Oncogenic viruses

On this page
🦠 Viral Oncogenesis Fundamentals: The Cellular Hijacking Blueprint
A handful of viruses have mastered a sinister trick: they don't just infect cells-they reprogram them toward cancer. You'll discover how these oncogenic viruses hijack cellular checkpoints, dismantle tumor suppressors, and leave diagnostic fingerprints that guide prevention and treatment. From the molecular sabotage of p53 and Rb to recognizing clinical patterns in hepatocellular carcinoma and cervical cancer, you'll build a complete framework connecting viral mechanisms to real-world cancer management and multi-system disease.
📌 Remember: VIRAL oncogenesis - Viral proteins, Immortalization, Regulatory bypass, Apoptosis resistance, Loss of tumor suppressors
The oncogenic virus arsenal includes 7 major families responsible for 15-20% of all human cancers worldwide. These pathogens have evolved sophisticated strategies to subvert cellular checkpoints, with DNA viruses typically integrating into host genomes and RNA retroviruses hijacking transcriptional machinery.
-
DNA Oncogenic Viruses
- Human Papillomavirus (HPV): >99% of cervical cancers, 150+ subtypes
- Epstein-Barr Virus (EBV): >90% of Burkitt lymphoma, 95% adult seroprevalence
- Hepatitis B Virus (HBV): 50-80% of hepatocellular carcinoma globally
- Integration sites: chromosome 17p, 11q, 1p most common
- Latency period: 20-30 years average from infection to cancer
- Human Herpesvirus 8 (HHV-8): 100% of Kaposi sarcoma cases
- Merkel Cell Polyomavirus: 80% of Merkel cell carcinomas
-
RNA Oncogenic Viruses
- Human T-lymphotropic Virus-1 (HTLV-1): 2-5% lifetime cancer risk
- Hepatitis C Virus (HCV): 25-30% of hepatocellular carcinoma
- Chronic infection rate: 75-85% of exposed individuals
- Cirrhosis development: 20% over 20 years
| Virus Family | Integration Pattern | Latency Period | Cancer Risk | Key Oncoproteins | Geographic Hotspots |
|---|---|---|---|---|---|
| HPV | Episomal → Integrated | 10-20 years | 0.1-15% | E6, E7 | Worldwide |
| EBV | Episomal maintenance | Variable | 0.001-40% | LMP1, EBNA1 | Africa, Asia |
| HBV | Random integration | 20-40 years | 5-25% | HBx, PreS/S | Asia, Africa |
| HHV-8 | Episomal latency | 5-15 years | 0.02-50% | LANA, vFLIP | Mediterranean, Africa |
| HTLV-1 | Proviral integration | 20-60 years | 2-5% | Tax, HBZ | Japan, Caribbean |
💡 Master This: Oncogenic viruses bypass p53 and Rb tumor suppressors through specific viral proteins - HPV E6 degrades p53 (t½ = 20 minutes vs normal 6 hours), while E7 inactivates Rb family proteins, creating the "perfect storm" for malignant transformation.
The transformation process follows a predictable 4-stage cascade: initial infection → persistent infection → dysplasia → invasive carcinoma. This timeline spans 10-40 years for most viral cancers, creating crucial intervention windows for prevention and early detection strategies.
Connect these foundational viral mechanisms through cellular pathway disruption to understand how specific oncoproteins orchestrate the transformation symphony.
🦠 Viral Oncogenesis Fundamentals: The Cellular Hijacking Blueprint
⚙️ Molecular Machinery Disruption: The Viral Sabotage Protocol
📌 Remember: CRASH pathway disruption - Cell cycle checkpoints, Repair mechanisms, Apoptosis resistance, Senescence bypass, Hypoxia adaptation
The viral transformation toolkit operates through 3 primary mechanisms: direct oncoprotein action, insertional mutagenesis, and chronic inflammation. DNA viruses predominantly use direct protein interference, while RNA viruses rely more heavily on insertional activation of cellular oncogenes.
