Cancer prevention strategies for oncogenic viruses US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cancer prevention strategies for oncogenic viruses. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cancer prevention strategies for oncogenic viruses US Medical PG Question 1: A scientist is researching the long term effects of the hepatitis viruses on hepatic tissue. She finds that certain strains are oncogenic and increase the risk of hepatocellular carcinoma. However, they appear to do so via different mechanisms. Which of the following answer choices correctly pairs the hepatitis virus with the correct oncogenic process?
- A. Hepatitis A virus - chronic inflammation
- B. Hepatitis C virus - chronic inflammation
- C. Hepatitis E virus - integration of viral DNA into host hepatocyte genome
- D. Hepatitis B virus - integration of viral DNA into host hepatocyte genome (Correct Answer)
- E. Hepatitis A virus - integration of viral DNA into host hepatocyte genome
Cancer prevention strategies for oncogenic viruses Explanation: ***Hepatitis B virus - integration of viral DNA into host hepatocyte genome***
- **Hepatitis B virus (HBV)** is a **DNA virus** that can integrate its genetic material into the host hepatocyte genome, leading to genomic instability and promoting oncogenesis.
- This integration, along with chronic inflammation and the production of viral regulatory proteins, contributes significantly to the development of **hepatocellular carcinoma (HCC)**.
*Hepatitis A virus - chronic inflammation*
- **Hepatitis A virus (HAV)** is an **RNA virus** that causes **acute hepatitis** but does not lead to chronic infection or chronic inflammation.
- Due to its acute and self-limiting nature, HAV is **not associated with hepatocellular carcinoma**.
*Hepatitis C virus - integration of viral DNA into host hepatocyte genome*
- **Hepatitis C virus (HCV)** is an **RNA virus** and therefore does not integrate its DNA into the host genome (as it has no DNA phase).
- HCV causes HCC primarily through **chronic inflammation**, **fibrosis**, and **cirrhosis**, not DNA integration.
*Hepatitis E virus - integration of viral DNA into host hepatocyte genome*
- **Hepatitis E virus (HEV)** is an **RNA virus** that typically causes acute, self-limiting hepatitis and does not integrate its genetic material into the host genome.
- While HEV can cause chronic infection in immunocompromised individuals, it is **not generally recognized as an oncogenic virus** leading to HCC.
*Hepatitis A virus - integration of viral DNA into host hepatocyte genome*
- **Hepatitis A virus (HAV)** is an **RNA virus**, meaning it does not have a DNA stage and therefore cannot integrate DNA into the host genome.
- HAV causes **acute, self-limiting infections** and is definitively **not associated with hepatocellular carcinoma**.
Cancer prevention strategies for oncogenic viruses US Medical PG Question 2: A 31-year-old female presents to her gynecologist for a routine Pap smear. Her last Pap smear was three years ago and was normal. On the current Pap smear, she is found to have atypical squamous cells of unknown significance (ASCUS). Reflex HPV testing is positive. What is the best next step?
- A. Colposcopy (Correct Answer)
- B. Repeat Pap smear and HPV testing in 5 years
- C. Repeat Pap smear in 3 years
- D. Repeat Pap smear in 1 year
- E. Loop electrosurgical excision procedure (LEEP)
Cancer prevention strategies for oncogenic viruses Explanation: ***Colposcopy***
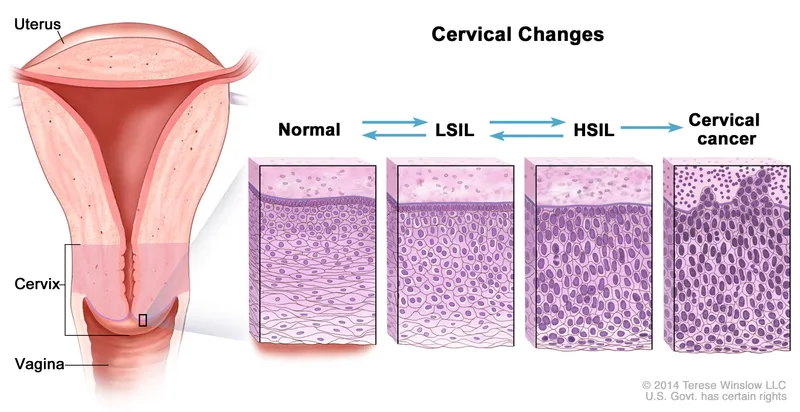
- A **colposcopy** is indicated for a patient over 25 with **atypical squamous cells of undetermined significance (ASCUS)** and a **positive high-risk human papillomavirus (HPV) test** to evaluate for cervical intraepithelial neoplasia (CIN).
