Dysbiosis and disease associations US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Dysbiosis and disease associations. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Dysbiosis and disease associations US Medical PG Question 1: An investigator is studying the growth of an organism in different media. The organism is inoculated on a petri dish that contains heated sheep blood, vancomycin, nystatin, trimethoprim, and colistin. The resulting growth medium is incubated at 37°C. Numerous small, white colonies are seen after incubation for 48 hours. This organism is most likely to cause which of the following conditions?
- A. Pontiac fever
- B. Pseudomembranous colitis
- C. Hemolytic uremic syndrome
- D. Oral thrush
- E. Gonorrhea (Correct Answer)
Dysbiosis and disease associations Explanation: ***Gonorrhea***
- The growth medium described is **Thayer-Martin agar**, a selective medium containing **heated sheep blood** (supplies NAD+), **vancomycin** (inhibits Gram-positives), **colistin** (inhibits Gram-negatives), **nystatin** (inhibits fungi), and **trimethoprim** (inhibits Proteus). This medium is specifically designed for the isolation of *Neisseria gonorrhoeae* from polymicrobial samples.
- *Neisseria gonorrhoeae* typically grows as **small, translucent-to-white colonies** on selective media like Thayer-Martin agar, and incubation at 37°C in CO2 (not explicitly mentioned but often required) for 24-48 hours yields visible growth, causing **gonorrhea**.
*Pontiac fever*
- Pontiac fever is a mild, self-limiting form of **legionellosis**, caused by *Legionella pneumophila*.
- *Legionella* requires a specialized medium such as **buffered charcoal yeast extract (BCYE) agar** for growth, not Thayer-Martin agar.
*Pseudomembranous colitis*
- This condition is caused by **toxin-producing *Clostridioides difficile***, often after antibiotic use.
- *C. difficile* is an obligate anaerobe and requires **anaerobic conditions** and specific selective media (e.g., CCFA agar) for isolation, not Thayer-Martin agar under aerobic conditions.
*Hemolytic uremic syndrome*
- Hemolytic uremic syndrome (HUS) is often caused by **Shiga toxin-producing *Escherichia coli* (STEC)**, particularly O157:H7.
- STEC can be isolated on media like **sorbitol MacConkey agar (SMAC)**, where O157:H7 appears as non-sorbitol fermenting colonies, distinct from the growth seen on Thayer-Martin.
*Oral thrush*
- Oral thrush is caused by *Candida albicans*, a yeast.
- *Candida* would be inhibited by **nystatin** in the Thayer-Martin medium, which is an antifungal agent.
Dysbiosis and disease associations US Medical PG Question 2: A previously healthy 20-year-old woman comes to the physician because of recurrent abdominal cramps, bloating, and diarrhea for 4 months. She describes her stools as greasy, foul-smelling, and difficult to flush. During this time she has had a 6-kg (13.2-lb) weight loss. She has no personal or family history of serious illness. Physical examination shows pallor and cheilitis. Laboratory studies show a hemoglobin concentration of 11 g/dL. Serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference range. Test of the stool for occult blood is negative and stool microscopy reveals no pathogens and no leukocytes. Analysis of a 24-hour stool sample shows 12 g of fat. The patient is asked to consume 25 g of d-xylose. Five hours later, its concentration is measured in urine at 2 g (N = > 4 g/5 h). The test is repeated after a two-week course of rifaximin, but the urinary concentration of d-xylose remains the same. Which of the following is the most likely diagnosis?
- A. Exocrine pancreatic insufficiency
- B. Bacterial overgrowth in the small intestine
- C. Tropheryma whipplei infection
- D. Hypersensitivity to gliadin (Correct Answer)
- E. Lactose intolerance
Dysbiosis and disease associations Explanation: ***Hypersensitivity to gliadin***
* The patient's symptoms (greasy, foul-smelling stools, weight loss, abdominal cramps, bloating, diarrhea, pallor, cheilitis, iron-deficiency anemia) are highly suggestive of **malabsorption**.
* The **impaired d-xylose absorption** that does not improve after antibiotics points to an intrinsic small bowel mucosal defect rather than bacterial overgrowth, making celiac disease (hypersensitivity to gliadin) the most likely diagnosis.
*Exocrine pancreatic insufficiency*
* While it causes **steatorrhea** and malabsorption, it typically presents with normal d-xylose absorption because **d-xylose is a monosaccharide that is absorbed directly by the intestinal mucosa without requiring pancreatic enzymes**.
