Acute HIV infection US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Acute HIV infection. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Acute HIV infection US Medical PG Question 1: A 19-year-old university student presents to the student clinic with painful joints. He states that over the past week his right wrist has become increasingly stiff. This morning he noticed pain and stiffness in his left ankle and left knee. The patient has celiac disease and takes a daily multivitamin. He says he is sexually active with multiple male and female partners. He smokes marijuana but denies intravenous drug abuse. He recently traveled to Uganda to volunteer at a clinic that specialized in treating patients with human immunodeficiency virus (HIV). He also went on an extended hiking trip last week in New Hampshire. Physical exam reveals swelling of the right wrist and a warm, swollen, erythematous left knee. The left Achilles tendon is tender to palpation. There are also multiple vesicopustular lesions on the dorsum of the right hand. No penile discharge is appreciated. Arthrocentesis of the left knee is performed. Synovial fluid results are shown below:
Synovial fluid:
Appearance: Cloudy
Leukocyte count: 40,000/mm^3 with neutrophil predominance
Gram stain is negative. A synovial fluid culture is pending. Which of the following is the patient’s most likely diagnosis?
- A. Lyme disease
- B. Disseminated gonococcal infection (Correct Answer)
- C. Dermatitis herpetiformis
- D. Reactive arthritis
- E. Septic arthritis
Acute HIV infection Explanation: ### Disseminated gonococcal infection
- The patient's presentation with **migratory polyarthralgia**, tenosynovitis (tender Achilles tendon), and **vesicopustular skin lesions** in a sexually active individual strongly suggests disseminated gonococcal infection.
- The synovial fluid showing **leukocyte count of 40,000/mm^3** with neutrophil predominance and a negative Gram stain is consistent with a non-septic (culture-negative) arthritis, which is common in disseminated gonococcal infection.
*Lyme disease*
- While Lyme disease can cause migratory arthralgia, it typically presents with an **erythema chronicum migrans rash** and is less commonly associated with vesicopustular lesions or tenosynovitis of the Achilles tendon.
- The high synovial fluid leukocyte count and pustular rash are less typical for early Lyme arthritis.
*Dermatitis herpetiformis*
- This is a cutaneous manifestation of **celiac disease**, characterized by intensely pruritic papules and vesicles, primarily on extensor surfaces.
- It does **not typically cause joint pain** or the acute inflammatory arthritis seen in this patient.
*Reactive arthritis*
- Reactive arthritis can cause oligoarthritis and enthesitis (like Achilles tendonitis), often following a genitourinary or gastrointestinal infection [1].
- However, it is **not typically associated with vesicopustular skin lesions**, and the migratory pattern with prominent tenosynovitis points away from this diagnosis.
*Septic arthritis*
- While the synovial fluid leukocyte count is high and consistent with infection, the **negative Gram stain** and the presence of **multiple pustular skin lesions** make a diagnosis of disseminated gonococcal infection more likely compared to typical septic arthritis from other bacteria [2].
- Disseminated gonococcal infection often presents as a _septic arthritis without pus_ or a _polyarthralgia-dermatitis syndrome_, where cultures may be negative.
Acute HIV infection US Medical PG Question 2: A 32-year-old man comes to the physician for a follow-up examination 1 week after being admitted to the hospital for oral candidiasis and esophagitis. His CD4+ T lymphocyte count is 180 cells/μL. An HIV antibody test is positive. Genotypic resistance assay shows the virus to be susceptible to all antiretroviral therapy regimens and therapy with dolutegravir, tenofovir, and emtricitabine is initiated. Which of the following sets of laboratory findings would be most likely on follow-up evaluation 3 months later?
$$$ CD4 +/CD8 ratio %%% HIV RNA %%% HIV antibody test $$$
- A. ↓ ↓ negative
- B. ↑ ↑ negative
- C. ↓ ↑ negative
- D. ↑ ↓ positive (Correct Answer)
- E. ↓ ↑ positive
Acute HIV infection Explanation: ***↑ ↓ positive***
- With effective **antiretroviral therapy (ART)**, the **CD4+/CD8 ratio** would increase as **CD4+ T cell counts rise** and **CD8+ T cell counts decrease**.
