Fecal microbiota transplantation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Fecal microbiota transplantation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Fecal microbiota transplantation US Medical PG Question 1: A 72-year-old woman presents to the clinic complaining of diarrhea for the past week. She mentions intense fatigue and intermittent, cramping abdominal pain. She has not noticed any blood in her stool. She recalls an episode of pneumonia last month for which she was hospitalized and treated with antibiotics. She has traveled recently to Florida to visit her family and friends. Her past medical history is significant for hypertension, peptic ulcer disease, and hypercholesterolemia for which she takes losartan, esomeprazole, and atorvastatin. She also has osteoporosis, for which she takes calcium and vitamin D and occasional constipation for which she takes an over the counter laxative as needed. Physical examination shows lower abdominal tenderness but is otherwise insignificant. Blood pressure is 110/70 mm Hg, pulse is 80/min, and respiratory rate is 18/min. Stool testing is performed and reveals the presence of anaerobic, gram-positive bacilli. Which of the following increased this patient’s risk of developing this clinical presentation?
- A. Hypercholesterolemia treated with atorvastatin
- B. Constipation treated with laxatives
- C. Osteoporosis treated with calcium and vitamin D
- D. Peptic ulcer disease treated with esomeprazole
- E. Recent antibiotic use for pneumonia treatment (Correct Answer)
Fecal microbiota transplantation Explanation: ***Recent antibiotic use for pneumonia treatment***
- **Antibiotic exposure** is the single most important risk factor for *Clostridioides difficile* infection (CDI), present in approximately 70% of cases.
- Antibiotics disrupt the normal protective gut microbiota, eliminating competitive bacteria and allowing *C. difficile* spores to germinate, colonize, and produce toxins.
- The patient's recent hospitalization and antibiotic treatment for pneumonia directly precipitated this infection by creating an ecological niche for *C. difficile* overgrowth.
- Common culprit antibiotics include fluoroquinolones, clindamycin, cephalosporins, and penicillins.
*Peptic ulcer disease treated with esomeprazole*
- **Proton pump inhibitors (PPIs)** like esomeprazole are an independent risk factor for CDI, increasing risk approximately 2-3 fold.
- PPIs reduce gastric acid production, which normally serves as a defense mechanism against ingested *C. difficile* spores.
- However, PPIs alone do not typically cause CDI without concurrent disruption of gut flora (usually by antibiotics).
- While this is a contributory risk factor in this patient, it is not the primary cause.
*Hypercholesterolemia treated with atorvastatin*
- **Statins** like atorvastatin have no established association with increased risk of *Clostridioides difficile* infection.
- They work by inhibiting HMG-CoA reductase to lower cholesterol and do not affect gastric pH or gut microbiota composition.
*Constipation treated with laxatives*
- Occasional **over-the-counter laxative use** is not a risk factor for *Clostridioides difficile* infection.
- While laxatives affect gut motility, they do not disrupt the protective gut microbiota or increase susceptibility to CDI.
*Osteoporosis treated with calcium and vitamin D*
- **Calcium and vitamin D supplementation** has no association with increased risk of *Clostridioides difficile* infection.
- These supplements support bone health and calcium metabolism without affecting gut flora or gastric acid production.
Fecal microbiota transplantation US Medical PG Question 2: A scientist is studying the mechanisms by which bacteria become resistant to antibiotics. She begins by obtaining a culture of vancomycin-resistant Enterococcus faecalis and conducts replicate plating experiments. In these experiments, colonies are inoculated onto a membrane and smeared on 2 separate plates, 1 containing vancomycin and the other with no antibiotics. She finds that all of the bacterial colonies are vancomycin resistant because they grow on both plates. She then maintains the bacteria in liquid culture without vancomycin while she performs her other studies. Fifteen generations of bacteria later, she conducts replicate plating experiments again and finds that 20% of the colonies are now sensitive to vancomycin. Which of the following mechanisms is the most likely explanation for why these colonies have become vancomycin sensitive?
