Beta-lactamase types and mechanisms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Beta-lactamase types and mechanisms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Beta-lactamase types and mechanisms US Medical PG Question 1: A 37-year-old woman with a history of anorectal abscesses complains of pain in the perianal region. Physical examination reveals mild swelling, tenderness, and erythema of the perianal skin. She is prescribed oral ampicillin and asked to return for follow-up. Two days later, the patient presents with a high-grade fever, syncope, and increased swelling. Which of the following would be the most common mechanism of resistance leading to the failure of antibiotic therapy in this patient?
- A. Intrinsic absence of a target site for the drug
- B. Use of an altered metabolic pathway
- C. Production of beta-lactamase enzyme (Correct Answer)
- D. Altered structural target for the drug
- E. Drug efflux pump
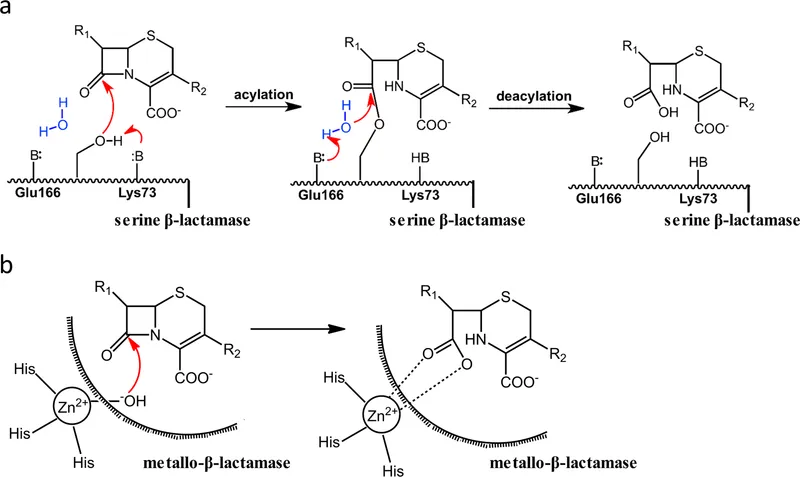
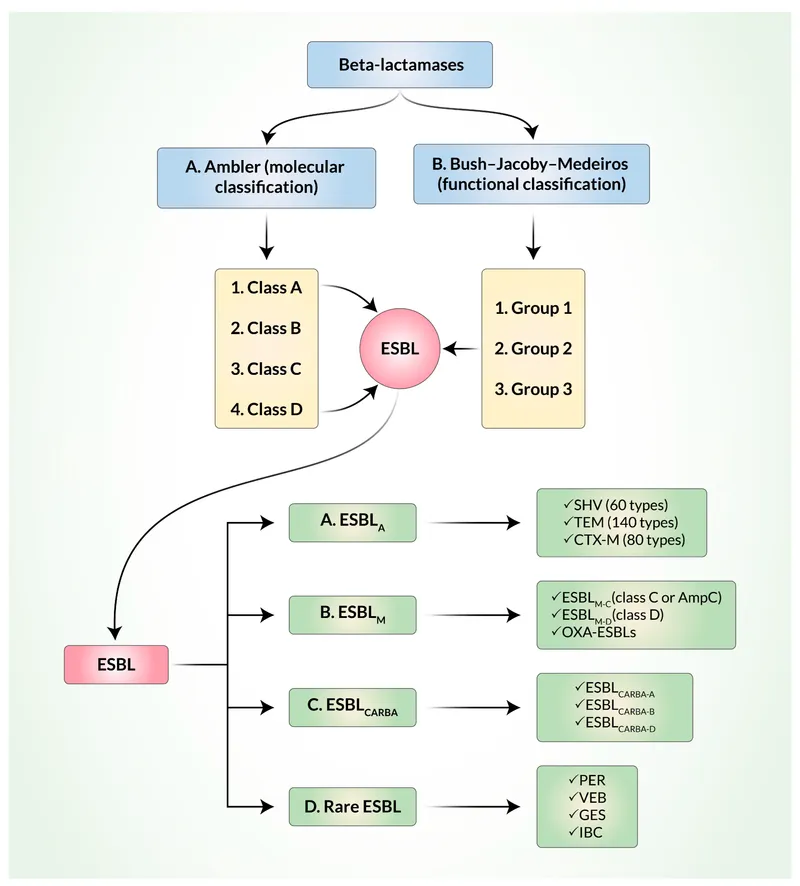
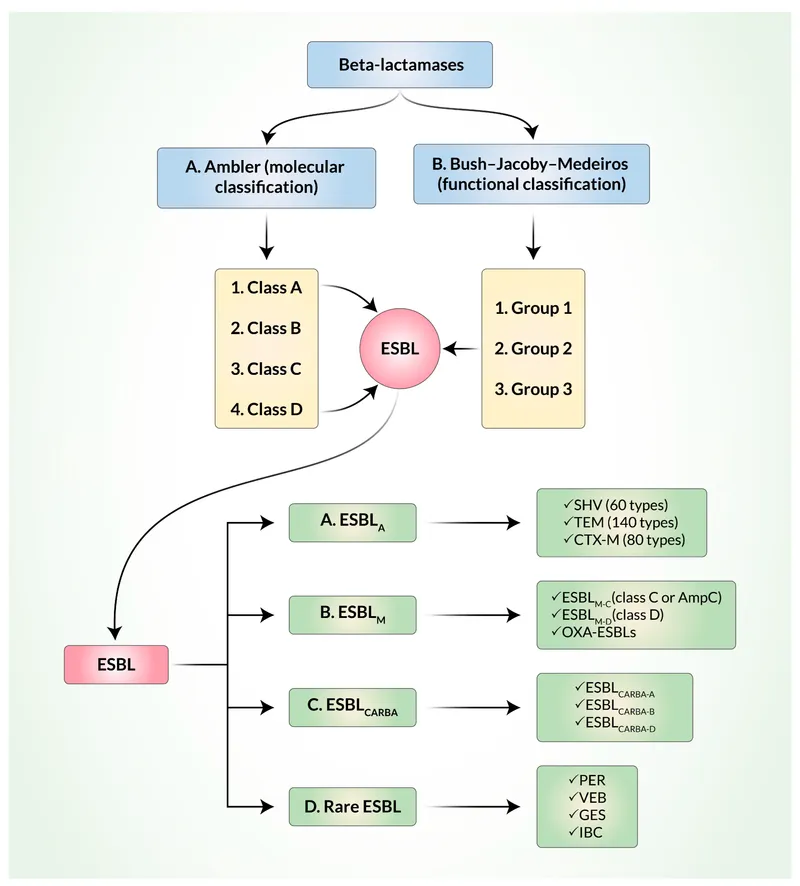
Beta-lactamase types and mechanisms Explanation: ***Production of beta-lactamase enzyme***
- The patient's symptoms of a rapidly worsening infection despite ampicillin treatment suggest the presence of a **beta-lactamase producing organism**. Ampicillin is a **beta-lactam antibiotic** that is inactivated by these enzymes.
- Anorectal abscesses and rapidly progressing soft tissue infections are often caused by **polymicrobial flora**, including staphylococci and enterococci, many of which can produce **beta-lactamase**.
*Intrinsic absence of a target site for the drug*
- While some bacteria inherently lack the target site for certain drugs (e.g., mycoplasma lacking a cell wall, thus being resistant to beta-lactams), this is less likely to be the **most common mechanism of acquired resistance** leading to treatment failure in a typical perianal infection.
- The rapid progression and failed initial treatment point towards an **acquired mechanism of resistance** rather than an intrinsic one.
*Use of an altered metabolic pathway*
- This mechanism, such as altered **folate synthesis pathways** in resistance to trimethoprim-sulfamethoxazole, is less common as the primary mechanism for ampicillin resistance.
- Ampicillin's mechanism of action primarily targets the **bacterial cell wall**, not a metabolic pathway in the same way.