- **HIV RNA (viral load)** would significantly decrease (ideally to undetectable levels) due to the suppression of viral replication, but HIV antibodies would remain positive indefinitely.
*↓ ↓ negative*
- A decrease in the **CD4+/CD8 ratio** and **HIV RNA** (viral load) along with a negative **HIV antibody test** is inconsistent with successful ART.
- A negative HIV antibody test would mean the patient was never infected, which contradicts the initial positive result and symptoms.
*↑ ↑ negative*
- An increase in the **CD4+/CD8 ratio** is expected with ART, but an increase in **HIV RNA** (viral load) indicates treatment failure.
- A negative **HIV antibody test** is impossible after a confirmed positive result, regardless of treatment success.
*↓ ↑ negative*
- A decrease in the **CD4+/CD8 ratio** would suggest worsening immune function, while an increase in **HIV RNA** indicates treatment failure.
- A negative **HIV antibody test** is not possible once a patient has developed antibodies to HIV.
*↓ ↑ positive*
- A decrease in the **CD4+/CD8 ratio** would indicate immune decline, contrary to the expected improvement with effective ART.
- An increase in **HIV RNA (viral load)** would signify treatment failure, even if HIV antibodies remain positive.
Acute HIV infection US Medical PG Question 3: A 17-year-old boy comes to the physician because of body aches and sore throat for 1 week. He has no history of serious illness and takes no medications. He lives with his parents; they recently adopted a cat from an animal shelter. He is sexually active with one female partner, and they use condoms consistently. His temperature is 38.7°C (101.7°F), pulse is 99/min, and blood pressure is 110/72 mm Hg. Examination shows bilateral posterior cervical lymphadenopathy. The pharynx is red and swollen. Laboratory studies show:
Hemoglobin 15 g/dL
Leukocyte count 11,500/mm3
Segmented neutrophils 48%
Band forms 2%
Basophils 0.5%
Eosinophils 1%
Lymphocytes 45%
Monocytes 3.5%
When the patient's serum is added to a sample of horse erythrocytes, the cells aggregate together. Which of the following is the most likely causal pathogen?
- A. Cytomegalovirus
- B. Influenza virus
- C. Toxoplasma gondii
- D. Epstein-Barr virus (Correct Answer)
- E. Human immunodeficiency virus
Acute HIV infection Explanation: ***Epstein-Barr virus***
- The patient's symptoms (fever, sore throat, **posterior cervical lymphadenopathy**) combined with **relative lymphocytosis** and a positive test where serum aggregates **horse erythrocytes** (heterophile antibody test, Monospot) are classic for **infectious mononucleosis** caused by EBV.
- While other conditions can cause similar symptoms, the specific constellation of fever, pharyngitis, posterior cervical lymphadenopathy, and a positive heterophile antibody test is highly indicative of EBV infection, particularly in an adolescent.
*Cytomegalovirus*
- CMV can cause a **mononucleosis-like syndrome** with fever, malaise, and abnormal liver function tests, but it typically presents with **absent pharyngitis** and **lymphadenopathy** is less prominent, or generalized rather than predominantly posterior cervical.
- CMV mononucleosis is characterized by a **negative heterophile antibody test**, differentiating it from EBV.
*Influenza virus*
- Influenza typically presents with an **acute onset of fever**, myalgia, headache, and respiratory symptoms like cough and rhinorrhea, and **lymphadenopathy is not a prominent feature**.
- Laboratory tests would show **neutrophilia or normal leukocyte count**, not the significant lymphocytosis seen here, and the heterophile antibody test would be negative.
*Toxoplasma gondii*
- **Toxoplasmosis** can cause **lymphadenopathy**, particularly cervical, but it's often **painless** and generalized. Pharyngitis and significant systemic symptoms like a high fever are less common, and it typically does not present with the same dramatic lymphocytosis.
- The positive heterophile antibody test in this case points away from toxoplasmosis, which would require specific serology for diagnosis and is sometimes linked to **cat exposure**, though not the primary finding here.
