Ventilator-associated pneumonia US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Ventilator-associated pneumonia. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Ventilator-associated pneumonia US Medical PG Question 1: A patient is hospitalized for pneumonia. Gram-positive cocci in clusters are seen on sputum gram stain. Which of the following clinical scenarios is most commonly associated with this form of pneumonia?
- A. Elderly patient who has trouble swallowing and poor dentition
- B. An alcoholic with evidence of empyema and "currant jelly sputum"
- C. An otherwise healthy young adult with a week of mild fatigue, chills, and cough
- D. Hospitalized adult with development of pneumonia symptoms 2 weeks following a viral illness (Correct Answer)
- E. HIV positive adult with a CD4 count less than 150 and an impaired diffusion capacity
Ventilator-associated pneumonia Explanation: ***Hospitalized adult with development of pneumonia symptoms 2 weeks following a viral illness***
- Gram-positive cocci in clusters suggests **Staphylococcus aureus**, which is a common cause of secondary bacterial pneumonia, often following **viral illnesses** (e.g., influenza).
- This scenario represents a classic presentation of **secondary bacterial pneumonia**, where the initial viral infection compromises the respiratory defenses, allowing bacterial superinfection.
*Elderly patient who has trouble swallowing and poor dentition*
- This scenario points towards **aspiration pneumonia**, often caused by a **polymicrobial infection** that includes oral anaerobes, not typically dominated by Gram-positive cocci in clusters.
- While *S. aureus* can cause aspiration pneumonia, the primary concern in this context would be **anaerobic bacteria**, given the aspiration risk factors.
*An alcoholic with evidence of empyema and \"currant jelly sputum\"*
- This description is highly suggestive of **Klebsiella pneumoniae** infection, which typically presents with thick, gelatinous, and often **blood-tinged sputum**.
- **Klebsiella** is a Gram-negative rod, not Gram-positive cocci in clusters.
*An otherwise healthy young adult with a week of mild fatigue, chills, and cough*
- This presentation is more consistent with **atypical pneumonia** caused by organisms like **Mycoplasma pneumoniae** or **Chlamydophila pneumoniae**, which would not show Gram-positive cocci in clusters on sputum stain.
- **Streptococcus pneumoniae** (Gram-positive cocci in chains) can also cause community-acquired pneumonia in otherwise healthy individuals, but the "clusters" indicate **Staphylococcus aureus**.
*HIV positive adult with a CD4 count less than 150 and an impaired diffusion capacity*
- This clinical picture strongly suggests **Pneumocystis jirovecii pneumonia (PJP)**, which is common in severely immunocompromised HIV patients.
- *P. jirovecii* is a fungus and would not be seen as Gram-positive cocci in clusters on a routine Gram stain.
Ventilator-associated pneumonia US Medical PG Question 2: A 69-year-old man is brought to the emergency department by his wife because of fever, cough, diarrhea, and confusion for 2 days. He recently returned from a cruise to the Caribbean. He has a history of chronic obstructive pulmonary disease. He has smoked one pack of cigarettes daily for 40 years. His temperature is 39.1°C (102.4°F), pulse is 83/min, and blood pressure is 111/65 mm Hg. He is confused and oriented only to person. Physical examination shows coarse crackles throughout both lung fields. His serum sodium concentration is 125 mEq/L. Culture of the most likely causal organism would require which of the following mediums?
- A. Charcoal yeast extract agar (Correct Answer)
- B. Eosin-methylene blue agar
- C. Mannitol salt agar
- D. Chocolate agar
- E. Eaton agar
Ventilator-associated pneumonia Explanation: ***Charcoal yeast extract agar***
- The patient's symptoms (fever, cough, diarrhea, confusion, hyponatremia) and risk factors (COPD, smoking history, recent cruise travel) are highly suggestive of **Legionnaires' disease** caused by *Legionella pneumophila*.
- *Legionella* is a fastidious organism that requires **cysteine** and **iron salts** for growth, which are provided in **buffered charcoal yeast extract (BCYE) agar**.
*Eosin-methylene blue agar*
- This is a **selective and differential medium** used for the isolation and differentiation of **Gram-negative enteric bacteria**, particularly useful for identifying coliforms like *E. coli*.
- It contains dyes that inhibit Gram-positive bacteria and differentiate lactose fermenters, which is not relevant for *Legionella*.
