Clostridium difficile infection US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Clostridium difficile infection. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Clostridium difficile infection US Medical PG Question 1: An 87-year-old male nursing home resident is currently undergoing antibiotic therapy for the treatment of a decubitus ulcer. One week into the treatment course, he experiences several episodes of watery diarrhea. Subsequent sigmoidoscopy demonstrates the presence of diffuse yellow plaques on the mucosa of the sigmoid colon. Which of the following is the best choice of treatment for this patient?
- A. Intravenous vancomycin
- B. Intravenous gentamicin
- C. Oral metronidazole (Correct Answer)
- D. Oral trimethoprim/sulfamethoxazole
- E. Oral morphine
Clostridium difficile infection Explanation: ***Oral metronidazole***
- The patient's presentation with **watery diarrhea** and **yellow plaques (pseudomembranes) on sigmoidoscopy** after antibiotic therapy is classic for **Clostridioides difficile infection (CDI)**.
- Among the options provided, **oral metronidazole** is the best choice as it achieves therapeutic concentrations in the colonic lumen and has activity against C. difficile.
- Current **IDSA guidelines** recommend oral **vancomycin or fidaxomicin** as first-line therapy for CDI; however, metronidazole remains an acceptable alternative, particularly in resource-limited settings or when first-line agents are unavailable.
- Metronidazole has good **colonic penetration** when administered orally and is effective against anaerobic bacteria including C. difficile.
*Intravenous vancomycin*
- While **vancomycin** is highly effective against C. difficile, it **must be administered orally** to treat CDI because IV vancomycin does not achieve adequate concentrations in the gut lumen.
- Intravenous vancomycin is excreted primarily by the kidneys and does not reach the colonic mucosa in therapeutic amounts.
- IV vancomycin is appropriate for systemic infections like **MRSA bacteremia or endocarditis**, but not for intestinal infections like CDI.
*Intravenous gentamicin*
- **Gentamicin** is an aminoglycoside antibiotic effective against **gram-negative bacteria** but has **no activity against C. difficile**, which is a gram-positive anaerobic bacillus.
- Aminoglycosides carry significant risks of **nephrotoxicity and ototoxicity**, making them inappropriate for this clinical scenario.
- Use of gentamicin would not address the underlying CDI and could worsen outcomes.
*Oral trimethoprim/sulfamethoxazole*
- **Trimethoprim/sulfamethoxazole** is a broad-spectrum antibiotic effective for various infections (UTIs, Pneumocystis, etc.) but has **no significant activity against C. difficile**.
- Continued antibiotic use with agents ineffective against C. difficile could further disrupt normal gut flora and potentially **worsen the CDI**.
*Oral morphine*
- **Morphine** is an opioid analgesic with **no antibacterial properties** and therefore cannot treat bacterial infections like CDI.
- Opioids can actually **slow gastrointestinal motility**, which may worsen outcomes in CDI by prolonging exposure to toxins.
- While it might provide symptomatic relief of abdominal discomfort, it does not address the underlying infection and is contraindicated in infectious diarrhea.
Clostridium difficile infection US Medical PG Question 2: On the 4th day of hospital admission due to pneumonia, a 69-year-old woman develops non-bloody diarrhea and abdominal pain. She is currently treated with ceftriaxone. Despite the resolution of fever after the first 2 days of admission, her temperature is now 38.5°C (101.3°F). On physical examination, she has mild generalized abdominal tenderness without abdominal guarding or rebound tenderness. Laboratory studies show re-elevation of leukocyte counts. Ceftriaxone is discontinued. Given the most likely diagnosis in this patient, which of the following is the most sensitive test?
- A. Nucleic acid amplification test (Correct Answer)
- B. Stool culture for bacterial isolation and toxin presence
- C. Enzyme immunoassay glutamate dehydrogenase
- D. Gram stain of stool sample
- E. Endoscopy
Clostridium difficile infection Explanation: ***Nucleic acid amplification test***
- **NAAT** (PCR) for *C. difficile* toxin genes is the most **sensitive** and specific test for routine clinical diagnosis of *C. difficile* infection.