* The normal function of the small intestinal mucosa would allow for adequate d-xylose absorption.
*Bacterial overgrowth in the small intestine*
* Symptoms can mimic malabsorption, and d-xylose absorption may be impaired due to bacterial consumption.
* However, the patient's d-xylose test did not improve after a course of **rifaximin**, which is an antibiotic effective against bacterial overgrowth.
*Tropheryma whipplei infection*
* Whipple's disease can cause malabsorption, **steatorrhea**, and abdominal symptoms similar to those described.
* However, it also commonly presents with **arthralgia, lymphadenopathy, and neurological symptoms**, which are absent in this patient.
*Lactose intolerance*
* This condition primarily causes bloating, cramps, and diarrhea, but typically does not lead to **significant weight loss** or **steatorrhea (greasy stools)**.
* D-xylose absorption would also be expected to be normal because it is a **monosaccharide** that is absorbed directly, unlike lactose which requires lactase.
Dysbiosis and disease associations US Medical PG Question 3: A 57-year-old HIV-positive male with a history of intravenous drug abuse presents to the emergency room complaining of arm swelling. He reports that he developed progressively worsening swelling and tenderness over the right antecubital fossa three days prior. He recently returned from a trip to Nicaragua. His past medical history is notable for an anaphylactoid reaction to vancomycin. His temperature is 101.4°F (38.6°C), blood pressure is 140/70 mmHg, pulse is 110/min, and respirations are 20/min. Physical examination reveals an erythematous, fluctuant, and tender mass overlying the right antecubital fossa. Multiple injection marks are noted across both upper extremities. He undergoes incision and drainage and is started on an antibiotic that targets the 50S ribosome. He is discharged with plans to follow up in one week. However, five days later he presents to the same emergency room complaining of abdominal cramps and watery diarrhea. Which of the following classes of pathogens is most likely responsible for this patient’s current symptoms?
- A. Gram-negative curved bacillus
- B. Gram-negative bacillus
- C. Anaerobic flagellated protozoan
- D. Gram-positive bacillus (Correct Answer)
- E. Gram-positive coccus
Dysbiosis and disease associations Explanation: ***Gram-positive bacillus***
- The patient was administered an antibiotic targeting the **50S ribosomal subunit** following incision and drainage for a suspected skin infection (likely **MRSA** given IV drug abuse). This strongly suggests **clindamycin** was used.
- **Clindamycin** is a known risk factor for developing **Clostridioides (formerly Clostridium) difficile infection (CDI)**, which is caused by a **Gram-positive, spore-forming bacillus** and manifests with **abdominal cramps and watery diarrhea**.
*Gram-negative curved bacillus*
- This class of pathogens includes organisms like **Vibrio cholerae** or **Campylobacter jejuni**, which can cause diarrhea.
- However, the patient's presentation with **colitis** after antibiotic use is more consistent with **Clostridioides difficile**, not typically a curved Gram-negative bacillus.
*Gram-negative bacillus*
- While some Gram-negative bacilli (e.g., E. coli, Salmonella) can cause diarrhea, their association with **antibiotic-induced colitis** following treatment for a skin abscess is less direct than that of *Clostridioides difficile*.
- The initial skin infection in IV drug users is most commonly staphylococcal (Gram-positive coccus), for which a 50S targeting antibiotic would be prescribed.
*Anaerobic flagellated protozoan*
- This description often refers to pathogens like **Giardia lamblia** or **Trichomonas vaginalis**, which are not bacteria.
- While *Giardia* can cause diarrhea, it typically causes **malabsorption** and **greasy stools**, and wouldn't be triggered by recent antibiotic use for a skin infection.
*Gram-positive coccus*
- **Gram-positive cocci** (e.g., Staphylococcus aureus) are the likely cause of the initial skin infection/abscess.
- However, they do not typically cause **antibiotic-associated colitis** with watery diarrhea; rather, the *antibiotic treatment itself* for these organisms can predispose to *Clostridioides difficile*.
Dysbiosis and disease associations US Medical PG Question 4: A 21-year-old woman comes to the physician because of a 4-day history of abdominal cramps and bloody diarrhea 5 times per day. Her symptoms began after she ate an egg sandwich from a restaurant. Her vital signs are within normal limits. Physical examination shows diffuse abdominal tenderness. Stool culture shows gram-negative rods that produce hydrogen sulfide and do not ferment lactose. Which of the following effects is most likely to occur if she receives antibiotic therapy?
