Group B streptococci US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Group B streptococci. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Group B streptococci US Medical PG Question 1: A neonate born at 33 weeks is transferred to the NICU after a complicated pregnancy and C-section. A week after being admitted, he developed a fever and became lethargic and minimally responsive to stimuli. A lumbar puncture is performed that reveals the following:
Appearance Cloudy
Protein 64 mg/dL
Glucose 22 mg/dL
Pressure 330 mm H20
Cells 295 cells/mm³ (> 90% PMN)
A specimen is sent to microbiology and reveals gram-negative rods. Which of the following is the next appropriate step in management?
- A. MRI scan of the head
- B. Start the patient on IV ceftriaxone
- C. Provide supportive measures only
- D. Start the patient on IV cefotaxime (Correct Answer)
- E. Start the patient on oral rifampin
Group B streptococci Explanation: ***Start the patient on IV cefotaxime***
- The cerebrospinal fluid (CSF) analysis with **cloudy appearance, elevated protein, low glucose, high pressure, and predominant PMNs**, coupled with **gram-negative rods** on microscopy, is highly suggestive of **bacterial meningitis** in a neonate.
- **Cefotaxime** is a third-generation cephalosporin commonly used for neonatal meningitis caused by gram-negative organisms due to its excellent CSF penetration and broad-spectrum activity, particularly against common neonatal pathogens like *E. coli* which can present as gram-negative rods.
*MRI scan of the head*
- An MRI would be considered **after initiating appropriate antibiotic treatment** to assess for complications like abscess formation or ventriculitis, not as the immediate next step in an acute, life-threatening infection.
- Delaying antibiotic treatment for imaging in acute bacterial meningitis can lead to increased morbidity and mortality.
*Start the patient on IV ceftriaxone*
- While ceftriaxone is a third-generation cephalosporin, it is **generally avoided in neonates** due to the risk of **biliary sludging** and **kernicterus**.
- Ceftriaxone competes with bilirubin for albumin binding sites, which is particularly risky in neonates who are already prone to hyperbilirubinemia.
*Provide supportive measures only*
- Given the strong evidence of **bacterial meningitis**, providing only supportive measures without specific antibiotic treatment would be inadequate and would lead to rapid deterioration and potentially fatal outcomes.
- Bacterial meningitis requires prompt and aggressive antimicrobial therapy.
*Start the patient on oral rifampin*
- **Rifampin is never used as monotherapy for bacterial meningitis** due to rapid resistance development and its primary role is in specific infections like tuberculosis or as part of combination therapy for certain resistant bacteria.
- Oral administration is also not ideal for acutely ill neonates with meningitis needing rapid, high-concentration antibiotics in the CSF.
Group B streptococci US Medical PG Question 2: A 14-year-old male is brought to the Emergency Department by his mother. She is worried because his face has become puffy and his urine has turned a tea-color. Patient history reveals the child recently suffered from a sore throat. The physician suspects a bacterial infection. Which of the following describes the likely bacteria responsible?
- A. Gram negative
- B. Bacitracin insensitive
- C. Catalase positive
- D. Beta-hemolytic (Correct Answer)
- E. Coagulase positive
Group B streptococci Explanation: ***Beta-hemolytic***
- The patient's symptoms (puffy face, tea-colored urine, recent sore throat) are classic for **post-streptococcal glomerulonephritis (PSGN)**, which is caused by a prior infection with **Group A Streptococcus (GAS)**.
- **GAS** (Streptococcus pyogenes) is known for its **beta-hemolytic** activity, meaning it completely lyses red blood cells on blood agar, creating clear zones around colonies.
*Gram negative*
- **Group A Streptococcus** (Streptococcus pyogenes) are **Gram-positive cocci**, not Gram-negative.
- Gram-negative bacteria have a different cell wall structure and typically cause different types of infections.
*Bacitracin insensitive*
- **Group A Streptococcus** (Streptococcus pyogenes) is typically **bacitracin sensitive**, meaning its growth is inhibited by bacitracin on a blood agar plate.
- This characteristic is used in laboratory settings to differentiate GAS from other beta-hemolytic streptococci.