*Human immunodeficiency virus*
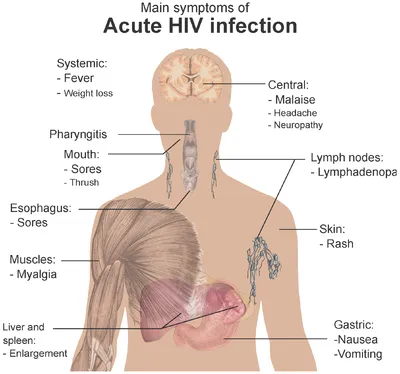
- **Acute HIV seroconversion syndrome** can present with a **mononucleosis-like illness**, including fever, pharyngitis, rash, and generalized lymphadenopathy, but **posterior cervical lymphadenopathy** specifically is not as classic as with EBV.
- The heterophile antibody test would be **negative** in HIV; diagnosis relies on HIV antigen/antibody testing or viral load measurement.
Acute HIV infection US Medical PG Question 4: A 40-year-old man presents with problems with his vision. He says he has been experiencing blurred vision and floaters in his left eye for the past few days. He denies any ocular pain, fever, or headaches. Past medical history is significant for HIV infection a few years ago, for which he is noncompliant with his antiretroviral medications and his most recent CD4 count was 100 cells/mm3. His temperature is 36.5°C (97.7°F), the blood pressure is 110/89 mm Hg, the pulse rate is 70/min, and the respiratory rate is 14/min. Ocular exam reveals a decreased vision in the left eye, and a funduscopic examination is shown in the image. The patient is admitted and immediately started on intravenous ganciclovir. A few days after admission he is still complaining of blurry vision and floaters, so he is switched to a different medication. Inhibition of which of the following processes best describes the mechanism of action of the newly added medication?
- A. Protein synthesis
- B. Nucleic acid synthesis (Correct Answer)
- C. Progeny virus release
- D. Viral penetration into host cells
- E. Viral uncoating
Acute HIV infection Explanation: ***Nucleic acid synthesis***
- This patient likely has **cytomegalovirus (CMV) retinitis**, characterized by **blurred vision**, **floaters**, and **necrotizing retinitis** in an HIV-positive individual with a **low CD4 count (100 cells/mm3)**.
- The initial drug, **ganciclovir**, targets nucleic acid synthesis by inhibiting viral DNA polymerase. If ganciclovir fails, a common second-line agent like **foscarnet** or **cidofovir** is used, and both also inhibit viral **nucleic acid (DNA) synthesis** through different mechanisms (foscarnet directly inhibits DNA polymerase, cidofovir is a nucleotide analog).
*Protein synthesis*
- This mechanism is targeted by certain antibacterial and antifungal drugs, but not typically by antiviral medications used for CMV.
- Antiviral drugs generally target specific viral processes, distinct from host protein synthesis, to limit toxicity.
*Progeny virus release*
- This mechanism is primarily targeted by **neuraminidase inhibitors** (e.g., oseltamivir, zanamivir) used to treat influenza, which prevent the release of new viral particles from infected cells.
- It is not a common mechanism for CMV antivirals.
*Viral penetration into host cells*
- Medications that inhibit viral penetration or entry, such as **fusion inhibitors** (e.g., enfuvirtide for HIV) or **CCR5 antagonists** (e.g., maraviroc for HIV), prevent the virus from entering the host cell.
- These mechanisms are not relevant to the treatment of CMV retinitis.
*Viral uncoating*
- **Amantadine** and **rimantadine** are examples of antiviral drugs that inhibit **viral uncoating** by interfering with the M2 ion channel in influenza A.
- This mechanism is specific to influenza viruses and is not involved in the action of CMV antiviral medications.
Acute HIV infection US Medical PG Question 5: A 44-year-old man with HIV comes to the physician for a routine follow-up examination. He has been noncompliant with his antiretroviral medication regimen for several years. He appears chronically ill and fatigued. CD4+ T-lymphocyte count is 180/mm³ (N ≥ 500). Further evaluation of this patient is most likely to show which of the following findings?
- A. Multifocal demyelination on brain MRI
- B. Violaceous lesions on skin exam (Correct Answer)
- C. Ring-enhancing lesions on brain MRI
- D. Cotton-wool spots on fundoscopy
- E. Ground-glass opacities on chest CT
Acute HIV infection Explanation: ***Violaceous lesions on skin exam***
- A CD4 count of 180/mm³ indicates severe **immunosuppression**, making the patient highly susceptible to **opportunistic infections** and cancers, such as Kaposi sarcoma.
