Prevention bundles and checklists US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Prevention bundles and checklists. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Prevention bundles and checklists US Medical PG Question 1: The surgical equipment used during a craniectomy is sterilized using pressurized steam at 121°C for 15 minutes. Reuse of these instruments can cause transmission of which of the following pathogens?
- A. Non-enveloped viruses
- B. Sporulating bacteria
- C. Prions (Correct Answer)
- D. Enveloped viruses
- E. Yeasts
Prevention bundles and checklists Explanation: ***Prions***
- Prions are **abnormally folded proteins** that are highly resistant to standard sterilization methods like steam autoclaving at 121°C, making them a risk for transmission through reused surgical instruments.
- They cause transmissible spongiform encephalopathies (TSEs) like **Creutzfeldt-Jakob disease**, where even trace amounts can be highly infectious.
*Non-enveloped viruses*
- Non-enveloped viruses are generally **more resistant to heat and disinfectants** than enveloped viruses but are typically inactivated by recommended steam sterilization protocols.
- Standard autoclaving conditions are effective in destroying most non-enveloped viruses.
*Sporulating bacteria*
- **Bacterial spores**, such as those from *Clostridium* or *Bacillus*, are known for their high resistance to heat and chemicals, but are usually **inactivated by steam sterilization at 121°C** for 15 minutes.
- This method is specifically designed to kill bacterial spores effectively.
*Enveloped viruses*
- Enveloped viruses are the **least resistant to heat and chemical disinfectants** due to their lipid envelope.
- They are readily **inactivated by standard steam sterilization** at 121°C.
*Yeasts*
- **Yeasts** are eukaryotic microorganisms that are typically **susceptible to heat sterilization**.
- They are effectively killed by typical steam autoclaving conditions used for surgical instruments.
Prevention bundles and checklists US Medical PG Question 2: A previously healthy 35-year-old woman is brought into the emergency department after being found unresponsive by her husband. Her husband finds an empty bottle of diazepam tablets in her pocket. She is stuporous. At the hospital, her blood pressure is 90/40 mm Hg, the pulse is 58/min, and the respirations are 6/min. The examination of the pupils shows normal size and reactivity to light. Deep tendon reflexes are 1+ bilaterally. Babinski sign is absent. All 4 extremities are hypotonic. The patient is intubated and taken to the critical care unit for mechanical ventilation and treatment. Regarding the prevention of pneumonia in this patient, which of the following strategies is most likely to achieve this goal?
- A. Nasogastric tube insertion
- B. Daily evaluation for ventilator weaning
- C. Subglottic drainage of secretions (Correct Answer)
- D. Oropharynx and gut antibacterial decontamination
- E. Prone positioning during mechanical ventilation
Prevention bundles and checklists Explanation: ***Subglottic drainage of secretions***
- This is a highly effective strategy to prevent **ventilator-associated pneumonia (VAP)** by continuously removing secretions that pool above the endotracheal tube cuff before they can be aspirated.
- Endotracheal tubes with a **subglottic secretion drainage port** reduce VAP incidence by preventing microaspiration of contaminated oropharyngeal secretions into the lower respiratory tract.
- This is a **specific mechanical intervention** that directly addresses one of the key pathogenic mechanisms of VAP.
*Nasogastric tube insertion*
- While an NG tube may be needed for feeding or gastric decompression, it does not directly prevent VAP and may **increase aspiration risk** by compromising the lower esophageal sphincter.
- NG tubes can promote gastroesophageal reflux and provide a conduit for bacterial migration.
*Daily evaluation for ventilator weaning*
- This is also a **critical component of VAP prevention** as part of the ventilator bundle, since reducing duration of mechanical ventilation is the most effective overall strategy to prevent VAP.
- However, in this question asking for a strategy to prevent pneumonia in an intubated patient, subglottic drainage is the more specific technical intervention, whereas daily weaning assessment is a broader protocol that reduces exposure time.