- It detects the **DNA** of toxin-producing *C. difficile* (tcdB gene) and is highly reliable even with low bacterial loads.
- NAAT has become the **gold standard** in most clinical settings due to its rapid turnaround time (hours) and excellent sensitivity (~90-95%) and specificity (~95%).
*Enzyme immunoassay glutamate dehydrogenase*
- **EIA GDH** detects an antigen common to all *C. difficile* strains (both toxin-producing and non-toxin-producing).
- While it has **high sensitivity** (~85-95%), it has **low specificity** and requires confirmation with a toxin test or NAAT, as it cannot distinguish between toxigenic and non-toxigenic strains.
- Often used as part of a **two-step algorithm** for screening.
*Gram stain of stool sample*
- A **Gram stain** of stool is generally not helpful for diagnosing *C. difficile* infection.
- It would show a mix of **gut flora** and would not specifically identify *C. difficile* or its toxins.
*Stool culture for bacterial isolation and toxin presence*
- **Stool culture** for *C. difficile* is technically the most sensitive method (~95-100%) but does not differentiate toxin-producing from non-toxin-producing strains without subsequent **toxin testing**.
- It is also **time-consuming** (2-3 days) and labor-intensive, making it impractical for routine clinical diagnosis.
- Primarily used for **research** or **epidemiological typing**.
*Endoscopy*
- **Endoscopy** with visualization of **pseudomembranes** is highly specific for severe *C. difficile* infection.
- However, it is an **invasive procedure**, not sensitive for mild-to-moderate disease, and is usually reserved for cases where diagnosis is unclear or severe complications (toxic megacolon, fulminant colitis) are suspected.
Clostridium difficile infection US Medical PG Question 3: A 42-year-old man with hypertension and type 2 diabetes mellitus is admitted to the hospital because of swelling and redness of the left leg for 3 days. He has chills and malaise. He is treated with intravenous clindamycin for 7 days. On the 8th day at the hospital, he has profuse, foul-smelling, and watery diarrhea. He has nausea and intermittent abdominal cramping. His temperature is 38°C (100.4°F), pulse is 97/min, and blood pressure is 110/78 mm Hg. Bowel sounds are hyperactive. Abdominal examination shows mild tenderness in the left lower quadrant. Rectal examination shows no abnormalities. His hemoglobin concentration is 14.3 g/dL, leukocyte count is 12,300/mm3, and C-reactive protein concentration is 62 mg/L (N=0.08–3.1). After discontinuing clindamycin, which of the following is the most appropriate pharmacotherapy for this patient's condition?
- A. Intravenous vancomycin
- B. Oral fidaxomicin (Correct Answer)
- C. Intravenous metronidazole
- D. Oral metronidazole
- E. Oral rifaximin
Clostridium difficile infection Explanation: ***Oral fidaxomicin***
- The patient's presentation with profuse, foul-smelling, watery diarrhea, abdominal cramping, and fever after prolonged antibiotic use (clindamycin) is highly suggestive of **Clostridioides difficile infection (CDI)**.
- **Oral fidaxomicin** is a first-line agent for initial CDI episodes with **superior efficacy** in reducing recurrence rates compared to metronidazole and similar cure rates to oral vancomycin. It is preferred due to its **narrow spectrum**, **bactericidal activity against C. difficile**, and **minimal disruption to normal colonic flora**.
- Current IDSA/SHEA guidelines recommend fidaxomicin or oral vancomycin as first-line therapy for initial CDI episodes.
*Intravenous vancomycin*
- **Intravenous vancomycin** has poor penetration into the GI tract and is therefore **ineffective for C. difficile infection (CDI)**, which is an intraluminal infection.
- Oral vancomycin is effective for CDI, but intravenous administration will not treat the infection.
*Intravenous metronidazole*
- **Intravenous metronidazole** has limited efficacy in treating **Clostridioides difficile infection (CDI)** as first-line therapy.
- While it achieves some colonic concentration even when given intravenously, oral agents (fidaxomicin or vancomycin) are preferred for initial episodes.
