Gastrointestinal microbiome US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Gastrointestinal microbiome. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Gastrointestinal microbiome US Medical PG Question 1: A 47-year-old man comes to the physician because of abdominal pain and foul-smelling, watery diarrhea for several days. He has not had nausea, vomiting, or blood in the stool. He has a history of alcohol use disorder and recently completed a 7-day course of clindamycin for pneumonia. He has not traveled out of the United States. Which of the following toxins is most likely to be involved in the pathogenesis of this patient's symptoms?
- A. Cereulide toxin
- B. Cholera toxin
- C. Clostridioides difficile cytotoxin (Correct Answer)
- D. Shiga toxin
- E. Alpha toxin
Gastrointestinal microbiome Explanation: ***Clostridioides difficile cytotoxin***
- The patient's history of recent **clindamycin** use, followed by **abdominal pain** and **foul-smelling, watery diarrhea**, is highly suggestive of *Clostridioides difficile* infection.
- *C. difficile* produces **cytotoxin (TcdB)** and **enterotoxin (TcdA)**, which lead to colitis and diarrhea, often after antimicrobial therapy.
*Cereulide toxin*
- This preformed toxin is produced by *Bacillus cereus* and typically causes a **short-incubation** emetic type of food poisoning, characterized by **nausea and vomiting**.
- The patient's symptoms are primarily diarrhea, and nausea/vomiting are absent, making this less likely.
*Cholera toxin*
- Produced by *Vibrio cholerae*, this toxin causes profuse, **"rice-water" diarrhea** with rapid dehydration.
- The patient has not traveled to endemic areas, and there is no mention of the characteristic severe dehydration or "rice-water" stool.
*Shiga toxin*
- This toxin, produced by *Shigella dysenteriae* and enterohemorrhagic *E. coli* (EHEC), typically causes **bloody diarrhea** and can lead to **hemolytic uremic syndrome (HUS)**.
- The patient's diarrhea is watery and explicitly stated to be without blood, ruling out Shiga toxin as the cause.
*Alpha toxin*
- This toxin is produced by *Clostridium perfringens* and is primarily associated with **gas gangrene** (myonecrosis) and some forms of food poisoning.
- While *C. perfringens* can cause diarrhea, it's typically mild and self-limiting, and the clinical picture in this patient, especially with recent antibiotic use, points more strongly to *C. difficile*.
Gastrointestinal microbiome US Medical PG Question 2: A 42-year-old man with hypertension and type 2 diabetes mellitus is admitted to the hospital because of swelling and redness of the left leg for 3 days. He has chills and malaise. He is treated with intravenous clindamycin for 7 days. On the 8th day at the hospital, he has profuse, foul-smelling, and watery diarrhea. He has nausea and intermittent abdominal cramping. His temperature is 38°C (100.4°F), pulse is 97/min, and blood pressure is 110/78 mm Hg. Bowel sounds are hyperactive. Abdominal examination shows mild tenderness in the left lower quadrant. Rectal examination shows no abnormalities. His hemoglobin concentration is 14.3 g/dL, leukocyte count is 12,300/mm3, and C-reactive protein concentration is 62 mg/L (N=0.08–3.1). After discontinuing clindamycin, which of the following is the most appropriate pharmacotherapy for this patient's condition?
- A. Intravenous vancomycin
- B. Oral fidaxomicin (Correct Answer)
- C. Intravenous metronidazole
- D. Oral metronidazole
- E. Oral rifaximin
Gastrointestinal microbiome Explanation: ***Oral fidaxomicin***
- The patient's presentation with profuse, foul-smelling, watery diarrhea, abdominal cramping, and fever after prolonged antibiotic use (clindamycin) is highly suggestive of **Clostridioides difficile infection (CDI)**.