- A. Orange discoloration of bodily fluids
- B. Pruritic maculopapular rash on the extensor surface
- C. Self-limiting systemic inflammatory response
- D. Prolonged fecal excretion of the pathogen (Correct Answer)
- E. Thrombocytopenia and hemolytic anemia
Dysbiosis and disease associations Explanation: ***Prolonged fecal excretion of the pathogen***
- The patient's symptoms (abdominal cramps, bloody diarrhea after eating an egg sandwich) and stool culture results (gram-negative rods, hydrogen sulfide producers, non-lactose fermenting) are highly suggestive of **Salmonella enterica** infection.
- Antibiotic treatment for non-typhoidal Salmonella gastroenteritis typically **prolongs fecal excretion** and does not shorten the illness, reserving antibiotics for severe cases or immunocompromised individuals.
*Orange discoloration of bodily fluids*
- **Orange discoloration of bodily fluids** (urine, sweat, tears) is a known side effect of **rifampin**, an antibiotic primarily used for tuberculosis and some bacterial meningitides.
- Rifampin is not indicated nor commonly used for Salmonella gastroenteritis.
*Pruritic maculopapular rash on the extensor surface*
- A **pruritic maculopapular rash on the extensor surfaces** is a common presentation of drug reactions, often associated with **penicillins** or **cephalosporins**, especially in viral infections (e.g., amoxicillin rash in mononucleosis).
- This is a general antibiotic side effect and not specifically linked to the outcome of treating Salmonella.
*Self-limiting systemic inflammatory response*
- A self-limiting systemic inflammatory response could be a general reaction to an active infection or a drug, but it's not the most likely or specific outcome of **antibiotic therapy in Salmonella gastroenteritis**.
- Worsening of symptoms can occur in some cases due to toxemia from bacterial lysis (e.g., Jarisch-Herxheimer reaction), but "self-limiting systemic inflammatory response" is too generic for this specific scenario.
*Thrombocytopenia and hemolytic anemia*
- **Thrombocytopenia and hemolytic anemia** in the setting of diarrheal illness strongly suggest **hemolytic uremic syndrome (HUS)**, which is typically associated with **Shiga toxin-producing E. coli** (STEC), particularly E. coli O157:H7.
- While Salmonella can cause severe disease, HUS is not a typical complication of its treatment, and antibiotics are often avoided in STEC infections due to increased risk of HUS.
Dysbiosis and disease associations US Medical PG Question 5: A 55-year-old man presents to the physician with complaints of 5 days of watery diarrhea, fever, and bloating. He has not noticed any blood in his stool. He states that his diet has not changed recently, and his family has been spared from diarrhea symptoms despite eating the same foods that he has been cooking at home. He has no history of recent travel outside the United States. His only medication is high-dose omeprazole, which he has been taking daily for the past few months to alleviate his gastroesophageal reflux disease (GERD). Which of the following is the most appropriate initial test to work up this patient’s symptoms?
- A. Stool toxin assay (Correct Answer)
- B. Colonoscopy
- C. Fecal occult blood test
- D. Stool culture
- E. Stool ova and parasite
Dysbiosis and disease associations Explanation: ***Stool toxin assay***
- The patient's presentation of **watery diarrhea** and fever, especially with a history of **high-dose omeprazole use**, strongly suggests **Clostridioides difficile infection**.
- **Omeprazole** (a proton pump inhibitor) reduces stomach acid, which can disrupt the normal gut flora and increase susceptibility to *C. difficile*; a **stool toxin assay** is the most direct diagnostic test for this infection.
*Colonoscopy*
- While a colonoscopy can visualize pseudomembranes associated with severe *C. difficile* colitis, it is an **invasive procedure** and not the initial diagnostic test of choice for suspected infectious diarrhea.
- It is usually reserved for cases with atypical presentations, suspected complications, or when other diagnostic tests are inconclusive.
*Fecal occult blood test*
- The patient describes **watery diarrhea** and specifically states he has **not noticed any blood in his stool**, making a fecal occult blood test unlikely to be helpful in this acute setting.
- This test is primarily used for screening **colorectal cancer** or identifying chronic gastrointestinal bleeding.