- **Kaposi sarcoma** typically presents with violaceous (purple-blue) cutaneous lesions, which are often the initial manifestation of the disease in HIV-positive patients.
*Multifocal demyelination on brain MRI*
- This finding is characteristic of **progressive multifocal leukoencephalopathy (PML)**, caused by the **JC virus**.
- PML typically occurs at **CD4 counts below 100/mm³**, lower than the patient's current count, although still possible with severe immunosuppression.
*Ring-enhancing lesions on brain MRI*
- **Ring-enhancing lesions** on brain MRI are often seen in cerebral **toxoplasmosis** or CNS **lymphoma** in HIV patients.
- Toxoplasmosis usually presents with focal neurological deficits and seizures, and is more common with CD4 counts below 100/mm³.
*Cotton-wool spots on fundoscopy*
- **Cotton-wool spots** are a common finding in **HIV retinopathy** due to retinal ischemia.
- While possible, they are non-specific and are usually asymptomatic, whereas the patient's presentation suggests a more prominent and diagnosable condition.
*Ground-glass opacities on chest CT*
- **Ground-glass opacities** on chest CT are characteristic of **Pneumocystis jirovecii pneumonia (PJP)**, a common opportunistic infection in HIV patients.
- While PJP is a strong possibility with a CD4 count <200/mm³, the question asks for a finding that is *most likely* given the patient's general appearance and the option of Kaposi sarcoma, which manifests directly on examination.
Acute HIV infection US Medical PG Question 6: A 28-year-old G1P0 woman at 16 weeks estimated gestational age presents for prenatal care. Routine prenatal screening tests are performed and reveal a positive HIV antibody test. The patient is extremely concerned about the possible transmission of HIV to her baby and wants to have the baby tested as soon as possible after delivery. Which of the following would be the most appropriate diagnostic test to address this patient’s concern?
- A. CD4+ T cell count
- B. Viral culture
- C. Polymerase chain reaction (PCR) for HIV RNA (Correct Answer)
- D. Antigen assay for p24
- E. EIA for HIV antibody
Acute HIV infection Explanation: ***Polymerase chain reaction (PCR) for HIV RNA***
- **PCR for HIV RNA** directly detects the viral genetic material, providing a definitive diagnosis of HIV infection in an infant.
- Unlike antibody tests, PCR can distinguish between passively acquired maternal antibodies and actual infant infection, making it suitable for newborns.
*CD4+ T cell count*
- **CD4+ T cell count** is used to monitor the progression of HIV infection and immunosuppression, not for initial diagnosis, especially in neonates.
- While it's an important marker for HIV disease, it does not confirm the presence of the virus itself in a newborn.
*Viral culture*
- **Viral culture** is a highly specific method for detecting HIV, but it is expensive, time-consuming, and technically demanding.
- It is not routinely used for rapid early diagnosis in neonates due to its practical limitations and the availability of faster, reliable alternatives like PCR.
*Antigen assay for p24*
- The **p24 antigen test** can detect early HIV infection in adults, but its sensitivity is lower in neonates compared to PCR, especially immediately after birth.
- It may not reliably detect infection in newborns due to low viral loads or the presence of maternal antibodies that complex the antigen.
*EIA for HIV antibody*
- An **EIA for HIV antibody** will detect maternal antibodies that have crossed the placenta, meaning it will be positive in nearly all infants born to HIV-positive mothers, regardless of the infant's infection status.
- This test cannot distinguish between passive maternal antibody transfer and true infant infection.
Acute HIV infection US Medical PG Question 7: A 19-year-old woman presents to the family medical center with a 2-week history of a sore throat. She says that she has felt increasingly tired during the day and has a difficult time staying awake during her classes at the university. She appears well-nourished with a low energy level. Her vital signs include the following: the heart rate is 82/min, the respiratory rate is 14/min, the temperature is 37.8°C (100.0°F), and the blood pressure is 112/82 mm Hg. Inspection of the pharynx is depicted in the picture. Palpation of the neck reveals posterior cervical lymphadenopathy. The membrane does not bleed upon scraping. What is the most specific finding for detecting the syndrome described in the vignette?