- The positive HPV test suggests a higher risk of underlying cervical disease requiring direct visualization and potentially biopsy of abnormal areas.
*Repeat Pap smear and HPV testing in 5 years*
- This option is incorrect because a **positive HPV test** along with ASCUS indicates a need for more immediate and invasive evaluation than routine screening.
- Waiting five years could allow progression of potential **cervical dysplasia** without intervention.
*Repeat Pap smear in 3 years*
- This timeframe is typically for women aged 21-29 with a normal Pap smear and negative HPV, or for follow-up after low-grade abnormalities, not for ASCUS with positive HPV.
- The presence of **high-risk HPV** mandates a more aggressive follow-up strategy.
*Repeat Pap smear in 1 year*
- This might be an option for ASCUS with a **negative HPV test** or for adolescents, but it is insufficient when high-risk HPV is positive.
- A **high-risk HPV infection** following an ASCUS result requires colposcopy to rule out significant cervical lesions.
*Loop electrosurgical excision procedure (LEEP)*
- A **LEEP** is a therapeutic procedure used to remove abnormal cervical tissue, usually performed after a colposcopy and biopsy confirms a high-grade lesion (CIN 2 or 3).
- Performing a LEEP immediately without a preceding colposcopy and biopsy would be **premature** as the diagnosis of the severity of cervical changes is not yet confirmed.
Cancer prevention strategies for oncogenic viruses US Medical PG Question 3: A 20-year-old man who is a biology major presents to his physician for a simple check-up. He is informed that he hasn't received a hepatitis B vaccine. When the first injection is applied, the medical professional informs him that he will need to come back 2 more times on assigned days, since the vaccine is given in 3 doses. Which of the following antibodies is produced first in the college student as a result of the first vaccination?
- A. IgE
- B. IgG
- C. IgM (Correct Answer)
- D. IgD
- E. IgA
Cancer prevention strategies for oncogenic viruses Explanation: ***IgM***
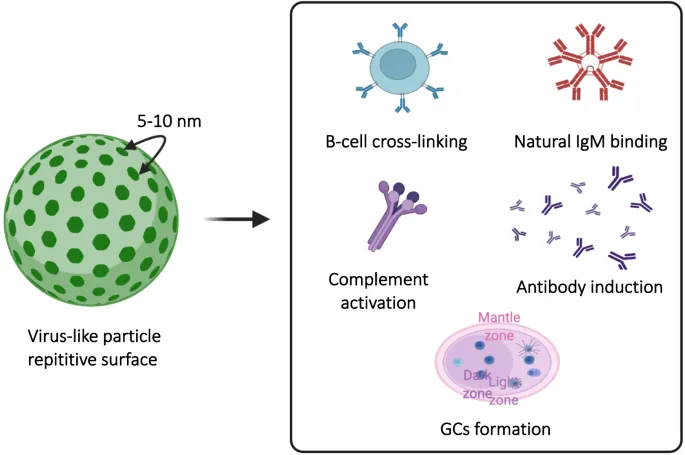
- Upon initial exposure to an antigen (like in the first vaccine dose), **IgM antibodies** are the first class to be produced and secreted by plasma cells.
- This **primary immune response** is characterized by a rapid, but short-lived, **IgM** peak.
*IgE*
- **IgE antibodies** are primarily involved in **allergic reactions** and defense against parasites, not the initial response to vaccination.
- Their production is typically triggered by exposure to specific allergens or parasites and mediated by Th2 helper T cells.
*IgG*
- **IgG antibodies** are the most abundant class in serum and are produced later in the primary response and predominantly during the **secondary immune response**.
- They provide **long-term immunity** and can cross the placenta, but are not the first antibody produced after initial antigen exposure.
*IgD*
- **IgD antibodies** are mainly found on the surface of **naive B cells** and act as B-cell receptors, playing a role in B-cell activation.
- They are not secreted in significant amounts into the serum and thus are not the first circulating antibody produced after vaccination.
*IgA*
- **IgA antibodies** are primarily found in **mucosal secretions** (e.g., saliva, tears, breast milk, gastrointestinal fluid) and play a key role in mucosal immunity.
