Environmental reservoirs in healthcare settings US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Environmental reservoirs in healthcare settings. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Environmental reservoirs in healthcare settings US Medical PG Question 1: The surgical equipment used during a craniectomy is sterilized using pressurized steam at 121°C for 15 minutes. Reuse of these instruments can cause transmission of which of the following pathogens?
- A. Non-enveloped viruses
- B. Sporulating bacteria
- C. Prions (Correct Answer)
- D. Enveloped viruses
- E. Yeasts
Environmental reservoirs in healthcare settings Explanation: ***Prions***
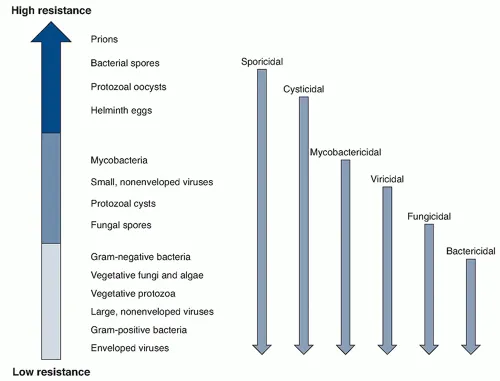
- Prions are **abnormally folded proteins** that are highly resistant to standard sterilization methods like steam autoclaving at 121°C, making them a risk for transmission through reused surgical instruments.
- They cause transmissible spongiform encephalopathies (TSEs) like **Creutzfeldt-Jakob disease**, where even trace amounts can be highly infectious.
*Non-enveloped viruses*
- Non-enveloped viruses are generally **more resistant to heat and disinfectants** than enveloped viruses but are typically inactivated by recommended steam sterilization protocols.
- Standard autoclaving conditions are effective in destroying most non-enveloped viruses.
*Sporulating bacteria*
- **Bacterial spores**, such as those from *Clostridium* or *Bacillus*, are known for their high resistance to heat and chemicals, but are usually **inactivated by steam sterilization at 121°C** for 15 minutes.
- This method is specifically designed to kill bacterial spores effectively.
*Enveloped viruses*
- Enveloped viruses are the **least resistant to heat and chemical disinfectants** due to their lipid envelope.
- They are readily **inactivated by standard steam sterilization** at 121°C.
*Yeasts*
- **Yeasts** are eukaryotic microorganisms that are typically **susceptible to heat sterilization**.
- They are effectively killed by typical steam autoclaving conditions used for surgical instruments.
Environmental reservoirs in healthcare settings US Medical PG Question 2: A 50-year-old male presents to the emergency room complaining of fever, shortness of breath, and diarrhea. He returned from a spa in the Rocky Mountains five days prior. He reports that over the past two days, he developed a fever, cough, dyspnea, and multiple watery stools. His past medical history is notable for major depressive disorder and peptic ulcer disease. He takes omeprazole and paroxetine. He does not smoke and drinks alcohol on social occasions. His temperature is 102.8°F (39.3°C), blood pressure is 120/70 mmHg, pulse is 65/min, and respirations are 20/min. Physical examination reveals dry mucus membranes, delayed capillary refill, and rales at the bilateral lung bases. A basic metabolic panel is shown below:
Serum:
Na+: 126 mEq/L
Cl-: 100 mEq/L
K+: 4.1 mEq/L
HCO3-: 23 mEq/L
Ca2+: 10.1 mg/dL
Mg2+: 2.0 mEq/L
Urea nitrogen: 14 mg/dL
Glucose: 90 mg/dL
Creatinine: 1.1 mg/dL
Which of the following is the most appropriate growth medium to culture the pathogen responsible for this patient’s condition?
- A. Eaton’s agar
- B. Bordet-Gengou agar
- C. Thayer-Martin agar
- D. Charcoal yeast agar with iron and cysteine (Correct Answer)
- E. Sorbitol-MacConkey agar
Environmental reservoirs in healthcare settings Explanation: ***Charcoal yeast agar with iron and cysteine***
- This patient's symptoms (fever, cough, dyspnea, diarrhea) after visiting a spa, combined with **hyponatremia** (Na+ 126 mEq/L), are highly characteristic of **Legionnaires' disease** caused by *Legionella pneumophila*.