*Catalase positive*
- **Group A Streptococcus** (Streptococcus pyogenes) is **catalase negative**, meaning it does not produce the enzyme catalase.
- **Staphylococcus species** are catalase-positive, which is a key differential test between *Staphylococcus* and *Streptococcus*.
*Coagulase positive*
- **Group A Streptococcus** (Streptococcus pyogenes) is **coagulase negative**.
- **Staphylococcus aureus** is a notable coagulase-positive bacterium, and coagulase production is a significant virulence factor for this organism, not for GAS.
Group B streptococci US Medical PG Question 3: A 27-year-old woman, gravida 2, para 1, at 37 weeks' gestation is admitted to the hospital in active labor. She has received routine prenatal care, but she has not been tested for group B streptococcal (GBS) colonization. Pregnancy and delivery of her first child were complicated by an infection with GBS that resulted in sepsis in the newborn. Current medications include folic acid and a multivitamin. Vital signs are within normal limits. The abdomen is nontender and contractions are felt every 4 minutes. There is clear amniotic fluid pooling in the vagina. The fetus is in a cephalic presentation. The fetal heart rate is 140/min. Which of the following is the most appropriate next step in management?
- A. Obtain vaginal-rectal swab for nucleic acid amplification testing
- B. Obtain vaginal-rectal swab for GBS culture
- C. Administer intrapartum intravenous penicillin (Correct Answer)
- D. Reassurance
- E. Obtain vaginal-rectal swab for GBS culture and nucleic acid amplification testing
Group B streptococci Explanation: ***Administer intrapartum intravenous penicillin***
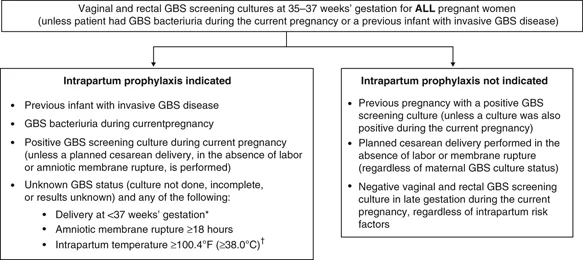
- This patient has a **previous infant with invasive GBS disease**, which is a strong indication for **intrapartum antibiotic prophylaxis (IAP)** regardless of current GBS colonization status.
- Penicillin is the **first-line agent** for GBS prophylaxis during labor to prevent vertical transmission to the newborn.
*Obtain vaginal-rectal swab for nucleic acid amplification testing*
- While **NAAT** can provide rapid results, the presence of a prior infant with invasive GBS disease is an **absolute indication** for IAP, making testing unnecessary.
- Waiting for NAAT results would **delay necessary antibiotic administration**, increasing the risk of GBS transmission.
*Obtain vaginal-rectal swab for GBS culture*
- A **GBS culture** typically takes 24-48 hours for results, which is too long given the patient is in active labor and requires immediate management.
- As with NAAT, a prior affected infant means that **IAP is indicated regardless of current culture results**.
*Reassurance*
- Reassurance alone is **insufficient** given the patient's history of a previous infant with GBS sepsis, which places her current fetus at high risk.
- **Active intervention** with antibiotics is crucial to prevent recurrence of GBS disease in the newborn.
*Obtain vaginal-rectal swab for GBS culture and nucleic acid amplification testing*
- Performing both tests is **unnecessary and delays treatment** in a patient with a clear indication for intrapartum antibiotics.
- The patient's history of a prior infant with GBS sepsis is classified as a **high-risk factor, necessitating immediate antibiotic prophylaxis** without waiting for test results.
Group B streptococci US Medical PG Question 4: A 27-year-old woman, gravida 2, para 1, at 36 weeks' gestation comes to the physician for a prenatal visit. She feels well. Fetal movements are adequate. This is her 7th prenatal visit. She had an ultrasound scan performed 1 month ago that showed a live intrauterine pregnancy consistent with a 32-week gestation with no anomalies. She had a Pap smear performed 1 year ago, which was normal. Vital signs are within normal limits. Pelvic examination shows a uterus consistent in size with a 36-week gestation. Her blood group and type is A negative. Which of the following is the most appropriate next step in management?
