Hepatitis C and hepatocellular carcinoma US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hepatitis C and hepatocellular carcinoma. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hepatitis C and hepatocellular carcinoma US Medical PG Question 1: A scientist is researching the long term effects of the hepatitis viruses on hepatic tissue. She finds that certain strains are oncogenic and increase the risk of hepatocellular carcinoma. However, they appear to do so via different mechanisms. Which of the following answer choices correctly pairs the hepatitis virus with the correct oncogenic process?
- A. Hepatitis A virus - chronic inflammation
- B. Hepatitis C virus - chronic inflammation
- C. Hepatitis E virus - integration of viral DNA into host hepatocyte genome
- D. Hepatitis B virus - integration of viral DNA into host hepatocyte genome (Correct Answer)
- E. Hepatitis A virus - integration of viral DNA into host hepatocyte genome
Hepatitis C and hepatocellular carcinoma Explanation: ***Hepatitis B virus - integration of viral DNA into host hepatocyte genome***
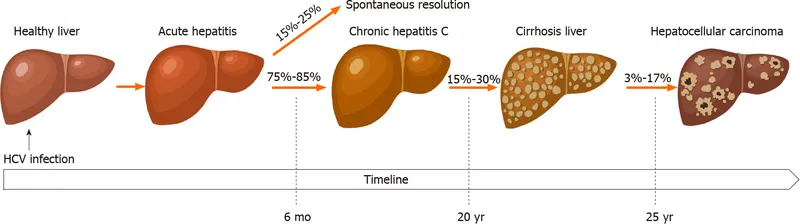
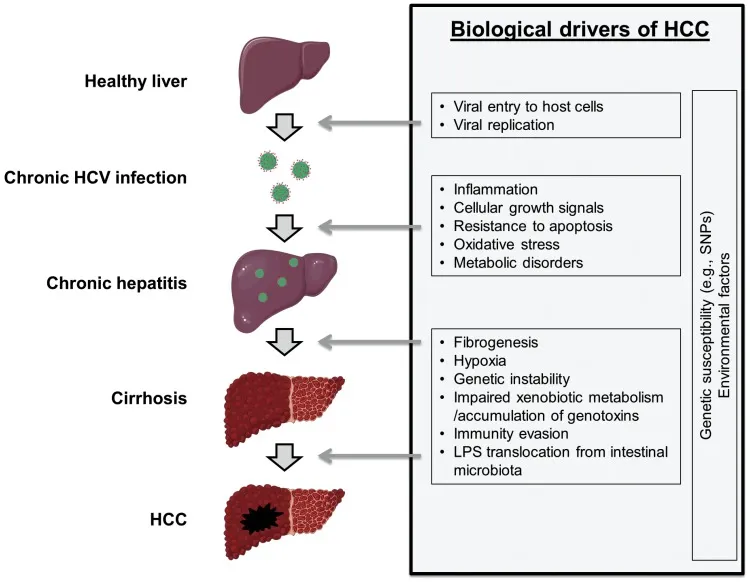
- **Hepatitis B virus (HBV)** is a **DNA virus** that can integrate its genetic material into the host hepatocyte genome, leading to genomic instability and promoting oncogenesis.
- This integration, along with chronic inflammation and the production of viral regulatory proteins, contributes significantly to the development of **hepatocellular carcinoma (HCC)**.
*Hepatitis A virus - chronic inflammation*
- **Hepatitis A virus (HAV)** is an **RNA virus** that causes **acute hepatitis** but does not lead to chronic infection or chronic inflammation.
- Due to its acute and self-limiting nature, HAV is **not associated with hepatocellular carcinoma**.
*Hepatitis C virus - integration of viral DNA into host hepatocyte genome*
- **Hepatitis C virus (HCV)** is an **RNA virus** and therefore does not integrate its DNA into the host genome (as it has no DNA phase).
- HCV causes HCC primarily through **chronic inflammation**, **fibrosis**, and **cirrhosis**, not DNA integration.
*Hepatitis E virus - integration of viral DNA into host hepatocyte genome*
- **Hepatitis E virus (HEV)** is an **RNA virus** that typically causes acute, self-limiting hepatitis and does not integrate its genetic material into the host genome.
- While HEV can cause chronic infection in immunocompromised individuals, it is **not generally recognized as an oncogenic virus** leading to HCC.
*Hepatitis A virus - integration of viral DNA into host hepatocyte genome*
- **Hepatitis A virus (HAV)** is an **RNA virus**, meaning it does not have a DNA stage and therefore cannot integrate DNA into the host genome.