- Both strategies are important; subglottic drainage addresses the "how" of prevention during intubation, while weaning protocols address the "duration" of risk exposure.
*Oropharynx and gut antibacterial decontamination*
- Selective digestive decontamination (SDD) aims to reduce bacterial colonization, but evidence for routine use is mixed and raises concerns about **antimicrobial resistance**.
- Not universally recommended as a primary VAP prevention strategy in most guidelines.
*Prone positioning during mechanical ventilation*
- **Prone positioning** is primarily indicated for improving oxygenation in **Acute Respiratory Distress Syndrome (ARDS)**, not for VAP prevention.
- While it may improve secretion drainage, it is not a standard VAP prevention measure and carries its own risks and logistical challenges.
Prevention bundles and checklists US Medical PG Question 3: A researcher is trying to determine whether a newly discovered substance X can be useful in promoting wound healing after surgery. She conducts this study by enrolling the next 100 patients that will be undergoing this surgery and separating them into 2 groups. She decides which patient will be in which group by using a random number generator. Subsequently, she prepares 1 set of syringes with the novel substance X and 1 set of syringes with a saline control. Both of these sets of syringes are unlabeled and the substances inside cannot be distinguished. She gives the surgeon performing the surgery 1 of the syringes and does not inform him nor the patient which syringe was used. After the study is complete, she analyzes all the data that was collected and performs statistical analysis. This study most likely provides which level of evidence for use of substance X?
- A. Level 3
- B. Level 1 (Correct Answer)
- C. Level 4
- D. Level 5
- E. Level 2
Prevention bundles and checklists Explanation: ***Level 1***
- The study design described is a **randomized controlled trial (RCT)**, which is considered the **highest level of evidence (Level 1)** in the hierarchy of medical evidence.
- Key features like **randomization**, **control group**, and **blinding (double-blind)** help minimize bias and strengthen the validity of the findings.
*Level 2*
- Level 2 evidence typically comprises **well-designed controlled trials without randomization** (non-randomized controlled trials) or **high-quality cohort studies**.
- While strong, they do not possess the same level of internal validity as randomized controlled trials.
*Level 3*
- Level 3 evidence typically includes **case-control studies** or **cohort studies**, which are observational designs and carry a higher risk of bias compared to RCTs.
- These studies generally do not involve randomization or intervention assignment by the researchers.
*Level 4*
- Level 4 evidence is usually derived from **case series** or **poor quality cohort and case-control studies**.
- These studies provide descriptive information or investigate associations without strong control for confounding factors.
*Level 5*
- Level 5 evidence is the **lowest level of evidence**, consisting of **expert opinion** or **animal research/bench research**.
- This level lacks human clinical data or systematic investigative rigor needed for higher evidence levels.
Prevention bundles and checklists US Medical PG Question 4: A 27-year-old man presents to the emergency department for altered mental status. The patient was found napping in a local market and brought to the hospital. The patient has a past medical history of polysubstance abuse and is homeless. His temperature is 104°F (40.0°C), blood pressure is 100/52 mmHg, pulse is 133/min, respirations are 25/min, and oxygen saturation is 99% on room air. Physical exam is notable for an altered man. Cardiopulmonary exam reveals a murmur over the left lower sternal border. A bedside ultrasound reveals a vegetation on the tricuspid valve. The patient is ultimately started on IV fluids, norepinephrine, vasopressin, vancomycin, and piperacillin-tazobactam. A central line is immediately placed in the internal jugular vein and the femoral vein secondary to poor IV access. Cardiothoracic surgery subsequently intervenes to remove the vegetation. While recovering in the ICU, days 3-5 are notable for an improvement in the patient’s symptoms. Two additional peripheral IVs are placed while in the ICU on day 5, and the femoral line is removed. On day 6, the patient's fever and hemodynamic status worsen. Though he is currently responding and not complaining of any symptoms including headache, photophobia, neck stiffness, or pain, he states he is feeling weak. Jolt accentuation of headache is negative and his abdominal exam is benign. A chest radiograph, urinalysis, and echocardiogram are unremarkable though the patient’s blood cultures are positive when drawn. Which of the following is the best next step in management?