- IV metronidazole may be used as adjunctive therapy in fulminant cases with ileus when oral agents cannot reach the colon.
*Oral metronidazole*
- **Oral metronidazole** was previously used for non-severe CDI but is **no longer recommended as first-line therapy** per updated IDSA/SHEA guidelines due to inferior cure rates and higher recurrence rates compared to vancomycin and fidaxomicin.
- It may be considered only when fidaxomicin and vancomycin are unavailable.
*Oral rifaximin*
- **Oral rifaximin** is sometimes used as **adjunctive therapy following standard treatment** to prevent recurrent C. difficile infection (CDI).
- It is **not recommended as initial monotherapy** for an active CDI episode.
Clostridium difficile infection US Medical PG Question 4: A 24-year-old man presents to the emergency department for severe abdominal pain for the past day. The patient states he has had profuse, watery diarrhea and abdominal pain that is keeping him up at night. The patient also claims that he sees blood on the toilet paper when he wipes and endorses having lost 5 pounds recently. The patient's past medical history is notable for IV drug abuse and a recent hospitalization for sepsis. His temperature is 99.5°F (37.5°C), blood pressure is 120/68 mmHg, pulse is 100/min, respirations are 14/min, and oxygen saturation is 98% on room air. On physical exam, you note a young man clutching his abdomen in pain. Abdominal exam demonstrates hyperactive bowel sounds and diffuse abdominal tenderness. Cardiopulmonary exam is within normal limits. Which of the following is the next best step in management?
- A. Vancomycin (Correct Answer)
- B. Mesalamine enema
- C. Metronidazole
- D. Clindamycin
- E. Supportive therapy and ciprofloxacin if symptoms persist
Clostridium difficile infection Explanation: ***Vancomycin***
- The patient's history of **IV drug abuse**, recent **hospitalization for sepsis**, and severe abdominal symptoms with **bloody diarrhea** and **weight loss** are highly suggestive of **Clostridioides difficile infection (CDI)**.
- **Oral vancomycin** is the recommended first-line treatment for **severe C. difficile infection**, especially with signs like systemic illness (tachycardia) and marked abdominal tenderness.
*Mesalamine enema*
- **Mesalamine** is an **anti-inflammatory drug** primarily used for **mild to moderate ulcerative colitis**, particularly when the disease is limited to the rectum or rectosigmoid colon.
- While inflammatory bowel disease can cause bloody diarrhea, the acute presentation with recent hospitalization and IV drug use makes **infectious etiologies**, particularly CDI, much more likely.
*Metronidazole*
- **Metronidazole** is an antibiotic that was previously used for uncomplicated **C. difficile infection**.
- However, **oral vancomycin** is now preferred for **initial CDI episodes** due to superior efficacy, especially in severe cases, and metronidazole is generally reserved for non-severe cases if vancomycin is unavailable or not tolerated.
*Clindamycin*
- **Clindamycin** is an antibiotic notorious for being a common cause of **antibiotic-associated C. difficile infection**.
- Giving clindamycin in this scenario would likely **worsen the patient's condition** if C. difficile is indeed the cause, as it promotes C. difficile overgrowth.
*Supportive therapy and ciprofloxacin if symptoms persist*
- While **supportive care** (hydration, electrolyte management) is essential, it is **insufficient as the sole treatment** for severe C. difficile infection.
- **Ciprofloxacin** is an antibiotic that is **ineffective against C. difficile** and could potentially exacerbate the infection by disrupting the normal gut microbiota.
Clostridium difficile infection US Medical PG Question 5: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Clostridium difficile infection Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Clostridium difficile infection US Medical PG Question 6: A 54-year-old man presents with fever, abdominal pain, nausea, and bloody diarrhea. He says that his symptoms started 36 hours ago and have not improved. Past medical history is significant for a left-leg abscess secondary to an injury he sustained from a fall 4 days ago while walking his dog. He has been taking clindamycin for this infection. In addition, he has long-standing gastroesophageal reflux disease, managed with omeprazole. His vital signs include: temperature 38.5°C (101.3°F), respiratory rate 19/min, heart rate 90/min, and blood pressure 110/70 mm Hg. Which of the following is the best course of treatment for this patient’s most likely diagnosis?