- A. Transabdominal doppler ultrasonography
- B. Rh antibody testing
- C. Swab for GBS culture (Correct Answer)
- D. Serum PAPP-A and HCG levels
- E. Complete blood count
Group B streptococci Explanation: ***Swab for GBS culture***
- All pregnant women should be screened for **Group B Streptococcus (GBS)** between **36 weeks 0 days and 37 weeks 6 days** of gestation.
- A positive GBS culture requires **intrapartum antibiotic prophylaxis** to prevent early-onset neonatal GBS disease.
*Transabdominal doppler ultrasonography*
- **Doppler ultrasonography** is primarily used to assess **fetal well-being** in cases of **fetal growth restriction**, preeclampsia, or other high-risk conditions.
- This patient has a **normal-sized uterus** and **adequate fetal movements**, indicating no immediate need for fetal Doppler assessment.
*Rh antibody testing*
- **Rh antibody testing** (indirect Coombs test) is performed early in pregnancy for Rh-negative women and typically repeated at **28 weeks' gestation** before anti-D immune globulin administration.
- Repeating this test at 36 weeks is not the most appropriate *next* step as the routine schedule for Rh immune globulin would typically be managed prior to this point.
*Serum PAPP-A and HCG levels*
- **Serum PAPP-A and HCG levels** are components of **first-trimester screening** for chromosomal abnormalities, performed between 11 and 14 weeks of gestation.
- At 36 weeks' gestation, these markers are not relevant for current fetal assessment.
*Complete blood count*
- A **complete blood count (CBC)** is routinely performed in the first trimester and often repeated in the **late second or early third trimester** (around 28 weeks) to check for anemia.
- While a CBC might be done as part of general prenatal care, it is not the most urgent or specifically indicated test at 36 weeks in the absence of symptoms.
Group B streptococci US Medical PG Question 5: You are treating a neonate with meningitis using ampicillin and a second antibiotic, X, that is known to cause ototoxicity. What is the mechanism of antibiotic X?
- A. It binds the 50S ribosomal subunit and inhibits formation of the initiation complex
- B. It binds the 30S ribosomal subunit and inhibits formation of the initiation complex (Correct Answer)
- C. It binds the 30S ribosomal subunit and reversibly inhibits translocation
- D. It binds the 50S ribosomal subunit and inhibits peptidyltransferase
- E. It binds the 50S ribosomal subunit and reversibly inhibits translocation
Group B streptococci Explanation: ***It binds the 30s ribosomal subunit and inhibits formation of the initiation complex***
- The second antibiotic, X, is likely an **aminoglycoside**, such as **gentamicin** or **amikacin**, which are commonly used in combination with ampicillin for neonatal meningitis and are known to cause ototoxicity.
- Aminoglycosides exert their bactericidal effect by **irreversibly binding to the 30S ribosomal subunit**, thereby **inhibiting the formation of the initiation complex** and leading to misreading of mRNA.
*It binds the 50S ribosomal subunit and inhibits formation of the initiation complex*
- This mechanism is characteristic of **linezolid**, which targets the 50S ribosomal subunit to prevent the formation of the initiation complex.
- While linezolid can cause side effects, **ototoxicity** is less commonly associated with it compared to aminoglycosides, and it is not a primary drug for neonatal meningitis alongside ampicillin.
*It binds the 50S ribosomal subunit and inhibits peptidyltransferase*
- This is the mechanism of action for **chloramphenicol**, which inhibits **peptidyltransferase** activity on the 50S ribosomal subunit, preventing peptide bond formation.
- Although chloramphenicol can cause **ototoxicity** and **aplastic anemia**, its use in neonates is limited due to the risk of **Gray Baby Syndrome**.
*It binds the 30s ribosomal subunit and reversibly inhibits translocation*
- This describes the mechanism of action of **tetracyclines**, which reversibly bind to the 30S ribosomal subunit and prevent the attachment of aminoacyl-tRNA, thereby inhibiting protein synthesis.
- Tetracyclines are **contraindicated in neonates** due to their potential to cause **tooth discoloration** and **bone growth inhibition**, and ototoxicity is not their primary adverse effect.
