Group A streptococci US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Group A streptococci. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Group A streptococci US Medical PG Question 1: A 7-year-old boy is brought to the physician because of a 5-day history of fever, malaise, and joint pain. He had a sore throat 4 weeks ago that resolved without treatment. His temperature is 38.6°C (101.5°F) and blood pressure is 84/62 mm Hg. Physical examination shows several firm, painless nodules under the skin near his elbows and the dorsal aspect of both wrists. Cardiopulmonary examination shows bilateral basilar crackles and a blowing, holosystolic murmur heard best at the cardiac apex. Both knee joints are warm. Laboratory studies show an erythrocyte sedimentation rate of 129 mm/h. The immune response seen in this patient is most likely due to the presence of which of the following?
- A. M protein (Correct Answer)
- B. CAMP factor
- C. TSST-1
- D. IgA protease
- E. Hyaluronic acid capsule
Group A streptococci Explanation: ***M protein***
- The constellation of symptoms (recent sore throat, fever, joint pain, subcutaneous nodules, and a new heart murmur) is highly suggestive of **acute rheumatic fever (ARF)**, which is triggered by a preceding infection with **Group A Streptococcus (GAS)**.
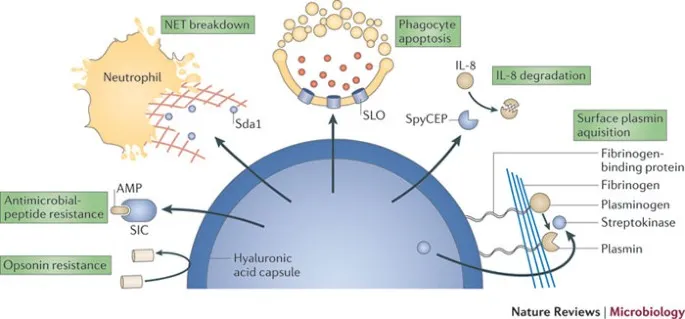
- The **M protein** is a major virulence factor of GAS that elicits a strong immune response, and antibodies directed against it can cross-react with host tissues (molecular mimicry), leading to the inflammatory damage seen in ARF.
*CAMP factor*
- **CAMP factor** is a virulence factor produced by *Streptococcus agalactiae* (Group B Streptococcus), not Group A Streptococcus, which is responsible for ARF.
- Group B Streptococcus is primarily associated with neonatal infections and does not cause rheumatic fever.
*TSST-1*
- **Toxic Shock Syndrome Toxin-1 (TSST-1)** is a superantigen produced by *Staphylococcus aureus* and is responsible for **toxic shock syndrome**, not acute rheumatic fever.
- Toxic shock syndrome presents with abrupt onset of fever, hypotension, diffuse rash, and multi-organ dysfunction, which differs from the patient's presentation.
*IgA protease*
- **IgA protease** is an enzyme produced by several bacterial species, including *Neisseria meningitidis*, *Haemophilus influenzae*, and *Streptococcus pneumoniae*, that cleaves IgA antibodies.
- While it contributes to bacterial colonization of mucous membranes, it is not the primary virulence factor responsible for the immune response leading to acute rheumatic fever.
*Hyaluronic acid capsule*
- The **hyaluronic acid capsule** of *Streptococcus pyogenes* (GAS) is a virulence factor that helps in evading phagocytosis by mimicking host connective tissue.
- While it prevents immune detection and aids in colonization, it does not directly elicit the cross-reactive immune response responsible for the tissue damage in acute rheumatic fever; that role is attributed primarily to the M protein.
Group A streptococci US Medical PG Question 2: Physical exam of a 15-year-old female reveals impetigo around her mouth. A sample of the pus is taken and cultured. Growth reveals gram-positive cocci in chains that are bacitracin sensitive. Which of the following symptoms would be concerning for a serious sequela of this skin infection?
