Development of microbiome from birth US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Development of microbiome from birth. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Development of microbiome from birth US Medical PG Question 1: A 6-day-old newborn is brought to the emergency department by his mother due to a high fever that started last night. His mother says that he was born via an uneventful vaginal delivery at home at 38 weeks gestation and was doing fine up until yesterday when he became disinterested in breastfeeding and spit up several times. His temperature is 39.5°C (103.1°F), pulse is 155/min, respirations are 45/min, and O2 sats are 92% on room air. He is lethargic and minimally responsive to stimuli. While on his back, his head is quickly lifted towards his chest which causes his legs to flex. The mother had only a few prenatal care visits and none at the end of the pregnancy. What is the most likely source of this patients infection?
- A. Tick bite
- B. During birth (Correct Answer)
- C. Infection from surgery
- D. Contaminated food
- E. Mother’s roommate
Development of microbiome from birth Explanation: ***During birth***
- The newborn's age (6 days old) and presentation with **fever**, **lethargy**, and **meningeal signs** (legs flexing upon lifting head, likely Brudzinski sign) are highly suggestive of **neonatal sepsis** or **meningitis**.
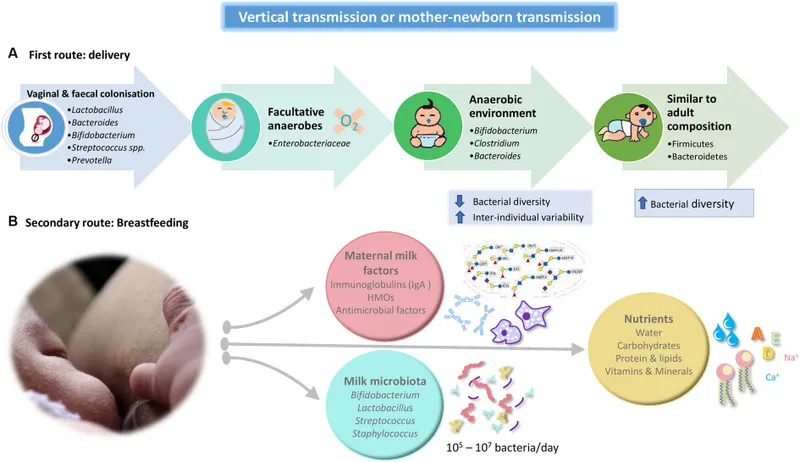
- Given the history of a home birth with limited prenatal care, the most probable source of infection would be vertical transmission **during passage through the birth canal**, especially if the mother was colonized with pathogens like Group B Streptococcus (GBS), E. coli, or had an untreated sexually transmitted infection.
*Tick bite*
- While tick-borne illnesses can cause fever, they are generally less common in this age group and the symptoms presented are more indicative of a widespread bacterial infection rather than a localized vector-borne illness.
- The neurological signs (meningeal irritation) are more consistent with meningitis, which is typically bacterial in newborns, rather than a common manifestation of a tick-borne disease in this age group.
*Infection from surgery*
- The patient had an **uneventful vaginal delivery at home**, meaning there was no surgical procedure involved, ruling out a surgical site infection.
- Surgical infections are typically seen after procedures like C-sections or circumcisions and would present differently.
*Contaminated food*
- A 6-day-old newborn is typically fed breast milk or formula and has no exposure to **solid or contaminated food** that would cause such an infection.
- Foodborne illnesses would usually present with prominent gastrointestinal symptoms like severe vomiting and diarrhea, which are not the primary features here.
*Mother’s roommate*
- While exposure to sick individuals can cause illness, the severe symptoms and rapid progression of the newborn's condition, along with the meningeal signs, point more towards a serious **vertical transmission during birth** rather than horizontal transmission from casual contact with a roommate.
- Diseases transmitted this way would also typically affect the respiratory tract before causing severe systemic illness.
Development of microbiome from birth US Medical PG Question 2: An investigator is studying the growth of an organism in different media. The organism is inoculated on a petri dish that contains heated sheep blood, vancomycin, nystatin, trimethoprim, and colistin. The resulting growth medium is incubated at 37°C. Numerous small, white colonies are seen after incubation for 48 hours. This organism is most likely to cause which of the following conditions?