- HAV causes **acute, self-limiting infections** and is definitively **not associated with hepatocellular carcinoma**.
Hepatitis C and hepatocellular carcinoma US Medical PG Question 2: A 32-year-old woman comes to the physician because of a 3-month history of fatigue and myalgia. Over the past month, she has had intermittent episodes of nausea. She has a history of intravenous drug use, but she has not used illicit drugs for the past five years. She has smoked one pack of cigarettes daily for 14 years and drinks one alcoholic beverage daily. She takes no medications. Her last visit to a physician was 4 years ago. Her temperature is 37°C (98.6°F), pulse is 90/min, respirations are 20/min, and blood pressure is 110/70 mm Hg. Physical examination shows jaundice and hepatosplenomegaly. There are also blisters and erosions on the dorsum of both hands. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 12 g/dL
Leukocyte count 8,300/mm3
Platelet count 250,000/mm3
Serum
Glucose 170 mg/dL
Albumin 3.0 g/dL
Total bilirubin 2.2 mg/dL
Alkaline phosphatase 80 U/L
AST 92 U/L
ALT 76 U/L
Hepatitis B surface antigen negative
Hepatitis B surface antibody positive
Hepatitis B core antibody positive
Hepatitis C antibody positive
Which of the following is the most appropriate next step in diagnosis?
- A. PCR for viral DNA
- B. Western blot for HIV
- C. Serology for anti-HAV IgM
- D. PCR for viral RNA (Correct Answer)
- E. Liver biopsy
Hepatitis C and hepatocellular carcinoma Explanation: ***Correct: PCR for viral RNA***
- The patient has high suspicion for **chronic hepatitis C infection** due to a history of intravenous drug use, the presence of **fatigue**, **myalgia**, **jaundice**, hepatosplenomegaly, and **elevated liver enzymes (AST and ALT)**
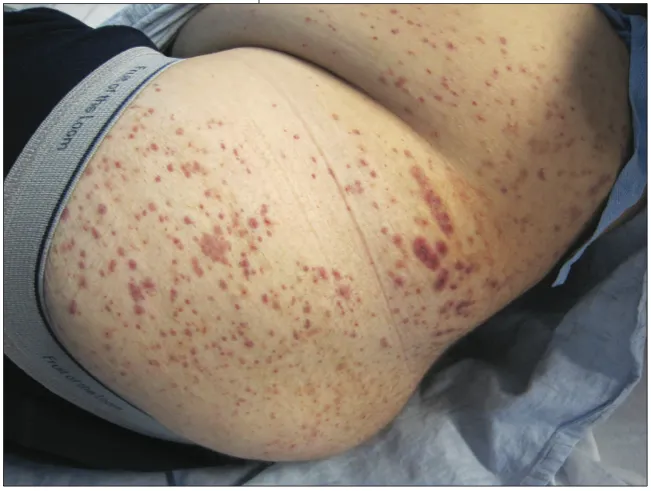
- The **blisters and erosions on the dorsum of both hands** are highly suggestive of **porphyria cutanea tarda (PCT)**, a well-established complication of chronic hepatitis C caused by hepatic uroporphyrinogen decarboxylase deficiency
- The positive **Hepatitis C antibody** indicates exposure to HCV, but does not distinguish between acute, chronic, or resolved infection
- **PCR for viral RNA (HCV RNA)** is required to confirm **active viral replication** and diagnose current hepatitis C infection, which is crucial for treatment decisions
- The elevated glucose (170 mg/dL) may also represent hepatogenous diabetes related to chronic liver disease
*Incorrect: PCR for viral DNA*
- This test is primarily used for diagnosing active infections caused by **DNA viruses**, such as **hepatitis B** (HBV DNA) or cytomegalovirus