- A. Myocarditis
- B. Joint swelling
- C. Fever
- D. Chorea
- E. Hematuria (Correct Answer)
Group A streptococci Explanation: ***Hematuria***
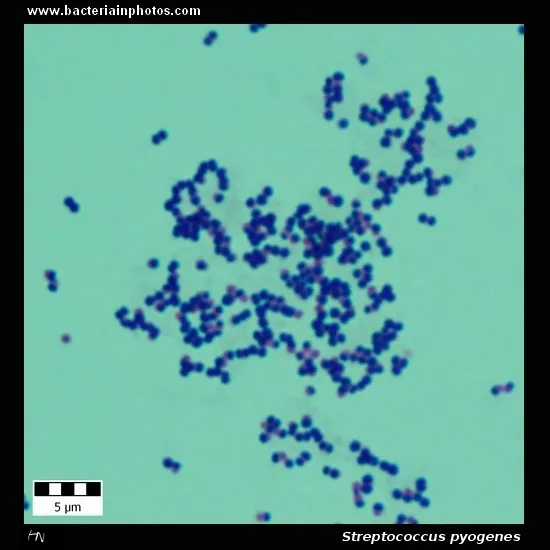
- The description of **impetigo** around the mouth caused by **gram-positive cocci in chains** that are **bacitracin-sensitive** points to *Streptococcus pyogenes* (Group A Streptococcus).
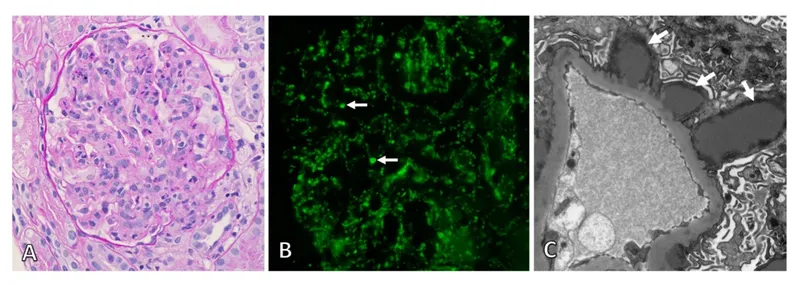
- A serious sequela of streptococcal skin infections (impetigo) is **post-streptococcal glomerulonephritis (PSGN)**, which presents with **hematuria**, proteinuria, edema, and hypertension.
*Myocarditis*
- **Myocarditis** can be a complication of **acute rheumatic fever (ARF)**, which is a sequela of **streptococcal pharyngitis**, not typically streptococcal skin infections (impetigo).
- While both rheumatic fever and PSGN are caused by *Streptococcus pyogenes*, the specific **M-types** associated with skin infections differ from those causing pharyngitis and ARF.
*Joint swelling*
- **Arthritis** (joint swelling) is a major criterion for **acute rheumatic fever**, which follows **streptococcal pharyngitis**, not impetigo.
- Although PSGN can cause arthralgia, significant arthritis is not a primary or alarming symptom of PSGN.
*Fever*
- **Fever** is a general symptom that can accompany any infection, including impetigo itself or many other conditions.
- While fever can be present in PSGN, it is not a specific or unique indicator of this particular serious sequela.
*Chorea*
- **Sydenham's chorea** is a neurological manifestation of **acute rheumatic fever**, which develops after **streptococcal pharyngitis**, not impetigo.
- It presents as involuntary, purposeless movements and is not associated with PSGN following impetigo.
Group A streptococci US Medical PG Question 3: A 15-year-old boy is brought to the office by his mother with complaints of facial puffiness and smoky urine. The mother noticed puffiness on her son’s face a week ago, and it has been progressively worsening since then. She also states that her son had a sore throat 3 weeks ago. The patient does not have fever/chills, changes in urinary frequency, or abdominal discomfort. On physical examination, facial edema is noted. The vital signs include: blood pressure 145/85 mm Hg, pulse 96/min, temperature 36.7°C (98.1°F), and respiratory rate 20/min.