- A. Point mutation
- B. Gain of function mutation
- C. Viral infection
- D. Plasmid loss (Correct Answer)
- E. Loss of function mutation
Fecal microbiota transplantation Explanation: ***Plasmid loss***
- The initial **vancomycin resistance** in *Enterococcus faecalis* is often mediated by genes located on **plasmids**, which are extrachromosomal DNA.
- In the absence of selective pressure (vancomycin), bacteria that lose the plasmid (and thus the resistance genes) have a **growth advantage** over those that retain the energetically costly plasmid, leading to an increase in sensitive colonies over generations.
*Point mutation*
- A **point mutation** typically involves a change in a single nucleotide and could lead to loss of resistance if it occurred in a gene conferring resistance.
- However, since there was no selective pressure for loss of resistance, it is less likely that 20% of the population would acquire such a specific point mutation to revert resistance.
*Gain of function mutation*
- A **gain of function mutation** would imply that the bacteria acquired a *new* advantageous trait, not the *loss* of resistance.
- This type of mutation would not explain why some colonies became sensitive to vancomycin after the drug was removed.
*Viral infection*
- **Viral infection** (bacteriophages) can transfer genes through transduction or cause bacterial lysis, but it's not the primary mechanism for a widespread reversion of resistance in the absence of antibiotic pressure.
- It would not explain the observed increase in vancomycin-sensitive colonies due to evolutionary pressure.
*Loss of function mutation*
- While a **loss of function mutation** in a gene conferring resistance could lead to sensitivity, it's generally less likely to explain a 20% shift without selective pressure than **plasmid loss**.
- Plasmids are often unstable and are easily lost in the absence of selection, whereas a specific gene mutation causing loss of function would need to arise and become prevalent in the population.
Fecal microbiota transplantation US Medical PG Question 3: A 42-year-old man with hypertension and type 2 diabetes mellitus is admitted to the hospital because of swelling and redness of the left leg for 3 days. He has chills and malaise. He is treated with intravenous clindamycin for 7 days. On the 8th day at the hospital, he has profuse, foul-smelling, and watery diarrhea. He has nausea and intermittent abdominal cramping. His temperature is 38°C (100.4°F), pulse is 97/min, and blood pressure is 110/78 mm Hg. Bowel sounds are hyperactive. Abdominal examination shows mild tenderness in the left lower quadrant. Rectal examination shows no abnormalities. His hemoglobin concentration is 14.3 g/dL, leukocyte count is 12,300/mm3, and C-reactive protein concentration is 62 mg/L (N=0.08–3.1). After discontinuing clindamycin, which of the following is the most appropriate pharmacotherapy for this patient's condition?
- A. Intravenous vancomycin
- B. Oral fidaxomicin (Correct Answer)
- C. Intravenous metronidazole
- D. Oral metronidazole
- E. Oral rifaximin
Fecal microbiota transplantation Explanation: ***Oral fidaxomicin***
- The patient's presentation with profuse, foul-smelling, watery diarrhea, abdominal cramping, and fever after prolonged antibiotic use (clindamycin) is highly suggestive of **Clostridioides difficile infection (CDI)**.
- **Oral fidaxomicin** is a first-line agent for initial CDI episodes with **superior efficacy** in reducing recurrence rates compared to metronidazole and similar cure rates to oral vancomycin. It is preferred due to its **narrow spectrum**, **bactericidal activity against C. difficile**, and **minimal disruption to normal colonic flora**.
- Current IDSA/SHEA guidelines recommend fidaxomicin or oral vancomycin as first-line therapy for initial CDI episodes.
*Intravenous vancomycin*
- **Intravenous vancomycin** has poor penetration into the GI tract and is therefore **ineffective for C. difficile infection (CDI)**, which is an intraluminal infection.
- Oral vancomycin is effective for CDI, but intravenous administration will not treat the infection.
*Intravenous metronidazole*
- **Intravenous metronidazole** has limited efficacy in treating **Clostridioides difficile infection (CDI)** as first-line therapy.