- A. Tetracycline
- B. Ciprofloxacin
- C. Trimethoprim-sulfamethoxazole
- D. Erythromycin
- E. Vancomycin (Correct Answer)
Clostridium difficile infection Explanation: ***Vancomycin***
- The patient's history of recent **clindamycin** use for an abscess, development of **fever, abdominal pain, nausea, and bloody diarrhea**, and use of **omeprazole** (a risk factor), strongly suggests **_Clostridioides difficile_ infection (CDI)**.
- **Oral vancomycin** is a first-line treatment for **severe non-fulminant CDI**, which this patient's symptoms (fever, bloody diarrhea) are consistent with.
*Tetracycline*
- **Tetracycline** is typically used for bacterial infections like **chlamydia, Lyme disease, and rickettsial infections**; it is not effective against _C. difficile_.
- It works by **inhibiting bacterial protein synthesis** but does not target the cell wall of _C. difficile_.
*Ciprofloxacin*
- **Ciprofloxacin**, a fluoroquinolone, is generally **contraindicated in CDI** as it can be a risk factor for developing the infection or exacerbate it due to disruption of gut flora.
- While effective against many gram-negative bacteria, it has **no significant activity against _C. difficile_**.
*Trimethoprim-sulfamethoxazole*
- **Trimethoprim-sulfamethoxazole** is a combination antibiotic used for various bacterial infections, including **UTIs and some respiratory infections**.
- It is **not effective against _C. difficile_** and is not recommended for its treatment.
*Erythromycin*
- **Erythromycin**, a macrolide, is effective against a range of bacterial infections including **atypical pneumonia and skin infections**.
- It has **no role in the treatment of _C. difficile_ infection** and its use could potentially further disrupt the gut microbiome.
Clostridium difficile infection US Medical PG Question 7: A 55-year-old man presents to the physician with complaints of 5 days of watery diarrhea, fever, and bloating. He has not noticed any blood in his stool. He states that his diet has not changed recently, and his family has been spared from diarrhea symptoms despite eating the same foods that he has been cooking at home. He has no history of recent travel outside the United States. His only medication is high-dose omeprazole, which he has been taking daily for the past few months to alleviate his gastroesophageal reflux disease (GERD). Which of the following is the most appropriate initial test to work up this patient’s symptoms?
- A. Stool toxin assay (Correct Answer)
- B. Colonoscopy
- C. Fecal occult blood test
- D. Stool culture
- E. Stool ova and parasite
Clostridium difficile infection Explanation: ***Stool toxin assay***
- The patient's presentation of **watery diarrhea** and fever, especially with a history of **high-dose omeprazole use**, strongly suggests **Clostridioides difficile infection**.
- **Omeprazole** (a proton pump inhibitor) reduces stomach acid, which can disrupt the normal gut flora and increase susceptibility to *C. difficile*; a **stool toxin assay** is the most direct diagnostic test for this infection.
*Colonoscopy*
- While a colonoscopy can visualize pseudomembranes associated with severe *C. difficile* colitis, it is an **invasive procedure** and not the initial diagnostic test of choice for suspected infectious diarrhea.
- It is usually reserved for cases with atypical presentations, suspected complications, or when other diagnostic tests are inconclusive.
*Fecal occult blood test*
- The patient describes **watery diarrhea** and specifically states he has **not noticed any blood in his stool**, making a fecal occult blood test unlikely to be helpful in this acute setting.
- This test is primarily used for screening **colorectal cancer** or identifying chronic gastrointestinal bleeding.
*Stool culture*
- A stool culture primarily identifies bacterial pathogens like *Salmonella*, *Shigella*, or *Campylobacter*, which typically cause diarrheal illnesses that may include **bloody stools** or have specific epidemiological links (e.g., foodborne outbreaks).
- Given the history of **omeprazole use** and the absence of blood, *C. difficile* is more likely than these common bacterial enteritides, and a stool culture does not detect *C. difficile* itself.