A complete blood count report shows:
Hemoglobin 10.1 g/dL
RBC 4.9 million cells/µL
Hematocrit 46%
Total leukocyte count 6,800 cells/µL
Neutrophils 70%
Lymphocytes 26%
Monocytes 3%
Eosinophil 1%
Basophils 0%
Platelets 210,000 cells/µL
ESR 18 mm (1st hour)
Urinalysis shows:
pH 6.4
Color dark brown
RBC plenty
WBC 3–4/HPF
Protein absent
Cast RBC and granular casts
Glucose absent
Crystal none
Ketone absent
Nitrite absent
Which of the following laboratory findings can be expected in this patient?
- A. Increased C3 level
- B. Positive streptozyme test (Correct Answer)
- C. Normal erythrocyte sedimentation rate
- D. Decreased serum creatinine
- E. Negative antistreptolysin O (ASO) titer
Group A streptococci Explanation: ***Positive streptozyme test***
- The clinical presentation of **facial puffiness**, **smoky urine**, and a history of a **sore throat 3 weeks prior** are highly suggestive of **post-streptococcal glomerulonephritis (PSGN)**.
- A **streptozyme test** detects antibodies to several streptococcal antigens (streptolysin O, hyaluronidase, streptokinase, DNase B, and NADase), making it a comprehensive and sensitive indicator of recent streptococcal infection.
*Increased C3 level*
- In **PSGN**, activation of the complement system by immune complexes typically leads to a **reduction in C3 levels**, not an increase.
- While C3 levels usually return to normal within 6-8 weeks, acutely they would be depressed.
*Normal erythrocyte sedimentation rate*
- The given ESR of **18 mm** is slightly elevated for a healthy child (normal range typically <15 mm/hr for this age group), indicating an ongoing inflammatory process.
- In conditions like PSGN, inflammation of the glomeruli would likely cause an **elevated ESR**.
*Decreased serum creatinine*
- The patient's blood pressure of **145/85 mm Hg** and the active urinary findings (RBC casts, granular casts) point towards **acute kidney injury** or **renal impairment**.
- This would lead to an **increased serum creatinine**, reflecting reduced glomerular filtration, rather than a decrease.
*Negative antistreptolysin O (ASO) titer*
- A **recent streptococcal infection** is the precursor to PSGN, and an **elevated ASO titer** is one of the key laboratory findings supporting this diagnosis.
- A negative ASO titer would argue against the diagnosis of PSGN, although other streptococcal antibodies (detected by a streptozyme test) can still be positive.
Group A streptococci US Medical PG Question 4: A previously healthy 17-year-old boy is brought to the emergency department because of fever, nausea, and myalgia for the past day. His temperature is 39.5°C (103.1°F), pulse is 112/min, and blood pressure is 77/55 mm Hg. Physical examination shows scattered petechiae over the anterior chest and abdomen. Blood culture grows an organism on Thayer-Martin agar. Which of the following virulence factors of the causal organism is most likely responsible for the high mortality rate associated with it?
- A. Immunoglobulin A protease
- B. Lipooligosaccharide (Correct Answer)
- C. Toxic shock syndrome toxin-1
- D. Lipoteichoic acid
- E. Erythrogenic exotoxin A
Group A streptococci Explanation: ***Lipooligosaccharide***
- The patient's presentation with **fever**, **hypotension**, and **petechiae**, along with a positive blood culture on Thayer-Martin agar, points to **meningococcemia** caused by *Neisseria meningitidis*.
- **Lipooligosaccharide (LOS)** acts as an **endotoxin**, triggering an excessive inflammatory response that leads to widespread vascular damage, **capillary leakage**, and **septic shock**, accounting for the high mortality.
*Immunoglobulin A protease*
- While *N. meningitidis* produces **IgA protease** to cleave secretory IgA and evade host defenses on mucosal surfaces, this factor is primarily involved in colonization and initial invasion rather than the systemic severity and mortality of septic shock.
- Its role is to help the bacteria **adhere and penetrate** host mucous membranes, but it does not directly cause the shock and petechiae seen in this severe presentation.
*Toxic shock syndrome toxin-1*
- **Toxic shock syndrome toxin-1 (TSST-1)** is a **superantigen** produced by *Staphylococcus aureus* that causes **toxic shock syndrome**, which can present with fever, rash, and hypotension.