- **Oral fidaxomicin** is a first-line agent for initial CDI episodes with **superior efficacy** in reducing recurrence rates compared to metronidazole and similar cure rates to oral vancomycin. It is preferred due to its **narrow spectrum**, **bactericidal activity against C. difficile**, and **minimal disruption to normal colonic flora**.
- Current IDSA/SHEA guidelines recommend fidaxomicin or oral vancomycin as first-line therapy for initial CDI episodes.
*Intravenous vancomycin*
- **Intravenous vancomycin** has poor penetration into the GI tract and is therefore **ineffective for C. difficile infection (CDI)**, which is an intraluminal infection.
- Oral vancomycin is effective for CDI, but intravenous administration will not treat the infection.
*Intravenous metronidazole*
- **Intravenous metronidazole** has limited efficacy in treating **Clostridioides difficile infection (CDI)** as first-line therapy.
- While it achieves some colonic concentration even when given intravenously, oral agents (fidaxomicin or vancomycin) are preferred for initial episodes.
- IV metronidazole may be used as adjunctive therapy in fulminant cases with ileus when oral agents cannot reach the colon.
*Oral metronidazole*
- **Oral metronidazole** was previously used for non-severe CDI but is **no longer recommended as first-line therapy** per updated IDSA/SHEA guidelines due to inferior cure rates and higher recurrence rates compared to vancomycin and fidaxomicin.
- It may be considered only when fidaxomicin and vancomycin are unavailable.
*Oral rifaximin*
- **Oral rifaximin** is sometimes used as **adjunctive therapy following standard treatment** to prevent recurrent C. difficile infection (CDI).
- It is **not recommended as initial monotherapy** for an active CDI episode.
Gastrointestinal microbiome US Medical PG Question 3: A 17-year-old girl is brought in by her mother due to rapid weight loss over the past month. The patient says she has been having episodes of diarrhea, which she attributes to laxatives she takes regularly to keep her weight down. She also says she has not had her period yet. The patient’s mother adds that the patient has been underperforming at school and acting very strangely at home. Her current BMI is 16.8 kg/m2. On physical examination, the skin on her limbs and around her neck is inflamed and erythematous. Her tongue is bright red and smooth. She states that over the last 2 weeks, she has been eating nothing but small portions of fruit. She is diagnosed with a vitamin deficiency. Which of the following statements is true about the vitamin most likely deficient in this patient?
- A. It increases the GI absorption of iron
- B. It is derived from tyrosine
- C. Synthesis requires vitamin B2 and B6 (Correct Answer)
- D. Synthesis requires vitamin B1 and B6
- E. It is used to treat hypertension
Gastrointestinal microbiome Explanation: ***Synthesis requires vitamin B2 and B6***
- The patient's symptoms (diarrhea, dermatitis, dementia-like behavior, glossitis, and weight loss) are classic for **pellagra**, which is caused by a deficiency in **niacin (vitamin B3)**.
- The synthesis of **niacin** from **tryptophan** requires **pyridoxine (vitamin B6)** and **riboflavin (vitamin B2)** as cofactors.
*It increases the GI absorption of iron*
- **Vitamin C** (ascorbic acid) enhances the **gastrointestinal absorption of non-heme iron** by reducing ferric iron to its ferrous form.
- Niacin does not play a direct role in the absorption of iron.
*It is derived from tyrosine*
- **Tyrosine** is a precursor to several important compounds, including **catecholamines** (dopamine, norepinephrine, epinephrine) and **thyroid hormones**.
- **Niacin** is predominantly synthesized from the essential amino acid **tryptophan**.
*Synthesis requires vitamin B1 and B6*
- While **vitamin B6** is essential for niacin synthesis from tryptophan, **vitamin B1 (thiamine)** is not directly involved in this pathway.
- Thiamine's primary role is in carbohydrate metabolism.
*It is used to treat hypertension*
- While **niacin** can affect lipid profiles, it is **not commonly used as a primary treatment for hypertension**.
