Hepatitis B and hepatocellular carcinoma US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hepatitis B and hepatocellular carcinoma. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hepatitis B and hepatocellular carcinoma US Medical PG Question 1: A 29-year-old man comes to the physician for a routine health maintenance examination. He feels well. He works as a nurse at a local hospital in the city. Three days ago, he had a needlestick injury from a patient whose serology is positive for hepatitis B. He completed the 3-dose regimen of the hepatitis B vaccine 2 years ago. His other immunizations are up-to-date. He appears healthy. Physical examination shows no abnormalities. He is concerned about his risk of being infected with hepatitis B following his needlestick injury. Serum studies show negative results for hepatitis B surface antigen, hepatitis B surface antibody, and hepatitis C antibody. Which of the following is the most appropriate next step in management?
- A. Revaccinate with 3-dose regimen of hepatitis B vaccine
- B. Revaccinate with two doses of hepatitis B vaccine
- C. Administer hepatitis B immunoglobulin
- D. Administer hepatitis B immunoglobulin and 3-dose regimen of hepatitis B vaccine (Correct Answer)
- E. Administer hepatitis B immunoglobulin and single dose hepatitis B vaccine
Hepatitis B and hepatocellular carcinoma Explanation: ***Administer hepatitis B immunoglobulin and 3-dose regimen of hepatitis B vaccine***
- This patient had prior vaccination but current serology shows **negative HBsAb**, indicating **non-response** to the vaccine (failure to develop protective antibodies).
- Given exposure to a hepatitis B positive patient, immediate post-exposure prophylaxis with **HBIG** is crucial for passive immunity and immediate protection.
- A **complete 3-dose revaccination series** should be initiated simultaneously, as per **CDC/ACIP guidelines** for vaccine non-responders with occupational exposure [1].
- This provides both immediate passive protection (HBIG) and attempts to establish active immunity through revaccination [1].
*Revaccinate with 3-dose regimen of hepatitis B vaccine*
- While revaccination is necessary due to the non-response, starting a 3-dose regimen alone without **HBIG** would leave the patient vulnerable during the initial period before vaccine response develops.
- After high-risk exposure in a non-responder, both passive (HBIG) and active (vaccine) immunity are required.
*Revaccinate with two doses of hepatitis B vaccine*
- A 2-dose regimen is insufficient; the standard revaccination schedule for non-responders is **3 doses** at 0, 1, and 6 months [1].
- Additionally, this option lacks **HBIG** for immediate protection after the high-risk exposure.
*Administer hepatitis B immunoglobulin*
- **HBIG** alone provides immediate passive immunity, which is crucial given the recent exposure and the patient's non-immune status.
- However, offering only HBIG without initiating active immunization (vaccine series) would leave the patient unprotected once the passive immunity wanes (approximately 3-6 months).
- This approach fails to address the need for long-term protection through revaccination.
*Administer hepatitis B immunoglobulin and single dose hepatitis B vaccine*
- While HBIG is appropriate for immediate protection, giving only a **single dose** of vaccine is inadequate.
- Standard post-exposure management for vaccine non-responders requires initiating a **complete 3-dose revaccination series**, not just one dose [1].
- A single dose would not provide adequate long-term protection for this non-responder.
Hepatitis B and hepatocellular carcinoma US Medical PG Question 2: A 57-year-old man comes to the physician for a follow-up visit. Serum studies show:
AST 134 U/L
ALT 152 U/L
Hepatitis B surface antigen Positive
A photomicrograph of the microscopic findings of a liver biopsy is shown. These biopsy findings are most characteristic of which of the following types of inflammatory reactions?
- A. Malignant transformation
- B. Granulomatous inflammation
- C. Chronic inflammation (Correct Answer)
- D. Acute inflammation
- E. Ischemic necrosis
Hepatitis B and hepatocellular carcinoma Explanation: ***Chronic inflammation***
- The combination of **elevated AST/ALT** and **positive Hepatitis B surface antigen** indicates persistent liver damage due to a chronic viral infection.
- Liver **biopsy findings** in such cases typically reveal **lymphocytic infiltrates**, fibrosis, and ongoing hepatocellular injury, which are hallmarks of chronic inflammation.
*Malignant transformation*
- While chronic viral hepatitis can lead to **hepatocellular carcinoma**, the question describes inflammatory findings, not **neoplastic changes** like cellular atypia or uncontrolled proliferation.