- However, the organism grown on **Thayer-Martin agar** is characteristic of *Neisseria meningitidis*, not *Staphylococcus aureus*.
*Lipoteichoic acid*
- **Lipoteichoic acid** is a major component of the cell wall of **Gram-positive bacteria**, acting as a potent proinflammatory molecule and contributing to septic shock in those infections.
- *Neisseria meningitidis* is a **Gram-negative bacterium**, and therefore does not possess lipoteichoic acid.
*Erythrogenic exotoxin A*
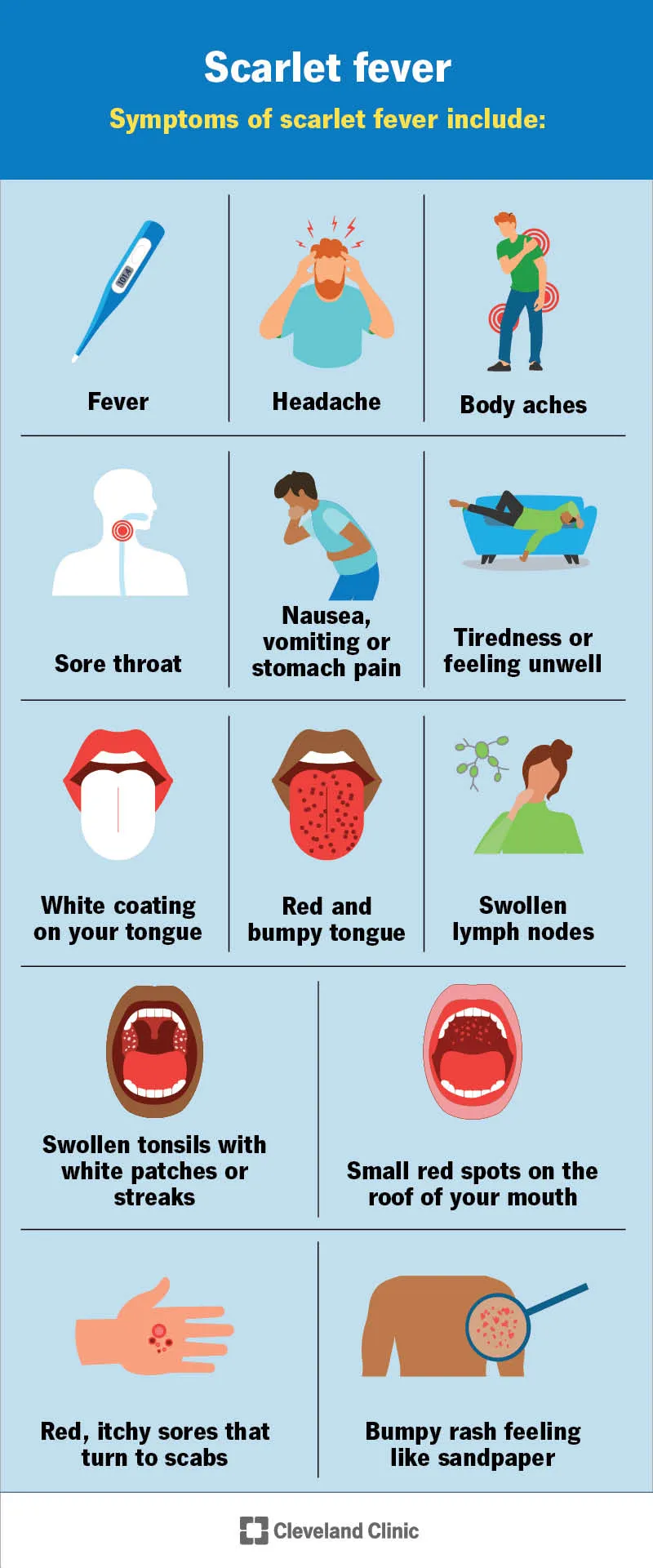
- **Erythrogenic exotoxin A** is primarily produced by ***Streptococcus pyogenes*** and is responsible for the characteristic rash of **scarlet fever**.