*Stool culture*
- A stool culture primarily identifies bacterial pathogens like *Salmonella*, *Shigella*, or *Campylobacter*, which typically cause diarrheal illnesses that may include **bloody stools** or have specific epidemiological links (e.g., foodborne outbreaks).
- Given the history of **omeprazole use** and the absence of blood, *C. difficile* is more likely than these common bacterial enteritides, and a stool culture does not detect *C. difficile* itself.
*Stool ova and parasite*
- This test is used to detect **parasitic infections** (e.g., Giardia, Cryptosporidium), which can cause watery diarrhea and bloating.
- However, given the specific risk factor of **omeprazole use**, **Clostridioides difficile** infection is a more probable diagnosis, making the stool toxin assay the more appropriate initial test.
Dysbiosis and disease associations US Medical PG Question 6: A 54-year-old man comes to the physician because of diarrhea that has become progressively worse over the past 4 months. He currently has 4–6 episodes of foul-smelling stools per day. Over the past 3 months, he has had fatigue and a 5-kg (11-lb) weight loss. He returned from Bangladesh 6 months ago after a year-long business assignment. He has osteoarthritis and hypertension. Current medications include amlodipine and naproxen. He appears pale and malnourished. His temperature is 37.3°C (99.1°F), pulse is 76/min, and blood pressure is 140/86 mm Hg. Examination shows pale conjunctivae and dry mucous membranes. Angular stomatitis and glossitis are present. The abdomen is distended but soft and nontender. Rectal examination shows no abnormalities. Laboratory studies show:
Hemoglobin 8.9 g/dL
Leukocyte count 4100/mm3
Platelet count 160,000/mm3
Mean corpuscular volume 110 μm3
Serum
Na+ 133 mEq/L
Cl- 98 mEq/l
K+ 3.3 mEq/L
Creatinine 1.1 mg/dL
IgA 250 mg/dL
Anti-tissue transglutaminase, IgA negative
Stool culture and studies for ova and parasites are negative. Test of the stool for occult blood is negative. Fecal fat content is 22 g/day (N < 7). Fecal lactoferrin is negative and elastase is within normal limits. Which of the following is the most appropriate next step in diagnosis?
- A. CT scan of the abdomen
- B. IgG against deamidated gliadin peptide
- C. Schilling test
- D. Enteroscopy
- E. PAS-stained biopsy of small bowel (Correct Answer)
Dysbiosis and disease associations Explanation: ***PAS-stained biopsy of small bowel***
- The patient's history of travel to Bangladesh, chronic diarrhea, malabsorption (weight loss, fatigue, elevated fecal fat, macrocytic anemia), and negative celiac serology (anti-tissue transglutaminase IgA) are highly suggestive of **Whipple's disease**.
- **Periodic Acid-Schiff (PAS) staining** of a small bowel biopsy is the gold standard for diagnosing Whipple's disease, revealing **PAS-positive macrophages** containing *Tropheryma whipplei*.
*CT scan of the abdomen*
- While a CT scan can identify structural abnormalities or masses, it is not the most direct diagnostic test for **malabsorptive conditions** like Whipple's disease.
- It would likely show non-specific findings such as **bowel wall thickening** or **lymphadenopathy**, but not the definitive histological changes.
*IgG against deamidated gliadin peptide*
- This test is used to diagnose **celiac disease**, but the patient's IgA anti-tissue transglutaminase was already negative, and this IgG test is typically performed when IgA deficiency is suspected or in young children.
- Given the strong suspicion of an infectious etiology due to travel history and systemic symptoms, focusing solely on celiac serology is less appropriate as the first next step.
*Schilling test*
- The Schilling test is an **obsolete test** that was historically used to assess **vitamin B12 absorption** and differentiate causes of B12 deficiency (pernicious anemia, bacterial overgrowth, or pancreatic insufficiency).
- This test is **no longer performed in clinical practice** due to unavailability of radioactive B12; modern evaluation uses serum B12, methylmalonic acid, and homocysteine levels.
- While the patient has macrocytic anemia, the test would not directly address the underlying cause of fat malabsorption and systemic symptoms present.
*Enteroscopy*
- Enteroscopy allows for visualization and biopsy of the small bowel beyond the reach of a standard upper endoscopy.