*Mannitol salt agar*
- This is a **selective and differential medium** primarily used for the isolation and identification of **staphylococci**, especially *Staphylococcus aureus*.
- It contains a high salt concentration to inhibit most bacteria and mannitol to differentiate *S. aureus* (which ferments mannitol) from other staphylococci.
*Chocolate agar*
- This enriched medium is used for the isolation of fastidious bacteria such as **Haemophilus influenzae** and **Neisseria species**, which require factors like **hemin (X factor)** and **NAD (V factor)**.
- While it supports the growth of many pathogenic bacteria, it does not provide the specific growth requirements for *Legionella*.
*Eaton agar*
- This specialized medium is primarily used for the isolation and cultivation of **Mycoplasma pneumoniae**, a common cause of "walking pneumonia."
- *Mycoplasma pneumoniae* is a bacterium that lacks a cell wall and has unique growth requirements, distinct from *Legionella*.
Ventilator-associated pneumonia US Medical PG Question 3: A 3-month-old boy is brought to the emergency room by his mother for 2 days of difficulty breathing. He was born at 35 weeks gestation but has otherwise been healthy. She noticed a cough and some trouble breathing in the setting of a runny nose. His temperature is 100°F (37.8°C), blood pressure is 64/34 mmHg, pulse is 140/min, respirations are 39/min, and oxygen saturation is 93% on room air. Pulmonary exam is notable for expiratory wheezing and crackles throughout and intercostal retractions. Oral mucosa is noted to be dry. Which of the following is the most appropriate diagnostic test?
- A. Chest radiograph
- B. Sputum culture
- C. Viral culture
- D. Polymerase chain reaction
- E. No further testing needed (Correct Answer)
Ventilator-associated pneumonia Explanation: ***No further testing needed***
- This patient presents with classic signs and symptoms of **bronchiolitis**, including a **preterm infant** (risk factor), **URI symptoms** followed by **respiratory distress** (cough, difficulty breathing), **expiratory wheezing**, and **crackles**.
- Bronchiolitis is a clinical diagnosis, and **routine testing** like chest X-rays or viral studies is generally **not recommended** for uncomplicated cases as it rarely changes management unless there are atypical features or concerns for other diagnoses.
*Chest radiograph*
- A chest X-ray is generally **not indicated** for typical bronchiolitis presentations. It may show hyperinflation or peribronchial thickening but these findings often do not alter management.
- It should only be considered if there are atypical signs, such as a localized finding on exam or concern for **pneumonia** or **atelectasis**, which are not strongly suggested here.
*Sputum culture*
- **Infants** typically **do not produce sputum** for culture.
- Bronchiolitis is primarily a **viral infection**, making bacterial sputum cultures **irrelevant** for initial diagnosis and management unless secondary bacterial infection is strongly suspected, for which there is no evidence here.
*Viral culture*
- While bronchiolitis is caused by viruses, typically **RSV**, **routine viral culture** or rapid antigen testing for RSV is usually **not necessary** for diagnosis in typical cases.
- Identification of the specific virus does not change the clinical management, which is primarily **supportive care**.
*Polymerase chain reaction*
- **PCR testing** can identify viral pathogens but is generally **not recommended** for uncomplicated bronchiolitis cases as it does not change the management plan, which focuses on supportive care.
- It might be considered in severe cases, for **infection control** purposes in a hospital setting, or if there is a specific need for **epidemiological surveillance**, none of which are described as immediate priorities for this patient.
Ventilator-associated pneumonia US Medical PG Question 4: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Ventilator-associated pneumonia Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Ventilator-associated pneumonia US Medical PG Question 5: A 67-year-old man is brought to the emergency department because of severe dyspnea and orthopnea for 6 hours. He has a history of congestive heart disease and an ejection fraction of 40%. The medical history is otherwise unremarkable. He appears confused. At the hospital, his blood pressure is 165/110 mm Hg, the pulse is 135/min, the respirations are 48/min, and the temperature is 36.2°C (97.2°F). Crackles are heard at both lung bases. There is pitting edema from the midtibia to the ankle bilaterally. The patient is intubated and admitted to the critical care unit for mechanical ventilation and treatment. Intravenous morphine, diuretics, and nitroglycerine are initiated. Which of the following is the most effective method to prevent nosocomial infection in this patient?