- While *S. pyogenes* can cause invasive infections, the clinical picture and the specific growth on **Thayer-Martin agar** are not consistent with streptococcal infection.
Group A streptococci US Medical PG Question 5: An 11-year-old boy presents with fever and joint pain for the last 3 days. His mother says that he had a sore throat 3 weeks ago but did not seek medical care at that time. The family immigrated from the Middle East 3 years ago. The patient has no past medical history. The current illness started with a fever and a swollen right knee that was very painful. The following day, his knee improved but his left elbow became swollen and painful. While in the waiting room, his left knee is also becoming swollen and painful. Vital signs include: temperature 38.7°C (101.6°F), and blood pressure 110/80 mm Hg. On physical examination, the affected joints are swollen and very tender to touch, and there are circular areas of redness on his back and left forearm (as shown in the image). Which of the following is needed to establish a diagnosis of acute rheumatic fever in this patient?
- A. Elevated erythrocyte sedimentation rate (ESR)
- B. Positive anti-streptococcal serology (Correct Answer)
- C. Elevated leukocyte count
- D. No other criterion is needed to establish the diagnosis of acute rheumatic fever
- E. Prolonged PR interval
Group A streptococci Explanation: ***Positive anti-streptococcal serology***
- A positive anti-streptococcal serology (e.g., elevated ASO titer or anti-DNase B) is a mandatory component for diagnosing **acute rheumatic fever** (ARF) when using the updated Jones criteria, as it confirms a preceding Group A Streptococcal infection.
- Given the history of a recent **sore throat** and clinical manifestations suggestive of ARF (migratory polyarthritis, fever, erythema marginatum), confirmation of a preceding streptococcal infection is crucial.
*Elevated erythrocyte sedimentation rate (ESR)*
- An elevated **ESR** is one of the **minor criteria** for ARF and indicates general inflammation, but it is not sufficient on its own to confirm the diagnosis.
- While supportive of an inflammatory process, it does not confirm the specific etiology of ARF, which requires evidence of a recent **streptococcal infection**.
*Elevated leukocyte count*
- An elevated **leukocyte count** (leukocytosis) is a non-specific indicator of inflammation or infection and is also considered a **minor criterion** for ARF.
- It does not definitively point to ARF or a preceding streptococcal infection and thus cannot solely establish the diagnosis.
*No other criterion is needed to establish the diagnosis of acute rheumatic fever*
- This statement is incorrect because the diagnosis of ARF requires fulfilling specific Jones criteria, which include evidence of a preceding **Group A Streptococcal infection** along with major and/or minor clinical manifestations.
- While the patient exhibits several major criteria (migratory polyarthritis, erythema marginatum), the diagnosis is incomplete without confirming the **streptococcal trigger**.
*Prolonged PR interval*
- A **prolonged PR interval** on an ECG is a sign of **carditis**, which is a **major criterion** for ARF.
- Although carditis can be a significant manifestation, it is not always present in every case and does not replace the requirement for evidence of a preceding **streptococcal infection** for diagnosis.
Group A streptococci US Medical PG Question 6: A 63-year-old man with aortic valve disease is admitted to the hospital for a 3-week history of progressively worsening fatigue, fever, and night sweats. He does not smoke, drink alcohol, or use illicit drugs. Temperature is 38.2°C (100.8°F). Physical examination shows a systolic murmur and tender, erythematous nodules on the finger pads. Blood cultures show alpha-hemolytic, gram-positive cocci that are catalase-negative and optochin-resistant. Which of the following is the most likely causal organism?
- A. Streptococcus pneumoniae
- B. Staphylococcus epidermidis
- C. Viridans streptococci (Correct Answer)
- D. Streptococcus pyogenes
- E. Streptococcus gallolyticus
Group A streptococci Explanation: ***Viridans streptococci***
- The patient's presentation with **subacute onset** of fever, fatigue, cardiac murmur, and **Osler nodes** (tender finger nodules) points to **infective endocarditis**. The micro-organism is described as **alpha-hemolytic**, **catalase-negative**, and **optochin-resistant**, which are characteristic features of **Viridans streptococci**.