- The patient's hepatitis B serology indicates **past infection with immunity** (HBsAg negative, HBsAb positive, HBcAb positive), so HBV DNA testing is not indicated
- The clinical picture points toward HCV (an RNA virus), not a DNA virus
*Incorrect: Western blot for HIV*
- While the patient has a history of intravenous drug use (a risk factor for HIV), initial HIV screening is done with a **fourth-generation antigen/antibody combination assay**, not Western blot
- **Western blot** is a confirmatory test used only when initial HIV screening tests are reactive
- HIV testing may be appropriate given her risk factors, but it does not address the most pressing concern of active hepatitis C infection with complications (PCT)
*Incorrect: Serology for anti-HAV IgM*
- **Anti-HAV IgM** indicates **acute hepatitis A infection**, typically transmitted via the fecal-oral route
- The patient's symptoms, risk factors (IV drug use), positive HCV antibody, and characteristic skin findings (PCT) are not consistent with hepatitis A as the primary diagnosis
- Hepatitis A would not explain the chronic nature of symptoms or the skin manifestations
*Incorrect: Liver biopsy*
- **Liver biopsy** is an invasive procedure used to assess the **extent of liver damage**, inflammation, and fibrosis/cirrhosis after diagnosis of liver disease has been established
- It is not the most appropriate initial step to confirm **active viral replication**; PCR for HCV RNA should be performed first to establish that there is ongoing infection
- Once active HCV is confirmed, non-invasive methods (e.g., FibroScan, serum markers) are often preferred over biopsy for staging liver fibrosis
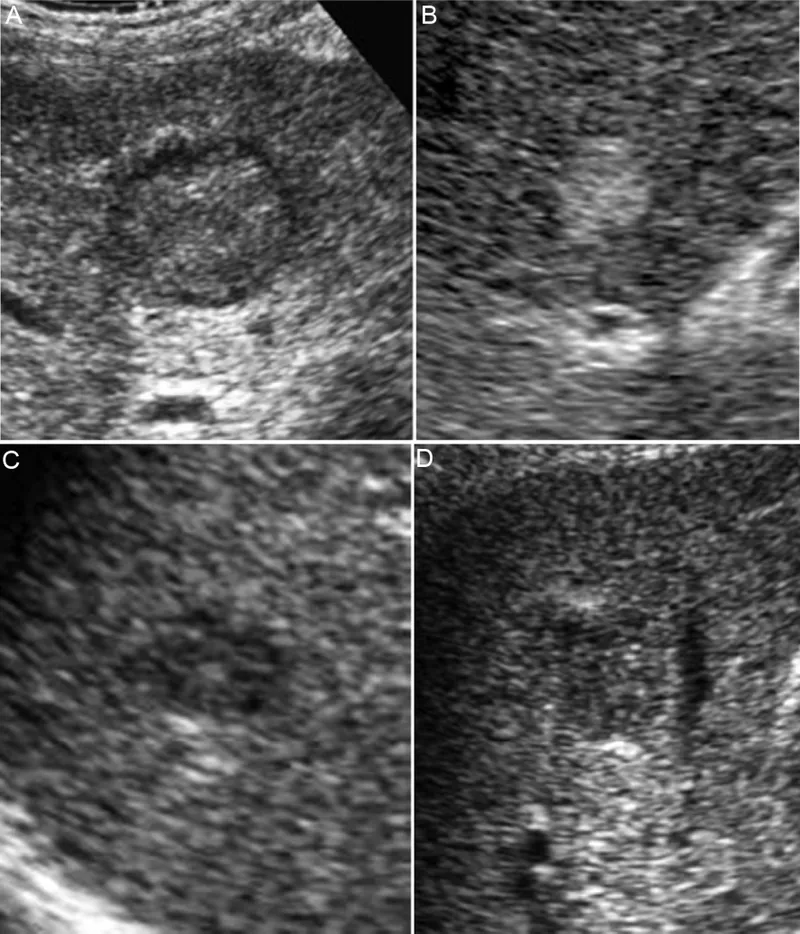
Hepatitis C and hepatocellular carcinoma US Medical PG Question 3: A 56-year-old African American presents to the emergency department due to abdominal pain, fatigue, and weight loss over the past 3 months. He has a long-standing history of chronic hepatitis B virus infection complicated by cirrhosis. On examination, he has jaundice, leg edema, and a palpable mass in the right upper abdominal quadrant. Abdominal ultrasound shows a 3-cm liver mass with poorly defined margins and coarse, irregular internal echoes. Lab results are shown:
Aspartate aminotransferase (AST) 90 U/L
Alanine aminotransferase (ALT) 50 U/L
Total bilirubin 2 mg/dL
Albumin 3 g/dL
Alkaline phosphatase 100 U/L
Alpha-fetoprotein 600 ng/mL
Which of the following is a feature of this patient's condition?