-
p53 Pathway Sabotage
- HPV E6: Recruits E6AP ubiquitin ligase, degrading p53 in <30 minutes
- SV40 Large T: Binds p53 DNA-binding domain, blocking transcriptional activity
- EBV EBNA5: Inhibits p53 acetylation at lysine 373/382
- Normal p53 half-life: 6-8 hours in unstressed cells
- Viral-infected cells: <20 minutes p53 degradation
- Result: >95% reduction in p53-mediated apoptosis
-
Rb Pathway Disruption
- HPV E7: Binds Rb/p107/p130 family, releasing E2F transcription factors
- Adenovirus E1A: Mimics cyclin E/CDK2 phosphorylation pattern
- Polyomavirus Large T: Contains LXCXE motif for Rb binding
- Normal G1/S checkpoint: 12-24 hours duration
- Viral bypass: <2 hours forced S-phase entry
- Consequence: 10-fold increased DNA replication errors
| Viral Protein | Target Pathway | Mechanism | Binding Affinity | Functional Outcome | Cancer Association |
|---|---|---|---|---|---|
| HPV E6 | p53 degradation | E6AP recruitment | Kd = 50 nM | 95% p53 loss | Cervical, anal |
| HPV E7 | Rb inactivation | Direct binding | Kd = 100 nM | E2F release | Cervical, head/neck |
| EBV LMP1 | NF-κB activation | TRAF binding | Constitutive | Survival signals | Lymphomas |
| HBV HBx | p53 inhibition | Cytoplasmic sequestration | Variable | Apoptosis block | Hepatocellular |
| HTLV Tax | Multiple pathways | Transcriptional hijack | High affinity | Growth promotion | T-cell leukemia |
💡 Master This: The "two-hit hypothesis" applies differently to viral cancers - viral oncoproteins can simultaneously inactivate both alleles of tumor suppressors through protein-protein interactions, bypassing the need for sequential genetic mutations and accelerating transformation timelines.
Chronic viral infections create oxidative stress environments with >5-fold elevated reactive oxygen species, leading to 8-oxoguanine DNA lesions at rates of 10⁴-10⁵ per cell per day. This oxidative damage, combined with impaired DNA repair, generates the genomic instability necessary for malignant progression.
Connect these molecular disruption patterns through clinical recognition frameworks to understand how viral signatures manifest in patient presentations.
⚙️ Molecular Machinery Disruption: The Viral Sabotage Protocol
🎯 Clinical Pattern Recognition: The Viral Cancer Fingerprint
-
Demographic Pattern Recognition
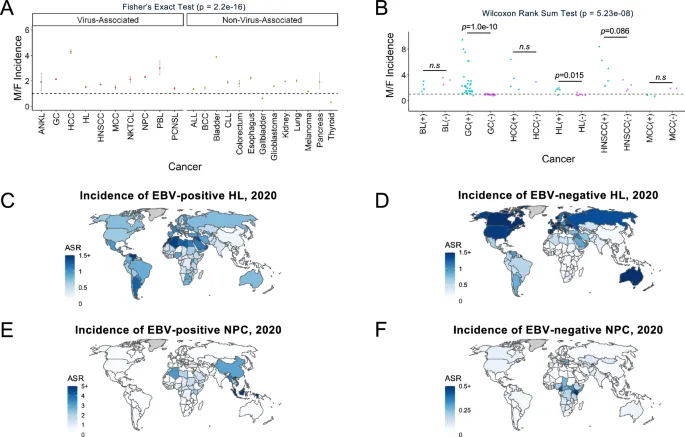
- Age-specific clustering: EBV lymphomas peak at <5 years and 15-25 years
- Geographic hotspots: Burkitt lymphoma 40-fold higher in equatorial Africa
- Gender predilections: Kaposi sarcoma 8:1 male predominance in HIV patients
- HPV cervical cancer: Peak incidence 35-44 years, 99.7% HPV-positive
- HBV hepatocellular carcinoma: 3:1 male predominance, 80% in Asia-Pacific
- HTLV-1 leukemia: 1.5:1 female predominance, >40 years typical onset
-
Anatomical Distribution Patterns
- HPV-associated cancers: Squamous epithelia preference
- Cervical: 83% of cases, predominantly transformation zone
- Anal: 95% HPV-positive, 80% in MSM population
- Oropharyngeal: 70% HPV-positive, tonsil/base of tongue predilection
- EBV lymphomas: B-cell compartments and epithelial sites
- Burkitt: Jaw involvement in 50% of endemic cases
- Hodgkin: Nodular sclerosis subtype, 30% EBV-positive
- Nasopharyngeal carcinoma: >95% EBV-positive, Southern Chinese predominance
- HPV-associated cancers: Squamous epithelia preference
📌 Remember: VIRAL cancer recognition - Very young or specific age, Immune compromised, Regional clustering, Anatomical predilection, Lymphoid involvement
The "see this, think viral" framework relies on pattern combinations rather than isolated findings. Multiple demographic and clinical factors create probability matrices that guide diagnostic workup and treatment selection.
