Multi-drug resistant gram-negatives US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Multi-drug resistant gram-negatives. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Multi-drug resistant gram-negatives US Medical PG Question 1: A 37-year-old woman with a history of anorectal abscesses complains of pain in the perianal region. Physical examination reveals mild swelling, tenderness, and erythema of the perianal skin. She is prescribed oral ampicillin and asked to return for follow-up. Two days later, the patient presents with a high-grade fever, syncope, and increased swelling. Which of the following would be the most common mechanism of resistance leading to the failure of antibiotic therapy in this patient?
- A. Intrinsic absence of a target site for the drug
- B. Use of an altered metabolic pathway
- C. Production of beta-lactamase enzyme (Correct Answer)
- D. Altered structural target for the drug
- E. Drug efflux pump
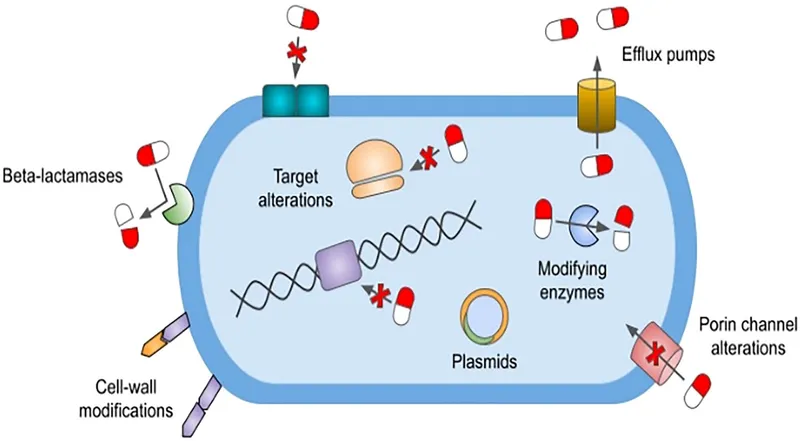
Multi-drug resistant gram-negatives Explanation: ***Production of beta-lactamase enzyme***
- The patient's symptoms of a rapidly worsening infection despite ampicillin treatment suggest the presence of a **beta-lactamase producing organism**. Ampicillin is a **beta-lactam antibiotic** that is inactivated by these enzymes.
- Anorectal abscesses and rapidly progressing soft tissue infections are often caused by **polymicrobial flora**, including staphylococci and enterococci, many of which can produce **beta-lactamase**.
*Intrinsic absence of a target site for the drug*
- While some bacteria inherently lack the target site for certain drugs (e.g., mycoplasma lacking a cell wall, thus being resistant to beta-lactams), this is less likely to be the **most common mechanism of acquired resistance** leading to treatment failure in a typical perianal infection.
- The rapid progression and failed initial treatment point towards an **acquired mechanism of resistance** rather than an intrinsic one.
*Use of an altered metabolic pathway*
- This mechanism, such as altered **folate synthesis pathways** in resistance to trimethoprim-sulfamethoxazole, is less common as the primary mechanism for ampicillin resistance.
- Ampicillin's mechanism of action primarily targets the **bacterial cell wall**, not a metabolic pathway in the same way.
*Altered structural target for the drug*
- This involves modifications to the **penicillin-binding proteins (PBPs)**, which are the targets of beta-lactam antibiotics like ampicillin. While a valid mechanism (e.g., in MRSA), the **production of beta-lactamase** is generally a more widespread and common cause of ampicillin failure, especially in infections involving mixed flora from the perianal region.
- Given the abrupt failure of ampicillin, **beta-lactamase inactivation** is a more immediate and common cause than a rapid mutational change in PBPs.
*Drug efflux pump*
- **Efflux pumps** actively remove antibiotics from the bacterial cell, contributing to resistance against various drug classes.
- While efflux pumps can play a role, the dominant mechanism for resistance to **ampicillin** in many common perianal pathogens is the **enzymatic degradation by beta-lactamases**.