- While useful for obtaining biopsies, simply performing an enteroscopy without knowing what to look for or what specific stain to request (referring to PAS) on the biopsy would be less targeted than ordering a **PAS-stained biopsy** specifically.
Dysbiosis and disease associations US Medical PG Question 7: A 45-year-old man comes to the physician because of a 1-month history of fever and poor appetite. Five weeks ago, he underwent molar extraction for dental caries. His temperature is 38°C (100.4°F). Cardiac examination shows a grade 2/6 holosystolic murmur heard best at the apex. A blood culture shows gram-positive, catalase-negative cocci. Transesophageal echocardiography shows a small vegetation on the mitral valve with mild regurgitation. The causal organism most likely has which of the following characteristics?
- A. Production of dextrans (Correct Answer)
- B. Production of CAMP factor
- C. Conversion of fibrinogen to fibrin
- D. Formation of germ tubes at body temperature
- E. Replication in host macrophages
Dysbiosis and disease associations Explanation: **Production of dextrans**
- The clinical picture of **fever**, **poor appetite**, a **holosystolic murmur**, and **mitral valve vegetation** following a dental procedure (molar extraction) strongly points to **infective endocarditis** caused by **Viridans streptococci**.
- **Viridans streptococci**, commonly found in the oral cavity, produce **dextrans**, which allow them to adhere to damaged heart valves and fibrin-platelet aggregates, initiating vegetation formation.
*Production of CAMP factor*
- **CAMP factor** is a characteristic of **Group B Streptococcus (Streptococcus agalactiae)**, which primarily causes infections in neonates and immunocompromised adults, not typically infective endocarditis post-dental procedure.
- *Streptococcus agalactiae* is also catalase-negative and gram-positive but is rarely associated with endocarditis arising from oral flora.
*Conversion of fibrinogen to fibrin*
- The ability to convert **fibrinogen to fibrin** is characteristic of **coagulase-positive organisms**, such as *Staphylococcus aureus*, which is a catalase-positive organism.
- The blood culture in this case specifically states **catalase-negative cocci**, ruling out *Staphylococcus aureus* as the causative agent.
*Formation of germ tubes at body temperature*
- **Germ tube formation** at body temperature is a distinguishing characteristic of *Candida albicans*, a **fungus**, not a gram-positive, catalase-negative coccus.
- While *Candida* can cause endocarditis, the microbiological findings described do not align with a fungal infection.
*Replication in host macrophages*
- **Intracellular replication in host macrophages** is characteristic of certain bacteria like *Mycobacterium tuberculosis*, *Listeria monocytogenes*, or *Salmonella typhi*, which typically cause systemic infections
- This characteristic is not associated with the gram-positive, catalase-negative cocci responsible for subacute bacterial endocarditis following dental procedures.
Dysbiosis and disease associations US Medical PG Question 8: A hospital implements a bundle to reduce catheter-associated bloodstream infections. Components include: chlorhexidine bathing, antibiotic-impregnated catheters, antiseptic catheter site dressings, and daily line necessity assessment. After implementation, bloodstream infections with coagulase-negative staphylococci decrease by 60%, but Candida bloodstream infections increase by 40%. Evaluate the microbiological mechanisms underlying these divergent outcomes and synthesize an optimal prevention strategy.
- A. Antibiotic-impregnated catheters select for resistant Candida; use non-antibiotic catheters
- B. The bundle successfully reduced bacterial infections, revealing underlying fungal infections; add antifungal prophylaxis
- C. Multiple interventions disrupted skin flora creating ecological niche for Candida; modify bundle to preserve some commensal bacteria while maintaining antisepsis (Correct Answer)
- D. Chlorhexidine bathing eliminates bacterial skin flora but promotes fungal colonization; discontinue chlorhexidine
- E. Candida increase represents surveillance bias from increased culturing; no change needed
Dysbiosis and disease associations Explanation: ***Multiple interventions disrupted skin flora creating ecological niche for Candida; modify bundle to preserve some commensal bacteria while maintaining antisepsis***
- Aggressive use of **chlorhexidine bathing** and **antibiotic-impregnated catheters** eliminates commensal bacterial flora that provide **colonization resistance** against opportunistic fungi.
- The reduction in **Coagulase-negative staphylococci** creates an available **ecological niche**, allowing *Candida* species to proliferate and colonize the catheter site more effectively.