| Cancer Type | Viral Association | Age Peak | Geographic Cluster | Histological Marker | 5-Year Survival |
|---|---|---|---|---|---|
| Cervical SCC | HPV 16/18 (70%) | 35-44 years | Worldwide | p16 overexpression | 92% (early) |
| Burkitt Lymphoma | EBV (95% endemic) | <10 years | Equatorial Africa | MYC translocation | 85% (pediatric) |
| Kaposi Sarcoma | HHV-8 (100%) | 30-50 years | Mediterranean/Africa | LANA expression | Variable |
| Hepatocellular | HBV (50-80%) | 50-70 years | Asia-Pacific | HBsAg positive | 18% (overall) |
| Nasopharyngeal | EBV (>95%) | 40-60 years | Southern China | EBER positive | 70% (early) |
- Histological Signature Recognition
- HPV cancers: p16 overexpression, koilocytic changes, basaloid morphology
- EBV lymphomas: Reed-Sternberg variants, EBER positivity, LMP1 expression
- HHV-8 tumors: Spindle cell morphology, slit-like vascular spaces, LANA nuclear dots
- Viral cytopathic effects: Multinucleation, nuclear inclusions, cellular gigantism
- Inflammatory patterns: Dense lymphocytic infiltrates, plasma cell predominance
- Vascular changes: Angiogenesis, endothelial proliferation, hemorrhage
💡 Master This: Viral cancers often present with better prognosis than viral-negative counterparts - HPV-positive oropharyngeal cancers have 60-80% better survival rates, while EBV-positive Hodgkin lymphoma shows superior treatment response compared to EBV-negative disease, reflecting enhanced immunogenicity.
The temporal progression patterns provide additional diagnostic clues. Viral cancers typically demonstrate accelerated growth phases following prolonged latency periods, creating "hockey stick" progression curves distinct from the gradual evolution of spontaneous malignancies.
Connect these recognition patterns through systematic diagnostic approaches to understand how clinical suspicion guides confirmatory testing strategies.
🎯 Clinical Pattern Recognition: The Viral Cancer Fingerprint
🔬 Diagnostic Precision: The Viral Detection Arsenal
-
HPV Detection Strategies
- Primary screening: Cobas HPV test detects 14 high-risk types with 95% sensitivity
- Genotyping: Linear Array identifies 37 HPV types including 16/18 specifically
- In-situ hybridization: INFORM HPV demonstrates viral integration patterns
- HPV DNA detection: 10-100 copies per cell threshold for positivity
- p16 immunostaining: >70% nuclear/cytoplasmic staining indicates transformation
- E6/E7 mRNA: APTIMA assay detects active viral transcription
-
EBV Diagnostic Panel
- EBER in-situ hybridization: Gold standard with >95% sensitivity
- LMP1 immunostaining: Positive in 40-60% of EBV-positive lymphomas
- EBNA1 detection: Indicates latent infection pattern
- Viral load quantification: >1000 copies/mL plasma suggests active disease
- IgG/IgM serology: VCA, EA, EBNA antibody patterns
- PCR sensitivity: <10 copies per reaction detection limit
📌 Remember: DETECT viral cancers - DNA/RNA testing, Enzyme immunoassays, Tissue morphology, Electron microscopy, Culture (rarely), Tumor markers
| Virus | Primary Detection | Sensitivity | Specificity | Turnaround Time | Cost Considerations |
|---|---|---|---|---|---|
| HPV | DNA PCR | 95-99% | 85-95% | 1-3 days | $50-150 |
| EBV | EBER ISH | >95% | >98% | 2-4 days | $75-200 |
| HBV | HBsAg/DNA | 99% | >99% | 2-6 hours | $25-100 |
| HCV | RNA PCR | >95% | >99% | 4-8 hours | $100-300 |
| HHV-8 | LANA IHC | 90-95% | >95% | 1-2 days | $100-250 |
- Quantitative Monitoring Strategies
- Real-time PCR: Dynamic range of 10¹-10⁹ copies/mL
- Digital droplet PCR: Absolute quantification without standard curves
- Next-generation sequencing: Viral integration mapping and mutation analysis
- HBV monitoring: Quarterly viral load assessment during treatment
- EBV surveillance: Monthly PCR in high-risk transplant patients
- HPV follow-up: Annual testing after treatment completion
💡 Master This: False-negative rates vary significantly by specimen type - cervical cytology HPV testing shows 5-10% false-negative rate, while tissue-based PCR reduces this to <2%, emphasizing the importance of appropriate specimen selection for accurate viral cancer diagnosis.