*Altered structural target for the drug*
- This involves modifications to the **penicillin-binding proteins (PBPs)**, which are the targets of beta-lactam antibiotics like ampicillin. While a valid mechanism (e.g., in MRSA), the **production of beta-lactamase** is generally a more widespread and common cause of ampicillin failure, especially in infections involving mixed flora from the perianal region.
- Given the abrupt failure of ampicillin, **beta-lactamase inactivation** is a more immediate and common cause than a rapid mutational change in PBPs.
*Drug efflux pump*
- **Efflux pumps** actively remove antibiotics from the bacterial cell, contributing to resistance against various drug classes.
- While efflux pumps can play a role, the dominant mechanism for resistance to **ampicillin** in many common perianal pathogens is the **enzymatic degradation by beta-lactamases**.
Beta-lactamase types and mechanisms US Medical PG Question 2: A 42-year-old woman with a history of multiple sclerosis and recurrent urinary tract infections comes to the emergency department because of flank pain and fever. Her temperature is 38.8°C (101.8°F). Examination shows left-sided costovertebral angle tenderness. She is admitted to the hospital and started on intravenous vancomycin. Three days later, her symptoms have not improved. Urine culture shows growth of Enterococcus faecalis. Which of the following best describes the most likely mechanism of antibiotic resistance in this patient?
- A. Increased efflux across bacterial cell membranes
- B. Production of beta-lactamase
- C. Alteration of penicillin-binding proteins
- D. Alteration of peptidoglycan synthesis (Correct Answer)
- E. Alteration of ribosomal targets
Beta-lactamase types and mechanisms Explanation: ***Alteration of peptidoglycan synthesis***
- **Vancomycin** targets the **D-Ala-D-Ala terminus** on the peptidoglycan precursor, preventing cross-linking during bacterial cell wall synthesis.
- **Vancomycin resistance in Enterococcus faecalis** occurs through acquisition of resistance genes (vanA, vanB) that encode enzymes modifying the peptidoglycan precursor from **D-Ala-D-Ala to D-Ala-D-Lac**.
- This structural change reduces vancomycin's binding affinity by approximately 1000-fold, rendering the antibiotic ineffective.
- The mechanism directly involves **alteration of the peptidoglycan synthesis pathway**, specifically the terminal amino acid residues of the pentapeptide precursor.
*Increased efflux across bacterial cell membranes*
- This mechanism involves **efflux pumps that actively transport antibiotics out of the bacterial cell**, reducing intracellular concentration.
- While efflux pumps contribute to resistance for antibiotics like **tetracyclines, fluoroquinolones, and macrolides**, this is not the primary mechanism of vancomycin resistance in Enterococcus.
*Production of beta-lactamase*
- **Beta-lactamase enzymes** hydrolyze the **beta-lactam ring** of antibiotics like **penicillins and cephalosporins**, rendering them inactive.
- **Vancomycin is a glycopeptide antibiotic, not a beta-lactam**, so its efficacy is not affected by beta-lactamase production.
*Alteration of ribosomal targets*
- This mechanism confers resistance to antibiotics that target **bacterial ribosomes** to inhibit protein synthesis, such as **macrolides, aminoglycosides, and tetracyclines**.
- **Vancomycin acts on cell wall synthesis**, not protein synthesis, so alteration of ribosomal targets is not relevant to vancomycin resistance.
*Alteration of penicillin-binding proteins*
- **Penicillin-binding proteins (PBPs)** are the targets of **beta-lactam antibiotics** (penicillins, cephalosporins, carbapenems).
- Alterations in PBPs cause resistance to beta-lactams, not to vancomycin.
- **Vancomycin does not interact with PBPs**; it binds directly to the D-Ala-D-Ala terminus of peptidoglycan precursors in the cell wall.