- A. It arises from the bile duct epithelium
- B. Daughter cysts are usually present on abdominal ultrasound
- C. Liver biopsy is required for diagnosis in a majority of patients
- D. It arises from hepatocytes (Correct Answer)
- E. Doppler blood flow shows venous pattern
Hepatitis C and hepatocellular carcinoma Explanation: ***It arises from hepatocytes***
- This patient's clinical presentation, including chronic **hepatitis B** with **cirrhosis**, an abdominal mass, and significantly elevated **alpha-fetoprotein (AFP)**, strongly indicates **hepatocellular carcinoma (HCC)**.
- HCC is a primary liver cancer that originates from the **hepatocytes**, the main functional cells of the liver.
*It arises from the bile duct epithelium*
- This describes **cholangiocarcinoma**, which arises from the **bile duct cells**.
- While cholangiocarcinoma is a primary liver cancer, its risk factors, imaging features, and tumor markers (e.g., **CA 19-9**) typically differ from those seen in this patient, and **AFP** elevation is not characteristic.
*Daughter cysts are usually present on abdominal ultrasound*
- **Daughter cysts** on ultrasound are characteristic of **hydatid cysts**, typically caused by **Echinococcus granulosus** infection.
- This parasitic condition presents differently, and the patient's elevated **AFP** and history of **cirrhosis** are not associated with hydatid disease.
*Liver biopsy is required for diagnosis in a majority of patients*
- In patients with **cirrhosis** and a lesion larger than 1 cm with characteristic imaging findings **(e.g., contrast enhancement on MRI/CT)**, along with a high **alpha-fetoprotein (AFP)** level, a biopsy is often **not required** for the diagnosis of HCC, as per standard guidelines.
- The combination of risk factors (cirrhosis, chronic HBV), elevated AFP, and imaging findings is sufficient for diagnosis in many cases, especially to avoid biopsy-related risks like bleeding or tumor seeding.
*Doppler blood flow shows venous pattern*
- **Hepatocellular carcinoma** typically exhibits a **hypervascular arterial enhancement pattern** on imaging with **early washout** in the venous phase.
- This is a key diagnostic feature, and flow showing a venous pattern would be inconsistent with HCC.
Hepatitis C and hepatocellular carcinoma US Medical PG Question 4: A 47-year-old woman comes to the physician because of a 3-week history of generalized fatigue, mild fever, abdominal pain, and nausea. She attended the state fair over a month ago, where she tried a number of regional foods, and wonders if it might have been caused by something she ate. She has also noticed darkening of her urine, which she attributes to not drinking enough water recently. She has type 2 diabetes mellitus. She drinks 1–2 beers daily. She works as nursing assistant in a rehabilitation facility. Current medications include glyburide, sitagliptin, and a multivitamin. She appears tired. Her temperature is 38.1°C (100.6°F), pulse is 99/min, and blood pressure is 110/74 mm Hg. Examination shows mild scleral icterus. The liver is palpated 2–3 cm below the right costal margin and is tender. Laboratory studies show:
Hemoglobin 10.6 g/dL
Leukocyte count 11600/mm3
Platelet count 221,000/mm3
Serum
Urea nitrogen 26 mg/dL
Glucose 122 mg/dL
Creatinine 1.3 mg/dL
Bilirubin 3.6 mg/dL
Total 3.6 mg/dL
Direct 2.4 mg/dL
Alkaline phosphatase 72 U/L
AST 488 U/L
ALT 798 U/L
Hepatitis A IgG antibody (HAV-IgG) positive
Hepatitis B surface antigen (HBsAg) positive
Hepatitis B core IgG antibody (anti-HBc) positive
Hepatitis B envelope antigen (HBeAg) positive
Hepatitis C antibody (anti-HCV) negative
Which of the following is the most likely diagnosis?
- A. Acute hepatitis B infection
- B. Resolved acute hepatitis B infection
- C. Active chronic hepatitis B infection (Correct Answer)
- D. Alcoholic hepatitis
- E. Inactive chronic hepatitis B infection
Hepatitis C and hepatocellular carcinoma Explanation: ***Active chronic hepatitis B infection***
- The presence of **HBsAg positive**, **anti-HBc IgG positive** (not IgM), and **HBeAg positive** indicates chronic hepatitis B infection with active viral replication.
- The key distinguishing feature is **anti-HBc IgG** rather than anti-HBc IgM. In acute hepatitis B, **anti-HBc IgM** would be positive, whereas **anti-HBc IgG** indicates infection that occurred more than 6 months ago (chronic infection).
- The **HBeAg positivity** indicates active viral replication and high infectivity, making this an "active" chronic infection rather than an inactive carrier state.