*It binds the 50s ribosomal subunit and reversibly inhibits translocation*
- This mechanism of reversibly inhibiting translocation by binding to the 50S ribosomal subunit is characteristic of **macrolides** (e.g., erythromycin, azithromycin) and **clindamycin**.
- While some macrolides can cause **transient ototoxicity**, they are not typically the second antibiotic of choice for neonatal meningitis in combination with ampicillin, and clindamycin's side effect profile is different.
Group B streptococci US Medical PG Question 6: A 6-month old child is brought to the ER by parents for one day of fever, decreased feeding, and lethargy. They report that neither she nor her siblings are immunized due to their concerns about vaccinations. On exam, the infant is toxic-appearing. Antibiotics are started and lumbar puncture reveals bacterial meningitis caused by a gram-negative, encapsulated organism that requires chocolate agar and the two factors shown in Image A for growth. Which organism does this best describe?
- A. Group B Streptococcus
- B. Haemophilus influenzae (Correct Answer)
- C. Moraxella catarrhalis
- D. Streptococcus pneumoniae
- E. Listeria monocytogenes
Group B streptococci Explanation: **Haemophilus influenzae**
- This organism is a **gram-negative, encapsulated coccobacillus** that requires **chocolate agar** and **factors X (hemin) and V (NAD+)** for growth, which perfectly matches the description.
- In unvaccinated children, *H. influenzae* type b (Hib) is a significant cause of **bacterial meningitis**, epiglottitis, and other invasive infections, especially considering the family's anti-vaccination stance.
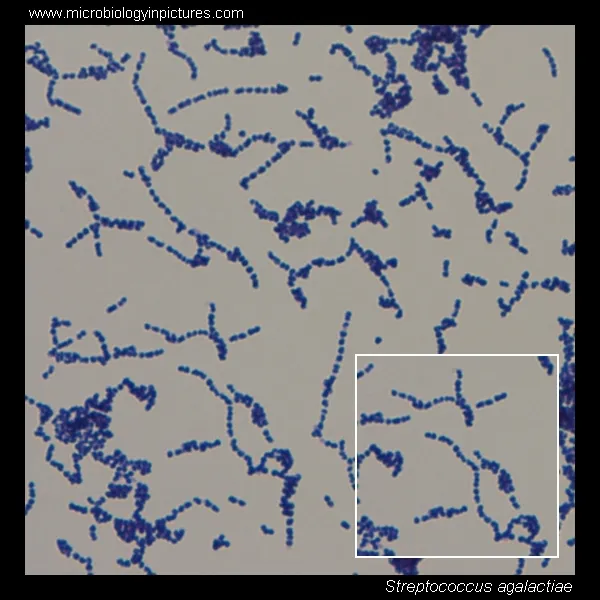
*Group B Streptococcus*
- **Group B Streptococcus (GBS)** is a **gram-positive coccus** and a common cause of early-onset neonatal sepsis and meningitis, typically in infants less than 3 months old.
- It does not require chocolate agar or specific growth factors X and V, and is **gram-positive**, not gram-negative.
*Moraxella catarrhalis*
- *Moraxella catarrhalis* is a **gram-negative diplococcus** and a common cause of otitis media, sinusitis, and bronchitis, but it is a rare cause of meningitis.
- While it is a gram-negative organism, it does not typically require chocolate agar or specific growth factors X and V for isolation, usually growing on standard blood agar.
*Streptococcus pneumoniae*
- *Streptococcus pneumoniae* is a **gram-positive coccus** that is a leading cause of bacterial meningitis in children and adults.
- It is **gram-positive**, not gram-negative, and grows on blood agar, not specifically requiring chocolate agar or factors X and V.
*Listeria monocytogenes*
- *Listeria monocytogenes* is a **gram-positive rod** and a cause of meningitis in neonates, immunocompromised individuals, and the elderly.
- It is a **gram-positive rod**, contrary to the gram-negative, encapsulated organism described, and does not require chocolate agar or factors X and V for growth.
Group B streptococci US Medical PG Question 7: A 62-year-old woman presents to the emergency department for evaluation of a spreading skin infection that began from an ulcer on her foot. The patient has type 2 diabetes mellitus that is poorly controlled. On examination, there is redness and erythema to the lower limb with skin breakdown along an extensive portion of the leg. The patient’s tissues separate readily from the fascial plane, prompting a diagnosis of necrotizing fasciitis. What is the exotoxin most likely associated with this patient’s presentation?