Beta-lactamase types and mechanisms US Medical PG Question 3: An 18-year old college freshman presents to his university clinic because he has not been feeling well for the past two weeks. He has had a persistent headache, occasional cough, and chills without rigors. The patient’s vital signs are normal and physical exam is unremarkable. His radiograph shows patchy interstitial lung infiltrates and he is diagnosed with atypical pneumonia. The patient is prescribed azithromycin and takes his medication as instructed. Despite adherence to his drug regimen, he returns to the clinic one week later because his symptoms have not improved. The organism responsible for this infection is likely resistant to azithromycin through which mechanism?
- A. Mutation in topoisomerase II
- B. Methylation of ribosomal binding site
- C. Presence of a beta-lactamase
- D. Decreased binding to RNA polymerase
- E. Insertion of drug efflux pumps (Correct Answer)
Beta-lactamase types and mechanisms Explanation: ***Insertion of drug efflux pumps***
- **Azithromycin** is a macrolide antibiotic that inhibits bacterial protein synthesis by binding to the **50S ribosomal subunit**.
- In **Mycoplasma pneumoniae** (the most common cause of atypical pneumonia in young adults), the **most common** mechanism of macrolide resistance is through **efflux pumps**, particularly the **mef genes**.
- These efflux pumps actively transport macrolides out of the bacterial cell, reducing intracellular drug concentration and conferring resistance.
- This mechanism is responsible for the majority of macrolide-resistant *M. pneumoniae* isolates worldwide.
*Methylation of ribosomal binding site*
- **Methylation** of the ribosomal binding site (specifically the **23S rRNA** via erm genes) does prevent azithromycin from binding effectively.
- While this is a valid macrolide resistance mechanism seen in organisms like *Streptococcus pneumoniae* and *Streptococcus pyogenes*, it is **less common** in *Mycoplasma pneumoniae*.
- Efflux pumps (mef) are the predominant mechanism in *M. pneumoniae* resistant strains.
*Mutation in topoisomerase II*
- **Topoisomerase II** (DNA gyrase) is the target of **fluoroquinolone antibiotics**, not macrolides.
- Mutations in this enzyme lead to resistance against fluoroquinolones, such as **ciprofloxacin**.
*Presence of a beta-lactamase*
- **Beta-lactamase enzymes** inactivate **beta-lactam antibiotics** (e.g., penicillin, cephalosporins) by hydrolyzing their beta-lactam ring.
- Additionally, *Mycoplasma pneumoniae* **lacks a cell wall**, making it inherently resistant to all beta-lactam antibiotics regardless of beta-lactamase production.
*Decreased binding to RNA polymerase*
- **RNA polymerase** is the target for antibiotics like **rifampin**, which inhibits bacterial transcription.
- Decreased binding to RNA polymerase would lead to rifampin resistance, not azithromycin resistance.
Beta-lactamase types and mechanisms US Medical PG Question 4: A 64-year-old female with type 2 diabetes mellitus comes to the physician because of a 1-week history of painful red swelling on her left thigh. Examination shows a 3- x 4-cm, tender, fluctuant mass. Incision and drainage of the abscess are performed. Culture of the abscess fluid grows gram-positive, coagulase-positive cocci that are resistant to oxacillin. Which of the following best describes the mechanism of resistance of the causal organism to oxacillin?
- A. Degradation of the antibiotic
- B. Decreased uptake of the antibiotic
- C. Decreased activation of the antibiotic
- D. Altered target of the antibiotic (Correct Answer)
- E. Acetylation of the antibiotic
Beta-lactamase types and mechanisms Explanation: ***Altered target of the antibiotic***
- The organism described (gram-positive, coagulase-positive cocci, oxacillin-resistant) is **methicillin-resistant *Staphylococcus aureus* (MRSA)**.
- MRSA achieves oxacillin (and other beta-lactam) resistance by acquiring the ***mecA* gene**, which encodes for a **modified penicillin-binding protein (PBP2a)** with reduced affinity for beta-lactam antibiotics.
*Degradation of the antibiotic*
- This mechanism, primarily through the production of **beta-lactamase enzymes**, can degrade beta-lactam antibiotics.