- The markedly elevated **AST (488 U/L)** and **ALT (798 U/L)** levels indicate significant hepatocellular damage with active inflammation.
- Clinical features of **scleral icterus**, **dark urine** (conjugated hyperbilirubinemia), **fever**, **fatigue**, and **abdominal pain** are consistent with active hepatitis.
*Acute hepatitis B infection*
- This is ruled out by the presence of **anti-HBc IgG** rather than **anti-HBc IgM**.
- In acute hepatitis B infection, **anti-HBc IgM** (the IgM class antibody to core antigen) would be positive, indicating recent infection.
- The presence of IgG class antibody indicates the infection occurred more than 6 months ago, establishing chronicity.
*Resolved acute hepatitis B infection*
- In resolved infection, **HBsAg** would be negative, and **anti-HBs** (Hepatitis B surface antibody) would be positive, indicating immunity.
- This patient is **HBsAg positive**, ruling out resolved infection.
- Resolved infection would not cause the current hepatocellular injury.
*Alcoholic hepatitis*
- Although the patient drinks 1-2 beers daily (modest consumption), the **AST:ALT ratio** (488:798 = 0.61) is less than 2:1.
- In alcoholic hepatitis, the AST:ALT ratio is typically **>2:1** due to alcohol-induced pyridoxine deficiency affecting ALT more than AST.
- The specific **viral serology markers** (positive HBsAg, HBeAg, and anti-HBc IgG) definitively establish hepatitis B as the cause of liver inflammation.
*Inactive chronic hepatitis B infection*
- In inactive chronic hepatitis B (also called inactive carrier state), **HBsAg** would be positive, but **HBeAg** would be negative with positive **anti-HBe** antibody.
- **ALT levels** are typically normal or minimally elevated (<40-50 U/L) in inactive carriers, not markedly elevated as in this case (ALT 798 U/L).
- The positive **HBeAg** and significantly elevated transaminases indicate active viral replication and inflammation, not an inactive state.
Hepatitis C and hepatocellular carcinoma US Medical PG Question 5: A previously healthy 48-year-old man comes to the physician because of a 2-month history of weight loss and yellowing of the skin. He works as a farmer and cultivates soybean and corn. He does not smoke, drink alcohol, or use illicit drugs. His vital signs are within normal limits. Physical examination shows scleral icterus and tender hepatomegaly. Ultrasonography of the abdomen shows a 5-cm nodular lesion in the right lobe of the liver. Further evaluation of the lesion confirms hepatocellular carcinoma. The activity of which of the following enzymes most likely contributed to the pathogenesis of this patient's condition?
- A. Cytochrome P450 monooxygenases (Correct Answer)
- B. Nuclear glycosylases
- C. Lysosomal serine proteases
- D. Cytosolic cysteine proteases
- E. Peroxisomal catalases
Hepatitis C and hepatocellular carcinoma Explanation: ***Cytochrome P450 monooxygenases***
- This patient, a farmer exposed to agricultural products like soybean and corn, likely developed **hepatocellular carcinoma** due to exposure to **aflatoxins**, which are common contaminants of these crops.
- **Aflatoxins** are metabolized by **hepatic cytochrome P450 monooxygenases** into highly reactive **epoxide intermediates**, which can bind to DNA and cause mutations, leading to cancer.
*Nuclear glycosylases*
- **Nuclear glycosylases** are involved in **DNA repair**, specifically in the base excision repair pathway, removing damaged or incorrect bases from DNA.
- While important for maintaining genomic integrity, their activity is not typically implicated in the initial formation of carcinogenic metabolites like those from aflatoxins.
*Lysosomal serine proteases*
- **Lysosomal serine proteases** are involved in protein degradation within lysosomes and are not directly involved in the metabolic activation of procarcinogens or the initial steps of DNA damage leading to hepatocellular carcinoma.
- Their primary role is in cellular waste management and nutrient recycling.
*Cytosolic cysteine proteases*
- **Cytosolic cysteine proteases**, such as calpains and caspases, are crucial for various cellular processes including apoptosis, but they do not typically play a direct role in the metabolic activation of procarcinogens or the genotoxic events leading to chemical-induced liver cancer.
- Their functions are generally related to protein turnover and cell signaling.
*Peroxisomal catalases*
- **Peroxisomal catalases** are enzymes primarily responsible for decomposing **hydrogen peroxide** into water and oxygen, protecting the cell from oxidative damage.