- While it achieves some colonic concentration even when given intravenously, oral agents (fidaxomicin or vancomycin) are preferred for initial episodes.
- IV metronidazole may be used as adjunctive therapy in fulminant cases with ileus when oral agents cannot reach the colon.
*Oral metronidazole*
- **Oral metronidazole** was previously used for non-severe CDI but is **no longer recommended as first-line therapy** per updated IDSA/SHEA guidelines due to inferior cure rates and higher recurrence rates compared to vancomycin and fidaxomicin.
- It may be considered only when fidaxomicin and vancomycin are unavailable.
*Oral rifaximin*
- **Oral rifaximin** is sometimes used as **adjunctive therapy following standard treatment** to prevent recurrent C. difficile infection (CDI).
- It is **not recommended as initial monotherapy** for an active CDI episode.
Fecal microbiota transplantation US Medical PG Question 4: A 21-year-old woman comes to the physician because of a 4-day history of abdominal cramps and bloody diarrhea 5 times per day. Her symptoms began after she ate an egg sandwich from a restaurant. Her vital signs are within normal limits. Physical examination shows diffuse abdominal tenderness. Stool culture shows gram-negative rods that produce hydrogen sulfide and do not ferment lactose. Which of the following effects is most likely to occur if she receives antibiotic therapy?
- A. Orange discoloration of bodily fluids
- B. Pruritic maculopapular rash on the extensor surface
- C. Self-limiting systemic inflammatory response
- D. Prolonged fecal excretion of the pathogen (Correct Answer)
- E. Thrombocytopenia and hemolytic anemia
Fecal microbiota transplantation Explanation: ***Prolonged fecal excretion of the pathogen***
- The patient's symptoms (abdominal cramps, bloody diarrhea after eating an egg sandwich) and stool culture results (gram-negative rods, hydrogen sulfide producers, non-lactose fermenting) are highly suggestive of **Salmonella enterica** infection.
- Antibiotic treatment for non-typhoidal Salmonella gastroenteritis typically **prolongs fecal excretion** and does not shorten the illness, reserving antibiotics for severe cases or immunocompromised individuals.
*Orange discoloration of bodily fluids*
- **Orange discoloration of bodily fluids** (urine, sweat, tears) is a known side effect of **rifampin**, an antibiotic primarily used for tuberculosis and some bacterial meningitides.
- Rifampin is not indicated nor commonly used for Salmonella gastroenteritis.
*Pruritic maculopapular rash on the extensor surface*
- A **pruritic maculopapular rash on the extensor surfaces** is a common presentation of drug reactions, often associated with **penicillins** or **cephalosporins**, especially in viral infections (e.g., amoxicillin rash in mononucleosis).
- This is a general antibiotic side effect and not specifically linked to the outcome of treating Salmonella.
*Self-limiting systemic inflammatory response*
- A self-limiting systemic inflammatory response could be a general reaction to an active infection or a drug, but it's not the most likely or specific outcome of **antibiotic therapy in Salmonella gastroenteritis**.
- Worsening of symptoms can occur in some cases due to toxemia from bacterial lysis (e.g., Jarisch-Herxheimer reaction), but "self-limiting systemic inflammatory response" is too generic for this specific scenario.
*Thrombocytopenia and hemolytic anemia*
- **Thrombocytopenia and hemolytic anemia** in the setting of diarrheal illness strongly suggest **hemolytic uremic syndrome (HUS)**, which is typically associated with **Shiga toxin-producing E. coli** (STEC), particularly E. coli O157:H7.
- While Salmonella can cause severe disease, HUS is not a typical complication of its treatment, and antibiotics are often avoided in STEC infections due to increased risk of HUS.