Multi-drug resistant gram-negatives US Medical PG Question 2: A 42-year-old woman with a history of multiple sclerosis and recurrent urinary tract infections comes to the emergency department because of flank pain and fever. Her temperature is 38.8°C (101.8°F). Examination shows left-sided costovertebral angle tenderness. She is admitted to the hospital and started on intravenous vancomycin. Three days later, her symptoms have not improved. Urine culture shows growth of Enterococcus faecalis. Which of the following best describes the most likely mechanism of antibiotic resistance in this patient?
- A. Increased efflux across bacterial cell membranes
- B. Production of beta-lactamase
- C. Alteration of penicillin-binding proteins
- D. Alteration of peptidoglycan synthesis (Correct Answer)
- E. Alteration of ribosomal targets
Multi-drug resistant gram-negatives Explanation: ***Alteration of peptidoglycan synthesis***
- **Vancomycin** targets the **D-Ala-D-Ala terminus** on the peptidoglycan precursor, preventing cross-linking during bacterial cell wall synthesis.
- **Vancomycin resistance in Enterococcus faecalis** occurs through acquisition of resistance genes (vanA, vanB) that encode enzymes modifying the peptidoglycan precursor from **D-Ala-D-Ala to D-Ala-D-Lac**.
- This structural change reduces vancomycin's binding affinity by approximately 1000-fold, rendering the antibiotic ineffective.
- The mechanism directly involves **alteration of the peptidoglycan synthesis pathway**, specifically the terminal amino acid residues of the pentapeptide precursor.
*Increased efflux across bacterial cell membranes*
- This mechanism involves **efflux pumps that actively transport antibiotics out of the bacterial cell**, reducing intracellular concentration.
- While efflux pumps contribute to resistance for antibiotics like **tetracyclines, fluoroquinolones, and macrolides**, this is not the primary mechanism of vancomycin resistance in Enterococcus.
*Production of beta-lactamase*
- **Beta-lactamase enzymes** hydrolyze the **beta-lactam ring** of antibiotics like **penicillins and cephalosporins**, rendering them inactive.
- **Vancomycin is a glycopeptide antibiotic, not a beta-lactam**, so its efficacy is not affected by beta-lactamase production.
*Alteration of ribosomal targets*
- This mechanism confers resistance to antibiotics that target **bacterial ribosomes** to inhibit protein synthesis, such as **macrolides, aminoglycosides, and tetracyclines**.
- **Vancomycin acts on cell wall synthesis**, not protein synthesis, so alteration of ribosomal targets is not relevant to vancomycin resistance.
*Alteration of penicillin-binding proteins*
- **Penicillin-binding proteins (PBPs)** are the targets of **beta-lactam antibiotics** (penicillins, cephalosporins, carbapenems).
- Alterations in PBPs cause resistance to beta-lactams, not to vancomycin.
- **Vancomycin does not interact with PBPs**; it binds directly to the D-Ala-D-Ala terminus of peptidoglycan precursors in the cell wall.
Multi-drug resistant gram-negatives US Medical PG Question 3: A 77-year-old woman is brought to the emergency department from her nursing home because she was found down overnight. On presentation she was found to be delirious and was unable to answer questions. Chart review shows that she is allergic to cephalosporins. Her temperature is 102.2°F (39°C), blood pressure is 105/52 mmHg, pulse is 94/min, and respirations are 23/min. Physical exam reveals a productive cough. A metabolic panel is obtained with the following results:
Serum:
Na+: 135 mEq/L
Cl-: 95 mEq/L
K+: 4 mEq/L
HCO3-: 19 mEq/L
BUN: 40 mg/dL
Creatinine: 2.5 mg/dL
Glucose: 150 mg/dL
Based on these findings two different drugs are started empirically. Gram stain on a blood sample is performed showing the presence of gram-positive organisms on all samples. One of the drugs is subsequently stopped. The drug that was most likely stopped has which of the following characteristics?