- While managing reactive oxygen species is vital, catalases are not involved in the metabolic activation of procarcinogens like aflatoxins; their role is more in detoxification of harmful byproducts.
Hepatitis C and hepatocellular carcinoma US Medical PG Question 6: An investigator is studying the rate of multiplication of hepatitis C virus in hepatocytes. The viral genomic material is isolated, enzymatically cleaved into smaller fragments and then separated on a formaldehyde agarose gel membrane. Targeted probes are then applied to the gel and visualized under x-ray. Which of the following is the most likely structure being identified by this test?
- A. Lipid-linked oligosaccharides
- B. Transcription factors
- C. Polypeptides
- D. Ribonucleic acids (Correct Answer)
- E. Deoxyribonucleic acids
Hepatitis C and hepatocellular carcinoma Explanation: ***Ribonucleic acids***
- The description of isolating "viral genomic material," which is then "enzymatically cleaved" and run on a "formaldehyde agarose gel," followed by the application of "targeted probes" and X-ray visualization, perfectly matches the technique of **Northern blotting**.
- Northern blotting is used to detect and quantify specific **RNA sequences**, which is consistent with the hepatitis C virus being an RNA virus.
*Lipid-linked oligosaccharides*
- These molecules are involved in protein glycosylation and are typically analyzed using techniques like **mass spectrometry** or **chromatography**, not Northern blotting.
- They are not nucleic acid material, which is implied by "viral genomic material" and enzymatic cleavage steps.
*Transcription factors*
- **Transcription factors** are proteins that regulate gene expression and would typically be identified using techniques like **Western blotting** (for protein detection) or Electrophoretic Mobility Shift Assay (EMSA) for DNA binding.
- They are not directly "genomic material" that would be cleaved and run on an agarose gel in this manner.
*Polypeptides*
- **Polypeptides** are chains of amino acids, i.e., proteins, which are normally detected using **Western blotting** after separation on an SDS-PAGE gel.
- The use of "formaldehyde agarose gel" and "enzymatic cleavage" points specifically to nucleic acid analysis, not protein analysis.
*Deoxyribonucleic acids*
- While DNA is genomic material and is often analyzed similarly, the use of a **formaldehyde agarose gel** is characteristic of RNA electrophoresis because formaldehyde prevents RNA from forming secondary structures.
- Furthermore, hepatitis C is a **single-stranded RNA virus**, meaning its genome is RNA, not DNA.
Hepatitis C and hepatocellular carcinoma US Medical PG Question 7: A 42-year-old male with a history significant for IV drug use comes to the emergency department complaining of persistent fatigue and malaise for the past three weeks. On physical exam, you observe a lethargic male with icteric sclera and hepatomegaly. AST and ALT are elevated at 600 and 750, respectively. HCV RNA is positive. Albumin is 3.8 g/dL and PT is 12. A liver biopsy shows significant inflammation with bridging fibrosis. What is the current first-line treatment?
- A. Sofosbuvir/Velpatasvir (Correct Answer)
- B. Glecaprevir/Pibrentasvir
- C. Sofosbuvir/Ledipasvir
- D. Ribavirin monotherapy
- E. Interferon monotherapy
Hepatitis C and hepatocellular carcinoma Explanation: ***Sofosbuvir/Velpatasvir***
- This is a **pan-genotypic direct-acting antiviral (DAA)** combination that is highly effective for all HCV genotypes and is recommended as a **first-line regimen** by AASLD/IDSA guidelines.
- It is particularly appropriate for patients with **significant fibrosis or compensated cirrhosis**, as seen in this patient with bridging fibrosis on biopsy.
- The standard treatment duration is **12 weeks** for treatment-naive patients, with high sustained virologic response (SVR) rates exceeding 95%.
- It has a favorable safety profile and is effective regardless of baseline viral load or HCV genotype.
*Glecaprevir/Pibrentasvir*
- While this is also an excellent **pan-genotypic DAA** combination with high efficacy, it requires longer treatment duration (12-16 weeks) in patients with **significant fibrosis (F3)** or cirrhosis.
- It is **contraindicated in decompensated cirrhosis (Child-Pugh B/C)**, making sofosbuvir-based regimens more universally applicable for patients with advanced liver disease.
- The often-cited 8-week treatment advantage applies primarily to patients **without cirrhosis**, not to this patient with bridging fibrosis.
*Sofosbuvir/Ledipasvir*
- This combination is primarily effective for **HCV genotypes 1, 4, 5, and 6** but is not truly pan-genotypic like sofosbuvir/velpatasvir.