- A. Pontiac fever
- B. Pseudomembranous colitis
- C. Hemolytic uremic syndrome
- D. Oral thrush
- E. Gonorrhea (Correct Answer)
Development of microbiome from birth Explanation: ***Gonorrhea***
- The growth medium described is **Thayer-Martin agar**, a selective medium containing **heated sheep blood** (supplies NAD+), **vancomycin** (inhibits Gram-positives), **colistin** (inhibits Gram-negatives), **nystatin** (inhibits fungi), and **trimethoprim** (inhibits Proteus). This medium is specifically designed for the isolation of *Neisseria gonorrhoeae* from polymicrobial samples.
- *Neisseria gonorrhoeae* typically grows as **small, translucent-to-white colonies** on selective media like Thayer-Martin agar, and incubation at 37°C in CO2 (not explicitly mentioned but often required) for 24-48 hours yields visible growth, causing **gonorrhea**.
*Pontiac fever*
- Pontiac fever is a mild, self-limiting form of **legionellosis**, caused by *Legionella pneumophila*.
- *Legionella* requires a specialized medium such as **buffered charcoal yeast extract (BCYE) agar** for growth, not Thayer-Martin agar.
*Pseudomembranous colitis*
- This condition is caused by **toxin-producing *Clostridioides difficile***, often after antibiotic use.
- *C. difficile* is an obligate anaerobe and requires **anaerobic conditions** and specific selective media (e.g., CCFA agar) for isolation, not Thayer-Martin agar under aerobic conditions.
*Hemolytic uremic syndrome*
- Hemolytic uremic syndrome (HUS) is often caused by **Shiga toxin-producing *Escherichia coli* (STEC)**, particularly O157:H7.
- STEC can be isolated on media like **sorbitol MacConkey agar (SMAC)**, where O157:H7 appears as non-sorbitol fermenting colonies, distinct from the growth seen on Thayer-Martin.
*Oral thrush*
- Oral thrush is caused by *Candida albicans*, a yeast.
- *Candida* would be inhibited by **nystatin** in the Thayer-Martin medium, which is an antifungal agent.
Development of microbiome from birth US Medical PG Question 3: A 20-week-old infant is brought to an urgent care clinic by her mother because she has not been eating well for the past 2 days. The mother said her daughter has also been "floppy" since yesterday morning and has been unable to move or open her eyes since the afternoon of the same day. The child has recently started solid foods, like cereals sweetened with honey. There is no history of loose, watery stools. On examination, the child is lethargic with lax muscle tone. She does not have a fever or apparent respiratory distress. What is the most likely mode of transmission of the pathogen responsible for this patient’s condition?
- A. Vertical transmission
- B. Vector-borne disease
- C. Direct contact
- D. Contaminated food (Correct Answer)
- E. Airborne transmission
Development of microbiome from birth Explanation: ***Contaminated food***
- The infant's symptoms of **lethargy**, widespread **flaccid paralysis** (floppy, unable to move or open eyes), and recent ingestion of **honey** (a known source of **Clostridium botulinum** spores) strongly suggest **infant botulism**.
- **Infant botulism** is acquired through the ingestion of **Clostridium botulinum spores**, typically from environmental sources or contaminated food like honey, which then germinate in the infant's immature gut.
*Vertical transmission*
- **Vertical transmission** refers to the passage of a pathogen from mother to offspring during pregnancy, birth, or breastfeeding.
- The clinical picture of **flaccid paralysis** and association with **honey ingestion** in this case does not align with typical vertically transmitted infections.
*Vector-borne disease*
- **Vector-borne diseases** are transmitted by an arthropod vector, such as mosquitoes or ticks.
- There is no clinical or epidemiological evidence in the scenario to suggest an **arthropod vector** as the source of this infant's illness.
*Direct contact*
- Diseases transmitted by **direct contact** typically require close physical interaction with an infected individual or their body fluids.