- **Malignant transformation** would present with disorganized architectural patterns and significant cellular pleomorphism.
*Granulomatous inflammation*
- **Granulomatous inflammation** is characterized by aggregates of activated macrophages (epithelioid cells), often with giant cells, which are not the primary feature described in chronic viral hepatitis.
- This type of inflammation is typically seen in diseases like **tuberculosis**, sarcoidosis, or fungal infections, not usually in viral hepatitis.
*Acute inflammation*
- **Acute inflammation** would present with a predominance of **neutrophils**, pronounced edema, and rapid onset of symptoms.
- The elevated liver enzymes and positive HBsAg suggest ongoing, long-term inflammation, which is characteristic of a chronic process.
*Ischemic necrosis*
- **Ischemic necrosis** is caused by a lack of blood supply, leading to cell death, and would typically present with **coagulative necrosis** of hepatocytes with minimal inflammatory infiltrate in the early stages.
- The clinical picture of chronic hepatitis B infection does not primarily involve an acute ischemic event affecting the liver.
Hepatitis B and hepatocellular carcinoma US Medical PG Question 3: Researchers are investigating oncogenes, specifically the KRAS gene that is associated with colon, lung, and pancreatic cancer. They have established that the gain-of-function mutation in this gene increases the chance of cancer development. They are also working to advance the research further to study tumor suppressor genes. Which of the genes below is considered a tumor suppressor gene?
- A. Her2/neu
- B. BRAF
- C. BCL-2
- D. JAK2
- E. Rb (Correct Answer)
Hepatitis B and hepatocellular carcinoma Explanation: ***Rb***
- The **retinoblastoma (Rb)** gene is a classic example of a **tumor suppressor gene**. Its protein product, Rb, plays a critical role in regulating the **cell cycle** by preventing uncontrolled cell division.
- When **Rb is mutated or inactivated**, cells can divide without proper checks, leading to tumor formation, particularly in cases like retinoblastoma.
*Her2/neu*
- **Her2/neu** (also known as ERBB2) is an **oncogene** that encodes a receptor tyrosine kinase involved in cell growth and differentiation.
- Its overexpression or amplification is associated with certain cancers, notably **breast cancer**, but it is not a tumor suppressor.
*BRAF*
- **BRAF** is an **oncogene** that codes for a serine/threonine kinase involved in the RAS/MAPK signaling pathway, which regulates cell growth.
- **Gain-of-function mutations** in BRAF are frequently found in melanoma, thyroid cancer, and colorectal cancer, promoting uncontrolled cell proliferation.
*BCL-2*
- **BCL-2** is an **anti-apoptotic gene**, meaning it prevents programmed cell death. While its overexpression can contribute to cancer by allowing abnormal cells to survive, it is not classified as a tumor suppressor gene.
- Instead, BCL-2 is considered an **oncogene** because mutations or overexpression promote cell survival and inhibit apoptosis.
*JAK2*
- **JAK2** (Janus Kinase 2) is a **proto-oncogene** encoding a tyrosine kinase involved in cytokine receptor signaling, which regulates hematopoiesis.
- **Gain-of-function mutations**, such as JAK2 V617F, are frequently found in **myeloproliferative neoplasms** (e.g., polycythemia vera, essential thrombocythemia, myelofibrosis), leading to uncontrolled blood cell production.
Hepatitis B and hepatocellular carcinoma US Medical PG Question 4: A 52-year-old male patient with chronic alcoholism presents to an ambulatory medical clinic, where the hepatologist elects to perform comprehensive hepatitis B screening, in addition to several other screening and preventative measures. Given the following choices, which serologic marker, if positive, would indicate the patient’s immunity to the hepatitis B virus?
- A. HBeAb
- B. HBeAg
- C. HBsAb (Correct Answer)
- D. HBsAg
- E. HBcAb
Hepatitis B and hepatocellular carcinoma Explanation: ***HBsAb***
- A positive **HBsAb** (Hepatitis B surface antibody) indicates immunity to hepatitis B virus, either from successful **vaccination** or **recovery from past infection**.
- This antibody provides **protective immunity** against future HBV infection and is the definitive marker of immunity.
*HBeAb*
- **HBeAb** (Hepatitis B e antibody) indicates **seroconversion** from HBeAg during chronic HBV infection, suggesting lower viral replication.
- It does **not confer immunity** against the virus itself and only reflects a phase of chronic infection.