- A. Add micafungin to the patient’s antibiotics
- B. Perform a lumbar puncture
- C. Remove all peripheral IV’s and send for cultures
- D. Add cefepime to the patient’s antibiotics
- E. Remove the central line and send for cultures (Correct Answer)
Prevention bundles and checklists Explanation: **Correct: Remove the central line and send for cultures**
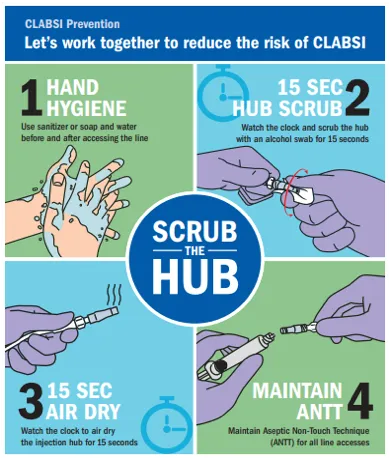
- The patient's worsening fever and hemodynamic instability on day 6, despite initial improvement, raise suspicion for a **catheter-related bloodstream infection (CRBSI)**, especially given the history of central line placement.
- **Prompt removal of the catheter** and sending the tip for culture is crucial for diagnosis and treatment of potential CRBSI, as the source of infection often resides within the biofilm on the catheter.
*Incorrect: Remove all peripheral IV's and send for cultures*
- While **peripheral IVs** can be a source of infection, the central line was placed earlier and is associated with a much higher risk of serious infection, especially in a critically ill patient.
- The patient's initial improvement followed by deterioration points more towards a **central line-associated infection** rather than new peripheral IVs placed only on day 5.
*Incorrect: Perform a lumbar puncture*
- Although the patient has altered mental status, the absence of focal neurological deficits, headache, photophobia, and neck stiffness, along with a negative **Jolt accentuation of headache**, makes **meningitis** less likely as the primary cause of deterioration.
- The more immediate and likely cause of worsening sepsis in this context is a **catheter-related infection**.
*Incorrect: Add micafungin to the patient's antibiotics*
- Adding an antifungal agent such as **micafungin** would be considered if there was a strong suspicion of a fungal infection, which is not indicated by the current blood cultures or clinical picture.
- Empiric antifungal therapy is typically reserved for patients with persistent fever refractory to broad-spectrum antibiotics, known fungal exposure, or specific risk factors.
*Incorrect: Add cefepime to the patient's antibiotics*
- The patient is already on **vancomycin and piperacillin-tazobactam**, which provides broad-spectrum coverage for both gram-positive and gram-negative bacteria, including *Pseudomonas aeruginosa*.
- Adding **cefepime** would broaden gram-negative coverage further but is usually unnecessary unless the current regimen is failing due to specific resistant organisms, and the more likely source of infection should be addressed first.
Prevention bundles and checklists US Medical PG Question 5: A 79-year-old man with a history of prostate cancer is brought to the emergency department because of lower abdominal pain for 1 hour. He has not urinated for 24 hours. Abdominal examination shows a palpable bladder that is tender to palpation. A pelvic ultrasound performed by the emergency department resident confirms the diagnosis of acute urinary retention. An attempt to perform transurethral catheterization is unsuccessful. A urology consultation is ordered and the urologist plans to attempt suprapubic catheterization. As the urologist is called to see a different emergency patient, she asks the emergency department resident to obtain informed consent for the procedure. The resident recalls a lecture about the different modes of catheterization, but he has never seen or performed a suprapubic catheterization himself. Which of the following statements by the emergency department resident is the most appropriate?
- A. “I would prefer that you obtain informed consent when you become available again.” (Correct Answer)
- B. “Suprapubic catheterization is not the treatment of choice for this patient.”