Fecal microbiota transplantation US Medical PG Question 5: A 58-year-old female, being treated on the medical floor for community-acquired pneumonia with levofloxacin, develops watery diarrhea. She reports at least 9 episodes of diarrhea within the last two days, with lower abdominal discomfort and cramping. Her temperature is 98.6° F (37° C), respiratory rate is 15/min, pulse is 67/min, and blood pressure is 122/98 mm Hg. Her physical examination is unremarkable. Laboratory testing shows:
Hb% 13 gm/dL
Total count (WBC): 13,400/mm3
Differential count:
Neutrophils: 80%
Lymphocytes: 15%
Monocytes: 5%
ESR: 33 mm/hr
What is the most likely diagnosis?
- A. Ulcerative colitis
- B. C. difficile colitis (Correct Answer)
- C. Osmotic diarrhea
- D. Giardiasis
- E. Irritable bowel syndrome
Fecal microbiota transplantation Explanation: ***C. difficile colitis***
- The patient's recent **antibiotic use (levofloxacin)**, followed by the development of **watery diarrhea** (9 episodes in 2 days) with abdominal cramping, is highly suggestive of *Clostridioides difficile* infection.
- The elevated **WBC count (13,400/mm3)** and **ESR (33 mm/hr)** indicate an inflammatory response, which is common in *C. difficile* colitis.
*Ulcerative colitis*
- Ulcerative colitis typically presents with **bloody diarrhea**, abdominal pain, and tenesmus, usually with a more chronic or relapsing course, which is not described.
- While it can manifest with flares, the direct temporal relationship with **antibiotic use** and the lack of bloody stools make it less likely.
*Osmotic diarrhea*
- Osmotic diarrhea is often related to the ingestion of **non-absorbable substances** (e.g., lactulose, sorbitol) or malabsorption and generally resolves with fasting.
- It is not typically associated with a significant **inflammatory response** (elevated WBC, ESR) or a clear link to recent antibiotic use.
*Giardiasis*
- Giardiasis is a parasitic infection that causes **protozoal diarrhea**, often characterized by foul-smelling, fatty stools, flatulence, and abdominal cramps.
- It is usually acquired from contaminated water and typically doesn't follow **antibiotic therapy** in this manner.
*Irritable bowel syndrome*
- IBS is a functional gastrointestinal disorder characterized by **chronic abdominal pain** and altered bowel habits (diarrhea, constipation, or both) in the absence of structural or biochemical abnormalities.
- It does not present as an acute, severe diarrheal illness linked to **antibiotic use** with systemic inflammatory markers.
Fecal microbiota transplantation US Medical PG Question 6: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Fecal microbiota transplantation Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Fecal microbiota transplantation US Medical PG Question 7: A 54-year-old man presents with fever, abdominal pain, nausea, and bloody diarrhea. He says that his symptoms started 36 hours ago and have not improved. Past medical history is significant for a left-leg abscess secondary to an injury he sustained from a fall 4 days ago while walking his dog. He has been taking clindamycin for this infection. In addition, he has long-standing gastroesophageal reflux disease, managed with omeprazole. His vital signs include: temperature 38.5°C (101.3°F), respiratory rate 19/min, heart rate 90/min, and blood pressure 110/70 mm Hg. Which of the following is the best course of treatment for this patient’s most likely diagnosis?
- A. Tetracycline
- B. Ciprofloxacin
- C. Trimethoprim-sulfamethoxazole
- D. Erythromycin
- E. Vancomycin (Correct Answer)
Fecal microbiota transplantation Explanation: ***Vancomycin***
- The patient's history of recent **clindamycin** use for an abscess, development of **fever, abdominal pain, nausea, and bloody diarrhea**, and use of **omeprazole** (a risk factor), strongly suggests **_Clostridioides difficile_ infection (CDI)**.
- **Oral vancomycin** is a first-line treatment for **severe non-fulminant CDI**, which this patient's symptoms (fever, bloody diarrhea) are consistent with.
*Tetracycline*
- **Tetracycline** is typically used for bacterial infections like **chlamydia, Lyme disease, and rickettsial infections**; it is not effective against _C. difficile_.
- It works by **inhibiting bacterial protein synthesis** but does not target the cell wall of _C. difficile_.