- While *Staphylococcus aureus* can produce beta-lactamases, oxacillin (a **penicillinase-resistant penicillin**) is specifically engineered to be stable against these enzymes.
*Decreased uptake of the antibiotic*
- Reduced permeability of the bacterial cell wall can lead to decreased uptake, a mechanism more commonly associated with **gram-negative bacteria** due to their outer membrane.
- This is not the primary mechanism of resistance for MRSA to oxacillin.
*Decreased activation of the antibiotic*
- Some antibiotics are prodrugs that require activation by bacterial enzymes, and resistance can arise from mutations affecting this activation.
- Oxacillin is active in its administered form and does not require bacterial activation.
*Acetylation of the antibiotic*
- **Enzymatic modification**, such as acetylation, adenylylation, or phosphorylation, is a common mechanism of resistance, particularly against **aminoglycoside antibiotics**.
- This specific mechanism is not responsible for oxacillin resistance in MRSA.
Beta-lactamase types and mechanisms US Medical PG Question 5: An investigator is studying a strain of bacteria that retains a blue color after crystal violet dye and acetone are applied. The bacteria are inoculated in a petri dish containing hypotonic saline. After the addition of an antibiotic, the bacteria swell and rupture. This antibiotic most likely belongs to which of the following classes?
- A. Macrolide
- B. Cephalosporin (Correct Answer)
- C. Sulfonamide
- D. Fluoroquinolone
- E. Tetracycline
Beta-lactamase types and mechanisms Explanation: ***Cephalosporin***
- This scenario describes a **Gram-positive bacterium** (retains blue color) which, after antibiotic treatment, swells and lyses in a hypotonic solution. This indicates a defect in the **peptidoglycan cell wall**.
- **Cephalosporins** are **β-lactam antibiotics** that inhibit bacterial cell wall synthesis by interfering with **peptidoglycan cross-linking**, leading to osmotic lysis in hypotonic environments.
*Macrolide*
- Macrolides like **azithromycin** and **erythromycin** inhibit bacterial **protein synthesis** by binding to the 50S ribosomal subunit.
- They do not directly target the cell wall, so they would not cause immediate osmotic lysis in this manner.
*Sulfonamide*
- Sulfonamides inhibit bacterial **folic acid synthesis** by acting as a competitive inhibitor of dihydropteroate synthase, disrupting DNA and RNA production.
- Their mechanism of action does not involve direct cell wall disruption or osmotic lysis.
*Fluoroquinolone*
- Fluoroquinolones interfere with bacterial **DNA replication and transcription** by inhibiting **DNA gyrase** and **topoisomerase IV**.
- This class of antibiotics does not primarily target the cell wall, and therefore would not lead to prompt osmotic swelling and rupture.
*Tetracycline*
- Tetracyclines inhibit bacterial **protein synthesis** by binding to the 30S ribosomal subunit, preventing the attachment of aminoacyl-tRNA.
- They do not affect the cell wall, so they would not cause the observed osmotic lysis.
Beta-lactamase types and mechanisms US Medical PG Question 6: A 15-year-old African-American male with a BMI of 22 is brought to his physician by his mother to address concerns about a change in his dietary habits. The patient's mother notes that he is constantly hungry and thirsty, despite his eating and drinking water in excess. She also reports an increase in his use of the bathroom. The physician begins explaining that her son's symptoms are likely due to which of the following?
- A. Pancreatic islet hyperplasia and hypertrophy
- B. The patient's weight
- C. Insulitis (Correct Answer)
- D. Amyloid deposition in pancreatic islets
- E. Insensitivity to insulin
Beta-lactamase types and mechanisms Explanation: ***Insulitis***
- This patient's symptoms of **polyphagia**, **polydipsia**, and **polyuria** are classic for **Type 1 Diabetes Mellitus (T1DM)**.
- **Insulitis** is the characteristic autoimmune inflammation of the pancreatic islets that destroys insulin-producing beta cells in T1DM.
*Pancreatic islet hyperplasia and hypertrophy*
- This is typically seen in conditions of **chronic insulin resistance**, such as early **Type 2 Diabetes Mellitus**, as the body attempts to compensate for increased insulin demand.