- *Legionella* is a fastidious organism that requires specialized media for growth, specifically charcoal yeast extract (BCYE) agar supplemented with **L-cysteine** and **iron salts**.
*Eaton’s agar*
- Eaton's agar is a specialized medium used for the primary isolation of **Mycoplasma pneumoniae**.
- *Mycoplasma pneumoniae* typically causes **atypical pneumonia** but does not present with severe gastrointestinal symptoms or hyponatremia as seen in this patient.
*Bordet-Gengou agar*
- Bordet-Gengou agar, containing potato extract, glycerol, and blood, is the selective medium used for the isolation of **Bordetella pertussis**, the causative agent of whooping cough.
- The clinical presentation of **pertussis** involves paroxysmal coughing fits, often with a 'whoop,' and is distinct from the patient's symptoms.
*Thayer-Martin agar*
- Thayer-Martin agar is a selective medium primarily used for the isolation of **Neisseria gonorrhoeae** and *Neisseria meningitidis*.
- These bacteria cause gonorrhea and meningitis, respectively, and are not associated with the respiratory and gastrointestinal symptoms described.
*Sorbitol-MacConkey agar*
- Sorbitol-MacConkey agar is a differential and selective medium used to detect **enterohemorrhagic Escherichia coli O157:H7** in stool samples, which appears as colorless colonies because it cannot ferment sorbitol.
- While the patient has diarrhea, the predominant respiratory symptoms, hyponatremia, and exposure history point away from E. coli O157:H7 as the primary pathogen.
Environmental reservoirs in healthcare settings US Medical PG Question 3: A patient is hospitalized for pneumonia. Gram-positive cocci in clusters are seen on sputum gram stain. Which of the following clinical scenarios is most commonly associated with this form of pneumonia?
- A. Elderly patient who has trouble swallowing and poor dentition
- B. An alcoholic with evidence of empyema and "currant jelly sputum"
- C. An otherwise healthy young adult with a week of mild fatigue, chills, and cough
- D. Hospitalized adult with development of pneumonia symptoms 2 weeks following a viral illness (Correct Answer)
- E. HIV positive adult with a CD4 count less than 150 and an impaired diffusion capacity
Environmental reservoirs in healthcare settings Explanation: ***Hospitalized adult with development of pneumonia symptoms 2 weeks following a viral illness***
- Gram-positive cocci in clusters suggests **Staphylococcus aureus**, which is a common cause of secondary bacterial pneumonia, often following **viral illnesses** (e.g., influenza).
- This scenario represents a classic presentation of **secondary bacterial pneumonia**, where the initial viral infection compromises the respiratory defenses, allowing bacterial superinfection.
*Elderly patient who has trouble swallowing and poor dentition*
- This scenario points towards **aspiration pneumonia**, often caused by a **polymicrobial infection** that includes oral anaerobes, not typically dominated by Gram-positive cocci in clusters.
- While *S. aureus* can cause aspiration pneumonia, the primary concern in this context would be **anaerobic bacteria**, given the aspiration risk factors.
*An alcoholic with evidence of empyema and \"currant jelly sputum\"*
- This description is highly suggestive of **Klebsiella pneumoniae** infection, which typically presents with thick, gelatinous, and often **blood-tinged sputum**.
- **Klebsiella** is a Gram-negative rod, not Gram-positive cocci in clusters.
*An otherwise healthy young adult with a week of mild fatigue, chills, and cough*
- This presentation is more consistent with **atypical pneumonia** caused by organisms like **Mycoplasma pneumoniae** or **Chlamydophila pneumoniae**, which would not show Gram-positive cocci in clusters on sputum stain.
- **Streptococcus pneumoniae** (Gram-positive cocci in chains) can also cause community-acquired pneumonia in otherwise healthy individuals, but the "clusters" indicate **Staphylococcus aureus**.