- C. “I would be happy to obtain informed consent on your behalf, but I'm not legally allowed to do so during my residency.”
- D. “I will make sure the patient reads and signs the informed consent form.”
- E. “I will ask the patient to waive informed consent because this is an urgent procedure.”
Prevention bundles and checklists Explanation: ***"I would prefer that you obtain informed consent when you become available again."***
- Informed consent requires that the person obtaining consent be **knowledgeable about the procedure**, its risks, benefits, and alternatives, and be able to answer the patient's questions thoroughly. The resident, having never performed or seen the procedure, cannot fulfill this requirement.
- The urologist, as the attending physician performing the procedure and the expert in suprapubic catheterization, is the most appropriate person to **educate the patient and obtain consent**.
*"Suprapubic catheterization is not the treatment of choice for this patient."*
- **Urethral catheterization is the first-line treatment for acute urinary retention**; however, it was unsuccessful.
- **Suprapubic catheterization is the appropriate next step** when transurethral catheterization fails or is contraindicated.
*"I would be happy to obtain informed consent on your behalf, but I'm not legally allowed to do so during my residency."*
- There is **no legal prohibition** for a resident to obtain informed consent, provided they are competent to do so and have adequate knowledge of the procedure.
- The issue here is the resident's **lack of knowledge and experience** with the particular procedure, not their legal status as a resident.
*"I will make sure the patient reads and signs the informed consent form."*
- Simply having the patient read and sign a form is **insufficient for valid informed consent**.
- Informed consent is a **process of communication** that ensures the patient understands the procedure, not just a signature on a document.
*"I will ask the patient to waive informed consent because this is an urgent procedure."*
- While this is an urgent situation, it is **not an emergency that precludes obtaining informed consent**.
- **Waiving informed consent** is generally reserved for life-threatening emergencies where immediate intervention is required to save a patient's life and there is no time to obtain consent, which is not the case here.
Prevention bundles and checklists US Medical PG Question 6: Three days after undergoing coronary bypass surgery, a 67-year-old man becomes unresponsive and hypotensive. He is intubated, mechanically ventilated, and a central line is inserted. Vasopressin and noradrenaline infusions are begun. A Foley catheter is placed. Six days later, he has high unrelenting fevers. He is currently receiving noradrenaline via an infusion pump. His temperature is 39.6°C (102.3°F), pulse is 113/min, and blood pressure is 90/50 mm Hg. Examination shows a sternal wound with surrounding erythema; there is no discharge from the wound. Crackles are heard at both lung bases. Cardiac examination shows an S3 gallop. Abdominal examination shows no abnormalities. A Foley catheter is present. His hemoglobin concentration is 10.8 g/dL, leukocyte count is 21,700/mm3, and platelet count is 165,000/mm3. Samples for blood culture are drawn simultaneously from the central line and peripheral IV line. Blood cultures from the central line show coagulase-negative cocci in clusters on the 8th postoperative day, and those from the peripheral venous line show coagulase-negative cocci in clusters on the 10th postoperative day. Which of the following is the most likely diagnosis in this patient?
- A. Central line-associated blood stream infection (Correct Answer)
- B. Catheter-associated urinary tract infection
- C. Surgical site infection
- D. Bowel ischemia
- E. Ventilator-associated pneumonia
Prevention bundles and checklists Explanation: ***Central line-associated blood stream infection***
- The patient exhibits signs of **sepsis** (fever, hypotension, tachycardia) following central line insertion, and **coagulase-negative cocci** (e.g., *Staphylococcus epidermidis*) were isolated from both central and peripheral blood cultures with differential times to positivity, indicating a central line origin.
- The organism isolated, **coagulase-negative cocci**, is a common cause of **central line-associated bloodstream infections** (CLABSI).
*Catheter-associated urinary tract infection*
- While a **Foley catheter** is present, there are no specific signs or symptoms of a **urinary tract infection**, such as dysuria, frequency, or hematuria.