- A. Resistance conveyed through acetylation
- B. Associated with red man syndrome
- C. Single-ringed ß-lactam structure (Correct Answer)
- D. Causes discolored teeth in children
- E. Accumulates inside bacteria via O2-dependent uptake
Multi-drug resistant gram-negatives Explanation: ***Single-ringed ß-lactam structure***
- The patient presents with **sepsis** due to **pneumonia** likely caused by **gram-positive organisms**. Given a cephalosporin allergy, **aztreonam** (a monobactam) would be an initial empirical antibiotic choice to cover gram-negative bacteria, alongside a drug for gram-positive coverage (like vancomycin).
- Since the **blood cultures** confirmed **gram-positive organisms**, the drug covering gram-negative bacteria (aztreonam) would be stopped. Aztreonam is characterized by its **single-ringed β-lactam structure**.
*Resistance conveyed through acetylation*
- This mechanism of resistance is typical of **aminoglycosides** (e.g., gentamicin) and **chloramphenicol**.
- Aminoglycosides were unlikely to be one of the empirically started drugs, as they are often used in combination with β-lactams, and this patient has a cephalosporin allergy.
*Associated with red man syndrome*
- **Red man syndrome** is a common adverse effect associated with **vancomycin** administration, especially with rapid infusion.
- Vancomycin would likely be continued, as it effectively targets gram-positive organisms, including **MRSA**, and is a suitable alternative given the cephalosporin allergy.
*Causes discolored teeth in children*
- This is a characteristic side effect of **tetracyclines** (e.g., doxycycline), which are contraindicated in young children and pregnant women due to their effects on bone and teeth development.
- Tetracyclines are not typically first-line empiric therapy for severe pneumonia or sepsis, especially in an elderly patient.
*Accumulates inside bacteria via O2-dependent uptake*
- This describes the mechanism of uptake for **aminoglycosides**. Their entry into bacteria is an **energy-dependent process** requiring oxygen.
- As mentioned, aminoglycosides are less likely to be the initial drug stopped in this scenario, as they target gram-negative bacteria.
Multi-drug resistant gram-negatives US Medical PG Question 4: Blood cultures are sent to the laboratory and empiric treatment with intravenous vancomycin is started. Blood cultures grow gram-negative bacilli identified as Cardiobacterium hominis. Which of the following is the most appropriate next step in management?
- A. Switch to intravenous gentamicin
- B. Switch to intravenous ampicillin
- C. Switch to intravenous ceftriaxone (Correct Answer)
- D. Switch to intravenous cefazolin
- E. Add intravenous rifampin
Multi-drug resistant gram-negatives Explanation: ***Switch to intravenous ceftriaxone***
- **Cardiobacterium hominis** is part of the **HACEK group** of bacteria, which are known for causing **endocarditis**.
- These organisms are typically susceptible to **beta-lactam antibiotics**, with **third-generation cephalosporins** like ceftriaxone being the drug of choice due to their excellent activity and good penetration.
*Switch to intravenous gentamicin*
- While **aminoglycosides** like gentamicin can be used in combination regimens for serious infections, they are generally **not monotherapy** for HACEK endocarditis and are associated with **nephrotoxicity** and **ototoxicity**.
- The primary treatment for HACEK endocarditis is a **beta-lactam antibiotic**, not an aminoglycoside alone.
*Switch to intravenous ampicillin*
- **Ampicillin** is a beta-lactam, but it may not consistently provide optimal coverage for all HACEK organisms, and some strains may have reduced susceptibility.
- **Third-generation cephalosporins** are preferred due to their broader and more consistent activity against this group.
*Switch to intravenous cefazolin*
- **Cefazolin** is a first-generation cephalosporin and typically has **limited activity** against gram-negative bacilli, especially those like Cardiobacterium hominis which require broader-spectrum beta-lactams.