- It is an acceptable alternative for genotype 1 infection but has been largely superseded by newer pan-genotypic regimens that don't require genotype testing.
- Treatment duration is typically **12 weeks** for treatment-naive patients without cirrhosis.
*Ribavirin monotherapy*
- **Ribavirin** is a nucleoside analog with **minimal antiviral activity** against HCV when used as monotherapy.
- It is only used as an **adjunctive agent** in combination with DAAs in specific circumstances (e.g., treatment-experienced patients with cirrhosis).
- Major side effect is **hemolytic anemia**, requiring close monitoring.
*Interferon monotherapy*
- **Interferon-alpha** monotherapy has very **poor efficacy** for chronic HCV, with sustained virologic response (SVR) rates of only 10-20%.
- It is associated with significant side effects including flu-like symptoms, depression, and cytopenias, making it **poorly tolerated**.
- This regimen is now **obsolete** and has been replaced by highly effective and well-tolerated DAA combinations.
Hepatitis C and hepatocellular carcinoma US Medical PG Question 8: A 63-year-old man presents to his primary care physician because he has been having headaches and hearing loss. In addition, he says that he has been having difficulty opening his jaw to eat and recurrent middle ear infections. Physical exam reveals enlarged neck lymph nodes and a mass in the nasopharynx. Biopsy of the mass reveals undifferentiated squamous epithelial cells. The organism that is most likely associated with this patient's disease is also associated with which of the following disorders?
- A. Kaposi sarcoma
- B. Hepatocellular carcinoma
- C. Adult T-cell lymphoma
- D. Burkitt lymphoma (Correct Answer)
- E. Vulvar carcinoma
Hepatitis C and hepatocellular carcinoma Explanation: ***Burkitt lymphoma***
- The patient's symptoms (headaches, hearing loss, difficulty opening jaw, recurrent middle ear infections, nasopharyngeal mass, enlarged neck lymph nodes) and biopsy results (undifferentiated squamous epithelial cells) point to **nasopharyngeal carcinoma**.
- **Nasopharyngeal carcinoma** is strongly associated with the **Epstein-Barr virus (EBV)**. EBV is also a causative agent in **Burkitt lymphoma**.
*Kaposi sarcoma*
- **Kaposi sarcoma** is caused by **Human Herpesvirus 8 (HHV-8)**, not EBV.
- It typically presents as vascular skin lesions and can affect visceral organs, differing from the nasopharyngeal carcinoma described.
*Hepatocellular carcinoma*
- **Hepatocellular carcinoma** is primarily associated with **Hepatitis B virus (HBV)** and **Hepatitis C virus (HCV)** infection, as well as cirrhosis from other causes.
- There is no significant association between EBV and hepatocellular carcinoma.
*Adult T-cell lymphoma*
- **Adult T-cell lymphoma** is caused by the **Human T-lymphotropic virus type 1 (HTLV-1)**.
- This is a retrovirus distinct from EBV.
*Vulvar carcinoma*
- **Vulvar carcinoma** is most frequently associated with **Human Papillomavirus (HPV)** infection, especially high-risk strains like HPV 16 and 18.
- It is not typically linked to EBV.
Hepatitis C and hepatocellular carcinoma US Medical PG Question 9: A 30-year-old woman presents to the clinic because of fever, joint pain, and a rash on her lower extremities. She admits to intravenous drug use. Physical examination reveals palpable petechiae and purpura on her lower extremities. Laboratory results reveal a negative antinuclear antibody, positive rheumatoid factor, and positive serum cryoglobulins. Which of the following underlying conditions in this patient is responsible for these findings?
- A. Dermatomyositis
- B. Systemic lupus erythematosus (SLE)
- C. Hepatitis C infection (Correct Answer)
- D. HIV infection
- E. Hepatitis B infection
Hepatitis C and hepatocellular carcinoma Explanation: ***Hepatitis C infection***
- The combination of **intravenous drug use**, **fever**, **joint pain**, **palpable purpura**, **positive rheumatoid factor**, and **positive serum cryoglobulins** is highly suggestive of **mixed cryoglobulinemia**, which is most commonly associated with chronic **Hepatitis C virus (HCV) infection**.
- **Cryoglobulinemia** is a systemic vasculitis caused by immune complex deposition, a common extrahepatic manifestation of HCV.
*Dermatomyositis*
- Characterized by **proximal muscle weakness** and characteristic skin rashes (e.g., **Gottron's papules**, **heliotrope rash**), which are not described here.