- **Viridans streptococci** are a common cause of **subacute bacterial endocarditis**, especially in patients with pre-existing valvular disease like the **aortic valve disease** mentioned.
*Streptococcus pneumoniae*
- While **Streptococcus pneumoniae** is also **alpha-hemolytic** and **catalase-negative**, it is typically **optochin-sensitive** and a common cause of **pneumonia** and **meningitis**, not usually subacute endocarditis from oral flora.
- Endocarditis caused by *S. pneumoniae* is rare and usually associated with a more fulminant course.
*Staphylococcus epidermidis*
- **Staphylococcus epidermidis** is a **coagulase-negative staphylococcus** that is a common cause of **prosthetic valve endocarditis** and is **catalase-positive**, unlike the organism described here.
- It is not typically alpha-hemolytic.
*Streptococcus pyogenes*
- **Streptococcus pyogenes** is **beta-hemolytic** and **catalase-negative**, and typically causes **pharyngitis** and **skin infections**, or sometimes **acute endocarditis**.
- It does not fit the description of an **alpha-hemolytic**, **optochin-resistant** organism.
*Streptococcus gallolyticus*
- **Streptococcus gallolyticus** (formerly *Streptococcus bovis*) is associated with **bacteremia** and **endocarditis**, particularly in patients with **gastrointestinal malignancies**.
- While it is **alpha-hemolytic** and **catalase-negative**, it is typically differentiated by its growth in **bile esculin** and is not primarily defined by optochin resistance characteristic of Viridans group.
Group A streptococci US Medical PG Question 7: A 27-year-old woman comes to the physician because of a 3-day history of a sore throat and fever. Her temperature is 38.5°C (101.3°F). Examination shows edematous oropharyngeal mucosa and enlarged tonsils with purulent exudate. There is tender cervical lymphadenopathy. If left untreated, which of the following conditions is most likely to occur in this patient?
- A. Rheumatic fever (Correct Answer)
- B. Rheumatoid arthritis
- C. Erythema multiforme
- D. Toxic shock syndrome
- E. Post-streptococcal glomerulonephritis
Group A streptococci Explanation: ***Rheumatic fever***
- The patient presents with classic symptoms of **streptococcal pharyngitis** (sore throat, fever, tonsillar exudate, tender cervical lymphadenopathy), which, if left untreated, is a major risk factor for developing **acute rheumatic fever**.
- **Acute rheumatic fever** is a serious inflammatory disease that can affect the **heart valves**, joints, brain, and skin, occurring in approximately **3% of untreated cases** of Group A Streptococcal pharyngitis.
*Rheumatoid arthritis*
- This is a **chronic autoimmune inflammatory disease** primarily affecting the synovial joints, not typically associated with an acute streptococcal infection.
- It involves a different pathophysiological mechanism and is not a direct complication of untreated streptococcal pharyngitis.
*Erythema multiforme*
- This is an **acute, self-limiting skin condition** often triggered by infections (e.g., Herpes simplex virus) or medications, resulting in target lesions.
- While infections can cause it, **streptococcal pharyngitis** is not a common or direct cause, and it's not a systemic complication similar to rheumatic fever.
*Toxic shock syndrome*
- This is a **rapidly progressing infectious disease** characterized by fever, rash, hypotension, and multi-organ failure, most often caused by toxins produced by *Staphylococcus aureus* or *Streptococcus pyogenes*.
- While *Streptococcus pyogenes* (Group A Strep) can cause it, toxic shock syndrome is an **acute complication** rather than a late sequela of untreated infection, making **rheumatic fever** the more characteristic delayed complication.
*Post-streptococcal glomerulonephritis*
- While this is another serious immune-mediated complication of **streptococcal infections**, it **more commonly follows skin infections (impetigo)** than pharyngitis.