- Its spectrum of activity is primarily against **gram-positive bacteria** and some **gram-negative cocci**.
*Add intravenous rifampin*
- **Rifampin** is primarily used for **mycobacterial infections** and in combination regimens for specific bacterial infections (e.g., bone and joint infections, prosthetic device infections) often due to resistant staphylococci.
- It is **not a first-line agent** for Cardiobacterium hominis infections and there's no indication for its use here with an organism susceptible to ceftriaxone.
Multi-drug resistant gram-negatives US Medical PG Question 5: A 64-year-old female with type 2 diabetes mellitus comes to the physician because of a 1-week history of painful red swelling on her left thigh. Examination shows a 3- x 4-cm, tender, fluctuant mass. Incision and drainage of the abscess are performed. Culture of the abscess fluid grows gram-positive, coagulase-positive cocci that are resistant to oxacillin. Which of the following best describes the mechanism of resistance of the causal organism to oxacillin?
- A. Degradation of the antibiotic
- B. Decreased uptake of the antibiotic
- C. Decreased activation of the antibiotic
- D. Altered target of the antibiotic (Correct Answer)
- E. Acetylation of the antibiotic
Multi-drug resistant gram-negatives Explanation: ***Altered target of the antibiotic***
- The organism described (gram-positive, coagulase-positive cocci, oxacillin-resistant) is **methicillin-resistant *Staphylococcus aureus* (MRSA)**.
- MRSA achieves oxacillin (and other beta-lactam) resistance by acquiring the ***mecA* gene**, which encodes for a **modified penicillin-binding protein (PBP2a)** with reduced affinity for beta-lactam antibiotics.
*Degradation of the antibiotic*
- This mechanism, primarily through the production of **beta-lactamase enzymes**, can degrade beta-lactam antibiotics.
- While *Staphylococcus aureus* can produce beta-lactamases, oxacillin (a **penicillinase-resistant penicillin**) is specifically engineered to be stable against these enzymes.
*Decreased uptake of the antibiotic*
- Reduced permeability of the bacterial cell wall can lead to decreased uptake, a mechanism more commonly associated with **gram-negative bacteria** due to their outer membrane.
- This is not the primary mechanism of resistance for MRSA to oxacillin.
*Decreased activation of the antibiotic*
- Some antibiotics are prodrugs that require activation by bacterial enzymes, and resistance can arise from mutations affecting this activation.
- Oxacillin is active in its administered form and does not require bacterial activation.
*Acetylation of the antibiotic*
- **Enzymatic modification**, such as acetylation, adenylylation, or phosphorylation, is a common mechanism of resistance, particularly against **aminoglycoside antibiotics**.
- This specific mechanism is not responsible for oxacillin resistance in MRSA.
Multi-drug resistant gram-negatives US Medical PG Question 6: An investigator is studying bacterial toxins in a nonpathogenic bacterial monoculture that has been inoculated with specific bacteriophages. These phages were previously cultured in a toxin-producing bacterial culture. After inoculation, a new toxin is isolated from the culture. Genetic sequencing shows that the bacteria have incorporated viral genetic information, including the gene for this toxin, into their genome. The described process is most likely responsible for acquired pathogenicity in which of the following bacteria?
- A. Staphylococcus aureus
- B. Haemophilus influenzae
- C. Neisseria meningitidis
- D. Streptococcus pneumoniae
- E. Corynebacterium diphtheriae (Correct Answer)
Multi-drug resistant gram-negatives Explanation: ***Corynebacterium diphtheriae***
- The process described, where a bacterium acquires new genetic information (e.g., a toxin gene) from a bacteriophage, is called **lysogenic conversion** or **phage conversion**. *Corynebacterium diphtheriae* is the **classic example** of this mechanism, acquiring its toxigenicity through phage-mediated transfer of the **diphtheria toxin gene (tox gene)** via bacteriophage β.