- **Niacin** is used, primarily in pharmacologic doses, to **lower LDL cholesterol** and **triglycerides** and **raise HDL cholesterol**, often in conjunction with other lipid-lowering agents.
Gastrointestinal microbiome US Medical PG Question 4: A 55-year-old man presents to the physician with complaints of 5 days of watery diarrhea, fever, and bloating. He has not noticed any blood in his stool. He states that his diet has not changed recently, and his family has been spared from diarrhea symptoms despite eating the same foods that he has been cooking at home. He has no history of recent travel outside the United States. His only medication is high-dose omeprazole, which he has been taking daily for the past few months to alleviate his gastroesophageal reflux disease (GERD). Which of the following is the most appropriate initial test to work up this patient’s symptoms?
- A. Stool toxin assay (Correct Answer)
- B. Colonoscopy
- C. Fecal occult blood test
- D. Stool culture
- E. Stool ova and parasite
Gastrointestinal microbiome Explanation: ***Stool toxin assay***
- The patient's presentation of **watery diarrhea** and fever, especially with a history of **high-dose omeprazole use**, strongly suggests **Clostridioides difficile infection**.
- **Omeprazole** (a proton pump inhibitor) reduces stomach acid, which can disrupt the normal gut flora and increase susceptibility to *C. difficile*; a **stool toxin assay** is the most direct diagnostic test for this infection.
*Colonoscopy*
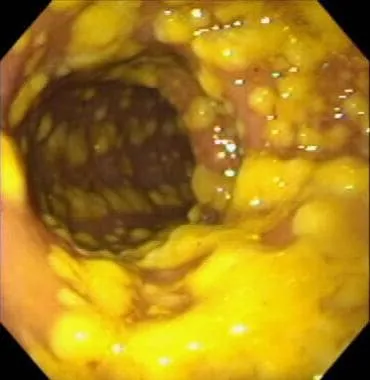
- While a colonoscopy can visualize pseudomembranes associated with severe *C. difficile* colitis, it is an **invasive procedure** and not the initial diagnostic test of choice for suspected infectious diarrhea.
- It is usually reserved for cases with atypical presentations, suspected complications, or when other diagnostic tests are inconclusive.
*Fecal occult blood test*
- The patient describes **watery diarrhea** and specifically states he has **not noticed any blood in his stool**, making a fecal occult blood test unlikely to be helpful in this acute setting.
- This test is primarily used for screening **colorectal cancer** or identifying chronic gastrointestinal bleeding.
*Stool culture*
- A stool culture primarily identifies bacterial pathogens like *Salmonella*, *Shigella*, or *Campylobacter*, which typically cause diarrheal illnesses that may include **bloody stools** or have specific epidemiological links (e.g., foodborne outbreaks).
- Given the history of **omeprazole use** and the absence of blood, *C. difficile* is more likely than these common bacterial enteritides, and a stool culture does not detect *C. difficile* itself.
*Stool ova and parasite*
- This test is used to detect **parasitic infections** (e.g., Giardia, Cryptosporidium), which can cause watery diarrhea and bloating.
- However, given the specific risk factor of **omeprazole use**, **Clostridioides difficile** infection is a more probable diagnosis, making the stool toxin assay the more appropriate initial test.
Gastrointestinal microbiome US Medical PG Question 5: A startup is working on a novel project in which they claim they can replicate the organelle that is defective in MELAS syndrome. Which of the following metabolic processes must they be able to replicate if their project is to mimic the metabolic processes of this organelle?
- A. Hexose monophosphate shunt
- B. Cholesterol synthesis
- C. Glycolysis
- D. Fatty acid (beta) oxidation (Correct Answer)
- E. Fatty acid synthesis
Gastrointestinal microbiome Explanation: ***Fatty acid (beta) oxidation***
- **MELAS syndrome** (Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-like episodes) is caused by defects in **mitochondrial function**.