- **Rheumatic fever** is the most characteristic and clinically significant late complication of untreated streptococcal **pharyngitis** specifically, with greater emphasis in clinical practice due to its potential for permanent cardiac valve damage.
Group A streptococci US Medical PG Question 8: A 5-year-old boy presents to your office with his mother. The boy has been complaining of a sore throat and headache for the past 2 days. His mother states that he had a fever of 39.3°C (102.7°F) and had difficulty eating. On examination, the patient has cervical lymphadenopathy and erythematous tonsils with exudates. A streptococcal rapid antigen detection test is negative. Which of the following is the most likely causative agent?
- A. A gram-negative, pleomorphic, obligate intracellular bacteria
- B. An enveloped, single-stranded, negative sense RNA virus
- C. A gram-positive, beta-hemolytic cocci in chains
- D. An enveloped, double-stranded DNA virus (Correct Answer)
- E. A naked, double-stranded DNA virus
Group A streptococci Explanation: ***An enveloped, double-stranded DNA virus***
- This description refers to **Epstein-Barr virus (EBV)**, which is a common cause of **infectious mononucleosis** in children and adolescents.
- Symptoms like **sore throat**, **fever**, **fatigue**, **cervical lymphadenopathy**, and **erythematous tonsils with exudates** are classic for mononucleosis; a negative strep test helps rule out bacterial pharyngitis.
*A gram-negative, pleomorphic, obligate intracellular bacteria*
- This describes organisms like **Chlamydia** or **Rickettsia**, which typically cause different sets of symptoms, such as sexually transmitted infections or tick-borne diseases.
- These are **not common causes of pharyngitis** with exudates and cervical lymphadenopathy in children.
*An enveloped, single-stranded, negative sense RNA virus*
- This describes viruses such as **influenza virus** or **respiratory syncytial virus (RSV)**.
- While these can cause pharyngitis, the overall clinical picture, particularly the prominent **lymphadenopathy** and **exudative tonsillitis** in the presence of a negative strep test, is less typical for these viruses compared to EBV.
*A gram-positive, beta-hemolytic cocci in chains*
- This describes **Group A Streptococcus (GAS)**, which is the causative agent of **streptococcal pharyngitis (strep throat)**.
- Although the symptoms are consistent with strep throat, the information states that the **rapid antigen detection test for streptococcus was negative**, making this diagnosis highly unlikely.
*A naked, double-stranded DNA virus*
- This describes viruses such as **adenoviruses** or **human papillomaviruses**.
- While adenoviruses can cause pharyngitis, the detailed clinical presentation of **prominent exudative tonsillitis** and **cervical lymphadenopathy** in the context of a negative strep test points more strongly to infectious mononucleosis caused by EBV.
Group A streptococci US Medical PG Question 9: A 16-year-old male is brought to the clinic by his mother for the complaints of fever, nonproductive cough, fatigue, lack of appetite, and sore throat for the past 2 months. Several other students at his high school have had similar symptoms. Physical exam shows a whitish membrane in his oropharynx, bilateral enlarged cervical lymphadenopathy, and mild splenomegaly. Which of the following tests is most likely to diagnose his condition?
- A. Monospot test (Correct Answer)
- B. Enzyme-linked immunosorbent assay
- C. Throat culture
- D. Urine culture
- E. Chest X-ray
Group A streptococci Explanation: ***Monospot test***
- The Monospot test detects **heterophile antibodies**, which are commonly produced during an acute Epstein-Barr virus (EBV) infection, the cause of **infectious mononucleosis**.
- The patient's symptoms (fever, fatigue, nonproductive cough, sore throat, cervical lymphadenopathy, splenomegaly) and the epidemiological context (several other students with similar symptoms) are highly suggestive of **infectious mononucleosis**.
*Enzyme-linked immunosorbent assay (ELISA)*
- While ELISA can detect antibodies to various pathogens, including EBV-specific antigens, the **Monospot test** is the more common and rapid initial diagnostic tool for infectious mononucleosis.