- A. > 10% atypical lymphocytes
- B. Positive rapid strep test
- C. Growth in Loffler’s medium
- D. Increased transaminase levels
- E. Positive monospot test (Correct Answer)
Acute HIV infection Explanation: ***Positive monospot test***
- The patient's symptoms (sore throat, fatigue, posterior cervical lymphadenopathy, pharyngitis with exudates, age) are highly suggestive of **infectious mononucleosis**, which is caused by the **Epstein-Barr virus (EBV)**.
- A **positive monospot test**, which detects **heterophile antibodies**, is the most specific and widely used rapid diagnostic test for infectious mononucleosis.
* > 10% atypical lymphocytes*
- While **atypical lymphocytes** are characteristic of infectious mononucleosis, they are not exclusive to EBV infection and can be seen in other viral infections (e.g., CMV, HIV). Therefore, this finding is less specific than a positive monospot test.
- A definitive diagnosis usually requires a combination of clinical symptoms and specific serological tests like the **monospot test** or **EBV-specific antibodies**.
*Positive rapid strep test*
- A rapid strep test detects **Group A Streptococcus (GAS)**. While bacterial pharyngitis can present with a sore throat, the accompanying fatigue and posterior cervical lymphadenopathy make streptococcal pharyngitis less likely as the primary diagnosis.
- The rapid strep test would be negative in infectious mononucleosis, and therefore, a positive result would rule out mononucleosis as the sole cause.
*Growth in Loffler’s medium*
- **Loffler's medium** is used to culture **Corynebacterium diphtheriae**, the causative agent of diphtheria. Diphtheria presents with a severe sore throat and a tenacious gray membrane that **bleeds upon scraping**, unlike the description in the vignette.
- While it's a specific diagnostic test for diphtheria, the patient's presentation does not align with diphtheria, and this test would not be positive in infectious mononucleosis.
*Increased transaminase levels*
- **Increased transaminase levels** (AST, ALT) indicate liver involvement, which can occur in infectious mononucleosis due to **hepatitis**.
- While this is a common finding in many cases of mononucleosis (and supports the diagnosis), it is an indicator of organ involvement rather than a specific diagnostic test for the presence of the virus or its unique immunological response (like the monospot test).
Acute HIV infection US Medical PG Question 8: A 35-year-old man comes to the emergency department with fever, chills, dyspnea, and a productive cough. His symptoms began suddenly 2 days ago. He was diagnosed with HIV 4 years ago and has been on triple antiretroviral therapy since then. He smokes one pack of cigarettes daily. He is 181 cm (5 ft 11 in) tall and weighs 70 kg (154 lb); BMI is 21.4 kg/m2. He lives in Illinois and works as a carpenter. His temperature is 38.8°C (101.8°F), pulse is 110/min, respirations are 24/min, and blood pressure is 105/74 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 92%. Examinations reveals crackles over the right lower lung base. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 11.5 g/dL
Leukocyte count 12,800/mm3
Segmented neutrophils 80%
Eosinophils 1%
Lymphocytes 17%
Monocytes 2%
CD4+ T-lymphocytes 520/mm3(N ≥ 500)
Platelet count 258,000/mm3
Serum
Na+ 137 mEq/L
Cl- 102 mEq/L
K+ 5.0 mEq/L
HCO3- 22 mEq/L
Glucose 92 mg/dL
An x-ray of the chest shows a right lower-lobe infiltrate of the lung. Which of the following is the most likely causal organism?
- A. Streptococcus pneumoniae (Correct Answer)
- B. Legionella pneumophila
- C. Pneumocystis jirovecii
- D. Staphylococcus aureus
- E. Cryptococcus neoformans
Acute HIV infection Explanation: ***Streptococcus pneumoniae***
- This patient presents with **fever, chills, productive cough, dyspnea, leukocytosis with neutrophilia, and a lobar infiltrate on chest X-ray**, which are classic signs of **community-acquired bacterial pneumonia**.