*HIV positive adult with a CD4 count less than 150 and an impaired diffusion capacity*
- This clinical picture strongly suggests **Pneumocystis jirovecii pneumonia (PJP)**, which is common in severely immunocompromised HIV patients.
- *P. jirovecii* is a fungus and would not be seen as Gram-positive cocci in clusters on a routine Gram stain.
Environmental reservoirs in healthcare settings US Medical PG Question 4: A 57-year-old HIV-positive male with a history of intravenous drug abuse presents to the emergency room complaining of arm swelling. He reports that he developed progressively worsening swelling and tenderness over the right antecubital fossa three days prior. He recently returned from a trip to Nicaragua. His past medical history is notable for an anaphylactoid reaction to vancomycin. His temperature is 101.4°F (38.6°C), blood pressure is 140/70 mmHg, pulse is 110/min, and respirations are 20/min. Physical examination reveals an erythematous, fluctuant, and tender mass overlying the right antecubital fossa. Multiple injection marks are noted across both upper extremities. He undergoes incision and drainage and is started on an antibiotic that targets the 50S ribosome. He is discharged with plans to follow up in one week. However, five days later he presents to the same emergency room complaining of abdominal cramps and watery diarrhea. Which of the following classes of pathogens is most likely responsible for this patient’s current symptoms?
- A. Gram-negative curved bacillus
- B. Gram-negative bacillus
- C. Anaerobic flagellated protozoan
- D. Gram-positive bacillus (Correct Answer)
- E. Gram-positive coccus
Environmental reservoirs in healthcare settings Explanation: ***Gram-positive bacillus***
- The patient was administered an antibiotic targeting the **50S ribosomal subunit** following incision and drainage for a suspected skin infection (likely **MRSA** given IV drug abuse). This strongly suggests **clindamycin** was used.
- **Clindamycin** is a known risk factor for developing **Clostridioides (formerly Clostridium) difficile infection (CDI)**, which is caused by a **Gram-positive, spore-forming bacillus** and manifests with **abdominal cramps and watery diarrhea**.
*Gram-negative curved bacillus*
- This class of pathogens includes organisms like **Vibrio cholerae** or **Campylobacter jejuni**, which can cause diarrhea.
- However, the patient's presentation with **colitis** after antibiotic use is more consistent with **Clostridioides difficile**, not typically a curved Gram-negative bacillus.
*Gram-negative bacillus*
- While some Gram-negative bacilli (e.g., E. coli, Salmonella) can cause diarrhea, their association with **antibiotic-induced colitis** following treatment for a skin abscess is less direct than that of *Clostridioides difficile*.
- The initial skin infection in IV drug users is most commonly staphylococcal (Gram-positive coccus), for which a 50S targeting antibiotic would be prescribed.
*Anaerobic flagellated protozoan*
- This description often refers to pathogens like **Giardia lamblia** or **Trichomonas vaginalis**, which are not bacteria.
- While *Giardia* can cause diarrhea, it typically causes **malabsorption** and **greasy stools**, and wouldn't be triggered by recent antibiotic use for a skin infection.
*Gram-positive coccus*
- **Gram-positive cocci** (e.g., Staphylococcus aureus) are the likely cause of the initial skin infection/abscess.
- However, they do not typically cause **antibiotic-associated colitis** with watery diarrhea; rather, the *antibiotic treatment itself* for these organisms can predispose to *Clostridioides difficile*.
Environmental reservoirs in healthcare settings US Medical PG Question 5: A 67-year-old man is brought to the emergency department because of severe dyspnea and orthopnea for 6 hours. He has a history of congestive heart disease and an ejection fraction of 40%. The medical history is otherwise unremarkable. He appears confused. At the hospital, his blood pressure is 165/110 mm Hg, the pulse is 135/min, the respirations are 48/min, and the temperature is 36.2°C (97.2°F). Crackles are heard at both lung bases. There is pitting edema from the midtibia to the ankle bilaterally. The patient is intubated and admitted to the critical care unit for mechanical ventilation and treatment. Intravenous morphine, diuretics, and nitroglycerine are initiated. Which of the following is the most effective method to prevent nosocomial infection in this patient?