- They are not the first antibody produced systemically in response to an initial vaccine exposure.
Cancer prevention strategies for oncogenic viruses US Medical PG Question 4: A 3255-g (7-lb) female newborn is delivered at term. Pregnancy and delivery were uncomplicated. On the day of her birth, she is given a routine childhood vaccine that contains a noninfectious glycoprotein. This vaccine will most likely help prevent infection by which of the following pathogens?
- A. Bordetella pertussis
- B. Rotavirus
- C. Poliovirus
- D. Haemophilus influenzae type b
- E. Hepatitis B virus (Correct Answer)
Cancer prevention strategies for oncogenic viruses Explanation: ***Hepatitis B virus***
- The **Hepatitis B vaccine** is routinely given at birth and contains a **noninfectious glycoprotein** (HBsAg) that elicits an immune response.
- This vaccine is crucial for preventing mother-to-child transmission and provides long-term protection against **Hepatitis B infection**.
*Bordetella pertussis*
- The vaccine for **Bordetella pertussis** (whooping cough) is part of the DTaP vaccine and is typically given at 2 months of age, not at birth.
- The DTaP vaccine usually contains **inactivated toxins** or acellular components, not solely a glycoprotein.
*Rotavirus*
- The **Rotavirus vaccine** is an **oral live-attenuated vaccine** administered in two or three doses, with the first dose typically given at 2 months of age.
- It does not contain a noninfectious glycoprotein.
*Poliovirus*
- The **Poliovirus vaccine** (IPV) is an **inactivated vaccine** given at 2 months of age, and the **oral poliovirus vaccine (OPV)** is a live-attenuated vaccine.
- Neither is routinely given at birth, nor described as a noninfectious glycoprotein.
*Haemophilus influenzae type b*
- The **Haemophilus influenzae type b (Hib) vaccine** is a polysaccharide-protein conjugate vaccine, first administered at 2 months of age.
- While it contains a protein component, it is not typically given at birth.
Cancer prevention strategies for oncogenic viruses US Medical PG Question 5: A 27-year-old woman comes to the physician for a routine health maintenance examination. She feels well. She had a chlamydia infection at the age of 22 years that was treated. Her only medication is an oral contraceptive. She has smoked one pack of cigarettes daily for 6 years. She has recently been sexually active with 3 male partners and uses condoms inconsistently. Her last Pap test was 4 years ago and results were normal. Physical examination shows no abnormalities. A Pap test shows atypical squamous cells of undetermined significance. Which of the following is the most appropriate next step in management?
- A. Repeat cytology in 6 months
- B. Perform laser ablation
- C. Perform loop electrosurgical excision procedure
- D. Perform HPV testing (Correct Answer)
- E. Perform cervical biopsy
Cancer prevention strategies for oncogenic viruses Explanation: ***Perform HPV testing***
- For women aged 25-29 with **Atypical Squamous Cells of Undetermined Significance (ASC-US)**, **HPV co-testing** is the preferred next step to risk-stratify for high-grade lesions.
- If **HPV is positive**, the patient should proceed to **colposcopy**; if HPV is negative, she can return to routine screening.
*Repeat cytology in 6 months*
- This approach is typically recommended for adolescents (age <21) with ASC-US or for women aged 21-24 where HPV testing is often not performed due to the high rate of transient HPV infections.
- For women aged ≥25 years with ASC-US, **reflex HPV testing** or **HPV co-testing** (if not done with the initial Pap) is generally preferred over repeat cytology alone.
*Perform laser ablation*
- **Laser ablation** is a treatment for **high-grade cervical intraepithelial neoplasia (CIN2/3)** identified after colposcopy and biopsy, not for initial ASC-US findings.
- Initiating a destructive procedure without further diagnostic evaluation would be premature and over-treatment for ASC-US.
*Perform loop electrosurgical excision procedure*
- **LEEP (loop electrosurgical excision procedure)** is a **diagnostic and therapeutic procedure** typically reserved for confirmed **high-grade CIN (CIN2 or CIN3)** or adenocarcinoma in situ.
- It is an invasive procedure and not appropriate as the initial management step for an ASC-US Pap result.
*Perform cervical biopsy*
- A **cervical biopsy** is performed during a **colposcopy** if abnormal areas are identified, usually following a positive HPV test or higher-grade abnormal cytology (e.g., LSIL, HSIL).