- It does not explain the acute onset of classic diabetic symptoms in a lean adolescent.
*The patient's weight*
- With a **BMI of 22**, the patient is within a healthy weight range and is not considered overweight or obese.
- While obesity is a major risk factor for **Type 2 Diabetes**, it is not typical for **Type 1 Diabetes**.
*Amyloid deposition in pancreatic islets*
- **Amyloid deposition**, specifically from **islet amyloid polypeptide (IAPP)**, is a pathological hallmark of **Type 2 Diabetes Mellitus**, not Type 1.
- This process contributes to beta-cell dysfunction and death in Type 2 Diabetes, but is secondary to the disease process, not the primary autoimmune destruction seen in Type 1.
*Insensitivity to insulin*
- **Insulin insensitivity** or **insulin resistance** is the defining feature of **Type 2 Diabetes Mellitus**.
- This patient's presentation of sudden symptoms in a lean adolescent strongly points to an absolute **deficiency of insulin**, not resistance.
Beta-lactamase types and mechanisms US Medical PG Question 7: A group of microbiological investigators is studying bacterial DNA replication in E. coli colonies. While the cells are actively proliferating, the investigators stop the bacterial cell cycle during S phase and isolate an enzyme involved in DNA replication. An assay of the enzyme's exonuclease activity determines that it is active on both intact and demethylated thymine nucleotides. Which of the following enzymes have the investigators most likely isolated?
- A. DNA ligase
- B. Telomerase
- C. Primase
- D. DNA topoisomerase
- E. DNA polymerase I (Correct Answer)
Beta-lactamase types and mechanisms Explanation: ***DNA polymerase I***
- **DNA polymerase I** possesses **5' to 3' exonuclease activity**, which is crucial for removing **RNA primers** (intact nucleotides) laid down by primase during DNA replication.
- This 5' to 3' exonuclease activity also allows it to excise damaged DNA, including DNA containing **demethylated thymine nucleotides**.
- It also has 3' to 5' exonuclease activity for proofreading.
- **Key distinction:** While DNA polymerase III (the main replicative enzyme) only has 3' to 5' exonuclease activity, DNA polymerase I has **both** 3' to 5' and 5' to 3' exonuclease activities, making it essential for primer removal and DNA repair.
*DNA ligase*
- **DNA ligase** functions to form a **phosphodiester bond** between adjacent nucleotides to seal nicks in the DNA backbone, but it does not have exonuclease activity.
- Its primary role is in joining Okazaki fragments and repairing single-strand breaks.
*Telomerase*
- **Telomerase** is a specialized reverse transcriptase that extends the telomeres at the ends of eukaryotic chromosomes, but is not present in prokaryotes like *E. coli*.
- It uses an RNA template to synthesize DNA, and it lacks exonuclease activity.
*Primase*
- **Primase** is an RNA polymerase that synthesizes short **RNA primers** on the DNA template, providing a starting point for DNA synthesis.
- It is involved in synthesizing primers, not in removing or excising nucleotides, and has no exonuclease activity.
*DNA topoisomerase*
- **DNA topoisomerases** relieve supercoiling in DNA during replication and transcription by cutting and rejoining DNA strands.
- While they act on DNA, their function is to manage topological stress, and they do not exhibit exonuclease activity on nucleotides.
Beta-lactamase types and mechanisms US Medical PG Question 8: A 27-year-old woman presents to the clinic with severe pain in her left knee of 1-day duration. Physical examination reveals a red, swollen, warm, and tender left knee with a decreased range of motion. The patient affirms that she has been sexually active with several partners over the last year and that 1 of her partners has complained of dysuria and yellow urethral discharge. An arthrocentesis was performed and showed a WBC count of 60,000/µL, with 90% polymorphonuclear leukocytes. Visualization of the patient's synovial fluid is provided in the image. Which of the following is a characteristic feature of the organism causing this condition?