- A. Nasogastric tube insertion
- B. Suprapubic catheter insertion
- C. Daily oropharynx decontamination with antiseptic agent (Correct Answer)
- D. Daily urinary catheter irrigation with antimicrobial agent
- E. Condom catheter placement
Environmental reservoirs in healthcare settings Explanation: ***Daily oropharynx decontamination with antiseptic agent***
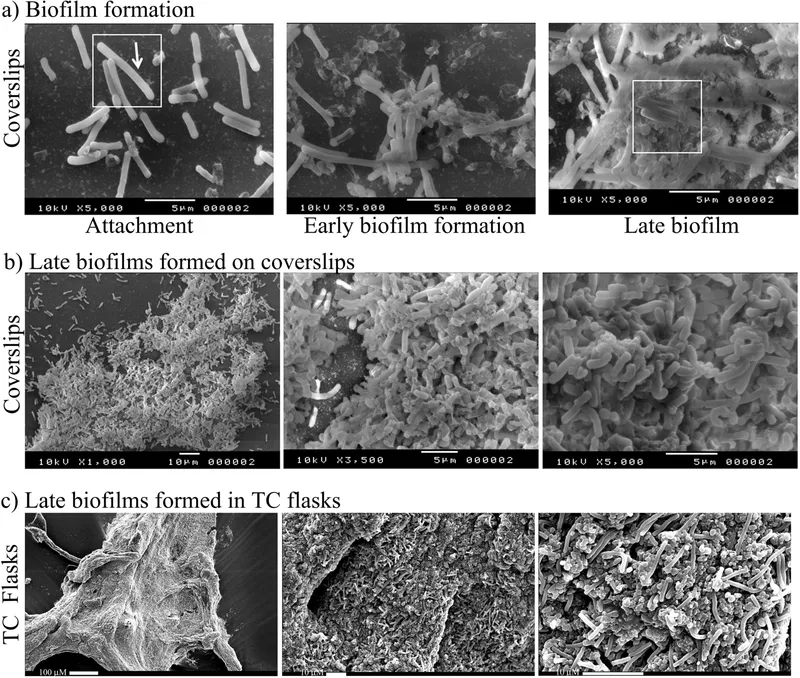
- **Oropharyngeal decontamination** helps reduce the bacterial load in the oral cavity, which is crucial for preventing **ventilator-associated pneumonia (VAP)** in intubated patients.
- Regular cleaning with an antiseptic agent disrupts the formation of **biofilms** and the aspiration of pathogenic bacteria into the lower respiratory tract.
*Nasogastric tube insertion*
- While a nasogastric tube can be important for nutrition and medication delivery, it does not directly prevent **nosocomial infections** and can even be a source of infection if not properly managed.
- It does not address the primary risk of pneumonia or other infections related to intubation and critical illness.
*Suprapubic catheter insertion*
- A suprapubic catheter is used for drainage of the bladder, but it is an invasive procedure with its own risks of **urinary tract infections (UTIs)** and is not indicated for preventing nosocomial infections in this patient's primary presentation.
- It is not a standard method to prevent the most common nosocomial infections in an intubated patient in the ICU.
*Daily urinary catheter irrigation with antimicrobial agent*
- Irrigating a urinary catheter daily with an antimicrobial agent is **not recommended** as a routine practice to prevent **catheter-associated urinary tract infections (CAUTIs)**.
- Such irrigation can disrupt the natural flora and potentially lead to **antimicrobial resistance** or further infection by promoting the growth of resistant organisms.
*Condom catheter placement*
- A condom catheter is a non-invasive external device used for urinary incontinence in males, but it's generally **less effective** than indwelling catheters for critical care patients requiring precise fluid output monitoring.
- It does not address the risk of **VAP**, which is a major concern for intubated patients, and may not be feasible or adequate for all bedridden patients in the ICU.