- The onset of **neurological symptoms** and the specific history of **honey ingestion** do not point to direct contact as the mode of transmission for botulism.
*Airborne transmission*
- **Airborne transmission** occurs when pathogens are spread through respiratory droplets or aerosols.
- The symptoms of **flaccid paralysis** and the history of recent **honey ingestion** are not consistent with an airborne pathogen.
Development of microbiome from birth US Medical PG Question 4: A 47-year-old man comes to the physician because of abdominal pain and foul-smelling, watery diarrhea for several days. He has not had nausea, vomiting, or blood in the stool. He has a history of alcohol use disorder and recently completed a 7-day course of clindamycin for pneumonia. He has not traveled out of the United States. Which of the following toxins is most likely to be involved in the pathogenesis of this patient's symptoms?
- A. Cereulide toxin
- B. Cholera toxin
- C. Clostridioides difficile cytotoxin (Correct Answer)
- D. Shiga toxin
- E. Alpha toxin
Development of microbiome from birth Explanation: ***Clostridioides difficile cytotoxin***
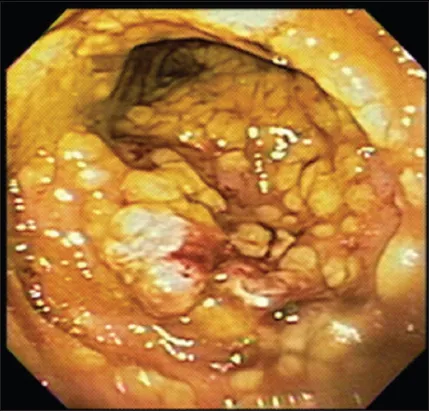
- The patient's history of recent **clindamycin** use, followed by **abdominal pain** and **foul-smelling, watery diarrhea**, is highly suggestive of *Clostridioides difficile* infection.
- *C. difficile* produces **cytotoxin (TcdB)** and **enterotoxin (TcdA)**, which lead to colitis and diarrhea, often after antimicrobial therapy.
*Cereulide toxin*
- This preformed toxin is produced by *Bacillus cereus* and typically causes a **short-incubation** emetic type of food poisoning, characterized by **nausea and vomiting**.
- The patient's symptoms are primarily diarrhea, and nausea/vomiting are absent, making this less likely.
*Cholera toxin*
- Produced by *Vibrio cholerae*, this toxin causes profuse, **"rice-water" diarrhea** with rapid dehydration.
- The patient has not traveled to endemic areas, and there is no mention of the characteristic severe dehydration or "rice-water" stool.
*Shiga toxin*
- This toxin, produced by *Shigella dysenteriae* and enterohemorrhagic *E. coli* (EHEC), typically causes **bloody diarrhea** and can lead to **hemolytic uremic syndrome (HUS)**.
- The patient's diarrhea is watery and explicitly stated to be without blood, ruling out Shiga toxin as the cause.
*Alpha toxin*
- This toxin is produced by *Clostridium perfringens* and is primarily associated with **gas gangrene** (myonecrosis) and some forms of food poisoning.
- While *C. perfringens* can cause diarrhea, it's typically mild and self-limiting, and the clinical picture in this patient, especially with recent antibiotic use, points more strongly to *C. difficile*.
Development of microbiome from birth US Medical PG Question 5: Which hormone is primarily responsible for initiating milk production postpartum?
- A. Prolactin (Correct Answer)
- B. Estrogen
- C. Oxytocin
- D. Progesterone
Development of microbiome from birth Explanation: ***Prolactin***
- **Prolactin** is the primary hormone responsible for **milk production (lactogenesis)** by stimulating alveolar epithelial cells in the mammary glands.
- Its levels rise significantly after childbirth, especially after the expulsion of the placenta, which leads to a drop in inhibitory hormones like progesterone.
*Estrogen*
- **Estrogen** plays a role in the **growth and development of the mammary glands** during pregnancy but inhibits milk production during gestation.
- High estrogen levels during pregnancy prevent prolactin from fully initiating lactation, and their sharp drop postpartum helps trigger milk synthesis.