*Antibiotic-impregnated catheters select for resistant Candida; use non-antibiotic catheters*
- While **antibiotic-impregnated catheters** reduce bacterial biofilm, they do not directly "select" for resistance in fungi, as antibiotics have no biochemical target in *Candida*.
- Removing them entirely may lead to a rebound in **staphylococcal infections**, failing to address the need for a balanced antiseptic strategy.
*The bundle successfully reduced bacterial infections, revealing underlying fungal infections; add antifungal prophylaxis*
- Adding **antifungal prophylaxis** as a routine measures increases the risk of developing **drug-resistant fungal strains** like *Candida auris*.
- This approach ignores the ecological disruption caused by the bundle and instead layers on more **antimicrobial pressure**, which is rarely a sustainable prevention strategy.
*Chlorhexidine bathing eliminates bacterial skin flora but promotes fungal colonization; discontinue chlorhexidine*
- Discontinuing **chlorhexidine bathing** would likely reverse the 60% reduction in **coagulase-negative staphylococcal** infections, which are a major source of morbidity.
- The goal should be optimization (e.g., targeted use or modified frequency) rather than total discontinuation of an effective **infection control** tool.
*Candida increase represents surveillance bias from increased culturing; no change needed*
- A 40% increase in **Candida bloodstream infections** is a significant clinical shift that requires a root-cause analysis rather than dismissal as **surveillance bias**.
- "No change needed" is incorrect because the bundle has created a new, clinically significant risk for **iatrogenic candidemia**.
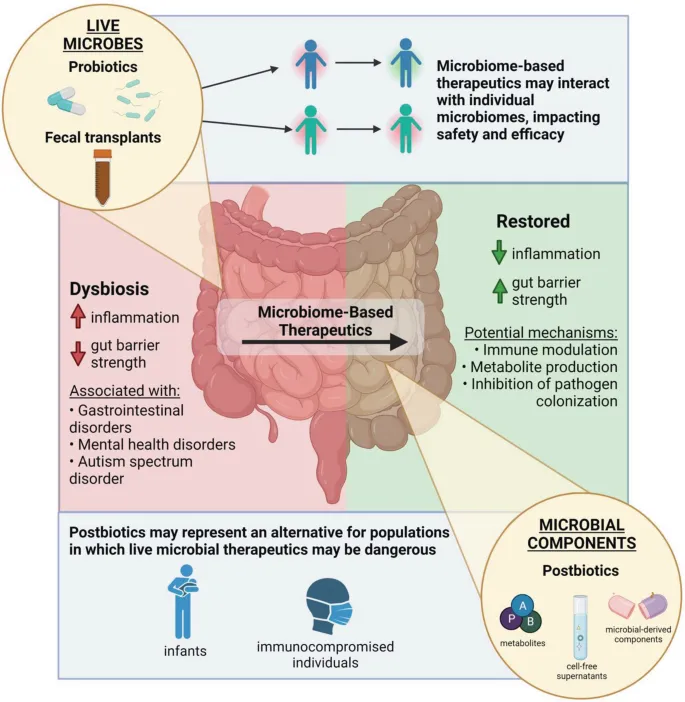
Dysbiosis and disease associations US Medical PG Question 9: A 68-year-old man develops Clostridioides difficile infection after hospitalization for pneumonia. He is treated with oral vancomycin with resolution of diarrhea. Two weeks later, he has recurrent C. difficile infection. After a second vancomycin course, he has a third recurrence. His physician must choose between extended vancomycin taper, fidaxomicin, or fecal microbiota transplantation (FMT). Synthesize the microbiological rationale for selecting FMT over continued antibiotic therapy in recurrent C. difficile infection.
- A. FMT restores colonization resistance that prevents C. difficile recurrence better than antibiotics that further disrupt flora (Correct Answer)
- B. FMT treats antibiotic-resistant C. difficile strains unresponsive to vancomycin
- C. FMT provides immune modulation that antibiotics cannot achieve
- D. FMT eradicates C. difficile spores more effectively than antibiotics
- E. FMT is more cost-effective than prolonged antibiotic courses
Dysbiosis and disease associations Explanation: ***FMT restores colonization resistance that prevents C. difficile recurrence better than antibiotics that further disrupt flora***
- Recurrent **Clostridioides difficile** infection (CDI) is driven by a persistent state of **dysbiosis** where the normal gut microbiome fails to inhibit spore germination and vegetative growth.