- **Beta-oxidation of fatty acids** is a crucial metabolic process that occurs within the mitochondria, generating ATP.
*Hexose monophosphate shunt*
- The **hexose monophosphate shunt** (pentose phosphate pathway) occurs in the **cytosol** and is primarily involved in producing NADPH and synthesizing nucleotides, not a primary mitochondrial function.
- Its dysfunction is not directly linked to the core metabolic defects seen in MELAS syndrome.
*Cholesterol synthesis*
- **Cholesterol synthesis** primarily occurs in the **cytosol** and the **endoplasmic reticulum**, not within the mitochondria.
- While cholesterol metabolism can be indirectly affected by mitochondrial health, it is not a direct mitochondrial metabolic pathway.
*Glycolysis*
- **Glycolysis** is the metabolic pathway that converts glucose into pyruvate, occurring in the **cytosol**.
- Although it precedes mitochondrial oxidative phosphorylation, glycolysis itself does not occur within the mitochondria.
*Fatty acid synthesis*
- **Fatty acid synthesis** primarily takes place in the **cytosol** and endoplasmic reticulum, utilizing NADPH from the hexose monophosphate shunt.
- It is an anabolic process, while MELAS typically involves defects in catabolic/energy-producing mitochondrial pathways.
Gastrointestinal microbiome US Medical PG Question 6: A researcher has identified a chemical compound that she expects may contribute to the development of colorectal cancer. She designs an experiment where she exposes 70 mice to a diet containing this compound with another 50 mice in a control group that was fed a regular diet. After 9 months, the mice were evaluated for tumor development at necropsy. In total, 14 mice in the experimental group developed colorectal tumor burden, and 1 mouse in the control group developed tumors. Based on this experiment, what risk of colorectal cancer can be attributable to this chemical compound?
- A. 22.0%
- B. 2.0%
- C. 12.5%
- D. 18.0% (Correct Answer)
- E. 20.0%
Gastrointestinal microbiome Explanation: ***18.0%***
- The **attributable risk (AR)** is calculated as the **incidence in the exposed group (Ie)** minus the **incidence in the unexposed group (Iu)**.
- In this case, **Ie = 14/70 = 0.20** and **Iu = 1/50 = 0.02**. Therefore, **AR = 0.20 - 0.02 = 0.18**, or **18.0%**.
*22.0%*
- This value might result from an incorrect calculation or misinterpretation of the attributable risk formula.
- It does not correctly represent the difference in risk between the exposed and unexposed groups.
*2.0%*
- This represents the **incidence of colorectal tumors in the control group (Iu)**, not the attributable risk.
- The attributable risk accounts for the excess risk specifically due to the exposure.
*12.5%*
- This value is not derived from the standard formula for attributable risk using the provided data.
- It might represent a misunderstanding of how to calculate risk difference from incidence rates.
*20.0%*
- This represents the **incidence of colorectal tumors in the experimental group (Ie)**, not the attributable risk.
- The attributable risk needs to subtract the background risk observed in the unexposed group.
Gastrointestinal microbiome US Medical PG Question 7: A 58-year-old female, being treated on the medical floor for community-acquired pneumonia with levofloxacin, develops watery diarrhea. She reports at least 9 episodes of diarrhea within the last two days, with lower abdominal discomfort and cramping. Her temperature is 98.6° F (37° C), respiratory rate is 15/min, pulse is 67/min, and blood pressure is 122/98 mm Hg. Her physical examination is unremarkable. Laboratory testing shows:
Hb% 13 gm/dL
Total count (WBC): 13,400/mm3
Differential count:
Neutrophils: 80%
Lymphocytes: 15%
Monocytes: 5%
ESR: 33 mm/hr
What is the most likely diagnosis?