*HBeAg*
- **HBeAg** (Hepatitis B e antigen) indicates **active viral replication** with high infectivity during ongoing hepatitis B infection.
- Its presence signifies a **replicative phase** of infection and increased risk of transmission to others.
*HBsAg*
- **HBsAg** (Hepatitis B surface antigen) indicates **active hepatitis B infection**, whether acute or chronic.
- This antigen is the **first serologic marker** to appear following exposure and confirms presence of the virus.
*HBcAb*
- **HBcAb** (Hepatitis B core antibody) indicates **previous or current exposure** to hepatitis B virus.
- It does **not differentiate** between acute, chronic, or resolved infection and does not confer protective immunity.
Hepatitis B and hepatocellular carcinoma US Medical PG Question 5: A 28-year-old man presents to the office with complaints of malaise, anorexia, and vomiting for the past 2 weeks. He also says that his urine is dark. The past medical history is unremarkable. The temperature is 36.8°C (98.2°F), the pulse is 72/min, the blood pressure is 118/63 mm Hg, and the respiratory rate is 15/min. The physical examination reveals a slightly enlarged, tender liver. No edema or spider angiomata are noted. Laboratory testing showed the following:
HBsAg Positive
IgM anti-HBc < 1:1,000
Anti-HBs Negative
HBeAg Positive
Anti-HBe Negative
HBV DNA 2.65 × 10⁹ IU/L
Alpha-fetoprotein 125 ng/mL
What is the most likely cause of this patient's condition?
- A. Acute HBV infection
- B. Passive immunity
- C. Acute resolving infection
- D. Resolved HBV infection (innate immunity)
- E. Acute exacerbation of chronic HBV infection (Correct Answer)
Hepatitis B and hepatocellular carcinoma Explanation: ***Acute exacerbation of chronic HBV infection***
- The combination of **HBsAg positive** (indicating extant infection) and **IgM anti-HBc < 1:1,000** (a low titer consistent with chronic infection, not acute) points towards a pre-existing chronic hepatitis B infection.
- The elevated **HBV DNA (2.65 × 109 IU/L)**, along with clinical symptoms like malaise, anorexia, vomiting, dark urine, and a tender liver, suggests an **acute exacerbation** of this chronic condition.
*Acute HBV infection*
- An acute HBV infection would typically present with a **high titer of IgM anti-HBc** and often **HBeAg positive** initially, but this patient's low IgM anti-HBc titer rules out a new acute infection.
- While symptoms align with acute hepatitis, the serology (low IgM anti-HBc) is not characteristic of primary acute infection.
*Passive immunity*
- Passive immunity would be characterized by the presence of **Anti-HBs without HBsAg**, which is not seen here.
- This scenario usually occurs after receiving hepatitis B immunoglobulin or transplacental transfer of antibodies.
*Acute resolving infection*
- A resolving acute infection would typically show a **decrease in HBsAg** and the **presence of Anti-HBs**, neither of which are observed in this patient.
- The **high viral load (HBV DNA)** and persistent HBsAg also contradict a resolving infection.
*Resolved HBV infection (innate immunity)*
- A resolved HBV infection is defined by the **absence of HBsAg** and the **presence of Anti-HBs**, along with anti-HBc.
- This patient still has **HBsAg present** and **Anti-HBs negative**, ruling out a resolved infection.
Hepatitis B and hepatocellular carcinoma US Medical PG Question 6: A 34-year-old woman, gravida 2, para 0, at 28 weeks' gestation comes to the physician for a prenatal visit. She has not had regular prenatal care. Her most recent ultrasound at 20 weeks of gestation confirmed accurate fetal dates and appropriate fetal development. She takes levothyroxine for hypothyroidism. She used to work as a nurse before she emigrated from Brazil 13 years ago. She lost her immunization records during the move and cannot recall all of her vaccinations. She appears well. Vital signs are within normal limits. Physical examination shows a fundal height of 26 cm and no abnormalities. An ELISA test for HIV is negative. Serology testing shows hepatitis B surface antibody positive, hepatitis B core antibody and surface antigen negative, and hepatitis A antibody negative. Hepatitis C antibody is positive with detectable RNA. Given her incomplete vaccination history and current serologic results, which of the following vaccinations is most appropriate to recommend at this time?