- A. It causes the Jarisch-Herxheimer reaction when treated with penicillin
- B. It produces a heat-labile toxin that prevents protein synthesis
- C. It selectively grows on Thayer-Martin medium (Correct Answer)
- D. It is a gram-positive diplococcus
- E. It ferments maltose
Beta-lactamase types and mechanisms Explanation: ***It selectively grows on Thayer-Martin medium***
- The patient's presentation with **septic arthritis**, a history of multiple sexual partners, and a partner with symptoms of **urethritis** suggests **gonococcal arthritis** caused by *Neisseria gonorrhoeae*.
- *Neisseria gonorrhoeae* is a fastidious organism that requires an enriched selective medium like **Thayer-Martin agar** for optimal growth, which contains antimicrobial agents to inhibit commensal flora.
*It causes the Jarisch-Herxheimer reaction when treated with penicillin*
- The **Jarisch-Herxheimer reaction** is typically associated with treatment of **spirochetal diseases** like **syphilis** (caused by *Treponema pallidum)* or **Lyme disease** (caused by *Borrelia burgdorferi*) with penicillin.
- This reaction results from the rapid lysis of spirochetes and the release of endotoxins, which is not characteristic of gonococcal infection or its treatment.
*It produces a heat-labile toxin that prevents protein synthesis*
- This description is characteristic of toxins produced by organisms like **diphtheria toxin** (*Corynebacterium diphtheriae*) or **Shiga toxin** (*Shigella dysenteriae* and enterohemorrhagic *E. coli*), which inhibit protein synthesis but are not associated with *Neisseria gonorrhoeae*.
- *Neisseria gonorrhoeae* possesses virulence factors like pili, Opa proteins, and LOS, but its primary pathogenicity mechanism does not involve a heat-labile toxin that prevents protein synthesis.
*It is a gram-positive diplococcus*
- The image clearly shows **gram-negative diplococci** within phagocytes (neutrophils), which is a classic microscopic finding for *Neisseria gonorrhoeae*.
- *Neisseria gonorrhoeae* is specifically a **Gram-negative organism**, not Gram-positive.
*It ferments maltose*
- *Neisseria gonorrhoeae* metabolizes **glucose only** and does not ferment maltose, which helps differentiate it from *Neisseria meningitidis* (which ferments both glucose and maltose).
- This metabolic characteristic is a key biochemical test used in the laboratory for the identification of *Neisseria* species.
Beta-lactamase types and mechanisms US Medical PG Question 9: A 29-year-old pregnant woman with no prior antibiotic exposure presents with gonorrhea. Culture of Neisseria gonorrhoeae shows resistance to penicillin, tetracycline, and fluoroquinolones. Genetic testing reveals she has a strain with chromosomal mutations in penA (mosaic allele), mtrR promoter, and gyrA. She reports her partner recently returned from Southeast Asia. Apply epidemiologic and resistance mechanism knowledge to determine the most appropriate management and public health action.
- A. Treat with ceftriaxone alone and report to local health department
- B. Treat with dual therapy (ceftriaxone plus azithromycin) and initiate partner notification with travel history documentation (Correct Answer)
- C. Perform cephalosporin susceptibility testing before treatment initiation
- D. Treat with azithromycin monotherapy due to pregnancy
- E. Initiate spectinomycin therapy and routine partner notification only
Beta-lactamase types and mechanisms Explanation: ***Treat with dual therapy (ceftriaxone plus azithromycin) and initiate partner notification with travel history documentation***
- The presence of the **mosaic penA allele** and **mtrR promoter mutations** signifies significant resistance potential; **dual therapy** with ceftriaxone and azithromycin remains critical for ensuring cure and slowing further resistance in highly resistant strains.
- Given the partner's travel to **Southeast Asia**, a region known for emerging **extensively drug-resistant (XDR)** gonorrhea, documenting travel and notification is vital for public health **surveillance**.
*Treat with ceftriaxone alone and report to local health department*
- While ceftriaxone is the backbone of treatment, using **monotherapy** for a strain already exhibiting multiple chromosomal resistance mutations (mosaic penA) increases the risk of selecting for **cephalosporin resistance**.