- A. Streptococcal pyogenic exotoxin A
- B. TSST-1
- C. Diphtheria toxin
- D. Exfoliative toxin
- E. Streptococcal pyogenic exotoxin B (Correct Answer)
Group B streptococci Explanation: ***Streptococcal pyogenic exotoxin B***
- **Streptococcal pyogenic exotoxin B** is a **cysteine protease** that directly degrades tissue, including collagen and fibronectin, leading to the rapid tissue destruction characteristic of **necrotizing fasciitis**.
- This exotoxin is frequently associated with **Group A Streptococcus (GAS)** infections, a common cause of severe soft tissue infections, especially in immunocompromised individuals like diabetics.
*Streptococcal pyogenic exotoxin A*
- This exotoxin acts as a **superantigen**, primarily causing symptoms of **streptococcal toxic shock syndrome** (STSS), characterized by fever, rash, and organ failure.
- While GAS can cause necrotizing fasciitis, Exotoxin A is more closely linked to toxic shock phenomena rather than direct tissue destruction.
*TSST-1*
- **Toxic Shock Syndrome Toxin-1 (TSST-1)** is produced by **Staphylococcus aureus** and is a classic cause of **staphylococcal toxic shock syndrome**.
- It acts as a **superantigen** but is not directly responsible for the extensive tissue necrosis seen in necrotizing fasciitis caused by streptococci.
*Diphtheria toxin*
- **Diphtheria toxin**, produced by *Corynebacterium diphtheriae*, inhibits **protein synthesis** by inactivating elongation factor-2 (EF-2), leading to cell death.
- It causes diphtheria, characterized by a **pseudomembrane** in the throat and myocarditis, not necrotizing fasciitis.
*Exfoliative toxin*
- **Exfoliative toxins A and B** are produced by **Staphylococcus aureus** and are responsible for **Staphylococcal Scalded Skin Syndrome (SSSS)**.
- These toxins cause cleavage of desmoglein-1 in the epidermis, leading to widespread blistering and desquamation, not deep tissue necrosis.
Group B streptococci US Medical PG Question 8: A person presents to the hospital with fever and chills. Fever profile is ordered and is found to be negative for malaria and dengue. Rk39 test is found to be positive. What is the treatment of choice?
- A. Amphotericin B (Correct Answer)
- B. Dapsone
- C. Hydroxychloroquine
- D. Griseofulvin
Group B streptococci Explanation: Amphotericin B
- A positive RK39 test suggests visceral leishmaniasis (kala-azar), especially with fever and chills in an endemic area [1].
- Amphotericin B (specifically liposomal Amphotericin B) is a highly effective and often the drug of choice for treating visceral leishmaniasis, particularly in severe cases or regions with antimonial resistance.
Dapsone
- Dapsone is primarily used in the treatment of leprosy and بعض forms of dermatitis (e.g., dermatitis herpetiformis).
- It has no significant role in treating leishmaniasis.
Hydroxychloroquine
- Hydroxychloroquine is an antimalarial drug also used for certain autoimmune diseases like lupus and rheumatoid arthritis [2].
- It is ineffective against leishmaniasis.
Griseofulvin
- Griseofulvin is an antifungal medication used to treat dermatophyte infections (e.g., ringworm of the skin, hair, or nails).
- It has no activity against Leishmania parasites.
Group B streptococci US Medical PG Question 9: A 32-year-old man comes to the physician with difficulty swallowing for several weeks. Examination of the oropharynx shows lesions on palate and tongue that can be easily scraped off. An image of the lesions is shown. Which of the following is a risk factor for this patient's findings?
- A. Inhalation of salbutamol
- B. Decline in CD4+ T-cells (Correct Answer)
- C. Chronic nicotine abuse
- D. Epstein-Barr virus infection
- E. Missed childhood vaccination
Group B streptococci Explanation: ***Decline in CD4+ T-cells***
- The patient's symptoms (difficulty swallowing, white lesions on the palate and tongue that can be scraped off), along with the images, are highly suggestive of **oral candidiasis (thrush)**.