*Oxytocin*
- **Oxytocin** is crucial for **milk ejection (let-down reflex)**, causing myoepithelial cells around the alveoli to contract and release milk.
- It does not directly cause milk production but rather aids in the release of milk that has already been synthesized.
*Progesterone*
- **Progesterone** is essential for the **development of the mammary glands** during pregnancy, contributing to alveolar growth.
- High levels of progesterone during pregnancy, along with estrogen, actually **inhibit** the full effect of prolactin, preventing milk production until after birth when these hormone levels drop.
Development of microbiome from birth US Medical PG Question 6: An exclusively breast-fed, 4-month-old boy is brought to the physician by his mother for a routine examination. He was born at term and delivery was uncomplicated. He received all standard treatment and testing prior to being discharged from the hospital. Examination shows no abnormalities. Without receiving additional supplementation at this time, this infant is at greatest risk of developing which of the following conditions?
- A. Intracranial bleed
- B. Microcytic anemia (Correct Answer)
- C. Rickets
- D. Scaly dermatitis
- E. Peripheral neuropathy
Development of microbiome from birth Explanation: ***Microcytic anemia***
- Exclusively breastfed infants are at risk for **iron deficiency anemia** because breast milk contains low levels of iron (~0.3 mg/L), and newborn iron stores are typically depleted by **4-6 months of age**.
- At 4 months, iron stores are beginning to deplete, and iron supplementation is typically initiated around this time; without supplementation, the infant is at greatest risk for developing **microcytic anemia** due to impaired hemoglobin synthesis.
- Iron deficiency causes red blood cells to be small (microcytic) and pale (hypochromic).
*Intracranial bleed*
- An intracranial bleed in an otherwise healthy infant is most commonly associated with **vitamin K deficiency bleeding (VKDB)**.
- However, the infant received **standard treatment** at birth, which includes vitamin K prophylaxis (typically 1 mg IM), making this highly unlikely.
*Rickets*
- Rickets is caused by **vitamin D deficiency**, leading to impaired bone mineralization.
- While breast milk is deficient in vitamin D, the **AAP recommends vitamin D supplementation (400 IU/day)** for all breastfed infants starting shortly after birth, which is part of standard care and would prevent rickets.
- No bone abnormalities are noted on examination.
*Scaly dermatitis*
- Scaly dermatitis, such as **seborrheic dermatitis (cradle cap)**, is common and physiological in infants but is not directly linked to a specific nutritional deficiency from exclusive breastfeeding.
- Severe, generalized scaly dermatitis could indicate **zinc deficiency** or **essential fatty acid deficiency**, but this is rare in otherwise healthy, exclusively breastfed term infants.
*Peripheral neuropathy*
- Peripheral neuropathy in infants can be caused by genetic, metabolic, or toxic conditions.
- It is **not** a common complication associated with exclusive breastfeeding in an otherwise healthy term infant.
Development of microbiome from birth US Medical PG Question 7: A 4-year-old girl is brought to the physician because her mother is concerned that she has been talking to an imaginary friend for 2 months. The child calls her friend 'Lucy' and says “Lucy is my best friend”. The child has multiple conversation and plays with the 'Lucy' throughout the day. The girl attends preschool regularly. She can copy a circle, tells stories, and can hop on one foot. Her maternal uncle has schizophrenia. Her parents are currently divorcing. The child's father has a history of illicit drug use. Physical examination shows no abnormalities. The mother is concerned about whether the child is acting out because of the divorce. Which of the following is the most appropriate next best step in management?
- A. Reassure the mother (Correct Answer)
- B. Perform MRI of the brain
- C. Schedule psychiatry consult
- D. Inform Child Protective Services
- E. Screen urine for drugs
Development of microbiome from birth Explanation: ***Reassure the mother***
- Imaginary friends are a **normal developmental phenomenon** in preschool-aged children, often associated with creativity and good social skills.
- The child's developmental milestones (copying a circle, hopping, telling stories) are appropriate for her age, indicating **healthy cognitive and motor development**.
*Perform MRI of the brain*
- There are **no neurological symptoms** or concerning signs in this case that would warrant an MRI of the brain.