- The diphtheria toxin is an **AB toxin** that ADP-ribosylates and thereby inactivates **elongation factor 2 (EF-2)**, inhibiting host cell protein synthesis and leading to the characteristic symptoms of diphtheria.
- This is the **prototypical and most clinically significant example** of lysogenic conversion in medical microbiology.
*Staphylococcus aureus*
- While *Staphylococcus aureus* can acquire some virulence factors via bacteriophages (e.g., **Panton-Valentine leukocidin**, some enterotoxins), many of its toxins are encoded on **mobile genetic elements** such as plasmids, pathogenicity islands, or chromosomal genes.
- However, *S. aureus* is **not the classic example** of lysogenic conversion described in this scenario. *C. diphtheriae* better exemplifies the acquisition of a major toxin exclusively through phage conversion.
*Haemophilus influenzae*
- *Haemophilus influenzae* primarily causes disease through its **polysaccharide capsule** (especially type b) and is a common cause of respiratory infections and meningitis.
- Its major virulence factors are typically chromosomally encoded or acquired through **transformation** (uptake of naked DNA), not through phage conversion for a primary toxin.
*Neisseria meningitidis*
- *Neisseria meningitidis* causes meningococcal disease, primarily due to its **polysaccharide capsule** and **endotoxin (LPS)**.
- While genetic exchange can occur, the acquisition of a major toxin gene by phage conversion as described is not a primary mechanism for its key virulence factors.
*Streptococcus pneumoniae*
- *Streptococcus pneumoniae* is a leading cause of pneumonia, meningitis, and otitis media, with its main virulence factor being its **polysaccharide capsule**.
- It primarily acquires genetic material through **transformation** (competence-mediated uptake of naked DNA), which contributes to antibiotic resistance and capsule types, but lysogenic conversion with toxin acquisition is not typical for its major virulence factors.
Multi-drug resistant gram-negatives US Medical PG Question 7: A 62-year-old woman with type 2 diabetes mellitus is brought to the emergency department by her husband because of fever, chills, and purulent drainage from a foot ulcer for 2 days. Her hemoglobin A1c was 15.4% 16 weeks ago. Physical examination shows a 2-cm ulcer on the plantar surface of the left foot with foul-smelling, purulent drainage and surrounding erythema. Culture of the abscess fluid grows several bacteria species, including gram-negative, anaerobic, non-spore-forming bacilli that are resistant to bile and aminoglycoside antibiotics. Which of the following is the most likely source of this genus of bacteria?
- A. Stomach
- B. Oropharynx
- C. Vagina
- D. Colon (Correct Answer)
- E. Skin
Multi-drug resistant gram-negatives Explanation: ***Colon***
- The description of the bacteria—**gram-negative, anaerobic, non-spore-forming bacilli** that are **resistant to bile** and **aminoglycoside antibiotics**—is highly characteristic of the genus *Bacteroides*, especially *Bacteroides fragilis*.
- *Bacteroides fragilis* is a prominent component of the normal **colonic microflora** and is frequently implicated in infections originating from breaches in the gastrointestinal tract, such as a diabetic foot ulcer with a mixed infection.
*Stomach*
- The stomach's highly acidic environment generally limits significant bacterial colonization, and it is not a primary source of mixed anaerobic infections as described.
- While *Helicobacter pylori* can colonize the stomach, it does not fit the described microbiological characteristics.
*Oropharynx*
- The oropharynx contains a diverse microbiota, including anaerobes like **Peptostreptococcus** and **Fusobacterium**, but it is not the typical source for *Bacteroides fragilis* or the specific resistance profile mentioned.
- Oropharyngeal anaerobes are more commonly associated with head and neck infections, aspiration pneumonia, or dental abscesses.
*Vagina*
- The vaginal flora includes various anaerobes such as **Gardnerella vaginalis** and some *Bacteroides* species, but it is not the most common or primary source of widespread mixed anaerobic infections matching this description.