- A. Undergo liver biopsy
- B. Schedule a cesarean delivery
- C. Start combination therapy with interferon α and ribavirin
- D. Counsel about transmission risks and plan postpartum treatment
- E. Hepatitis A vaccination (Correct Answer)
Hepatitis B and hepatocellular carcinoma Explanation: ***Hepatitis A vaccination***
- The patient has no prior immunity to **Hepatitis A**, as indicated by the **negative Hepatitis A antibody** serology.
- Vaccination against **Hepatitis A** is crucial in this patient, especially given her increased risk of exposure due to being a former healthcare worker and a positive hepatitis C infection.
*Undergo liver biopsy*
- A **liver biopsy** is an invasive procedure and is generally not recommended during pregnancy, especially when other diagnostic or management strategies are available.
- While it can assess the degree of liver damage, it is usually reserved for specific indications and is not the most appropriate immediate step for vaccine recommendation.
*Schedule a cesarean delivery*
- **Hepatitis C viral transmission** to the fetus is primarily vertical during birth, but a **cesarean delivery** has not been shown to significantly reduce this risk compared to vaginal delivery.
- The decision regarding delivery method is typically made based on obstetric indications rather than solely for Hepatitis C prevention.
*Start combination therapy with interferon α and ribavirin*
- **Interferon α** and **ribavirin** are contraindicated during pregnancy due to their **teratogenic effects** and severe side effects.
- Antiviral treatment for Hepatitis C is generally deferred until **postpartum**.
*Counsel about transmission risks and plan postpartum treatment*
- While counseling about **transmission risks** and planning **postpartum treatment** for Hepatitis C is essential, it addresses the existing Hepatitis C infection rather than prescribing a vaccination, which is the direct question.
- It is an important part of comprehensive care for this patient but not the most appropriate *vaccination* recommendation.
Hepatitis B and hepatocellular carcinoma US Medical PG Question 7: A previously healthy 48-year-old man comes to the physician because of a 2-month history of weight loss and yellowing of the skin. He works as a farmer and cultivates soybean and corn. He does not smoke, drink alcohol, or use illicit drugs. His vital signs are within normal limits. Physical examination shows scleral icterus and tender hepatomegaly. Ultrasonography of the abdomen shows a 5-cm nodular lesion in the right lobe of the liver. Further evaluation of the lesion confirms hepatocellular carcinoma. The activity of which of the following enzymes most likely contributed to the pathogenesis of this patient's condition?
- A. Cytochrome P450 monooxygenases (Correct Answer)
- B. Nuclear glycosylases
- C. Lysosomal serine proteases
- D. Cytosolic cysteine proteases
- E. Peroxisomal catalases
Hepatitis B and hepatocellular carcinoma Explanation: ***Cytochrome P450 monooxygenases***
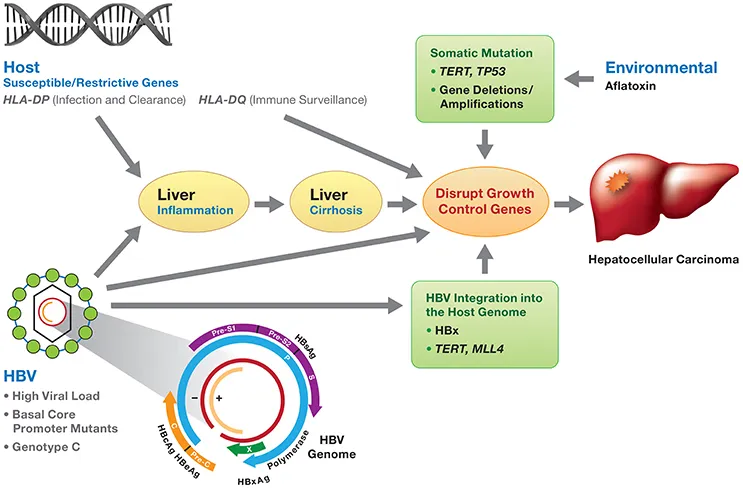
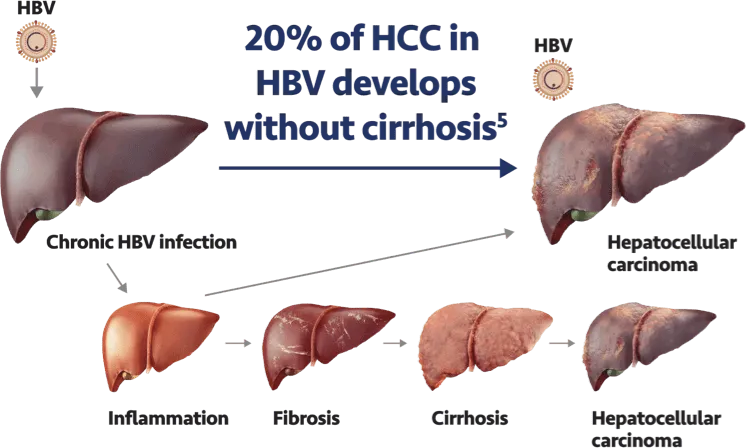
- This patient, a farmer exposed to agricultural products like soybean and corn, likely developed **hepatocellular carcinoma** due to exposure to **aflatoxins**, which are common contaminants of these crops.