- The microbiology results (coagulase-negative cocci in blood, not urine) do not support a urinary source for the infection.
*Surgical site infection*
- There is **erythema** around the sternal wound, suggesting a superficial infection, but no **discharge** or deepening wound involvement is noted.
- A surgical site infection would typically manifest with more prominent localized signs and would be less likely to cause a systemic bloodstream infection with coagulase-negative cocci detected *before* peripheral line cultures.
*Bowel ischemia*
- This condition is often associated with **abdominal pain**, distension, and signs of organ dysfunction.
- The abdominal examination is explicitly stated as normal, making bowel ischemia unlikely.
*Ventilator-associated pneumonia*
- The patient has crackles at lung bases and is mechanically ventilated, but there are no specific findings like new infiltrates on chest imaging or purulent sputum that would strongly indicate **pneumonia**.
- The isolated organism in the blood (coagulase-negative cocci) is not a typical pathogen for ventilator-associated pneumonia, which usually involves Gram-negative rods or *Staphylococcus aureus*.
Prevention bundles and checklists US Medical PG Question 7: A 67-year-old man is brought to the emergency department because of severe dyspnea and orthopnea for 6 hours. He has a history of congestive heart disease and an ejection fraction of 40%. The medical history is otherwise unremarkable. He appears confused. At the hospital, his blood pressure is 165/110 mm Hg, the pulse is 135/min, the respirations are 48/min, and the temperature is 36.2°C (97.2°F). Crackles are heard at both lung bases. There is pitting edema from the midtibia to the ankle bilaterally. The patient is intubated and admitted to the critical care unit for mechanical ventilation and treatment. Intravenous morphine, diuretics, and nitroglycerine are initiated. Which of the following is the most effective method to prevent nosocomial infection in this patient?
- A. Nasogastric tube insertion
- B. Suprapubic catheter insertion
- C. Daily oropharynx decontamination with antiseptic agent (Correct Answer)
- D. Daily urinary catheter irrigation with antimicrobial agent
- E. Condom catheter placement
Prevention bundles and checklists Explanation: ***Daily oropharynx decontamination with antiseptic agent***
- **Oropharyngeal decontamination** helps reduce the bacterial load in the oral cavity, which is crucial for preventing **ventilator-associated pneumonia (VAP)** in intubated patients.
- Regular cleaning with an antiseptic agent disrupts the formation of **biofilms** and the aspiration of pathogenic bacteria into the lower respiratory tract.
*Nasogastric tube insertion*
- While a nasogastric tube can be important for nutrition and medication delivery, it does not directly prevent **nosocomial infections** and can even be a source of infection if not properly managed.
- It does not address the primary risk of pneumonia or other infections related to intubation and critical illness.
*Suprapubic catheter insertion*
- A suprapubic catheter is used for drainage of the bladder, but it is an invasive procedure with its own risks of **urinary tract infections (UTIs)** and is not indicated for preventing nosocomial infections in this patient's primary presentation.
- It is not a standard method to prevent the most common nosocomial infections in an intubated patient in the ICU.
*Daily urinary catheter irrigation with antimicrobial agent*
- Irrigating a urinary catheter daily with an antimicrobial agent is **not recommended** as a routine practice to prevent **catheter-associated urinary tract infections (CAUTIs)**.
- Such irrigation can disrupt the natural flora and potentially lead to **antimicrobial resistance** or further infection by promoting the growth of resistant organisms.
*Condom catheter placement*
- A condom catheter is a non-invasive external device used for urinary incontinence in males, but it's generally **less effective** than indwelling catheters for critical care patients requiring precise fluid output monitoring.
- It does not address the risk of **VAP**, which is a major concern for intubated patients, and may not be feasible or adequate for all bedridden patients in the ICU.