The integration status of viral DNA provides crucial prognostic information. Episomal viral DNA typically indicates reversible infection, while integrated viral sequences suggest irreversible transformation with higher malignant potential and reduced treatment responsiveness.
Connect these diagnostic precision tools through evidence-based treatment algorithms to understand how viral identification guides therapeutic decision-making.
🔬 Diagnostic Precision: The Viral Detection Arsenal
⚖️ Treatment Algorithm Mastery: The Viral Cancer Counteroffensive
📌 Remember: ATTACK viral cancers - Antivirals first, Targeted therapy, Tumor debulking, Adjuvant immunotherapy, Combination protocols, Keep monitoring
-
HPV-Associated Cancer Treatment
- Surgical management: Wide local excision with 1-2 cm margins
- Radiation therapy: 70 Gy in 35 fractions for definitive treatment
- Concurrent chemotherapy: Cisplatin 40 mg/m² weekly during radiation
- Complete response rates: 85-90% for early-stage disease
- 5-year survival: 92% stage I, 75% stage II, 45% stage III
- HPV-positive oropharyngeal: De-escalation trials reducing toxicity
-
EBV Lymphoma Protocols
- Rituximab-based regimens: R-CHOP for 6-8 cycles
- Antiviral integration: Ganciclovir during lytic reactivation
- Immunotherapy: Anti-CD20, anti-CD30 targeted approaches
- Burkitt lymphoma: >90% cure rate with intensive protocols
- Hodgkin lymphoma: 85% 10-year survival with ABVD
- Post-transplant lymphoproliferative: Rituximab monotherapy first-line
| Cancer Type | First-Line Treatment | Response Rate | Median Survival | Viral-Specific Therapy | Monitoring Schedule |
|---|---|---|---|---|---|
| HPV Cervical | Surgery + RT/Chemo | 85-90% | >10 years | None standard | Every 3-6 months |
| EBV Lymphoma | R-CHOP × 6 cycles | 80-95% | 8-10 years | Rituximab | Monthly during Rx |
| HBV Hepatocellular | Resection/Transplant | 60-80% | 3-5 years | Entecavir/Tenofovir | Every 3 months |
| Kaposi Sarcoma | HAART + Chemotherapy | 70-85% | 5-8 years | Antiretrovirals | Every 2-3 months |
| Merkel Cell | Surgery + RT | 65-75% | 2-3 years | None established | Every 3 months |
- Antiviral Integration Strategies
- HBV hepatocellular carcinoma: Entecavir 0.5 mg daily reduces recurrence risk by 40%
- EBV reactivation: Valganciclovir 900 mg BID during high-risk periods
- CMV co-infection: Ganciclovir 5 mg/kg BID prevents viral synergy
- Viral suppression targets: HBV <2000 IU/mL, EBV <1000 copies/mL
- Resistance monitoring: Quarterly genotypic testing during treatment
- Drug interactions: Significant CYP450 effects with cancer chemotherapy
💡 Master This: Timing of antiviral therapy critically impacts outcomes - initiating nucleoside analogs 2-4 weeks before cancer treatment prevents viral reactivation in >90% of HBV patients, while concurrent initiation reduces efficacy to 60-70% due to immune suppression.
The immunotherapy revolution has particular relevance for viral cancers. Checkpoint inhibitors show enhanced efficacy against virally-infected tumors due to increased neoantigen presentation and pre-existing immune activation, with response rates 20-30% higher than viral-negative counterparts.