- Although the patient is **HIV-positive**, his CD4+ count is >500/mm3 and he is on antiretroviral therapy, indicating relatively preserved immune function, making *S. pneumoniae* the most common cause of pneumonia even in HIV-infected individuals with controlled disease.
*Legionella pneumophila*
- While *Legionella* can cause pneumonia with fever and dyspnea, it is often associated with **gastrointestinal symptoms** (e.g., diarrhea) and **hyponatremia**, which are not present here.
- Exposure to contaminated water sources is a common risk factor, and the lobar infiltrate is less typical than diffuse or patchy infiltrates.
*Pneumocystis jirovecii*
- *Pneumocystis pneumonia (PJP)* is typically seen in **HIV patients with severely suppressed immune systems (CD4+ count <200/mm3)**.
- The patient's CD4+ count (520/mm3) is above this threshold, and PJP usually presents with diffuse interstitial infiltrates rather than a lobar infiltrate.
*Staphylococcus aureus*
- *S. aureus* pneumonia often occurs in the context of recent **influenza infection, intravenous drug use, or hospitalization**, or can present rapidly with **necrotizing pneumonia** or **empyema**.
- While possible, the absence of these specific risk factors or severe features makes it less likely than *S. pneumoniae* in this specific presentation.
*Cryptococcus neoformans*
- *Cryptococcus neoformans* is an opportunistic fungus that typically causes **pulmonary or central nervous system infections**, especially in severely immunocompromised patients (CD4+ count usually <100/mm3).
- Pulmonary cryptococcosis often manifests as **nodules or cavitary lesions**, or can be asymptomatic, which differs from the acute lobar pneumonia presented.
Acute HIV infection US Medical PG Question 9: A 26-year-old female medical student presents to occupational health after sustaining a needlestick injury. She reports that she was drawing blood from an HIV-positive patient when she stuck herself percutaneously while capping the needle. She immediately washed the puncture wound with betadine. The medical student has a negative HIV serology from the beginning of medical school two years ago. She is monogamous with one male partner and denies any intravenous drug use. The source patient was recently diagnosed with HIV, and has a CD4 count of 550 cells/µL. His most recent viral load is 1,800,000 copies/mL, and he was started on HAART three days ago.
Which of the following is the best next step to manage the female medical student’s exposure?
- A. Draw her repeat HIV serology and initiate three-drug antiretroviral therapy if positive
- B. Perform genotype testing on source patient and initiate antiretroviral therapy tailored to results
- C. Immediately initiate three-drug antiretroviral therapy
- D. Draw her repeat HIV serology and immediately initiate three-drug antiretroviral therapy (Correct Answer)
- E. Draw her repeat HIV serology and initiate three-drug antiretroviral therapy if negative
Acute HIV infection Explanation: ***Draw her repeat HIV serology and immediately initiate three-drug antiretroviral therapy***
- This approach ensures that baseline **HIV status** is established while simultaneously providing **post-exposure prophylaxis (PEP)** as quickly as possible. Time is critical for PEP efficacy.
- The patient has a high-risk exposure (percutaneous injury, high viral load source) warranting immediate initiation of a **three-drug antiretroviral regimen** to prevent seroconversion.
*Draw her repeat HIV serology and initiate three-drug antiretroviral therapy if positive*
- Waiting for serology results before initiating therapy would delay PEP, significantly reducing its effectiveness in potentially preventing **HIV transmission**.
- If the student is already HIV-positive from a prior undisclosed exposure, PEP for a new exposure is not the primary concern; rather, she would need full **HIV treatment**. However, the immediate concern after an exposure is always prevention.
*Immediately initiate three-drug antiretroviral therapy*
- While immediate initiation of PEP is correct, it is still crucial to obtain a **baseline HIV serology** for the exposed individual.
- This baseline allows for clear documentation of the pre-exposure HIV status, which is vital for any future testing and counseling following the exposure.
*Draw her repeat HIV serology and initiate three-drug antiretroviral therapy if negative*
- Waiting for serology results to return before starting PEP is incorrect as this would significantly delay the initiation of therapy.
- The critical window for effective PEP is within hours of exposure, ideally within 72 hours.