- ELISA for EBV-specific antibodies (e.g., VCA-IgM, VCA-IgG) might be used if the Monospot test is negative but clinical suspicion remains high, especially in younger children or atypical presentations.
*Throat culture*
- A throat culture is used to identify bacterial infections, such as **Streptococcus pyogenes** (strep throat).
- Although the patient has a sore throat and a whitish membrane, his other systemic symptoms (fatigue, splenomegaly, lack of appetite for 2 months) are not typical for a bacterial pharyngitis which usually responds to antibiotics. A **nonproductive cough** also makes bacterial pharyngitis less likely.
*Urine culture*
- A urine culture is used to diagnose **urinary tract infections**.
- The patient's symptoms are not indicative of a urinary tract infection.
*Chest X-ray*
- A chest X-ray is used to evaluate the lungs for conditions such as **pneumonia**, **bronchitis**, or other respiratory pathologies.
- While the patient has a nonproductive cough, the predominant systemic symptoms (fever, fatigue, lymphadenopathy, splenomegaly) point towards a systemic viral infection rather than primarily a lung issue that would be definitively diagnosed by a chest X-ray.
Group A streptococci US Medical PG Question 10: A 54-year-old woman comes to the physician because of lower back pain, night sweats, and a 5-kg (11-lb) weight loss during the past 4 weeks. She has rheumatoid arthritis treated with adalimumab. Her temperature is 38°C (100.4°F). Physical examination shows tenderness over the T10 and L1 spinous processes. Passive extension of the right hip causes pain in the right lower quadrant. The patient's symptoms are most likely caused by an organism with which of the following virulence factors?
- A. Proteins that bind to the Fc region of immunoglobulin G
- B. Protease that cleaves immunoglobulin A
- C. Polysaccharide capsule that prevents phagocytosis
- D. Surface glycolipids that prevent phagolysosome fusion (Correct Answer)
- E. Polypeptides that inactivate elongation factor 2
Group A streptococci Explanation: ***Surface glycolipids that prevent phagolysosome fusion***
- The patient's symptoms (low back pain, night sweats, weight loss, fever, spinal tenderness, and hip pain) in a patient on **adalimumab** (a TNF-alpha inhibitor) suggest **disseminated tuberculosis** (Pott disease).
- *Mycobacterium tuberculosis* uses **mycolic acids** and other surface glycolipids to prevent phagolysosome fusion, allowing it to survive and replicate within macrophages.
*Proteins that bind to the Fc region of immunoglobulin G*
- This virulence factor is characteristic of bacteria like *Staphylococcus aureus* (Protein A) and *Streptococcus pyogenes* (Protein G), which is not consistent with the clinical picture.
- These proteins interfere with opsonization and antibody-mediated immunity, but are not the primary mechanism of *Mycobacterium tuberculosis* survival within macrophages.
*Protease that cleaves immunoglobulin A*
- **IgA protease** is a virulence factor for bacteria such as *Neisseria gonorrhoeae*, *Neisseria meningitidis*, and *Streptococcus pneumoniae*, which colonize mucosal surfaces.
- This mechanism helps these bacteria evade mucosal immunity, but it is not relevant to the pathogenesis of tuberculosis.
*Polysaccharide capsule that prevents phagocytosis*
- A polysaccharide capsule is a major virulence factor for many encapsulated bacteria (e.g., *Streptococcus pneumoniae*, *Haemophilus influenzae*, *Neisseria meningitidis*) that helps them evade phagocytosis.
- However, *Mycobacterium tuberculosis* is not primarily characterized by a polysaccharide capsule for immune evasion; its internal survival within macrophages is more critical.
*Polypeptides that inactivate elongation factor 2*
- Toxins that inactivate **elongation factor 2** are associated with *Corynebacterium diphtheriae* (**diphtheria toxin**) and *Pseudomonas aeruginosa* (**exotoxin A**), leading to inhibition of protein synthesis.
- This mechanism is not involved in the pathogenesis of *Mycobacterium tuberculosis* infection or its ability to cause disseminated disease.
More Group A streptococci US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.