- A. Nasogastric tube insertion
- B. Suprapubic catheter insertion
- C. Daily oropharynx decontamination with antiseptic agent (Correct Answer)
- D. Daily urinary catheter irrigation with antimicrobial agent
- E. Condom catheter placement
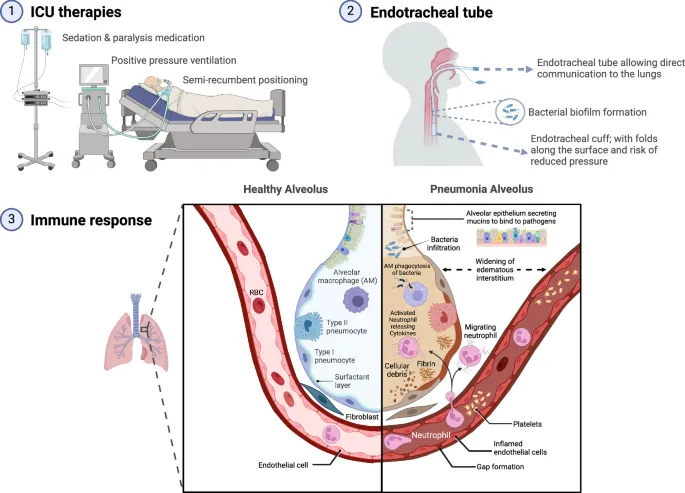
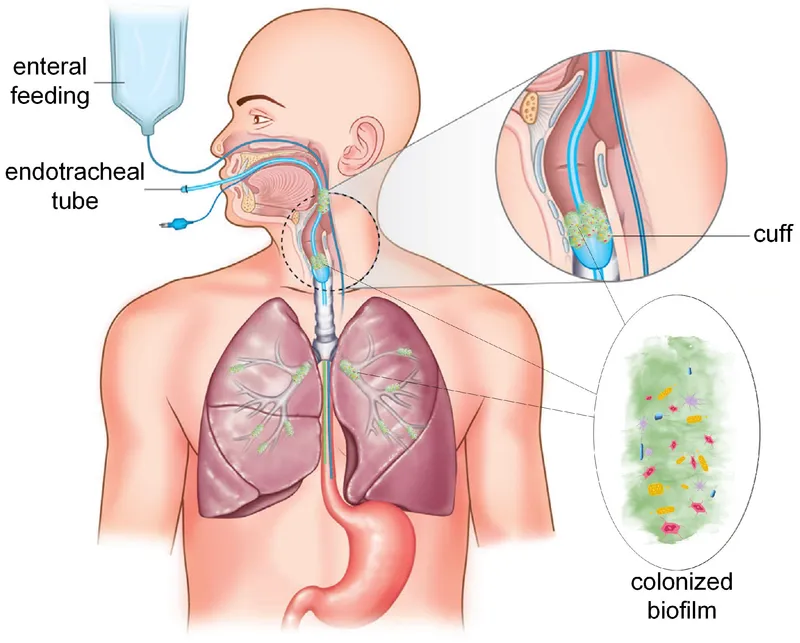
Ventilator-associated pneumonia Explanation: ***Daily oropharynx decontamination with antiseptic agent***
- **Oropharyngeal decontamination** helps reduce the bacterial load in the oral cavity, which is crucial for preventing **ventilator-associated pneumonia (VAP)** in intubated patients.
- Regular cleaning with an antiseptic agent disrupts the formation of **biofilms** and the aspiration of pathogenic bacteria into the lower respiratory tract.
*Nasogastric tube insertion*
- While a nasogastric tube can be important for nutrition and medication delivery, it does not directly prevent **nosocomial infections** and can even be a source of infection if not properly managed.
- It does not address the primary risk of pneumonia or other infections related to intubation and critical illness.
*Suprapubic catheter insertion*
- A suprapubic catheter is used for drainage of the bladder, but it is an invasive procedure with its own risks of **urinary tract infections (UTIs)** and is not indicated for preventing nosocomial infections in this patient's primary presentation.
- It is not a standard method to prevent the most common nosocomial infections in an intubated patient in the ICU.