- Infections originating from the vagina would typically be linked to pelvic or genitourinary conditions.
*Skin*
- The skin surface predominantly harbors **aerobic** and **facultative anaerobic bacteria** like **Staphylococcus** and **Streptococcus** species.
- While skin breaches can lead to infections, the described **anaerobic, gram-negative, bile-resistant** profile points away from the typical skin flora as the primary source for the specific bacterial characteristics given.
Multi-drug resistant gram-negatives US Medical PG Question 8: While testing various strains of Streptococcus pneumoniae, a researcher discovers that a certain strain of this bacteria is unable to cause disease in mice when deposited in their lungs. What physiological test would most likely deviate from normal in this strain of bacteria as opposed to a typical strain?
- A. Quellung reaction (Correct Answer)
- B. Hemolytic reaction when grown on sheep blood agar
- C. Bile solubility
- D. Optochin sensitivity
- E. Motility
Multi-drug resistant gram-negatives Explanation: ***Quellung reaction***
- The **Quellung reaction** tests for the presence of the **polysaccharide capsule**, which is the primary virulence factor of *S. pneumoniae*.
- An **avirulent strain** that cannot cause disease would most likely lack the capsule and show a **negative Quellung reaction** (no capsular swelling), deviating from the **positive reaction** seen in typical encapsulated pathogenic strains.
- The capsule enables *S. pneumoniae* to evade phagocytosis and complement-mediated killing, which is essential for establishing infection in the lungs.
*Hemolytic reaction when grown on sheep blood agar*
- Both virulent and avirulent strains of *S. pneumoniae* typically exhibit **alpha-hemolysis** (partial hemolysis, producing a greenish discoloration) on sheep blood agar due to the production of pneumolysin.
- This characteristic does not differentiate between pathogenic and non-pathogenic strains in terms of disease-causing ability.
*Bile solubility*
- *S. pneumoniae* is characteristically **bile-soluble** due to the presence of autolysin enzymes that are activated by bile salts, leading to cellular lysis.
- This property is a **species characteristic** present in both virulent and avirulent strains, thus it would not explain the inability to cause disease.
*Optochin sensitivity*
- *S. pneumoniae* is universally **sensitive to optochin**, a chemical agent that inhibits its growth and is used for laboratory identification.
- This characteristic is used for **species identification** but does not correlate with strain virulence or disease-causing ability.
*Motility*
- *Streptococcus pneumoniae* is a **non-motile** bacterium; it lacks flagella.
- This characteristic is consistent across all strains and is not a virulence factor for this species.
Multi-drug resistant gram-negatives US Medical PG Question 9: A 42-year-old woman comes to the physician because of increasing pain in the right hip for 2 months. The pain is intermittent, presenting at the lateral side of the hip and radiating towards the thigh. It is aggravated while climbing stairs or lying on the right side. Two weeks ago, the patient was treated with a course of oral prednisone for exacerbation of asthma. Her current medications include formoterol-budesonide and albuterol inhalers. Vital signs are within normal limits. Examination shows tenderness to palpation over the upper lateral part of the right thigh. There is no swelling. The patient is placed in the left lateral decubitus position. Abducting the extended right leg against the physician's resistance reproduces the pain. The remainder of the examination shows no abnormalities. An x-ray of the pelvis shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Osteoarthritis of the hip
- B. Osteonecrosis of femoral head
- C. Lumbosacral radiculopathy
- D. Greater trochanteric pain syndrome (Correct Answer)
- E. Iliotibial band syndrome
Multi-drug resistant gram-negatives Explanation: ***Greater trochanteric pain syndrome***
- The patient's symptoms of **lateral hip pain** radiating to the thigh, aggravated by activity and lying on the affected side, and **tenderness over the greater trochanter** are classic for **greater trochanteric pain syndrome** (GTPS).
- Pain reproduction with **abduction against resistance** (a specific test for GTPS) and normal X-rays further support this diagnosis.