- Novel Therapeutic Approaches
- CAR-T cell therapy: Anti-CD19 for EBV lymphomas
- Therapeutic vaccines: HPV E6/E7 peptide vaccines
- Adoptive cell transfer: EBV-specific CTLs for post-transplant disease
- Clinical trial enrollment: 30-40% of viral cancer patients eligible
- Response rates: 40-60% in refractory disease
- Toxicity profiles: Generally favorable compared to conventional chemotherapy
Connect these treatment algorithms through multi-system integration approaches to understand how viral cancers interact with host immunity and other malignancies.
⚖️ Treatment Algorithm Mastery: The Viral Cancer Counteroffensive
🔗 Multi-System Integration: The Viral-Host Ecosystem
-
Immune System Integration
- HLA associations: HLA-B*5701 confers 90% protection against HIV progression
- Cytokine networks: IL-10 overproduction promotes EBV persistence
- T-cell exhaustion: PD-1 upregulation in chronic viral infections
- CD8+ T-cell dysfunction: >70% express exhaustion markers in chronic HBV
- NK cell impairment: 50% reduced cytotoxicity in EBV-positive patients
- Regulatory T-cells: 2-3 fold increased in viral cancer microenvironments
-
Metabolic Reprogramming Networks
- Viral hijacking: HPV E7 enhances glycolysis by 40-60%
- Lipid metabolism: HBV HBx promotes fatty acid synthesis
- Amino acid depletion: EBV increases glutamine consumption by 3-fold
- Warburg effect enhancement: >80% of viral cancers show aerobic glycolysis
- Mitochondrial dysfunction: Complex I activity reduced by 30-50%
- Oxidative stress: ROS levels elevated 5-10 fold above normal
📌 Remember: SYSTEM integration - Susceptibility genes, Yield to immune dysfunction, Synergistic infections, Tumor microenvironment, Environmental factors, Metabolic reprogramming
The microbiome-viral-cancer axis represents an emerging frontier in understanding viral oncogenesis. Bacterial dysbiosis can enhance viral persistence, promote inflammation, and modulate immune responses in ways that significantly impact cancer development and treatment outcomes.
| System Component | Viral Impact | Cancer Risk Modifier | Therapeutic Target | Clinical Biomarker | Research Priority |
|---|---|---|---|---|---|
| Immune Function | Exhaustion/Dysfunction | 3-10 fold increase | Checkpoint inhibitors | PD-1, CTLA-4 | High |
| Metabolism | Glycolysis/Glutaminolysis | 2-5 fold increase | Metabolic inhibitors | Lactate, Glutamine | Medium |
| Microbiome | Dysbiosis patterns | 1.5-3 fold increase | Probiotics/FMT | 16S sequencing | High |
| Genetics | Susceptibility alleles | 2-20 fold increase | Gene therapy | HLA typing | Medium |
| Environment | Co-carcinogen exposure | 1.5-5 fold increase | Lifestyle modification | Exposure biomarkers | Low |
- Genetic Susceptibility Networks
- GWAS findings: >50 loci associated with viral cancer susceptibility
- HLA class I/II: Peptide presentation efficiency varies 100-fold
- Cytokine gene polymorphisms: TNF-α, IL-10, IFN-γ variants
- HLA-DRB1*1501: 3-fold increased EBV lymphoma risk
- IL-10 -1082 G/G: 2-fold higher EBV viral loads
- IFNL3 rs12979860: CC genotype predicts HCV clearance
💡 Master This: Viral integration sites are influenced by chromatin accessibility and transcriptional activity - HPV integration occurs preferentially in actively transcribed genes and fragile sites, with MYC locus integration conferring 3-fold higher progression risk and resistance to standard therapies.
The tumor microenvironment in viral cancers displays unique characteristics that distinguish them from spontaneous malignancies. Viral antigens create chronic inflammatory states with distinct immune infiltration patterns that can be therapeutically exploited through precision immunotherapy approaches.
- Microenvironment Characteristics
- Immune infiltration: Higher TIL density in viral-positive tumors
- Angiogenesis patterns: VEGF overexpression in >80% of viral cancers
- Fibroblast activation: CAF populations differ between viral/non-viral tumors
- CD8+ T-cell infiltration: 2-3 fold higher in HPV-positive cancers
- PD-L1 expression: >50% of viral tumors vs <20% viral-negative
- Mutational burden: Lower in viral cancers but higher immunogenicity
Connect these multi-system integration concepts through rapid mastery frameworks to understand how viral cancer knowledge translates into clinical expertise tools.