- Imaginary friends are not indicative of a brain abnormality or neurological disorder.
*Schedule psychiatry consult*
- A psychiatry consult is **not indicated** as the child's behavior is developmentally appropriate.
- While there is a family history of schizophrenia and parental stress, the child is exhibiting typical childhood play and not symptoms of a mental health disorder.
*Inform Child Protective Services*
- There is **no evidence of child abuse or neglect** in the provided information.
- Although the parents are divorcing and the father has a history of drug use, there are no specific concerns raised about the child's safety or well-being that would require CPS involvement.
*Screen urine for drugs*
- A drug screen is **not relevant** to the child's behavior or a concern for drug use by the child.
- While the father has a history of illicit drug use, this does not automatically imply the child is being exposed to drugs, and the child's symptoms are unrelated to drug exposure.
Development of microbiome from birth US Medical PG Question 8: A 28-year-old woman with a past history of type 1 diabetes presents to your office with a 2-week history of vaginal itching and soreness accompanied by a white, clumpy vaginal discharge which she says resembles cheese curds. Her last HbA1c from a month ago was 7.8%, and her last cervical cytology from 10 months ago was reported as normal. She has a blood pressure of 118/76 mmHg, respiratory rate of 14/min, and heart rate of 74/min. Pelvic examination reveals multiple small erythematous lesions in the inguinal and perineal area, vulvar erythema, and excoriations. Inspection demonstrates a normal cervix and a white, adherent, thick, non-malodorous vaginal discharge. Which of the following is most likely to be present in a saline wet mount from the vaginal discharge of this patient?
- A. Clue cells on saline smear
- B. Gram-negative diplococci
- C. Hyphae (Correct Answer)
- D. Motile flagellates
- E. Multinucleated giant cells
Development of microbiome from birth Explanation: ***Hyphae***
- The patient's symptoms of **vaginal itching**, soreness, and a **white, clumpy discharge resembling cheese curds** are classic for **vulvovaginal candidiasis** (yeast infection).
- A **saline wet mount** in such cases typically reveals **hyphae** and **budding yeast forms** of *Candida albicans*.
*Clue cells on saline smear*
- **Clue cells** are characteristic of **bacterial vaginosis**, which is typically associated with a **thin, grayish discharge** and a **fishy odor** (amine odor), neither of which are described here.
- The discharge in this patient is described as **thick and non-malodorous**, which is inconsistent with bacterial vaginosis.
*Gram-negative diplococci*
- **Gram-negative diplococci** are the hallmark of **gonorrhea**, caused by *Neisseria gonorrhoeae*.
- Gonorrhea often presents with **purulent discharge** and cervical inflammation, or it can be asymptomatic; it does not typically cause the **clumpy discharge** and intense itching seen in this patient.
*Motile flagellates*
- **Motile flagellates** are characteristic of **trichomoniasis**, caused by *Trichomonas vaginalis*.
- This infection usually presents with a **frothy, yellow-green discharge**, a **fishy odor**, and cervical petechiae (strawberry cervix), which are not a feature of this patient's presentation.
*Multinucleated giant cells*
- **Multinucleated giant cells** are indicative of **herpes simplex virus (HSV) infection**, particularly when found on a **Tzanck smear** of a lesion.
- While the patient has erythematous lesions, the primary complaint of **vaginal discharge** and itching points away from herpes as the main cause of the discharge.
Development of microbiome from birth US Medical PG Question 9: A 16-year-old boy presents to his pediatrician because he has noticed white plaques forming on his tongue over the last 5 days. He recently returned from a boy scout trip where he traveled across the country and hiked through the woods. His past medical history is significant for asthma for which he uses an inhaler as needed. He says that during the trip he felt short of breath several times and had to use the inhaler. He also says that several of his friends appeared to get sick on the same trip and were coughing a lot. He has not experienced any other symptoms since returning from the trip. On presentation, he is found to have white plaques on the tongue that can be scraped off. Which of the following is a characteristic of the most likely cause of this patient's disease?
