is the most likely diagnosis?
- A. Anal cancer (Correct Answer)
- B. Polyps
- C. Anal fissure
- D. Hemorrhoids
- E. Proctitis
HPV-associated cancers Explanation: ***Anal cancer***
- The patient's presentation with **perianal pain**, **bleeding**, **discharge**, and **edematous verrucous anal folds** (suggesting a lesion) are highly suspicious for anal cancer. His history of unprotected sexual relationships with men is a significant risk factor for **HPV infection**, which is a leading cause of anal squamous cell carcinoma.
- The proctosigmoidoscopy findings of an **anal canal ulcer with well-defined, indurated borders** and a white background further point towards a malignant lesion, making anal cancer the most likely diagnosis.
*Polyps*
- While polyps can cause bleeding, they typically do not present with **indurated, painful verrucous lesions** or an ulcer with defined borders.
- Polyps are usually soft and less likely to cause the severe perianal pain and perineal heaviness described.
*Anal fissure*
- An anal fissure is a **linear tear** in the anal canal, causing sharp pain during defecation and bright red blood.
- It would not typically present with **edematous verrucous anal folds**, perineal heaviness, or an indurated ulcer as seen on proctosigmoidoscopy.
*Hemorrhoids*
- Hemorrhoids commonly cause **bright red bleeding** and can cause discomfort or heaviness.
- However, they usually appear as swollen vascular cushions and do not typically present as **indurated, painful verrucous lesions** or an ulcer with defined borders.
*Proctitis*
- Proctitis is an inflammation of the rectum, causing rectal pain, tenesmus, and bleeding, often due to **inflammatory bowel disease** or **infections**.
- While it can cause some of the symptoms, it wouldn't typically manifest as a distinct **indurated, verrucous lesion** or an ulcer with firm borders, which are more indicative of a mass.
HPV-associated cancers US Medical PG Question 8: A 5-year-old girl presents to the emergency room with acute airway obstruction. Physical examination shows cough, episodic wheezing, and excess mucus production. Increased quantities of which of the following would predispose the child to extrinsic asthma:
- A. Kupffer cells
- B. Th17 lymphocytes
- C. Th1 lymphocytes
- D. Treg lymphocytes
- E. Th2 lymphocytes (Correct Answer)
HPV-associated cancers Explanation: ***Th2 lymphocytes***
- **Th2 lymphocytes** play a central role in the pathogenesis of **extrinsic (allergic) asthma** by promoting allergic inflammation.
- They produce cytokines like **IL-4, IL-5, and IL-13**, which drive **IgE production**, **eosinophil activation**, and **mucus hypersecretion**, all characteristic features of asthma.
*Kupffer cells*
- **Kupffer cells** are specialized macrophages found in the liver, primarily involved in clearing pathogens and debris from the portal circulation.
- They are not directly involved in the pathogenesis of airway obstruction or allergic asthma.
*Th17 lymphocytes*
- **Th17 lymphocytes** are involved in host defense against extracellular bacteria and fungi and contribute to inflammation in autoimmune diseases.
- While they can be involved in some forms of severe asthma, they are not the primary drivers of **extrinsic, allergic asthma** characterized by IgE and eosinophilia.
*Th1 lymphocytes*
- **Th1 lymphocytes** primarily mediate cellular immunity against intracellular pathogens and are involved in delayed-type hypersensitivity reactions.
- They produce **IFN-γ**, which typically *suppresses* Th2 responses, and are therefore generally considered protective against allergic asthma.
*Treg lymphocytes*
- **Treg lymphocytes** (regulatory T cells) are crucial for maintaining immune tolerance and suppressing excessive immune responses.
- Their primary role is to *prevent* allergic and autoimmune diseases; therefore, an *increase* in their numbers would typically *reduce* the likelihood of asthma, not predispose to it.
HPV-associated cancers US Medical PG Question 9: An 82-year-old woman is brought to the physician by her daughter because of a 3-day history of a runny nose, headache, and cough. The patient's grandson recently had similar symptoms. Her vital signs are within normal limits. Pulse oximetry on room air shows an oxygen saturation of 99%. Lungs are clear to auscultation. Testing of nasal secretions is performed to identify the viral strain. Electron microscopy shows a non-enveloped RNA virus with an icosahedral capsid. Binding to which of the following is responsible for the virulence of this virus?
- A. CD21
- B. Integrin
- C. ICAM-1 (Correct Answer)
- D. P antigen
- E. Sialic acid residues
HPV-associated cancers Explanation: Both the clinical presentation (runny nose, headache, cough, viral spread) and the electron microscopy finding of a **non-enveloped RNA virus with an icosahedral capsid** are characteristic of a **rhinovirus** (a member of the Picornaviridae family).
***Correct: ICAM-1***
- **Rhinoviruses** primarily infect the upper respiratory tract and bind to **ICAM-1 (intercellular adhesion molecule-1)** on respiratory epithelial cells.
- Approximately **90% of rhinovirus serotypes** use ICAM-1 as their primary cellular receptor.