- ASC-US alone does not automatically warrant an immediate colposcopy and biopsy without prior **HPV risk stratification**.
Cancer prevention strategies for oncogenic viruses US Medical PG Question 6: A 17-year-old high school student presents to the physician’s office for a health maintenance examination. He is a recent immigrant from Venezuela and has no complaints at this time. Past medical history is significant for appendicitis at age 10, treated with an appendectomy. He denies the use of alcohol and cigarettes. He admits to occasionally smoking marijuana with his friends. He is sexually active with 1 woman partner and uses condoms inconsistently. The vital signs are within normal limits. Physical examination is unremarkable except for a laparoscopic surgical scar on the right iliac region. Routine blood tests are pending. What is the most appropriate next step in management?
- A. HPV vaccine (Correct Answer)
- B. Urine toxicology
- C. HPV vaccine as a legal adult at age 18
- D. Ceftriaxone and azithromycin as prophylaxis
- E. Azithromycin as prophylaxis only
Cancer prevention strategies for oncogenic viruses Explanation: ***HPV vaccine***
- The **Human Papillomavirus (HPV) vaccine** is recommended for all adolescents, regardless of sexual activity status, to provide protection against HPV-related cancers and genital warts.
- Given the patient's age and inconsistent use of condoms, vaccination is a **primary prevention strategy** against future HPV infection.
*Urine toxicology*
- While the patient admits to **occasional marijuana use**, a urine toxicology screen is not the most immediate or appropriate next step in management during a routine health maintenance exam, as it does not address a pressing health concern or immediate risk.
- Counseling on substance use and its risks would be more beneficial than a drug screen in this context.
*HPV vaccine as a legal adult at age 18*
- The **recommended age for HPV vaccination** is between 11 and 12 years, but it can be initiated as early as 9 years and given up to age 26 for those not adequately vaccinated.
- Delaying vaccination until age 18 would mean missing an opportunity for early protection and is not medically advisable given current guidelines.
*Ceftriaxone and azithromycin as prophylaxis*
- This combination is appropriate for the **treatment of gonorrhea and chlamydia infections**, respectively, but there is no indication for prophylactic antibiotic treatment in this patient.
- There are no symptoms of sexually transmitted infections (STIs), and a full workup for STIs should be conducted first if indicated based on risk factors, not prophylactic treatment.
*Azithromycin as prophylaxis only*
- **Azithromycin is used to treat chlamydia infections**, but like the combination therapy, there is no indication for prophylactic use in this patient.
- Prophylactic treatment with antibiotics is not a standard approach for preventing STIs without a confirmed exposure or infection.
Cancer prevention strategies for oncogenic viruses US Medical PG Question 7: A 16-year-old girl comes to her primary care physician for an annual check-up. She has no specific complaints. Her medical history is significant for asthma. She uses an albuterol inhaler as needed. She has no notable surgical history. Her mom had breast cancer and her grandfather died of colon cancer. She received all her childhood scheduled vaccinations up to age 8. She reports that she is doing well in school but hates math. She is sexually active with her boyfriend. They use condoms consistently, and they both tested negative recently for gonorrhea, chlamydia, syphilis and human immunodeficiency virus. She asks about birth control. In addition to educating the patient on her options for contraception, which of the following is the best next step in management?
- A. Cytology and human papilloma virus (HPV) testing now and then every 3 years
- B. No HPV-related screening as the patient is low risk
- C. No HPV-related screening and administer HPV vaccine (Correct Answer)
- D. Cytology and HPV testing now and then every 5 years
- E. Cytology now and then every 3 years
Cancer prevention strategies for oncogenic viruses Explanation: ***No HPV-related screening and administer HPV vaccine***
- Current guidelines from organizations like the **American College of Obstetricians and Gynecologists (ACOG)** recommend **HPV vaccination** for individuals aged 9 to 26 years, regardless of sexual activity.
- **Cervical cancer screening (Pap smears and HPV testing)** is not recommended for individuals under 21 years old, as HPV infections in this age group are highly likely to clear spontaneously.
*Cytology and human papilloma virus (HPV) testing now and then every 3 years*
- **Cervical cancer screening** with cytology and HPV testing is not recommended for individuals under **21 years old**, even if sexually active.