Environmental reservoirs in healthcare settings US Medical PG Question 6: A 69-year-old man is brought to the emergency department by his wife because of fever, cough, diarrhea, and confusion for 2 days. He recently returned from a cruise to the Caribbean. He has a history of chronic obstructive pulmonary disease. He has smoked one pack of cigarettes daily for 40 years. His temperature is 39.1°C (102.4°F), pulse is 83/min, and blood pressure is 111/65 mm Hg. He is confused and oriented only to person. Physical examination shows coarse crackles throughout both lung fields. His serum sodium concentration is 125 mEq/L. Culture of the most likely causal organism would require which of the following mediums?
- A. Charcoal yeast extract agar (Correct Answer)
- B. Eosin-methylene blue agar
- C. Mannitol salt agar
- D. Chocolate agar
- E. Eaton agar
Environmental reservoirs in healthcare settings Explanation: ***Charcoal yeast extract agar***
- The patient's symptoms (fever, cough, diarrhea, confusion, hyponatremia) and risk factors (COPD, smoking history, recent cruise travel) are highly suggestive of **Legionnaires' disease** caused by *Legionella pneumophila*.
- *Legionella* is a fastidious organism that requires **cysteine** and **iron salts** for growth, which are provided in **buffered charcoal yeast extract (BCYE) agar**.
*Eosin-methylene blue agar*
- This is a **selective and differential medium** used for the isolation and differentiation of **Gram-negative enteric bacteria**, particularly useful for identifying coliforms like *E. coli*.
- It contains dyes that inhibit Gram-positive bacteria and differentiate lactose fermenters, which is not relevant for *Legionella*.
*Mannitol salt agar*
- This is a **selective and differential medium** primarily used for the isolation and identification of **staphylococci**, especially *Staphylococcus aureus*.
- It contains a high salt concentration to inhibit most bacteria and mannitol to differentiate *S. aureus* (which ferments mannitol) from other staphylococci.
*Chocolate agar*
- This enriched medium is used for the isolation of fastidious bacteria such as **Haemophilus influenzae** and **Neisseria species**, which require factors like **hemin (X factor)** and **NAD (V factor)**.
- While it supports the growth of many pathogenic bacteria, it does not provide the specific growth requirements for *Legionella*.
*Eaton agar*
- This specialized medium is primarily used for the isolation and cultivation of **Mycoplasma pneumoniae**, a common cause of "walking pneumonia."
- *Mycoplasma pneumoniae* is a bacterium that lacks a cell wall and has unique growth requirements, distinct from *Legionella*.
Environmental reservoirs in healthcare settings US Medical PG Question 7: A 32-year-old woman presents to your office with abdominal pain and bloating over the last month. She also complains of intermittent, copious, non-bloody diarrhea over the same time. Last month, she had a cough that has since improved but has not completely resolved. She has no sick contacts and has not left the country recently. She denies any myalgias, itching, or rashes. Physical and laboratory evaluations are unremarkable. Examination of her stool reveals the causative organism. This organism is most likely transmitted to the human host through which of the following routes?
- A. Insect bite
- B. Penetration of skin (Correct Answer)
- C. Sexual contact
- D. Inhalation
- E. Animal bite
Environmental reservoirs in healthcare settings Explanation: ***Penetration of skin***
- The symptoms of **abdominal pain**, **bloating**, **intermittent copious non-bloody diarrhea**, and a recent **cough** are highly suggestive of a **hookworm infection**.
- Hookworm larvae (filariform larvae) primarily penetrate the skin, usually through bare feet, as their mode of entry into the human host.
*Insect bite*
- Although some parasitic infections are transmitted by insect bites (e.g., malaria, Chagas disease), hookworms are not transmitted this way.
- **Insect-borne diseases** typically present with different clinical manifestations or geographical associations.
*Sexual contact*
- **Sexually transmitted infections** involve direct contact of mucous membranes or body fluids during sexual activity.
- Hookworm infection transmission through sexual contact is not a recognized route.
*Inhalation*
- **Inhalation** is a route of transmission for respiratory pathogens (e.g., influenza, tuberculosis) or certain fungal infections, but not for hookworms.
- While hookworm larvae migrate through the lungs, the initial infection pathway is not via inhalation.
*Animal bite*
- **Animal bites** transmit diseases like rabies or certain bacterial infections, but not parasitic hookworms.