- A. Ulcerative colitis
- B. C. difficile colitis (Correct Answer)
- C. Osmotic diarrhea
- D. Giardiasis
- E. Irritable bowel syndrome
Gastrointestinal microbiome Explanation: ***C. difficile colitis***
- The patient's recent **antibiotic use (levofloxacin)**, followed by the development of **watery diarrhea** (9 episodes in 2 days) with abdominal cramping, is highly suggestive of *Clostridioides difficile* infection.
- The elevated **WBC count (13,400/mm3)** and **ESR (33 mm/hr)** indicate an inflammatory response, which is common in *C. difficile* colitis.
*Ulcerative colitis*
- Ulcerative colitis typically presents with **bloody diarrhea**, abdominal pain, and tenesmus, usually with a more chronic or relapsing course, which is not described.
- While it can manifest with flares, the direct temporal relationship with **antibiotic use** and the lack of bloody stools make it less likely.
*Osmotic diarrhea*
- Osmotic diarrhea is often related to the ingestion of **non-absorbable substances** (e.g., lactulose, sorbitol) or malabsorption and generally resolves with fasting.
- It is not typically associated with a significant **inflammatory response** (elevated WBC, ESR) or a clear link to recent antibiotic use.
*Giardiasis*
- Giardiasis is a parasitic infection that causes **protozoal diarrhea**, often characterized by foul-smelling, fatty stools, flatulence, and abdominal cramps.
- It is usually acquired from contaminated water and typically doesn't follow **antibiotic therapy** in this manner.
*Irritable bowel syndrome*
- IBS is a functional gastrointestinal disorder characterized by **chronic abdominal pain** and altered bowel habits (diarrhea, constipation, or both) in the absence of structural or biochemical abnormalities.
- It does not present as an acute, severe diarrheal illness linked to **antibiotic use** with systemic inflammatory markers.
Gastrointestinal microbiome US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Gastrointestinal microbiome Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Gastrointestinal microbiome US Medical PG Question 9: A hospital implements a bundle to reduce catheter-associated bloodstream infections. Components include: chlorhexidine bathing, antibiotic-impregnated catheters, antiseptic catheter site dressings, and daily line necessity assessment. After implementation, bloodstream infections with coagulase-negative staphylococci decrease by 60%, but Candida bloodstream infections increase by 40%. Evaluate the microbiological mechanisms underlying these divergent outcomes and synthesize an optimal prevention strategy.
- A. Antibiotic-impregnated catheters select for resistant Candida; use non-antibiotic catheters
- B. The bundle successfully reduced bacterial infections, revealing underlying fungal infections; add antifungal prophylaxis
- C. Multiple interventions disrupted skin flora creating ecological niche for Candida; modify bundle to preserve some commensal bacteria while maintaining antisepsis (Correct Answer)
- D. Chlorhexidine bathing eliminates bacterial skin flora but promotes fungal colonization; discontinue chlorhexidine
- E. Candida increase represents surveillance bias from increased culturing; no change needed
Gastrointestinal microbiome Explanation: ***Multiple interventions disrupted skin flora creating ecological niche for Candida; modify bundle to preserve some commensal bacteria while maintaining antisepsis***
- Aggressive use of **chlorhexidine bathing** and **antibiotic-impregnated catheters** eliminates commensal bacterial flora that provide **colonization resistance** against opportunistic fungi.
- The reduction in **Coagulase-negative staphylococci** creates an available **ecological niche**, allowing *Candida* species to proliferate and colonize the catheter site more effectively.
*Antibiotic-impregnated catheters select for resistant Candida; use non-antibiotic catheters*
- While **antibiotic-impregnated catheters** reduce bacterial biofilm, they do not directly "select" for resistance in fungi, as antibiotics have no biochemical target in *Candida*.
- Removing them entirely may lead to a rebound in **staphylococcal infections**, failing to address the need for a balanced antiseptic strategy.
*The bundle successfully reduced bacterial infections, revealing underlying fungal infections; add antifungal prophylaxis*
- Adding **antifungal prophylaxis** as a routine measures increases the risk of developing **drug-resistant fungal strains** like *Candida auris*.