*Daily urinary catheter irrigation with antimicrobial agent*
- Irrigating a urinary catheter daily with an antimicrobial agent is **not recommended** as a routine practice to prevent **catheter-associated urinary tract infections (CAUTIs)**.
- Such irrigation can disrupt the natural flora and potentially lead to **antimicrobial resistance** or further infection by promoting the growth of resistant organisms.
*Condom catheter placement*
- A condom catheter is a non-invasive external device used for urinary incontinence in males, but it's generally **less effective** than indwelling catheters for critical care patients requiring precise fluid output monitoring.
- It does not address the risk of **VAP**, which is a major concern for intubated patients, and may not be feasible or adequate for all bedridden patients in the ICU.
Ventilator-associated pneumonia US Medical PG Question 6: Patient of pneumonia on ventilator with wt. 50 kg. RR 14/min, bicarbonate - 18, pH 7.3, pCO2 48 mmHg, pO2 110 mmHg, PEEP 12 cm H2O, tidal volume 420 mL, SpO2 - 100% with FiO2 90%. What is next step in management?
- A. Increase PEEP
- B. Increase tidal volume
- C. Decrease fio2 (Correct Answer)
- D. Decrease RR
Ventilator-associated pneumonia Explanation: **Decrease FiO2**
- The patient has an **SpO2 of 100% with a FiO2 of 90%**, indicating **hyperoxia** induced by excessive oxygen delivery.
- Decreasing FiO2 is the appropriate next step to prevent **oxygen toxicity** (e.g., absorption atelectasis, free radical damage) while maintaining adequate oxygenation.
*Increase PEEP*
- The patient's **PaO2 of 110 mmHg** is already well within the normal to high range, suggesting that oxygenation is adequate.
- Increasing PEEP would be considered if the patient had **refractory hypoxemia**, not hyperoxia.
*Increase tidal volume*
- The current tidal volume of **420 mL for a 50 kg patient (8.4 mL/kg)** is already at the higher end of lung-protective ventilation (typically 6-8 mL/kg).
- Increasing tidal volume further could lead to **ventilator-induced lung injury** (VILI) due to volutrauma, especially in a patient with pneumonia.
*Decrease RR*
- The patient has a **pCO2 of 48 mmHg** and a **pH of 7.3**, indicating **respiratory acidosis** (hypoventilation).
- Decreasing the respiratory rate would further exacerbate the acidosis by reducing minute ventilation and increasing pCO2, which is inappropriate.
Ventilator-associated pneumonia US Medical PG Question 7: A previously healthy 35-year-old woman is brought into the emergency department after being found unresponsive by her husband. Her husband finds an empty bottle of diazepam tablets in her pocket. She is stuporous. At the hospital, her blood pressure is 90/40 mm Hg, the pulse is 58/min, and the respirations are 6/min. The examination of the pupils shows normal size and reactivity to light. Deep tendon reflexes are 1+ bilaterally. Babinski sign is absent. All 4 extremities are hypotonic. The patient is intubated and taken to the critical care unit for mechanical ventilation and treatment. Regarding the prevention of pneumonia in this patient, which of the following strategies is most likely to achieve this goal?
- A. Nasogastric tube insertion
- B. Daily evaluation for ventilator weaning
- C. Subglottic drainage of secretions (Correct Answer)
- D. Oropharynx and gut antibacterial decontamination
- E. Prone positioning during mechanical ventilation
Ventilator-associated pneumonia Explanation: ***Subglottic drainage of secretions***
- This is a highly effective strategy to prevent **ventilator-associated pneumonia (VAP)** by continuously removing secretions that pool above the endotracheal tube cuff before they can be aspirated.
- Endotracheal tubes with a **subglottic secretion drainage port** reduce VAP incidence by preventing microaspiration of contaminated oropharyngeal secretions into the lower respiratory tract.
- This is a **specific mechanical intervention** that directly addresses one of the key pathogenic mechanisms of VAP.
*Nasogastric tube insertion*
- While an NG tube may be needed for feeding or gastric decompression, it does not directly prevent VAP and may **increase aspiration risk** by compromising the lower esophageal sphincter.
- NG tubes can promote gastroesophageal reflux and provide a conduit for bacterial migration.
*Daily evaluation for ventilator weaning*
- This is also a **critical component of VAP prevention** as part of the ventilator bundle, since reducing duration of mechanical ventilation is the most effective overall strategy to prevent VAP.