*Stool ova and parasite*
- This test is used to detect **parasitic infections** (e.g., Giardia, Cryptosporidium), which can cause watery diarrhea and bloating.
- However, given the specific risk factor of **omeprazole use**, **Clostridioides difficile** infection is a more probable diagnosis, making the stool toxin assay the more appropriate initial test.
Clostridium difficile infection US Medical PG Question 8: A 72-year-old patient presents to the emergency department because of abdominal pain, diarrhea, and fever. He was started on levofloxacin for community-acquired pneumonia 2 weeks prior with resolution of his pulmonary symptoms. He has had hypertension for 20 years, for which he takes amlodipine. His temperature is 38.3°C (101.0°F), pulse is 90/min, and blood pressure is 110/70 mm Hg. On examination, mild abdominal distension with minimal tenderness was found. Laboratory tests reveal a peripheral white blood cell count of 12.000/mm3 and a stool guaiac mildly positive for occult blood. Which of the following best describe the mechanism of this patient illness?
- A. Damage to the gastrointestinal tract by enteropathogenic viruses
- B. Autoimmune inflammation of the rectum
- C. Disruption of normal bowel flora and infection by spore-forming rods (Correct Answer)
- D. Decreased blood flow to the gastrointestinal tract
- E. Presence of osmotically active, poorly absorbed solutes in the bowel lumen
Clostridium difficile infection Explanation: ***Disruption of normal bowel flora and infection by spore-forming rods***
- This describes **Clostridioides difficile infection (CDI)**, which is strongly suggested by the patient's recent antibiotic use (levofloxacin, a fluoroquinolone) followed by abdominal pain, diarrhea, fever, and leukocytosis.
- Antibiotics disrupt the normal gut microbiome, allowing **C. difficile (spore-forming rods)** to proliferate and produce toxins that cause colitis.
*Damage to the gastrointestinal tract by enteropathogenic viruses*
- While viral gastroenteritis can cause these symptoms, the **recent history of antibiotic use** makes CDI a much more likely diagnosis.
- Viral infections typically resolve spontaneously and are less likely to cause a significant **leukocytosis** and **occult blood in stool** in this context.
*Autoimmune inflammation of the rectum*
- Conditions like **ulcerative colitis**, an autoimmune disease, can cause similar symptoms but typically have a **chronic or relapsing course** and are not usually triggered by recent antibiotic use.
- The acute presentation following antibiotics strongly points away from an autoimmune process.
*Decreased blood flow to the gastrointestinal tract*
- **Ischemic colitis** can cause abdominal pain and bloody diarrhea, especially in older patients with vascular risk factors (like hypertension).
- However, the prominent **fever** and **leukocytosis**, coupled with recent antibiotic use, are more indicative of an infectious process like CDI than ischemia.
*Presence of osmotically active, poorly absorbed solutes in the bowel lumen*
- This mechanism describes **osmotic diarrhea**, which can be caused by malabsorption (e.g., lactose intolerance) or certain laxatives.
- Osmotic diarrhea typically **resolves with fasting** and is not usually associated with fever, significant leukocytosis, or occult blood in the stool, which are present here.
Clostridium difficile infection US Medical PG Question 9: A 12-month-old boy is brought to the emergency department by his mother for several hours of crying and severe abdominal pain, followed by dark and bloody stools in the last hour. The mother reports that she did not note any vomiting or fevers leading up to this incident. She does report that the boy and his 7-year-old sister recently had “stomach bugs” but that both have been fine and that the sister has gone back to school. The boy was born by spontaneous vaginal delivery at 39 weeks and 5 days after a normal pregnancy. His temperature is 100.4°F (38.0°C), blood pressure is 96/72 mmHg, pulse is 90/min, respirations are 22/min. Which of the following was most likely to play a role in the pathogenesis of this patient’s disease?
- A. Vascular malformation
- B. Hyperplasia of Peyer patches (Correct Answer)
- C. Embolism to the mesenteric vessels
- D. Intestinal mass
- E. Failure of neural crest migration
Clostridium difficile infection Explanation: ***Hyperplasia of Peyer patches***
- The presentation of a 12-month-old with **severe abdominal pain**, **crying spells**, and **dark, bloody stools** (likely **currant jelly stools**) is highly suggestive of **intussusception**.