- While dermatomyositis can be associated with inflammatory markers, it typically does not present with palpable purpura or positive cryoglobulins.
*Systemic lupus erythematosus (SLE)*
- While SLE can cause **fever**, **arthralgia**, and a **rash**, the patient's **negative antinuclear antibody (ANA)** makes SLE highly unlikely.
- **Cryoglobulinemia** is rare in SLE, and the specific finding of palpable purpura points away from typical SLE rashes.
*HIV infection*
- HIV can cause a variety of skin lesions and arthralgias, but **palpable purpura** and **mixed cryoglobulinemia** are not its primary or most common manifestations.
- While **rheumatoid factor** can be positive in HIV, the overall clinical picture strongly favors HCV-associated cryoglobulinemia.
*Hepatitis B infection*
- Hepatitis B can be associated with **vasculitis** (e.g., **polyarteritis nodosa**) and immune complex-mediated disease.
- However, **mixed cryoglobulinemia**, characterized by the specific combination of symptoms and laboratory findings presented, is overwhelmingly more associated with **Hepatitis C** than Hepatitis B.
Hepatitis C and hepatocellular carcinoma US Medical PG Question 10: A 48-year-old homeless male presents to the ED because he hasn’t felt well recently. He states that he has been feeling nauseous and extremely weak over the past few days. He has several previous admissions for alcohol intoxication and uses heroin occasionally. His temperature is 100.9°F (38.3°C), blood pressure is 127/89 mmHg, and pulse is 101/min. His physical examination is notable for palmar erythema, tender hepatomegaly, and gynecomastia. His laboratory findings are notable for:
AST: 170 U/L
ALT: 60 U/L
GGT: 400 (normal range: 0-45 U/L)
Alkaline phosphatase: 150 IU/L
Direct bilirubin: 0.2 mg/dL
Total bilirubin: 0.8 mg/dL
WBC: 10,500
Serum iron: 100 µg/dL
TIBC: 300 µg/dL (normal range: 250–370 µg/dL)
Serum acetaminophen screen: Negative
Serum AFP: 6 ng/mL (normal range: < 10ng/mL)
Which of the following is the most likely cause of this patient’s symptoms?
- A. Acute viral hepatitis
- B. Acute cholangitis
- C. Hereditary hemochromatosis
- D. Hepatocellular carcinoma
- E. Alcoholic hepatitis (Correct Answer)
Hepatitis C and hepatocellular carcinoma Explanation: ***Alcoholic hepatitis***
- The patient's history of **heavy alcohol use**, along with symptoms such as **nausea**, **weakness**, **palmar erythema**, **tender hepatomegaly**, and **gynecomastia**, strongly points to alcoholic hepatitis.
- Laboratory findings of **AST:ALT ratio > 2:1** (170:60), **elevated GGT** (400 U/L), and **mildly elevated WBC** are characteristic of alcoholic liver injury.
*Acute viral hepatitis*
- While acute viral hepatitis can cause similar symptoms and elevated transaminases, the **AST:ALT ratio being significantly greater than 1** (specifically >2) is highly suggestive of alcoholic liver disease, whereas viral hepatitis typically shows ALT > AST.
- The elevated GGT is also more indicative of chronic alcohol use rather than acute viral infection.
*Acute cholangitis*
- Acute cholangitis typically presents with **Charcot's triad** (fever, right upper quadrant pain, jaundice) or **Reynolds' pentad** (Charcot's triad plus altered mental status and hypotension), along with **elevated alkaline phosphatase** and **direct bilirubin**.
- This patient's symptoms do not align with a classic presentation of cholangitis, and his direct bilirubin is normal.
*Hereditary hemochromatosis*
- Hereditary hemochromatosis is characterized by **iron overload**, which would manifest as **elevated serum iron** and **transferrin saturation**, along with a **decreased TIBC**.
- This patient's serum iron is normal, and his TIBC is within the normal range, ruling out iron overload as the primary cause.
*Hepatocellular carcinoma*
- HCC is a form of **liver cancer** that often develops in the setting of chronic liver disease (e.g., cirrhosis). While his history of alcohol use puts him at risk for cirrhosis, his **alpha-fetoprotein (AFP)** level is normal.
- The acute presentation with elevated transaminases and inflammatory markers is more consistent with acute hepatitis rather than carcinoma, which typically presents insidiously.
More Hepatitis C and hepatocellular carcinoma US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.