- This approach ignores the ecological disruption caused by the bundle and instead layers on more **antimicrobial pressure**, which is rarely a sustainable prevention strategy.
*Chlorhexidine bathing eliminates bacterial skin flora but promotes fungal colonization; discontinue chlorhexidine*
- Discontinuing **chlorhexidine bathing** would likely reverse the 60% reduction in **coagulase-negative staphylococcal** infections, which are a major source of morbidity.
- The goal should be optimization (e.g., targeted use or modified frequency) rather than total discontinuation of an effective **infection control** tool.
*Candida increase represents surveillance bias from increased culturing; no change needed*
- A 40% increase in **Candida bloodstream infections** is a significant clinical shift that requires a root-cause analysis rather than dismissal as **surveillance bias**.
- "No change needed" is incorrect because the bundle has created a new, clinically significant risk for **iatrogenic candidemia**.
Gastrointestinal microbiome US Medical PG Question 10: A 68-year-old man develops Clostridioides difficile infection after hospitalization for pneumonia. He is treated with oral vancomycin with resolution of diarrhea. Two weeks later, he has recurrent C. difficile infection. After a second vancomycin course, he has a third recurrence. His physician must choose between extended vancomycin taper, fidaxomicin, or fecal microbiota transplantation (FMT). Synthesize the microbiological rationale for selecting FMT over continued antibiotic therapy in recurrent C. difficile infection.
- A. FMT restores colonization resistance that prevents C. difficile recurrence better than antibiotics that further disrupt flora (Correct Answer)
- B. FMT treats antibiotic-resistant C. difficile strains unresponsive to vancomycin
- C. FMT provides immune modulation that antibiotics cannot achieve
- D. FMT eradicates C. difficile spores more effectively than antibiotics
- E. FMT is more cost-effective than prolonged antibiotic courses
Gastrointestinal microbiome Explanation: ***FMT restores colonization resistance that prevents C. difficile recurrence better than antibiotics that further disrupt flora***
- Recurrent **Clostridioides difficile** infection (CDI) is driven by a persistent state of **dysbiosis** where the normal gut microbiome fails to inhibit spore germination and vegetative growth.
- **Fecal Microbiota Transplantation (FMT)** reintroduces a diverse ecosystem of commensal bacteria that compete for nutrients and restore **secondary bile acid metabolism**, effectively restoring the gut's **colonization resistance**.
*FMT treats antibiotic-resistant C. difficile strains unresponsive to vancomycin*
- CDI recurrence is rarely due to **antibiotic resistance**; C. difficile remains highly susceptible to **vancomycin** and **fidaxomicin** in vitro.
- The failure of therapy is due to the survival of **dormant spores** in a disrupted microbiome, not the presence of resistant vegetative cells.
*FMT provides immune modulation that antibiotics cannot achieve*
- While the microbiome does interact with the immune system, the primary mechanism of FMT in treating CDI is **microbial competition** and metabolic restoration rather than systemic **immune modulation**.
- Antibiotics like **fidaxomicin** can also have minor anti-inflammatory effects, but this is not the rationale for choosing FMT over pharmacological therapy.
*FMT eradicates C. difficile spores more effectively than antibiotics*
- Neither antibiotics nor FMT directly "kill" or **eradicate spores**; spores are biologically inert and resistant to most environmental stressors.
- FMT works by preventing those spores from **germinating** into toxin-producing vegetative cells by restoring the inhibitory environment of a healthy gut.
*FMT is more cost-effective than prolonged antibiotic courses*
- While FMT may be **cost-effective** in the long term by preventing further hospitalizations, this is a pharmacoeconomic rationale rather than a **microbiological** one.
- The question specifically asks for the **microbiological rationale**, which pertains to the restoration of the ecological balance of the gut flora.
More Gastrointestinal microbiome US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.