- In children, intussusception is most commonly idiopathic, but often associated with recent viral illnesses causing **lymphoid hyperplasia** (Peyer patches) in the ileum, which then acts as a lead point for telescoping.
*Vascular malformation*
- This condition is a less common cause of rectal bleeding in infants and children and typically presents with **painless rectal bleeding**.
- It does not explain the acute, severe abdominal pain and signs of obstruction seen in intussusception.
*Embolism to the mesenteric vessels*
- **Mesenteric ischemia** due to embolism is rare in this age group and usually associated with underlying cardiac conditions or clotting disorders.
- While it can cause severe abdominal pain and bloody stools, the cyclical nature of pain and absence of significant risk factors make it less likely.
*Intestinal mass*
- Although an intestinal mass can be a lead point for intussusception (especially in older children or adults), it is a less common cause in uncomplicated cases in infants compared to **Peyer patch hyperplasia**.
- An intestinal mass would typically remain a fixed mass, and symptoms might be more chronic or progress differently.
*Failure of neural crest migration*
- This describes the pathogenesis of **Hirschsprung disease**, which presents with constipation, abdominal distention, and failure to pass meconium, rather than acute severe abdominal pain and bloody stools.
- The symptoms in this patient are acute and more indicative of an obstructive process like intussusception.
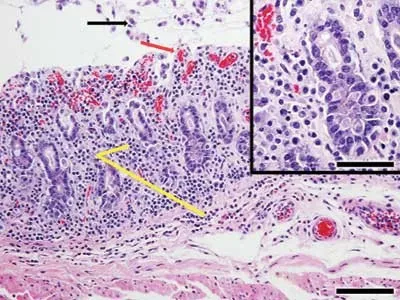
Clostridium difficile infection US Medical PG Question 10: A 7-year-old girl is brought to the physician by her mother because of a 4-week history of irritability, diarrhea, and a 2.2-kg (5-lb) weight loss that was preceded by a dry cough. The family returned from a vacation to Indonesia 2 months ago. Her vital signs are within normal limits. Abdominal examination shows mild tenderness with no guarding or rebound and increased bowel sounds. Her leukocyte count is 9,200/mm3 with 20% eosinophils. A photomicrograph of a wet stool mount is shown. Which of the following is the most appropriate pharmacotherapy?
- A. Diethylcarbamazine
- B. Metronidazole
- C. Albendazole (Correct Answer)
- D. Praziquantel
- E. Doxycycline
Clostridium difficile infection Explanation: ***Albendazole***
- The image shows a **hookworm egg**, characterized by its thin shell and developing larva inside; clinical features like **eosinophilia**, diarrhea, weight loss, and travel to an endemic area (Indonesia) are consistent with hookworm infection.
- **Albendazole** is the drug of choice for treating hookworm infections and other intestinal nematode infections.
*Diethylcarbamazine*
- This drug is primarily used for treating **lymphatic filariasis** (e.g., Wuchereria bancrofti, Brugia malayi) and **Loiasis** (African eye worm).
- It is not effective against hookworm infections.
*Metronidazole*
- **Metronidazole** is an antimicrobial agent effective against certain parasitic infections like **Giardia**, **Entamoeba histolytica**, and bacterial vaginosis.
- It is not indicated for the treatment of hookworm infections.
*Praziquantel*
- **Praziquantel** is an anthelminthic drug primarily used to treat infections caused by **flukes** (e.g., Schistosoma species) and **tapeworms** (e.g., Taenia species).
- It is not effective against hookworm infections.
*Doxycycline*
- **Doxycycline** is a tetracycline antibiotic with broad-spectrum activity against various bacterial infections and is also used in the treatment of some parasitic infections like **malaria prophylaxis** and **filariasis** (due to activity against Wolbachia endosymbionts).
- It is not a primary treatment for hookworm infections.
More Clostridium difficile infection US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.