- Hookworm infection does not result from direct contact with an animal's saliva or puncture wound.
Environmental reservoirs in healthcare settings US Medical PG Question 8: A 55-year-old man presents to the physician with complaints of 5 days of watery diarrhea, fever, and bloating. He has not noticed any blood in his stool. He states that his diet has not changed recently, and his family has been spared from diarrhea symptoms despite eating the same foods that he has been cooking at home. He has no history of recent travel outside the United States. His only medication is high-dose omeprazole, which he has been taking daily for the past few months to alleviate his gastroesophageal reflux disease (GERD). Which of the following is the most appropriate initial test to work up this patient’s symptoms?
- A. Stool toxin assay (Correct Answer)
- B. Colonoscopy
- C. Fecal occult blood test
- D. Stool culture
- E. Stool ova and parasite
Environmental reservoirs in healthcare settings Explanation: ***Stool toxin assay***
- The patient's presentation of **watery diarrhea** and fever, especially with a history of **high-dose omeprazole use**, strongly suggests **Clostridioides difficile infection**.
- **Omeprazole** (a proton pump inhibitor) reduces stomach acid, which can disrupt the normal gut flora and increase susceptibility to *C. difficile*; a **stool toxin assay** is the most direct diagnostic test for this infection.
*Colonoscopy*
- While a colonoscopy can visualize pseudomembranes associated with severe *C. difficile* colitis, it is an **invasive procedure** and not the initial diagnostic test of choice for suspected infectious diarrhea.
- It is usually reserved for cases with atypical presentations, suspected complications, or when other diagnostic tests are inconclusive.
*Fecal occult blood test*
- The patient describes **watery diarrhea** and specifically states he has **not noticed any blood in his stool**, making a fecal occult blood test unlikely to be helpful in this acute setting.
- This test is primarily used for screening **colorectal cancer** or identifying chronic gastrointestinal bleeding.
*Stool culture*
- A stool culture primarily identifies bacterial pathogens like *Salmonella*, *Shigella*, or *Campylobacter*, which typically cause diarrheal illnesses that may include **bloody stools** or have specific epidemiological links (e.g., foodborne outbreaks).
- Given the history of **omeprazole use** and the absence of blood, *C. difficile* is more likely than these common bacterial enteritides, and a stool culture does not detect *C. difficile* itself.
*Stool ova and parasite*
- This test is used to detect **parasitic infections** (e.g., Giardia, Cryptosporidium), which can cause watery diarrhea and bloating.
- However, given the specific risk factor of **omeprazole use**, **Clostridioides difficile** infection is a more probable diagnosis, making the stool toxin assay the more appropriate initial test.
Environmental reservoirs in healthcare settings US Medical PG Question 9: A 42-year-old man presents with unremitting diarrhea that has lasted for 2 weeks. He describes his bowel movements as watery, non-bloody, foul-smelling, and greasy. He also has cramping abdominal pain associated with the diarrhea. He says that his symptoms started right after he returned from a father-son camping trip to the mountains. His son has similar symptoms. His vital signs include: pulse 78/min, respiratory rate 15/min, temperature 37.2°C (99.0°F), and blood pressure 120/70 mm Hg. A stool sample is obtained and microscopic analysis is significant for the findings shown in the image below. Which of the following pathogens is most likely responsible for this patient’s condition?
- A. Giardia lamblia (Correct Answer)
- B. Yersinia enterocolitica
- C. Bacillus cereus
- D. Clostridium difficile
- E. Campylobacter jejuni
Environmental reservoirs in healthcare settings Explanation: ***Giardia lamblia***
- The patient's symptoms of **watery, non-bloody, foul-smelling, greasy stools** (steatorrhea) with abdominal cramping after a camping trip are classic for giardiasis. The image shows a **trophozoite of Giardia lamblia**, characterized by its pear shape, multiple flagella, and two nuclei, often described as having an "old man's face" appearance.
- The **epidemiological context** (camping trip, son with similar symptoms) suggests exposure to contaminated water, a common source of *Giardia* infection.