*Ciprofloxacin*
- **Ciprofloxacin**, a fluoroquinolone, is generally **contraindicated in CDI** as it can be a risk factor for developing the infection or exacerbate it due to disruption of gut flora.
- While effective against many gram-negative bacteria, it has **no significant activity against _C. difficile_**.
*Trimethoprim-sulfamethoxazole*
- **Trimethoprim-sulfamethoxazole** is a combination antibiotic used for various bacterial infections, including **UTIs and some respiratory infections**.
- It is **not effective against _C. difficile_** and is not recommended for its treatment.
*Erythromycin*
- **Erythromycin**, a macrolide, is effective against a range of bacterial infections including **atypical pneumonia and skin infections**.
- It has **no role in the treatment of _C. difficile_ infection** and its use could potentially further disrupt the gut microbiome.
Fecal microbiota transplantation US Medical PG Question 8: A 49-year-old man presents to the emergency department with acute onset of pain and redness of the skin of his lower leg for the past 3 days. He has had type 2 diabetes mellitus for the past 12 years, but he is not compliant with his medications. He has smoked 10–15 cigarettes per day for the past 20 years. His temperature is 38°C (100.4°F), pulse is 95/min, and blood pressure is 110/70 mm Hg. On physical examination, the pretibial area is erythematous, edematous, and tender. He is diagnosed with acute cellulitis, and intravenous ceftazidime sodium is started. On the 5th day of antibiotic therapy, the patient complains of severe watery diarrhea, fever, and abdominal tenderness without rigidity. Complete blood count is ordered for the patient and shows 14,000 white blood cells/mm3. Which of the following is the best initial therapy for this patient?
- A. Intravenous vancomycin
- B. Oral ciprofloxacin
- C. Fecal microbiota transplantation
- D. Oral vancomycin (Correct Answer)
- E. Oral metronidazole
Fecal microbiota transplantation Explanation: ***Oral vancomycin***
- The patient exhibits classic symptoms of **Clostridioides difficile infection (CDI)**: watery diarrhea, fever, abdominal tenderness, and leukocytosis following antibiotic use (ceftazidime). Oral vancomycin is the **first-line therapy** for severe CDI.
- Oral vancomycin achieves high intraluminal concentrations, effectively targeting C. difficile in the colon with minimal systemic absorption.
*Intravenous vancomycin*
- Intravenous vancomycin has **poor penetration** into the gastrointestinal tract and is therefore ineffective for treating C. difficile infection.
- It is primarily used for systemic infections caused by **methicillin-resistant Staphylococcus aureus (MRSA)**.
*Oral ciprofloxacin*
- **Fluoroquinolones** like ciprofloxacin are associated with an increased risk of developing C. difficile infection due to their broad-spectrum activity.
- They are not effective treatments for C. difficile and can potentially worsen the condition or select for resistant strains.