- Initiating screening now at age 16 would be **over-screening** and could lead to unnecessary procedures and anxiety given the high rate of spontaneous HPV clearance in adolescents.
*No HPV-related screening as the patient is low risk*
- While the patient is not yet indicated for cervical cancer screening, stating "no HPV-related screening as the patient is low risk" is incomplete. The patient is sexually active, putting her at risk for future HPV infection.
- The most appropriate action is to **offer the HPV vaccine** to prevent future infections, regardless of current screening guidelines.
*Cytology and HPV testing now and then every 5 years*
- This screening frequency (every 5 years) for co-testing is typically recommended for women **over 30 years old** with negative results, not for a 16-year-old.
- As with other screening options, initiating any cervical cancer screening at this age is **not recommended** by current guidelines.
*Cytology now and then every 3 years*
- This option refers to **cytology-only screening**, which is recommended every 3 years for individuals aged 21-29.
- Again, initiating any form of cervical cancer screening at **age 16 is not appropriate** according to current guidelines.
Cancer prevention strategies for oncogenic viruses US Medical PG Question 8: A previously healthy 53-year-old man is brought to the emergency department 45 minutes after the onset of a severe headache. He returned from a vacation in the mountains 4 days ago, during which he went swimming in a freshwater lake. On arrival, he is confused. His temperature is 39°C (102.2°F) and blood pressure is 105/68 mm Hg. Neurologic examination shows diffuse hyperreflexia. An MRI of the brain shows asymmetrical, bitemporal hyperintensities. A lumbar puncture is performed. Cerebrospinal fluid analysis shows:
Leukocyte count 120/mm3
Segmented neutrophils 10%
Lymphocytes 90%
Erythrocyte count 15/mm3
Glucose 45 mg/dL
Opening pressure 130 mm Hg
Protein 75 mg/dL
Which of the following is the most likely causal pathogen?
- A. Herpes simplex virus (Correct Answer)
- B. La Crosse virus
- C. Rabies virus
- D. Enterovirus
- E. Naegleria fowleri
Cancer prevention strategies for oncogenic viruses Explanation: ***Herpes simplex virus***
- The combination of **acute severe headache**, **fever**, **confusion**, **bitemporal hyperintensities** on MRI, and CSF showing a **lymphocytic pleocytosis** with some red blood cells (erythrocytes) is highly suggestive of **herpes simplex encephalitis (HSV encephalitis)**.
- HSV encephalitis characteristically causes **temporal lobe involvement**, leading to focal neurological deficits and neuropsychiatric symptoms, and CSF often has **lymphocytic predominance** with a slightly elevated protein.
*La Crosse virus*
- This virus causes **encephalitis** primarily in children and adolescents, often preceded by fever, headache, and nausea; seizures are common.
- While it can cause encephalitis, the **bitemporal hyperintensities** and specific CSF findings (lymphocytic pleocytosis, erythrocytes) are more classic for HSV.
*Rabies virus*
- Rabies presents as **encephalitis** with symptoms escalating from non-specific flu-like illness to neurological symptoms like hydrophobia, hallucinations, and paralysis.
- The patient's presentation with **acute severe headache** and rapid onset of confusion, without a history of animal bite, makes rabies less likely.
*Enterovirus*
- Enteroviruses are a common cause of **aseptic meningitis** and can cause **encephalitis**, especially in children.
- While they can cause fever, headache, and CSF lymphocytic pleocytosis, **bitemporal hyperintensities** and significant confusion pointing to focal neurological involvement are less characteristic.
*Naegleria fowleri*
- *Naegleria fowleri* causes **primary amoebic meningoencephalitis (PAM)**, typically in individuals with recent freshwater exposure, leading to rapid onset of severe headache, fever, and altered mental status.
- CSF analysis in PAM usually shows a **neutrophilic pleocytosis** rather than lymphocytic predominance, differentiating it from HSV encephalitis.
Cancer prevention strategies for oncogenic viruses US Medical PG Question 9: An investigator studying influenza virus variability isolates several distinct influenza virus strains from the respiratory secretions of a study subject. Mass spectrometry analysis of one strain shows that it expresses neuraminidase on its surface. Subsequent sequencing of this strain shows that its genome lacks the neuraminidase gene. Which of the following is the most likely explanation for this finding?