*Perform genotype testing on source patient and initiate antiretroviral therapy tailored to results*
- While **genotype testing** on the source patient provides valuable information about drug resistance, it should not delay the immediate initiation of **empiric PEP** for the exposed individual.
- PEP must be started as soon as possible, and the regimen can be adjusted later if the genotype results indicate resistance to the initial drugs.
Acute HIV infection US Medical PG Question 10: An investigator is studying the mechanism of HIV infection in cells obtained from a human donor. The effect of a drug that impairs viral fusion and entry is being evaluated. This drug acts on a protein that is cleaved off of a larger glycosylated protein in the endoplasmic reticulum of the host cell. The protein that is affected by the drug is most likely encoded by which of the following genes?
- A. gag
- B. env (Correct Answer)
- C. tat
- D. pol
- E. rev
Acute HIV infection Explanation: ***env***
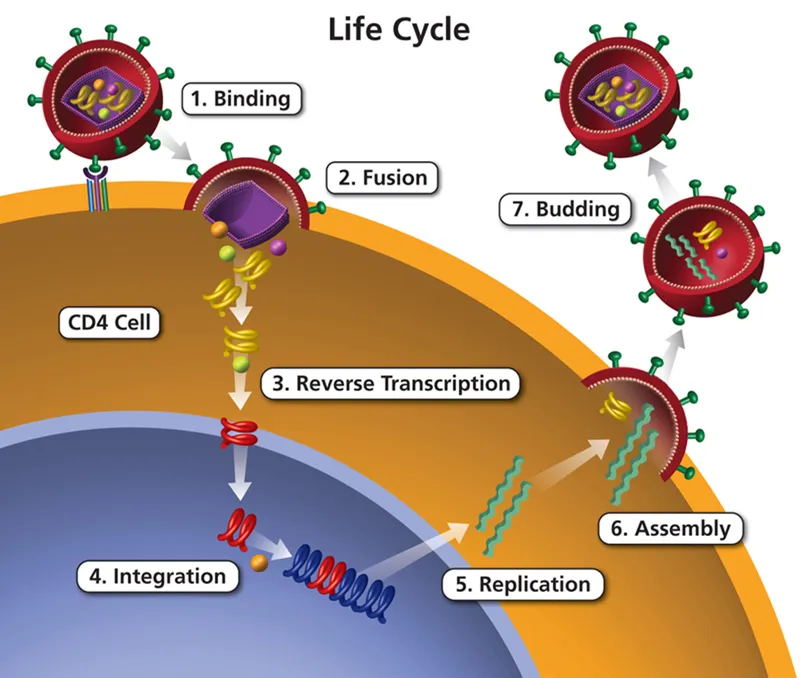
- The **env (envelope) gene** of HIV encodes for the precursor protein **gp160**, which is then cleaved by host cellular proteases into **gp120** and **gp41** within the endoplasmic reticulum.
- **gp120** and **gp41** together form the viral envelope glycoproteins responsible for viral binding to host cells and **fusion/entry**, making them the target of drugs that impair these processes.
*gag*
- The **gag (group-specific antigen) gene** encodes for structural proteins of the viral core, such as **p24 (capsid protein)**, p17 (matrix protein), and p7 (nucleocapsid protein).
- These proteins are primarily involved in the assembly of new virions and do not directly mediate viral fusion and entry.
*tat*
- The **tat (trans-activator of transcription) gene** encodes a regulatory protein that significantly enhances the transcription of viral genes.
- It plays a crucial role in the viral life cycle by increasing the efficiency of HIV gene expression, but it is not directly involved in viral fusion or entry.
*pol*
- The **pol (polymerase) gene** encodes for essential viral enzymes, including **reverse transcriptase**, integrase, and protease.
- These enzymes are critical for converting viral RNA into DNA, integrating viral DNA into the host genome, and cleaving viral polyproteins, respectively, but they are not involved in mediating viral entry.
*rev*
- The **rev (regulator of virion expression) gene** encodes a regulatory protein that facilitates the transport of unspliced and partially spliced viral RNAs from the nucleus to the cytoplasm.
- This transport is crucial for the synthesis of structural and enzymatic proteins and for packaging viral RNA into new virions, but it does not directly participate in viral fusion and entry.
More Acute HIV infection US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.