*Osteoarthritis of the hip*
- Typically causes **groin pain** that can radiate to the buttock or knee, not primarily lateral hip pain.
- X-rays would likely show signs of **joint space narrowing**, osteophytes, or subchondral sclerosis, which are absent here.
*Osteonecrosis of femoral head*
- While **corticosteroid use** is a risk factor, osteonecrosis usually presents with **groin or buttock pain** and would likely show abnormalities on X-ray (advanced stages) or MRI (early stages).
- The specific tenderness and pain reproduction with abduction against resistance are not typical for osteonecrosis.
*Lumbosacral radiculopathy*
- Would typically present with pain radiating **down the leg** in a dermatomal pattern, often accompanied by **neurological deficits** such as sensory loss, weakness, or reflex changes.
- The examination findings of isolated lateral hip tenderness and pain with resisted abduction do not support radiculopathy.
*Iliotibial band syndrome*
- More commonly affects **runners** or cyclists and causes pain along the **lateral aspect of the knee**, although it can present as lateral hip pain.
- While it can manifest with lateral hip pain, the focal tenderness over the greater trochanter and pain on resisted abduction make **GTPS** a more precise diagnosis.
Multi-drug resistant gram-negatives US Medical PG Question 10: A 31-year-old woman makes an appointment with a fertility specialist because she has not been able to conceive despite trying for over a year with her husband. She is concerned because her husband has 2 children from a previous marriage whereas she has no children. After obtaining a detailed history as well as lab tests, the specialist prescribes a certain drug. Interestingly, this drug is able to stimulate receptors in the presence of low hormone levels and inhibit the same receptors in the presence of high hormone levels. The drug that is most likely being prescribed in this case is associated with which of the following adverse events?
- A. Hirsutism
- B. Deep venous thrombosis
- C. Thrombophilia
- D. Osteoporosis
- E. Visual disturbances (Correct Answer)
Multi-drug resistant gram-negatives Explanation: ***Visual disturbances***
- The description of the drug activating receptors in low hormone states and inhibiting them in high hormone states, coupled with its use for infertility, strongly suggests **clomiphene citrate**, a selective estrogen receptor modulator (SERM).
- **Visual disturbances** such as blurred vision, scotomas, or photopsia are a relatively common adverse effect of clomiphene due to its effect on estrogen receptors in the retina.
*Hirsutism*
- **Hirsutism** (excessive hair growth) is typically associated with conditions causing androgen excess, like **polycystic ovary syndrome (PCOS)**, and is not a direct common adverse effect of clomiphene.
- While clomiphene aims to induce ovulation, it does not directly cause an increase in androgens leading to hirsutism.
*Deep venous thrombosis*
- Although some hormonal treatments can increase the risk of **DVT**, clomiphene's association with DVT is **not as primary or common** as other adverse effects, and it's less direct compared to estrogen-containing medications.
- The mechanism of action of clomiphene as a SERM modulating estrogen receptors does not typically lead to a significant procoagulant state comparable to exogenous estrogen.
*Thrombophilia*
- **Thrombophilia** refers to an increased tendency to form blood clots; while some hormonal medications can exacerbate thrombophilia, clomiphene is **not generally recognized** for causing thrombophilia or significantly increasing its risk.
- Its mechanism of action primarily involves stimulating gonadotropin release rather than directly altering coagulation factors to induce thrombophilia.
*Osteoporosis*
- While **estrogen deficiency** can lead to osteoporosis, clomiphene's role is to modulate estrogen receptors; it can cause some anti-estrogenic effects, but **osteoporosis is not a common acute or direct adverse event** of its short-term use for fertility.
- Long-term use of anti-estrogenic drugs like tamoxifen can increase osteoporosis risk, but clomiphene is typically used for a limited duration, making osteoporosis less relevant as an immediate adverse event.
More Multi-drug resistant gram-negatives US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.