- A. Complementation
- B. Recombination
- C. Transduction
- D. Phenotypic mixing (Correct Answer)
- E. Reassortment
Cancer prevention strategies for oncogenic viruses Explanation: ***Phenotypic mixing***
- **Phenotypic mixing** occurs when a virus genome is packaged into a capsid or envelope proteins derived from a *different* but co-infecting virus. In this case, the influenza strain's genome lacks the **neuraminidase gene**, but it expresses neuraminidase on its surface because it acquired the protein from another co-infecting strain.
- This process is temporary, as the progeny of this mixed virus will replicate normally according to its own **genome**, and thus would not express neuraminidase unless it also inherited the gene.
*Complementation*
- **Complementation** occurs when two viruses infect the same cell, and one virus provides a **gene product** (a protein) that the other virus, which has a defective gene, needs to replicate.
- In complementation, the defective virus *replicates its own genome*, but uses the protein supplied by the other virus; it would not express a protein derived directly from another virus's genome on its surface if its own genome did not encode it.
*Recombination*
- **Recombination** involves the exchange of genetic material between two different but related viruses, resulting in a **hybrid genome** containing genes from both parental viruses.
- If recombination had occurred, the virus's genome *would* contain the neuraminidase gene, which is contradicted by the finding that the genome *lacks* it.
*Transduction*
- **Transduction** is a process where **bacteriophages** (viruses that infect bacteria) transfer bacterial DNA from one bacterium to another. This mechanism is specific to bacteria and their phages, and is not applicable to human influenza viruses.
- This process involves the transfer of genetic material between bacteria via a viral vector, which is unrelated to the expression of a surface protein from a *non-encoded gene* in influenza.
*Reassortment*
- **Reassortment** is a unique characteristic of viruses with **segmented genomes**, such as influenza, where segments can be exchanged between different strains during co-infection.
- If reassortment had occurred, the influenza strain's genome *would have acquired* the neuraminidase gene segment, which contradicts the finding that the genome *lacks* the neuraminidase gene.
Cancer prevention strategies for oncogenic viruses US Medical PG Question 10: A 30-year-old woman presents to the clinic because of fever, joint pain, and a rash on her lower extremities. She admits to intravenous drug use. Physical examination reveals palpable petechiae and purpura on her lower extremities. Laboratory results reveal a negative antinuclear antibody, positive rheumatoid factor, and positive serum cryoglobulins. Which of the following underlying conditions in this patient is responsible for these findings?
- A. Dermatomyositis
- B. Systemic lupus erythematosus (SLE)
- C. Hepatitis C infection (Correct Answer)
- D. HIV infection
- E. Hepatitis B infection
Cancer prevention strategies for oncogenic viruses Explanation: ***Hepatitis C infection***
- The combination of **intravenous drug use**, **fever**, **joint pain**, **palpable purpura**, **positive rheumatoid factor**, and **positive serum cryoglobulins** is highly suggestive of **mixed cryoglobulinemia**, which is most commonly associated with chronic **Hepatitis C virus (HCV) infection**.
- **Cryoglobulinemia** is a systemic vasculitis caused by immune complex deposition, a common extrahepatic manifestation of HCV.
*Dermatomyositis*
- Characterized by **proximal muscle weakness** and characteristic skin rashes (e.g., **Gottron's papules**, **heliotrope rash**), which are not described here.
- While dermatomyositis can be associated with inflammatory markers, it typically does not present with palpable purpura or positive cryoglobulins.
*Systemic lupus erythematosus (SLE)*
- While SLE can cause **fever**, **arthralgia**, and a **rash**, the patient's **negative antinuclear antibody (ANA)** makes SLE highly unlikely.
- **Cryoglobulinemia** is rare in SLE, and the specific finding of palpable purpura points away from typical SLE rashes.
*HIV infection*
- HIV can cause a variety of skin lesions and arthralgias, but **palpable purpura** and **mixed cryoglobulinemia** are not its primary or most common manifestations.
- While **rheumatoid factor** can be positive in HIV, the overall clinical picture strongly favors HCV-associated cryoglobulinemia.
*Hepatitis B infection*
- Hepatitis B can be associated with **vasculitis** (e.g., **polyarteritis nodosa**) and immune complex-mediated disease.
- However, **mixed cryoglobulinemia**, characterized by the specific combination of symptoms and laboratory findings presented, is overwhelmingly more associated with **Hepatitis C** than Hepatitis B.
More Cancer prevention strategies for oncogenic viruses US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.