- This approach is less robust than dual therapy in the context of suspected **imported resistant strains** from high-risk geographic regions.
*Perform cephalosporin susceptibility testing before treatment initiation*
- Delaying treatment for **Neisseria gonorrhoeae** waiting for susceptibility results is inappropriate as it allows for ongoing **transmission** and potential progression to **pelvic inflammatory disease**.
- Clinical guidelines recommend **empiric treatment** based on local prevalence and travel history while simultaneously performing surveillance cultures.
*Treat with azithromycin monotherapy due to pregnancy*
- **Azithromycin monotherapy** is contraindicated for gonorrhea treatment because it has a low barrier to resistance and would fail to cover chromosomal mutations affecting **efflux pumps (mtrR)**.
- While both drugs are safe in **pregnancy**, azithromycin must be used in **combination** with ceftriaxone to prevent treatment failure.
*Initiate spectinomycin therapy and routine partner notification only*
- **Spectinomycin** is a second-line agent that is currently not readily available in the United States and has poor efficacy for **pharyngeal infections**.
- Focusing only on routine notification ignores the critical **epidemiologic significance** of the Southeast Asian travel history associated with highly resistant strains.
Beta-lactamase types and mechanisms US Medical PG Question 10: A 67-year-old woman with persistent Enterococcus faecium bacteremia despite appropriate vancomycin therapy undergoes repeat culture. The isolate now shows vancomycin MIC of 128 μg/mL (previously 2 μg/mL). PCR testing reveals the presence of vanA gene cluster. Hospital epidemiology traces potential sources. What is the most likely mechanism by which this organism acquired high-level vancomycin resistance?
- A. Spontaneous chromosomal mutation during therapy
- B. Transposon-mediated transfer from vancomycin-resistant enterococci (Correct Answer)
- C. Transformation with DNA from lysed resistant bacteria
- D. Increased vancomycin efflux pump expression
- E. Alteration in cell wall synthesis without genetic acquisition
Beta-lactamase types and mechanisms Explanation: ***Transposon-mediated transfer from vancomycin-resistant enterococci***
- High-level vancomycin resistance in Enterococcus is primarily mediated by the **vanA gene cluster**, which is carried on the **Tn1546 transposon** and spread via **conjugation**.
- This mechanism involves the replacement of the terminal **D-Ala-D-Ala** of peptidoglycan precursors with **D-Ala-D-Lac**, resulting in a 1000-fold decrease in vancomycin binding affinity.
*Spontaneous chromosomal mutation during therapy*
- While mutations can cause resistance to some antibiotics (like rifampin), **high-level vancomycin resistance** in enterococci is not caused by single-point mutations.
- A sudden jump in MIC from 2 to 128 μg/mL is characteristic of **horizontal gene transfer** rather than the gradual accumulation of chromosomal mutations.
*Transformation with DNA from lysed resistant bacteria*
- **Transformation** (uptake of naked DNA) is less common in enterococci compared to **conjugation** for the transfer of large, complex gene clusters like **vanA**.
- The epidemiological tracing implied in the scenario is classic for the spread of **plasmids** and **transposons** between colonized patients in a hospital setting.
*Increased vancomycin efflux pump expression*
- **Efflux pumps** are significant for resistance against drugs like tetracyclines or fluoroquinolones, but they are not the mechanism for **vancomycin resistance**.
- Vancomycin is a large **glycopeptide molecule**; resistance is achieved through **structural modification** of its target (cell wall precursors) rather than active expulsion.
*Alteration in cell wall synthesis without genetic acquisition*
- Vancomycin-intermediate S. aureus (**VISA**) involves cell wall thickening without new gene acquisition, but this results in a **smaller, gradual MIC increase**.
- The detection of the **vanA gene** by PCR confirms that the resistance is due to **acquired genetic material** rather than a purely metabolic or adaptive physiological change.
More Beta-lactamase types and mechanisms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.