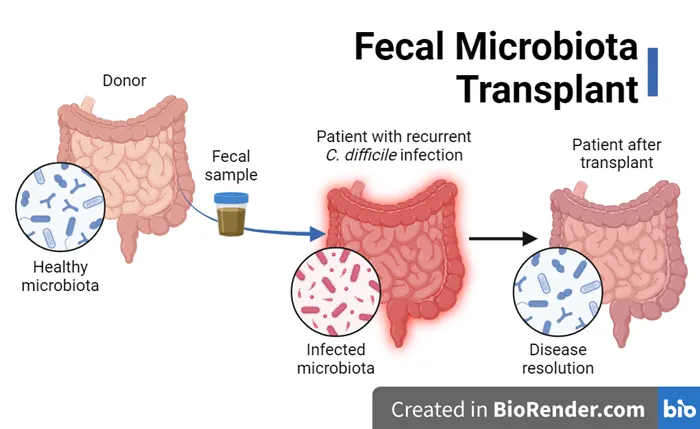
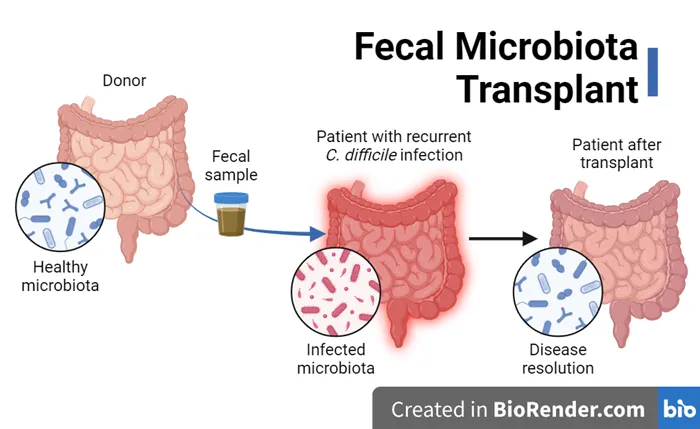
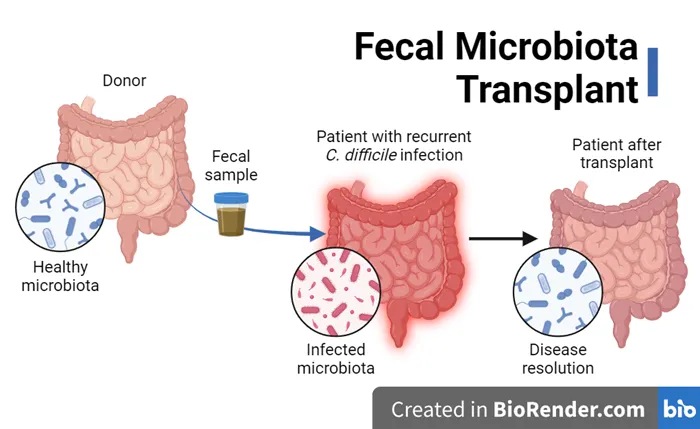
*Fecal microbiota transplantation*
- **Fecal microbiota transplantation (FMT)** is a highly effective treatment for recurrent C. difficile infection, but it is typically reserved for patients who have failed multiple courses of standard antibiotic therapy.
- It is not considered the initial therapy for acute, uncomplicated C. difficile infection.
*Oral metronidazole*
- **Oral metronidazole** was historically used for C. difficile infection but is **no longer recommended** as first-line therapy per current **2021 IDSA/SHEA guidelines** due to inferior clinical outcomes compared to vancomycin or fidaxomicin.
- Given the patient's fever and leukocytosis indicating severe infection, vancomycin is the preferred initial treatment.
Fecal microbiota transplantation US Medical PG Question 9: A 68-year-old man comes to the physician because of a 1-month history of fatigue, low-grade fevers, and cough productive of blood-tinged sputum. He has type 2 diabetes mellitus and chronic kidney disease and underwent kidney transplantation 8 months ago. His temperature is 38.9°C (102.1°F) and pulse is 98/min. Examination shows rhonchi in the right lower lung field. An x-ray of the chest shows a right-sided lobar consolidation. A photomicrograph of specialized acid-fast stained tissue from a blood culture is shown. Which of the following is the strongest predisposing factor for this patient's condition?
- A. Sharing of unsterile IV needles
- B. Poor oral hygiene
- C. Exposure to contaminated air-conditioning unit
- D. Exposure to contaminated soil (Correct Answer)
- E. Crowded living situation
Fecal microbiota transplantation Explanation: ***Exposure to contaminated soil***
- The photomicrograph shows **acid-fast stain** demonstrating **filamentous, branching gram-positive rods**, consistent with **Nocardia species**.
- **Nocardiosis** is acquired through **inhalation of Nocardia spores from contaminated soil or dust**, which is the primary environmental source and route of transmission.
- While this patient's **immunocompromised status** (post-kidney transplant on immunosuppressive therapy) is the critical host factor that predisposes him to infection, **soil exposure** is the specific environmental predisposing factor among the options listed.