- **Fecal Microbiota Transplantation (FMT)** reintroduces a diverse ecosystem of commensal bacteria that compete for nutrients and restore **secondary bile acid metabolism**, effectively restoring the gut's **colonization resistance**.
*FMT treats antibiotic-resistant C. difficile strains unresponsive to vancomycin*
- CDI recurrence is rarely due to **antibiotic resistance**; C. difficile remains highly susceptible to **vancomycin** and **fidaxomicin** in vitro.
- The failure of therapy is due to the survival of **dormant spores** in a disrupted microbiome, not the presence of resistant vegetative cells.
*FMT provides immune modulation that antibiotics cannot achieve*
- While the microbiome does interact with the immune system, the primary mechanism of FMT in treating CDI is **microbial competition** and metabolic restoration rather than systemic **immune modulation**.
- Antibiotics like **fidaxomicin** can also have minor anti-inflammatory effects, but this is not the rationale for choosing FMT over pharmacological therapy.
*FMT eradicates C. difficile spores more effectively than antibiotics*
- Neither antibiotics nor FMT directly "kill" or **eradicate spores**; spores are biologically inert and resistant to most environmental stressors.
- FMT works by preventing those spores from **germinating** into toxin-producing vegetative cells by restoring the inhibitory environment of a healthy gut.
*FMT is more cost-effective than prolonged antibiotic courses*
- While FMT may be **cost-effective** in the long term by preventing further hospitalizations, this is a pharmacoeconomic rationale rather than a **microbiological** one.
- The question specifically asks for the **microbiological rationale**, which pertains to the restoration of the ecological balance of the gut flora.
Dysbiosis and disease associations US Medical PG Question 10: A research team is designing a probiotic intervention to prevent Clostridioides difficile infection in patients receiving antibiotics. They must choose between: (1) single-strain Lactobacillus; (2) multi-strain bacterial cocktail; (3) fecal microbiota transplantation; (4) prebiotic fiber supplementation. Evaluate which approach best applies principles of colonization resistance and normal flora restoration for PRIMARY prevention during antibiotic therapy.
- A. Multi-strain bacterial cocktail best recreates colonization resistance
- B. Fecal microbiota transplantation most completely restores normal flora
- C. Prebiotic fiber selectively promotes beneficial flora growth
- D. Single-strain Lactobacillus provides simplest and safest intervention
- E. No intervention has proven efficacy for primary prevention during antibiotics (Correct Answer)
Dysbiosis and disease associations Explanation: ***No intervention has proven efficacy for primary prevention during antibiotics***
- Despite theoretical benefits, clinical evidence does not support the routine use of probiotics or prebiotics for the **primary prevention** of *Clostridioides difficile* infection (CDI) while a patient is undergoing antibiotic therapy.
- Factors such as **antibiotic interference** with the probiotic strain's survival and the failure to achieve robust **engraftment** mean that **antibiotic stewardship** remains the only proven preventive strategy.
*Multi-strain bacterial cocktail best recreates colonization resistance*
- While **diverse microbiotas** are superior for **colonization resistance**, multi-strain probiotics are still killed or inhibited by the concurrent antibiotics being administered.
- They lack the complex **metabolic interactions** found in native flora required to successfully outcompete *C. difficile* spores during active antibiotic disruption.
*Fecal microbiota transplantation most completely restores normal flora*
- **Fecal microbiota transplantation (FMT)** is highly effective for treating **recurrent CDI**, but it is not indicated or validated for **primary prevention**.
- The complexity and risk profile of FMT make it unsuitable for routine use in patients simply starting a course of standard antibiotics.
*Prebiotic fiber selectively promotes beneficial flora growth*
- **Prebiotics** are non-digestible fibers intended to stimulate growth of "good" bacteria, but they cannot restore **bacterial diversity** when the source bacteria are being killed by antibiotics.
- There is currently **insufficient clinical evidence** to recommend prebiotics as a reliable method to prevent the onset of CDI in the clinical setting.
*Single-strain Lactobacillus provides simplest and safest intervention*
- **Single-strain probiotics** like *Lactobacillus* are often overwhelmed by the microbial shift (dysbiosis) caused by broad-spectrum antibiotics.
- These interventions are too simplified to mimic the **ecological niche protection** provided by the healthy, complex human microbiome.
More Dysbiosis and disease associations US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.