Prevention bundles and checklists US Medical PG Question 8: A surgical ICU has implemented multiple interventions over 18 months: chlorhexidine bathing, antibiotic stewardship, contact precautions for MRSA, and environmental cleaning protocols. Despite these efforts, MRSA surgical site infection rates remain unchanged at 8 per 1000 surgical procedures. Universal MRSA screening shows 15% of admitted patients are colonized. Evaluate the most effective evidence-based strategy to reduce MRSA SSI rates further.
- A. Targeted decolonization only for MRSA-positive patients with mupirocin and chlorhexidine
- B. Isolation of all surgical patients in private rooms until discharge
- C. Routine screening and decolonization of all healthcare workers
- D. Extended vancomycin prophylaxis for all surgical patients for 48 hours postoperatively
- E. Universal MRSA decolonization for all surgical patients regardless of screening results (Correct Answer)
Prevention bundles and checklists Explanation: ***Universal MRSA decolonization for all surgical patients regardless of screening results***
- **Universal decolonization** has been proven more effective than screening-based strategies in high-risk settings like the ICU, significantly reducing **MRSA surgical site infections** and bloodstream infections.
- This approach is superior because it addresses **undetected carriers**, eliminates delays associated with waiting for lab cultures, and is often more **cost-effective** and easier to implement.
*Targeted decolonization only for MRSA-positive patients with mupirocin and chlorhexidine*
- While logical, **targeted decolonization** is less effective than the universal approach because it misses patients who may be **falsely negative** or colonized at levels below detection thresholds.
- Evidence from recent large-scale trials shows that **targeted strategies** do not reduce MRSA infection rates as drastically as treating the entire cohort at risk.
*Isolation of all surgical patients in private rooms until discharge*
- This strategy is **logistically impractical** and extremely expensive, focusing on **containment** rather than the active reduction of the patient's own bacterial load (colonization).
- Research indicates that **contact precautions** and isolation alone are less effective than decolonization protocols in preventing **autoinoculation** during surgery.
*Routine screening and decolonization of all healthcare workers*
- Screening of **healthcare workers (HCWs)** is not recommended as a routine practice; it is typically reserved for **outbreak investigations** where an epidemiological link is suspected.
- Constant recolonization from patients and the environment makes **HCW decolonization** an unsustainable and transient solution for reducing overall SSI rates.
*Extended vancomycin prophylaxis for all surgical patients for 48 hours postoperatively*
- **Extended antibiotic prophylaxis** beyond 24 hours provides no additional protection against SSIs and significantly increases the risk of **C. difficile** and antibiotic resistance.
- Proper surgical prophylaxis involves **timely administration** before the incision, not prolonged courses which violate **antibiotic stewardship** principles.
Prevention bundles and checklists US Medical PG Question 9: A 70-year-old man with prosthetic aortic valve develops fever and bacteremia 3 weeks after valve replacement. Blood cultures grow Enterococcus faecium resistant to ampicillin and vancomycin (VRE). Susceptibilities show sensitivity to linezolid and daptomycin. TEE shows a small vegetation on the prosthetic valve. Creatinine is 1.8 mg/dL (baseline 1.0). Evaluate the optimal treatment strategy considering the infection location and drug characteristics.
- A. Combination daptomycin and linezolid (Correct Answer)
- B. Linezolid plus gentamicin for synergy
- C. Daptomycin plus ampicillin despite resistance
- D. Daptomycin monotherapy with high dose (10-12 mg/kg)
- E. Linezolid monotherapy for 6 weeks
Prevention bundles and checklists Explanation: ***Combination daptomycin and linezolid***
- For **VRE prosthetic valve endocarditis (PVE)**, monotherapy often fails due to high bacterial inoculum and **biofilm formation**, necessitating synergistic combinations.
- **Daptomycin** provides bactericidal activity, while **linezolid** enhances biofilm penetration; this combination is a salvage strategy to prevent the emergence of **daptomycin resistance** during prolonged therapy.