*Yersinia enterocolitica*
- This pathogen typically causes **bloody diarrhea**, fever, and sometimes abdominal pain that can mimic appendicitis (*pseudoappendicitis*), which are not present in this case.
- It's mainly associated with consuming **undercooked pork** or contaminated milk products, not typically recreational water exposure.
*Bacillus cereus*
- This bacterium causes **food poisoning** with either an emetic form (vomiting) due to preformed toxins in **fried rice** or a diarrheal form (watery diarrhea) associated with meat and vegetable dishes.
- The incubation periods are usually short (1-6 hours for emetic, 6-15 hours for diarrheal), which does not fit the 2-week duration described.
*Clostridium difficile*
- *C. difficile* infection is characterized by **watery diarrhea** and **abdominal cramps**, often following **antibiotic use** or in healthcare settings, which are not mentioned here.
- While it can cause severe diarrhea, the stool is usually not described as greasy, and the image does not show *C. difficile* organisms or their toxins.
*Campylobacter jejuni*
- This bacterium is a common cause of **bacterial gastroenteritis**, typically presenting with **bloody diarrhea**, fever, and abdominal pain.
- It is often acquired from contaminated **poultry** or unpasteurized milk, and is associated with complications like **Guillain-Barré syndrome**, none of which are suggested by the clinical picture or image.
Environmental reservoirs in healthcare settings US Medical PG Question 10: A surgical ICU has implemented multiple interventions over 18 months: chlorhexidine bathing, antibiotic stewardship, contact precautions for MRSA, and environmental cleaning protocols. Despite these efforts, MRSA surgical site infection rates remain unchanged at 8 per 1000 surgical procedures. Universal MRSA screening shows 15% of admitted patients are colonized. Evaluate the most effective evidence-based strategy to reduce MRSA SSI rates further.
- A. Targeted decolonization only for MRSA-positive patients with mupirocin and chlorhexidine
- B. Isolation of all surgical patients in private rooms until discharge
- C. Routine screening and decolonization of all healthcare workers
- D. Extended vancomycin prophylaxis for all surgical patients for 48 hours postoperatively
- E. Universal MRSA decolonization for all surgical patients regardless of screening results (Correct Answer)
Environmental reservoirs in healthcare settings Explanation: ***Universal MRSA decolonization for all surgical patients regardless of screening results***
- **Universal decolonization** has been proven more effective than screening-based strategies in high-risk settings like the ICU, significantly reducing **MRSA surgical site infections** and bloodstream infections.
- This approach is superior because it addresses **undetected carriers**, eliminates delays associated with waiting for lab cultures, and is often more **cost-effective** and easier to implement.
*Targeted decolonization only for MRSA-positive patients with mupirocin and chlorhexidine*
- While logical, **targeted decolonization** is less effective than the universal approach because it misses patients who may be **falsely negative** or colonized at levels below detection thresholds.
- Evidence from recent large-scale trials shows that **targeted strategies** do not reduce MRSA infection rates as drastically as treating the entire cohort at risk.
*Isolation of all surgical patients in private rooms until discharge*
- This strategy is **logistically impractical** and extremely expensive, focusing on **containment** rather than the active reduction of the patient's own bacterial load (colonization).
- Research indicates that **contact precautions** and isolation alone are less effective than decolonization protocols in preventing **autoinoculation** during surgery.
*Routine screening and decolonization of all healthcare workers*
- Screening of **healthcare workers (HCWs)** is not recommended as a routine practice; it is typically reserved for **outbreak investigations** where an epidemiological link is suspected.
- Constant recolonization from patients and the environment makes **HCW decolonization** an unsustainable and transient solution for reducing overall SSI rates.
*Extended vancomycin prophylaxis for all surgical patients for 48 hours postoperatively*
- **Extended antibiotic prophylaxis** beyond 24 hours provides no additional protection against SSIs and significantly increases the risk of **C. difficile** and antibiotic resistance.
- Proper surgical prophylaxis involves **timely administration** before the incision, not prolonged courses which violate **antibiotic stewardship** principles.
More Environmental reservoirs in healthcare settings US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.