- This binding facilitates viral entry and is the key factor in the **virulence** of rhinovirus, leading to common cold symptoms.
*Incorrect: CD21*
- **CD21** is the receptor for **Epstein-Barr virus (EBV)**, which causes infectious mononucleosis, a condition distinct from the common cold.
- EBV is an **enveloped DNA virus**, unlike the non-enveloped RNA virus described in this case.
*Incorrect: Integrin*
- **Integrins** are cell adhesion receptors used by some viruses for entry (e.g., certain adenoviruses and enteroviruses).
- However, they are **not the primary receptor** for rhinovirus, which predominantly uses ICAM-1.
- The description of an **icosahedral non-enveloped RNA virus** with upper respiratory symptoms specifically points to rhinovirus and ICAM-1.
*Incorrect: P antigen*
- The **P antigen** (globoside) is the receptor for **parvovirus B19**, which causes Fifth disease (erythema infectiosum) and aplastic crisis.
- Parvovirus B19 is a **non-enveloped DNA virus** (not RNA), which is distinct from the virus described in this question.
*Incorrect: Sialic acid residues*
- **Sialic acid residues** are the receptors for **influenza viruses** (via hemagglutinin) for viral attachment and entry.
- Influenza viruses are **enveloped RNA viruses** and typically cause more severe systemic symptoms (fever, myalgias) than the mild upper respiratory symptoms described here.
HPV-associated cancers US Medical PG Question 10: A 53-year-old man presents to an urgent care center with severe fever that began during the day along with muscle and joint pains. He states that he felt fine the day before but then developed a fever to 103°F (39.4°C) and had to leave work after which he developed a headache and body pains. The patient states that he was recently in South Asia for a business trip and was otherwise feeling well since returning 2 weeks ago. On exam, the patient’s temperature is 103.3°F (39.6°C), blood pressure is 110/84 mmHg, pulse is 94/min, and respirations are 14/min. On physical exam, the patient appears flushed and has a rash that blanches when touched. On laboratory workup, the pathogen was identified as an enveloped virus with an icosahedral capsid and had positive-sense, single-stranded linear RNA. Which of the following is the most likely cause of this patient's presentation?
- A. Dengue virus (Correct Answer)
- B. Norovirus
- C. Coronavirus
- D. Marburg virus
- E. Saint Louis encephalitis virus
HPV-associated cancers Explanation: ***Dengue virus***
- The patient's presentation with **acute onset of high fever**, severe **muscle and joint pains** ("breakbone fever"), headache, and a **blanching rash** after recent travel to **South Asia** is highly characteristic of dengue fever.
- The description of the pathogen as an **enveloped virus** with an **icosahedral capsid** and **positive-sense, single-stranded linear RNA** perfectly matches the **Flaviviridae family** to which the dengue virus belongs.
- Among the options, only dengue virus and Saint Louis encephalitis virus have these exact structural characteristics (both are flaviviruses), but the **clinical presentation** with severe myalgia/arthralgia and travel to South Asia clearly points to dengue.
*Norovirus*
- Norovirus typically causes **gastroenteritis**, characterized primarily by **vomiting, diarrhea**, and abdominal cramps, which are not the dominant symptoms in this patient.
- While fever can occur, it's usually **mild** and not as prominent as the high fever and severe myalgia/arthralgia seen in dengue.
- **Structurally**, norovirus is **non-enveloped** (naked capsid), which does not match the pathogen description.
*Coronavirus*
- Coronaviruses are associated with **respiratory illnesses** (e.g., common cold, SARS, MERS, COVID-19) causing symptoms like cough, shortness of breath, and sore throat.
- While fever and body aches can occur, the **severe joint pains** and typical rash are not hallmarks of coronavirus infections.
- **Structurally**, coronaviruses have **helical nucleocapsid symmetry**, not icosahedral, which excludes this option based on the pathogen description.
*Marburg virus*
- Marburg virus causes a severe **hemorrhagic fever** with symptoms including high fever, severe headache, malaise, followed by gastrointestinal symptoms, and eventually **hemorrhagic manifestations** (e.g., bleeding from orifices, petechiae, purpura).
- The patient's presentation does not describe any hemorrhagic signs, and the rash is blanching, not petechial or purpuric.
- **Structurally**, Marburg is a filovirus with **helical symmetry** and **negative-sense ssRNA**, not positive-sense with icosahedral capsid, which excludes this option.
*Saint Louis encephalitis virus*
- Saint Louis encephalitis virus causes a **neuroinvasive disease** characterized by encephalitis, presenting with altered mental status, seizures, and focal neurological deficits, although some patients may have milder fever and headache.
- While it shares the **same viral structure** as dengue (both are flaviviruses with enveloped, icosahedral, (+)ssRNA), the **clinical presentation** differs significantly—this patient lacks neurological symptoms.
- The prominent **severe myalgia, arthralgia**, typical blanching rash, and **travel history to dengue-endemic South Asia** distinguish dengue from Saint Louis encephalitis.
More HPV-associated cancers US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.