🔗 Multi-System Integration: The Viral-Host Ecosystem
🎯 Clinical Mastery Arsenal: The Viral Cancer Command Center
📌 Remember: MASTER viral cancers - Monitor viral loads, Assess immune status, Screen high-risk populations, Target viral pathways, Evaluate treatment response, Recognize resistance patterns
-
Rapid Recognition Matrix
- Age + Geography + Anatomy = Viral Probability
- Young + Endemic area + Jaw mass = Burkitt lymphoma (EBV)
- Middle-aged + Mediterranean + Purple lesions = Kaposi sarcoma (HHV-8)
- Elderly + Asia + Liver mass = Hepatocellular carcinoma (HBV/HCV)
- Sensitivity thresholds: >80% for geographic clustering
- Specificity markers: >90% for anatomical predilection
- Positive predictive value: >70% when 3+ factors present
-
Essential Quantitative Arsenal
- HPV viral load: >1000 copies/cell indicates high-grade dysplasia
- EBV DNA: >1000 copies/mL plasma suggests active lymphoma
- HBV DNA: >20,000 IU/mL requires immediate antiviral therapy
- CD4+ count: <200 cells/μL dramatically increases viral cancer risk
- Treatment thresholds: Viral suppression targets for each pathogen
- Monitoring intervals: Risk-stratified surveillance schedules
- Resistance markers: Genetic signatures predicting treatment failure
| Clinical Scenario | Viral Suspect | Key Test | Threshold | Action Required | Timeline |
|---|---|---|---|---|---|
| Cervical dysplasia | HPV 16/18 | DNA PCR | >1000 copies | Colposcopy + biopsy | 2-4 weeks |
| Atypical lymphoma | EBV | EBER ISH | Positive | Staging + R-CHOP | 1-2 weeks |
| Liver mass + HBsAg | HBV | Viral load | >2000 IU/mL | Antiviral + oncology | Immediate |
| Purple skin lesions | HHV-8 | LANA stain | Positive | HIV test + staging | 1 week |
| Nasopharyngeal mass | EBV | Plasma DNA | >4000 copies | MRI + biopsy | 1-2 weeks |
- Treatment Decision Trees
- Viral load + Immune status + Cancer stage = Treatment intensity
- High viral load + Low immunity + Advanced cancer = Maximum therapy
- Low viral load + Normal immunity + Early cancer = Standard protocols
- Dose modifications: Viral status influences chemotherapy tolerance
- Sequence optimization: Antiviral timing affects cancer treatment efficacy
- Combination strategies: Synergistic vs antagonistic drug interactions
💡 Master This: Immune reconstitution inflammatory syndrome (IRIS) occurs in 10-25% of patients when antiviral therapy rapidly suppresses viral loads during cancer treatment - corticosteroid prophylaxis prevents severe reactions in high-risk scenarios.
The prognostic stratification system for viral cancers incorporates viral-specific factors alongside traditional staging parameters, creating enhanced prediction models with superior accuracy for survival estimation and treatment planning.
- Prognostic Integration Framework
- Viral factors: Load, genotype, integration status, resistance mutations
- Host factors: HLA type, immune function, co-infections, genetic susceptibility
- Tumor factors: Stage, grade, viral protein expression, immune infiltration
- Risk stratification: Low, intermediate, high categories
- Survival prediction: Median survival estimates with confidence intervals
- Treatment selection: Evidence-based protocol recommendations
This comprehensive viral cancer mastery framework transforms complex pathophysiology into immediately actionable clinical tools, enabling rapid recognition, evidence-based treatment, and optimal patient outcomes through systematic application of viral-specific knowledge.
🎯 Clinical Mastery Arsenal: The Viral Cancer Command Center
Practice Questions: Oncogenic viruses
Test your understanding with these related questions
A 38-year-old woman makes an appointment with her family physician for a routine check-up after being away due to travel for 1 year. She recently had a screening Pap smear, which was negative for malignancy. Her past medical history is significant for a Pap smear 2 years ago that reported a low-grade squamous intraepithelial lesion (LSIL). A subsequent colposcopy diagnosed high-grade cervical intraepithelial neoplasia (CIN2). The patient is surprised by the differences in her diagnostic tests. You explain to her the basis for the difference and reassure her. With this in mind, which of the following HPV serotypes is most likely to be present in the patient?