- However, in this question asking for a strategy to prevent pneumonia in an intubated patient, subglottic drainage is the more specific technical intervention, whereas daily weaning assessment is a broader protocol that reduces exposure time.
- Both strategies are important; subglottic drainage addresses the "how" of prevention during intubation, while weaning protocols address the "duration" of risk exposure.
*Oropharynx and gut antibacterial decontamination*
- Selective digestive decontamination (SDD) aims to reduce bacterial colonization, but evidence for routine use is mixed and raises concerns about **antimicrobial resistance**.
- Not universally recommended as a primary VAP prevention strategy in most guidelines.
*Prone positioning during mechanical ventilation*
- **Prone positioning** is primarily indicated for improving oxygenation in **Acute Respiratory Distress Syndrome (ARDS)**, not for VAP prevention.
- While it may improve secretion drainage, it is not a standard VAP prevention measure and carries its own risks and logistical challenges.
Ventilator-associated pneumonia US Medical PG Question 8: A 45-year-old male presents to his primary care physician complaining of drainage from his left great toe. He has had an ulcer on his left great toe for over eight months. He noticed increasing drainage from the ulcer over the past week. His past medical history is notable for diabetes mellitus on insulin complicated by peripheral neuropathy and retinopathy. His most recent hemoglobin A1c was 9.4%. He has a 25 pack-year smoking history. He has multiple sexual partners and does not use condoms. His temperature is 100.8°F (38.2°C), blood pressure is 150/70 mmHg, pulse is 100/min, and respirations are 18/min. Physical examination reveals a 1 cm ulcer on the plantar aspect of the left great toe surrounded by an edematous and erythematous ring. Exposed bone can be palpated with a probe. There are multiple small cuts and bruises on both feet. A bone biopsy reveals abundant gram-negative rods that do not ferment lactose. The pathogen most likely responsible for this patient’s current condition is also strongly associated with which of the following conditions?
- A. Otitis externa (Correct Answer)
- B. Waterhouse-Friedrichsen syndrome
- C. Gastroenteritis
- D. Toxic shock syndrome
- E. Rheumatic fever
Ventilator-associated pneumonia Explanation: ***Otitis externa***
- The patient's presentation with a chronic **diabetic foot ulcer** with exposed bone and **gram-negative, non-lactose fermenting rods** on bone biopsy indicates **osteomyelitis** caused by ***Pseudomonas aeruginosa***.
- ***Pseudomonas aeruginosa*** is strongly associated with **otitis externa** (swimmer's ear), particularly **malignant otitis externa** in diabetic and immunocompromised patients.
- This is a classic association tested on USMLE: *Pseudomonas* causes both diabetic foot osteomyelitis and otitis externa.
*Waterhouse-Friedrichsen syndrome*
- This syndrome involves adrenal hemorrhage and fulminant sepsis, classically caused by ***Neisseria meningitidis***.
- Not associated with *Pseudomonas aeruginosa*.
*Gastroenteritis*
- Primarily caused by enteric pathogens such as *Salmonella*, *Shigella*, *Campylobacter*, *E. coli*, or viral agents.
- *Pseudomonas aeruginosa* is not a typical cause of gastroenteritis.
*Toxic shock syndrome*
- Caused by exotoxins from ***Staphylococcus aureus*** (TSST-1) or **Group A Streptococcus** (pyrogenic exotoxins).
- Not associated with *Pseudomonas aeruginosa*.
*Rheumatic fever*
- A delayed autoimmune complication of **Group A Streptococcal pharyngitis**.
- Not related to *Pseudomonas* infections or diabetic foot ulcers.
Ventilator-associated pneumonia US Medical PG Question 9: A 20-year-old woman presents for a follow-up visit with her physician. She has a history of cystic fibrosis and is currently under treatment. She has recently been struggling with recurrent bouts of cough and foul-smelling, mucopurulent sputum over the past year. Each episode lasts for about a week or so and then subsides. She does not have a fever or chills during these episodes. She has been hospitalized several times for pneumonia as a child and continues to struggle with diarrhea. Physically she appears to be underweight and in distress. Auscultation reveals reduced breath sounds on the lower lung fields with prominent rhonchi. Which of the following infectious agents is most likely associated with the recurrent symptoms this patient is experiencing?