- **Aflatoxins** are metabolized by **hepatic cytochrome P450 monooxygenases** into highly reactive **epoxide intermediates**, which can bind to DNA and cause mutations, leading to cancer.
*Nuclear glycosylases*
- **Nuclear glycosylases** are involved in **DNA repair**, specifically in the base excision repair pathway, removing damaged or incorrect bases from DNA.
- While important for maintaining genomic integrity, their activity is not typically implicated in the initial formation of carcinogenic metabolites like those from aflatoxins.
*Lysosomal serine proteases*
- **Lysosomal serine proteases** are involved in protein degradation within lysosomes and are not directly involved in the metabolic activation of procarcinogens or the initial steps of DNA damage leading to hepatocellular carcinoma.
- Their primary role is in cellular waste management and nutrient recycling.
*Cytosolic cysteine proteases*
- **Cytosolic cysteine proteases**, such as calpains and caspases, are crucial for various cellular processes including apoptosis, but they do not typically play a direct role in the metabolic activation of procarcinogens or the genotoxic events leading to chemical-induced liver cancer.
- Their functions are generally related to protein turnover and cell signaling.
*Peroxisomal catalases*
- **Peroxisomal catalases** are enzymes primarily responsible for decomposing **hydrogen peroxide** into water and oxygen, protecting the cell from oxidative damage.
- While managing reactive oxygen species is vital, catalases are not involved in the metabolic activation of procarcinogens like aflatoxins; their role is more in detoxification of harmful byproducts.
Hepatitis B and hepatocellular carcinoma US Medical PG Question 8: A 25-year-old man presents to the office for a 3-day history of fever and fatigue. Upon further questioning, he says that he also had constant muscular pain, headaches, and fever during these days. He adds additional information by giving a history of regular unprotected sexual relationship with multiple partners. He is a non-smoker and drinks alcohol occasionally. The heart rate is 102/min, respiratory rate is 18/min, temperature is 38.0°C (100.4°F), and blood pressure is 120/80 mm Hg. On physical examination, he is icteric and hepatosplenomegaly is evident with diffuse muscular and abdominal tenderness particularly in the right upper quadrant. The serologic markers show the following pattern:
Anti-HAV IgM negative
HBsAg positive
Anti-HBs negative
IgM anti-HBc positive
Anti-HCV negative
Anti-HDV negative
What is the most likely diagnosis?
- A. Viral hepatitis D
- B. Viral hepatitis C
- C. Viral hepatitis A
- D. Viral hepatitis E
- E. Viral hepatitis B (Correct Answer)
Hepatitis B and hepatocellular carcinoma Explanation: ***Viral hepatitis B***
- The combination of **HBsAg positive** and **IgM anti-HBc positive** indicates an **acute hepatitis B infection**.
- Symptoms like **fever**, **fatigue**, **muscular pain**, **icterus**, and **hepatosplenomegaly** are consistent with acute viral hepatitis.
*Viral hepatitis D*
- This is ruled out by the **negative Anti-HDV** marker, as hepatitis D requires co-infection with hepatitis B.
- While patients can be co-infected with HBV and HDV, the serology explicitly excludes HDV in this case.
*Viral hepatitis C*
- This is excluded by the **negative Anti-HCV** marker, which would be positive in hepatitis C infection.
- Though sexually transmitted, the serological markers point away from HCV.
*Viral hepatitis A*
- This is ruled out by the **negative Anti-HAV IgM** marker.
- Hepatitis A is typically transmitted via the **fecal-oral route**, which is less consistent with the patient's sexual history.
*Viral hepatitis E*
- While hepatitis E can cause acute hepatitis, it is typically diagnosed by **IgM anti-HEV** antibodies, which are not provided as positive here.