- A. Acute angle branching
- B. Spherules containing endospores
- C. Germ tube formation (Correct Answer)
- D. Latex agglutination
- E. Broad-based budding
Development of microbiome from birth Explanation: ***Germ tube formation***
- This patient presents with **oral thrush (candidiasis)**, characterized by **white plaques on the tongue that can be scraped off**. His history of **asthma and inhaler use** (likely corticosteroids) is a risk factor.
- **Germ tube formation** is a rapid diagnostic test for *Candida albicans*, the most common cause of oral thrush, where yeast cells produce filament-like extensions when incubated in serum.
*Acute angle branching*
- This is characteristic of **Aspergillus species**, which typically cause invasive mold infections in immunocompromised individuals, or allergic bronchopulmonary aspergillosis, not oral thrush.
- *Aspergillus* infections are not typically associated with easily scraped-off oral plaques.
*Spherules containing endospores*
- **Spherules containing endospores** are the characteristic tissue form of **Coccidioides immitis/posadasii**, a dimorphic fungus causing coccidioidomycosis (Valley fever), typically presenting as a pulmonary infection.
- This feature is not associated with *Candida albicans* or oral thrush, though the patient's travel history could suggest dimorphic fungal exposure.
*Latex agglutination*
- **Latex agglutination** is a serological test primarily used for detecting **cryptococcal capsular antigen** in cerebrospinal fluid or serum, indicating cryptococcosis.
- It is not a characteristic feature or primary diagnostic method for *Candida* infections like oral thrush.
*Broad-based budding*
- **Broad-based budding** is a microscopic characteristic of **Blastomyces dermatitidis**, a dimorphic fungus causing blastomycosis, typically a pulmonary infection that can disseminate to skin, bone, or other organs.
- This feature is not associated with *Candida albicans* or oral thrush.
Development of microbiome from birth US Medical PG Question 10: A 46-year-old woman comes to the physician for a 6-month history of worsening bronchial asthma control. Before this issue began, she only used her salbutamol inhaler once a day. Now, she has to use it multiple times daily and also reports frequent nighttime awakening. Seven months ago, she moved to an apartment that is damp and has mold on some of the walls. The physician injects 0.1 mL of Candida albicans extract on the mid-volar surface of the right arm intradermally. After 48 hours there is a palpable induration of 17 mm. This reaction is most likely a result of release of which of the following substances?
- A. Interleukin-10
- B. Superoxide anion
- C. Tryptase
- D. Interferon-γ (Correct Answer)
- E. Lysozyme
Development of microbiome from birth Explanation: ***Interferon-γ***
- The patient's worsened asthma, fungal exposure, and positive delayed-type hypersensitivity (DTH) skin test to *Candida albicans* suggest a **Th1-mediated immune response**.
- **Interferon-γ (IFN-γ)** is a key cytokine produced by Th1 cells, crucial for activating macrophages and cell-mediated immunity, which drives the induration observed in DTH reactions.
*Interleukin-10*
- **Interleukin-10 (IL-10)** is primarily an **anti-inflammatory cytokine** that suppresses immune responses, particularly Th1 and Th2 activity.
- Its release is associated with downregulating, rather than mediating, the robust inflammatory reaction seen in a positive DTH test.
*Superoxide anion*
- **Superoxide anion** is a reactive oxygen species produced by phagocytes (e.g., neutrophils, macrophages) as part of the **respiratory burst** to kill ingested pathogens.
- While important for host defense, it is not the primary mediator responsible for the induration and cellular infiltration characteristic of a *Candida* DTH skin test.
*Tryptase*
- **Tryptase** is an enzyme released by **mast cells** upon activation, typically during **immediate hypersensitivity reactions (Type I)**.
- Its presence is indicative of allergic reactions mediated by IgE, which manifest as wheal and flare, not the delayed induration seen in this case.
*Lysozyme*
- **Lysozyme** is an enzyme found in secretions (e.g., tears, saliva) and phagocytes, which degrades bacterial cell walls.
- It plays a role in innate immunity against bacteria but is not directly involved in the mediation of a delayed-type hypersensitivity reaction to fungal antigens.
More Development of microbiome from birth US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.