- A. Mycobacterium avium
- B. Pseudomonas (Correct Answer)
- C. Histoplasma
- D. Pneumococcus
- E. Listeria
Ventilator-associated pneumonia Explanation: ***Pseudomonas***
- **Pseudomonas aeruginosa** is a common and opportunistic pathogen in patients with **cystic fibrosis** due to altered mucus secretion and impaired mucociliary clearance.
- Recurrent cough, foul-smelling, and **mucopurulent sputum** are classic symptoms of **Pseudomonas** lung infections in CF patients, often leading to chronic colonization and bronchiectasis.
*Mycobacterium avium*
- While *Mycobacterium avium complex* (MAC) can infect patients with cystic fibrosis, it typically causes a **more indolent and chronic lung disease** rather than recurrent, self-limiting bouts of cough and sputum.
- MAC infections are often associated with **nodular or cavitary lesions** on imaging and may require prolonged multidrug therapy.
*Histoplasmosis*
- **Histoplasmosis** is a fungal infection endemic to certain geographic regions (e.g., Ohio and Mississippi River valleys) and is acquired by inhaling spores.
- It's **not a typical or recurrent pathogen** in cystic fibrosis patients in the way bacterial infections are, and its presentation often includes fever, chills, and disseminated disease in immunocompromised individuals.
*Pneumococcus*
- *Streptococcus pneumoniae* (**Pneumococcus**) is a common cause of **acute bacterial pneumonia** in the general population, including young children.
- While CF patients can get pneumococcal infections, the pattern of **recurrent bouts of foul-smelling mucopurulent sputum** without fever and the chronic nature of the lung disease point away from typical acute pneumococcal infection and more towards a chronic colonizer like *Pseudomonas*.
*Listeria*
- *Listeria monocytogenes* is primarily a cause of **foodborne illness**, leading to gastroenteritis, meningitis, or sepsis, particularly in immunocompromised individuals, pregnant women, and neonates.
- It is **not a common respiratory pathogen**, and its presentation does not align with the described recurrent pulmonary symptoms in a cystic fibrosis patient.
Ventilator-associated pneumonia US Medical PG Question 10: While testing various strains of Streptococcus pneumoniae, a researcher discovers that a certain strain of this bacteria is unable to cause disease in mice when deposited in their lungs. What physiological test would most likely deviate from normal in this strain of bacteria as opposed to a typical strain?
- A. Quellung reaction (Correct Answer)
- B. Hemolytic reaction when grown on sheep blood agar
- C. Bile solubility
- D. Optochin sensitivity
- E. Motility
Ventilator-associated pneumonia Explanation: ***Quellung reaction***
- The **Quellung reaction** tests for the presence of the **polysaccharide capsule**, which is the primary virulence factor of *S. pneumoniae*.
- An **avirulent strain** that cannot cause disease would most likely lack the capsule and show a **negative Quellung reaction** (no capsular swelling), deviating from the **positive reaction** seen in typical encapsulated pathogenic strains.
- The capsule enables *S. pneumoniae* to evade phagocytosis and complement-mediated killing, which is essential for establishing infection in the lungs.
*Hemolytic reaction when grown on sheep blood agar*
- Both virulent and avirulent strains of *S. pneumoniae* typically exhibit **alpha-hemolysis** (partial hemolysis, producing a greenish discoloration) on sheep blood agar due to the production of pneumolysin.
- This characteristic does not differentiate between pathogenic and non-pathogenic strains in terms of disease-causing ability.
*Bile solubility*
- *S. pneumoniae* is characteristically **bile-soluble** due to the presence of autolysin enzymes that are activated by bile salts, leading to cellular lysis.
- This property is a **species characteristic** present in both virulent and avirulent strains, thus it would not explain the inability to cause disease.
*Optochin sensitivity*
- *S. pneumoniae* is universally **sensitive to optochin**, a chemical agent that inhibits its growth and is used for laboratory identification.
- This characteristic is used for **species identification** but does not correlate with strain virulence or disease-causing ability.
*Motility*
- *Streptococcus pneumoniae* is a **non-motile** bacterium; it lacks flagella.
- This characteristic is consistent across all strains and is not a virulence factor for this species.
More Ventilator-associated pneumonia US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.