- Nocardia is an opportunistic pathogen that primarily affects immunocompromised individuals, causing pulmonary infection that can disseminate.
*Sharing of unsterile IV needles*
- Sharing unsterile IV needles is a common route for transmitting **bloodborne pathogens** (e.g., HIV, hepatitis B/C) or causing bacterial endocarditis and soft tissue infections.
- This is not the typical route of acquisition for **pulmonary nocardiosis**, which is acquired via inhalation.
*Poor oral hygiene*
- Poor oral hygiene predisposes to dental caries, periodontal disease, and aspiration of oral flora causing pneumonia or lung abscess.
- **Actinomyces** (not acid-fast) is associated with poor oral hygiene and can be confused with Nocardia morphologically, but Actinomyces is not acid-fast positive.
- This is not a risk factor for acquiring **Nocardia** infection.
*Exposure to contaminated air-conditioning unit*
- Contaminated air-conditioning units and water systems are associated with **Legionella pneumophila**, causing Legionnaires' disease.
- Legionella is not acid-fast and does not show the branching filamentous morphology seen with Nocardia.
*Crowded living situation*
- Crowded living situations increase risk of person-to-person transmission of respiratory pathogens such as **Mycobacterium tuberculosis**, influenza, and other droplet-spread infections.
- **Nocardia** is acquired from environmental sources (soil, dust), not through person-to-person transmission.
Fecal microbiota transplantation US Medical PG Question 10: A 55-year-old man presents to the physician with complaints of 5 days of watery diarrhea, fever, and bloating. He has not noticed any blood in his stool. He states that his diet has not changed recently, and his family has been spared from diarrhea symptoms despite eating the same foods that he has been cooking at home. He has no history of recent travel outside the United States. His only medication is high-dose omeprazole, which he has been taking daily for the past few months to alleviate his gastroesophageal reflux disease (GERD). Which of the following is the most appropriate initial test to work up this patient’s symptoms?
- A. Stool toxin assay (Correct Answer)
- B. Colonoscopy
- C. Fecal occult blood test
- D. Stool culture
- E. Stool ova and parasite
Fecal microbiota transplantation Explanation: ***Stool toxin assay***
- The patient's presentation of **watery diarrhea** and fever, especially with a history of **high-dose omeprazole use**, strongly suggests **Clostridioides difficile infection**.
- **Omeprazole** (a proton pump inhibitor) reduces stomach acid, which can disrupt the normal gut flora and increase susceptibility to *C. difficile*; a **stool toxin assay** is the most direct diagnostic test for this infection.
*Colonoscopy*
- While a colonoscopy can visualize pseudomembranes associated with severe *C. difficile* colitis, it is an **invasive procedure** and not the initial diagnostic test of choice for suspected infectious diarrhea.
- It is usually reserved for cases with atypical presentations, suspected complications, or when other diagnostic tests are inconclusive.
*Fecal occult blood test*
- The patient describes **watery diarrhea** and specifically states he has **not noticed any blood in his stool**, making a fecal occult blood test unlikely to be helpful in this acute setting.
- This test is primarily used for screening **colorectal cancer** or identifying chronic gastrointestinal bleeding.
*Stool culture*
- A stool culture primarily identifies bacterial pathogens like *Salmonella*, *Shigella*, or *Campylobacter*, which typically cause diarrheal illnesses that may include **bloody stools** or have specific epidemiological links (e.g., foodborne outbreaks).
- Given the history of **omeprazole use** and the absence of blood, *C. difficile* is more likely than these common bacterial enteritides, and a stool culture does not detect *C. difficile* itself.
*Stool ova and parasite*
- This test is used to detect **parasitic infections** (e.g., Giardia, Cryptosporidium), which can cause watery diarrhea and bloating.
- However, given the specific risk factor of **omeprazole use**, **Clostridioides difficile** infection is a more probable diagnosis, making the stool toxin assay the more appropriate initial test.
More Fecal microbiota transplantation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.