- A significant decline in **CD4+ T-cells**, often seen in conditions like **HIV/AIDS**, severely compromises the immune system and is a major risk factor for opportunistic infections like oral candidiasis.
*Inhalation of salbutamol*
- Inhaled corticosteroids, not bronchodilators like salbutamol, are known to increase the risk of oral candidiasis by altering the oral flora and suppressing local immunity.
- While prolonged use of any inhaler without rinsing can contribute to oral issues, salbutamol itself is not a direct risk factor for candidiasis.
*Chronic nicotine abuse*
- **Chronic nicotine abuse** (smoking) is associated with conditions like **leukoplakia**, erythroplakia, and an increased risk of oral cancer, but it is not a direct risk factor for oral candidiasis.
- **Leukoplakia** lesions, unlike candidiasis, are typically **non-scrapable**.
*Epstein-Barr virus infection*
- **Epstein-Barr virus (EBV)** is primarily associated with **oral hairy leukoplakia** in immunocompromised individuals.
- **Oral hairy leukoplakia** presents as white, corrugated, and **non-scrapable lesions**, typically on the lateral borders of the tongue, which differs from the described findings.
*Missed childhood vaccination*
- **Missed childhood vaccinations** increase the risk of common pediatric infectious diseases like measles, mumps, and rubella.
- There is **no direct link** between missed routine childhood vaccinations and the development of oral candidiasis in adulthood.
Group B streptococci US Medical PG Question 10: A 24-hour-old newborn presents to the emergency department after a home birth because of fever, irritability alternating with lethargy, and poor feeding. The patient’s mother says symptoms acutely onset 12 hours ago and have not improved. No significant past medical history. His mother did not receive any prenatal care, and she had rupture of membranes 20 hours prior to delivery. His vital signs include: heart rate 150/min, respiratory rate 65/min, temperature 39.0°C (102.2°F), and blood pressure 60/40 mm Hg. On physical examination, the patient has delayed capillary refill. Laboratory studies show a pleocytosis and a low glucose level in the patient’s cerebrospinal fluid. Which of the following is the most likely causative organism for this patient’s condition?
- A. Group A Streptococcus
- B. Enterovirus
- C. Group B Streptococcus (Correct Answer)
- D. Streptococcus pneumoniae
- E. Cryptococcus neoformans
Group B streptococci Explanation: ***Group B Streptococcus***
- This newborn presents with **fever, irritability/lethargy, poor feeding**, and signs of **sepsis (tachycardia, tachypnea, hypotension, delayed capillary refill)**, along with **abnormal CSF (pleocytosis, low glucose)**, indicating **neonatal meningitis**.
- **Group B Streptococcus (GBS)** is the **most common cause of early-onset neonatal sepsis and meningitis**, especially with risk factors such as **lack of prenatal care** and **prolonged rupture of membranes (>18 hours)**, as seen in this case.
*Group A Streptococcus*
- While Group A Streptococcus can cause severe infections, it is an **uncommon cause of neonatal sepsis and meningitis** compared to GBS.
- More typically associated with **pharyngitis, impetigo, and necrotizing fasciitis** in older children and adults.
*Enterovirus*
- Enteroviruses are a common cause of **viral meningitis in neonates and infants**, but typically present with a **lymphocytic pleocytosis** and **normal CSF glucose**, in contrast to the features (pleocytosis, low glucose) seen here.
- While fever and irritability can be present, the CSF findings point more towards a bacterial infection.
*Streptococcus pneumoniae*
- *Streptococcus pneumoniae* can cause bacterial meningitis but is **less common in the immediate neonatal period** (first 7 days of life) compared to GBS.
- Risk factors often include **preterm birth** or **underlying immune deficiencies**, which are not specified here.
*Cryptococcus neoformans*
- *Cryptococcus neoformans* is an **opportunistic fungal pathogen** that typically causes meningitis in **immunocompromised individuals**, such as those with HIV/AIDS.
- It is **extremely rare** in immunocompetent newborns and would not be the most likely cause in this clinical scenario.
More Group B streptococci US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.