*Linezolid plus gentamicin for synergy*
- **Gentamicin** synergy is typically reserved for **ampicillin-susceptible** enterococci and requires a cell-wall active agent to facilitate entry, which linezolid (protein synthesis inhibitor) does not provide.
- The patient has an elevated **creatinine (1.8 mg/dL)**, making the use of **nephrotoxic aminoglycosides** like gentamicin highly risky and suboptimal.
*Daptomycin plus ampicillin despite resistance*
- While **ampicillin** can sometimes enhance daptomycin binding by reducing the net negative surface charge of the bacteria, it is generally less effective when high-level **ampicillin resistance** is already confirmed in *E. faecium*.
- This strategy is typically considered when other secondary agents are unavailable or contraindicated, but it is not superior to linezolid-based combinations in VRE endocarditis.
*Daptomycin monotherapy with high dose (10-12 mg/kg)*
- High-dose **daptomycin (10-12 mg/kg)** is recommended for endocarditis, but monotherapy for **prosthetic valve** infections carries a high risk of treatment failure.
- *Enterococcus faecium* can rapidly develop **resistance** (via the LiaFSR system) during daptomycin monotherapy, making a second agent necessary for such a high-burden infection.
*Linezolid monotherapy for 6 weeks*
- **Linezolid** is primarily **bacteriostatic** against enterococci, which is generally insufficient for the definitive treatment of **infective endocarditis** where bactericidal activity is required.
- Long-term use (over 2 weeks) carries significant risks of **bone marrow suppression** (thrombocytopenia) and **mitochondrial toxicity**, making it unsafe as a sole agent for a 6-week course.
Prevention bundles and checklists US Medical PG Question 10: A hospital implements a bundle to reduce catheter-associated urinary tract infections (CAUTI): daily review of catheter necessity, aseptic insertion technique, and proper maintenance. After 6 months, CAUTI rates decrease by 40% but then plateau. Compliance audits show 95% adherence to the bundle. The infection control team must evaluate the next intervention to achieve further reduction.
- A. Focus on reducing overall catheter utilization and early removal (Correct Answer)
- B. Increase frequency of catheter changes to every 72 hours
- C. Switch to suprapubic catheters for long-term needs
- D. Add prophylactic antibiotics for catheterized patients
- E. Implement antimicrobial-coated catheters for all patients
Prevention bundles and checklists Explanation: ***Focus on reducing overall catheter utilization and early removal***
- Since **compliance** with the bundle is already high at **95%**, the most influential risk factor for infection remains the **duration of catheterization**.
- Implementing **nurse-driven protocols** for early removal and utilizing **bladder scanners** to avoid insertion are the most effective strategies to further reduce **CAUTI** rates.
*Increase frequency of catheter changes to every 72 hours*
- Routine **scheduled catheter changes** are not recommended as they increase the risk of introducing **uropathogens** into the bladder during the procedure.
- Catheters should only be changed if there is a clinical indication, such as **obstruction**, **leakage**, or established **infection**.
*Switch to suprapubic catheters for long-term needs*
- **Suprapubic catheters** are invasive surgical procedures that may carry risks of **bowel injury** and are not indicated for general hospital-wide infection reduction.
- While they may reduce some urethral complications, they do not fundamentally eliminate the risk of **biofilm formation** and subsequent bacteriuria.
*Add prophylactic antibiotics for catheterized patients*
- Routine use of **prophylactic antibiotics** is strongly discouraged because it fosters the development of **multi-drug resistant organisms (MDROs)**.
- Evidence shows it does not prevent long-term **CAUTI** and may lead to complications like **Clostridioides difficile** infection.
*Implement antimicrobial-coated catheters for all patients*
- There is **limited clinical evidence** that antimicrobial-coated catheters provide a significant, cost-effective reduction in **symptomatic CAUTIs** compared to standard catheters.
- These are generally reserved for high-risk patients or specific units where other **prevention bundles** have consistently failed, rather than universal implementation.
More Prevention bundles and checklists US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.