- Transmission is usually **fecal-oral**, which is not the primary risk factor suggested by the patient's history.
Hepatitis B and hepatocellular carcinoma US Medical PG Question 9: In a previous experiment infecting hepatocytes, it was shown that viable HDV virions were only produced in the presence of a co-infection with HBV. To better understand which HBV particle was necessary for the production of viable HDV virions, the scientist encoded in separate plasmids the various antigens/proteins of HBV and co-infected the hepatocytes with HDV. In which of the experiments would viable HDV virions be produced in conjunction with the appropriate HBV antigen/protein?
- A. HBV DNA polymerase
- B. HBV RNA polymerase
- C. HBsAg (Correct Answer)
- D. HBcAg
- E. HBeAg
Hepatitis B and hepatocellular carcinoma Explanation: ***HBsAg***
- **Hepatitis D virus (HDV)** is a **defective virus** that requires co-infection with **hepatitis B virus (HBV)** to complete its replication cycle.
- Specifically, HDV uses the **hepatitis B surface antigen (HBsAg)**, encoded by HBV, to form its **outer envelope** and assemble viable virions.
*HBV DNA polymerase*
- HBV DNA polymerase is essential for **HBV DNA replication**, converting the viral pregenomic RNA into DNA.
- It plays no direct role in the **packaging or formation of the HDV envelope**.
*HBV RNA polymerase*
- HBV, like other DNA viruses, utilizes the **host cell's RNA polymerase** for transcription of its RNA templates, not its own.
- HBV itself does not encode an RNA polymerase, and even if it did, it would not be relevant for HDV virion packaging.
*HBcAg*
- **Hepatitis B core antigen (HBcAg)** forms the **capsid** of the HBV virion, encapsulating the viral genome.
- While critical for HBV replication, it is **not incorporated into the HDV virion outer envelope**.
*HBeAg*
- **Hepatitis B e-antigen (HBeAg)** is a soluble protein derived from **HBcAg** that is secreted into the blood.
- It plays a role in **immune modulation** and is a marker of HBV replication but does not contribute to HDV virion assembly.
Hepatitis B and hepatocellular carcinoma US Medical PG Question 10: A 63-year-old man presents to his primary care physician because he has been having headaches and hearing loss. In addition, he says that he has been having difficulty opening his jaw to eat and recurrent middle ear infections. Physical exam reveals enlarged neck lymph nodes and a mass in the nasopharynx. Biopsy of the mass reveals undifferentiated squamous epithelial cells. The organism that is most likely associated with this patient's disease is also associated with which of the following disorders?
- A. Kaposi sarcoma
- B. Hepatocellular carcinoma
- C. Adult T-cell lymphoma
- D. Burkitt lymphoma (Correct Answer)
- E. Vulvar carcinoma
Hepatitis B and hepatocellular carcinoma Explanation: ***Burkitt lymphoma***
- The patient's symptoms (headaches, hearing loss, difficulty opening jaw, recurrent middle ear infections, nasopharyngeal mass, enlarged neck lymph nodes) and biopsy results (undifferentiated squamous epithelial cells) point to **nasopharyngeal carcinoma**.
- **Nasopharyngeal carcinoma** is strongly associated with the **Epstein-Barr virus (EBV)**. EBV is also a causative agent in **Burkitt lymphoma**.
*Kaposi sarcoma*
- **Kaposi sarcoma** is caused by **Human Herpesvirus 8 (HHV-8)**, not EBV.
- It typically presents as vascular skin lesions and can affect visceral organs, differing from the nasopharyngeal carcinoma described.
*Hepatocellular carcinoma*
- **Hepatocellular carcinoma** is primarily associated with **Hepatitis B virus (HBV)** and **Hepatitis C virus (HCV)** infection, as well as cirrhosis from other causes.
- There is no significant association between EBV and hepatocellular carcinoma.
*Adult T-cell lymphoma*
- **Adult T-cell lymphoma** is caused by the **Human T-lymphotropic virus type 1 (HTLV-1)**.
- This is a retrovirus distinct from EBV.
*Vulvar carcinoma*
- **Vulvar carcinoma** is most frequently associated with **Human Papillomavirus (HPV)** infection, especially high-risk strains like HPV 16 and 18.
- It is not typically linked to EBV.
More Hepatitis B and hepatocellular carcinoma US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.