Enterococci US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Enterococci. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Enterococci US Medical PG Question 1: A 37-year-old woman with a history of anorectal abscesses complains of pain in the perianal region. Physical examination reveals mild swelling, tenderness, and erythema of the perianal skin. She is prescribed oral ampicillin and asked to return for follow-up. Two days later, the patient presents with a high-grade fever, syncope, and increased swelling. Which of the following would be the most common mechanism of resistance leading to the failure of antibiotic therapy in this patient?
- A. Intrinsic absence of a target site for the drug
- B. Use of an altered metabolic pathway
- C. Production of beta-lactamase enzyme (Correct Answer)
- D. Altered structural target for the drug
- E. Drug efflux pump
Enterococci Explanation: ***Production of beta-lactamase enzyme***
- The patient's symptoms of a rapidly worsening infection despite ampicillin treatment suggest the presence of a **beta-lactamase producing organism**. Ampicillin is a **beta-lactam antibiotic** that is inactivated by these enzymes.
- Anorectal abscesses and rapidly progressing soft tissue infections are often caused by **polymicrobial flora**, including staphylococci and enterococci, many of which can produce **beta-lactamase**.
*Intrinsic absence of a target site for the drug*
- While some bacteria inherently lack the target site for certain drugs (e.g., mycoplasma lacking a cell wall, thus being resistant to beta-lactams), this is less likely to be the **most common mechanism of acquired resistance** leading to treatment failure in a typical perianal infection.
- The rapid progression and failed initial treatment point towards an **acquired mechanism of resistance** rather than an intrinsic one.
*Use of an altered metabolic pathway*
- This mechanism, such as altered **folate synthesis pathways** in resistance to trimethoprim-sulfamethoxazole, is less common as the primary mechanism for ampicillin resistance.
- Ampicillin's mechanism of action primarily targets the **bacterial cell wall**, not a metabolic pathway in the same way.
*Altered structural target for the drug*
- This involves modifications to the **penicillin-binding proteins (PBPs)**, which are the targets of beta-lactam antibiotics like ampicillin. While a valid mechanism (e.g., in MRSA), the **production of beta-lactamase** is generally a more widespread and common cause of ampicillin failure, especially in infections involving mixed flora from the perianal region.
- Given the abrupt failure of ampicillin, **beta-lactamase inactivation** is a more immediate and common cause than a rapid mutational change in PBPs.
*Drug efflux pump*
- **Efflux pumps** actively remove antibiotics from the bacterial cell, contributing to resistance against various drug classes.
- While efflux pumps can play a role, the dominant mechanism for resistance to **ampicillin** in many common perianal pathogens is the **enzymatic degradation by beta-lactamases**.
Enterococci US Medical PG Question 2: A 75-year-old man presents to his primary care provider with malaise and low-grade fever after he underwent a cystoscopy for recurrent cystitis and pyelonephritis two weeks ago. His past medical history is significant for coronary artery disease and asthma. His current medications include aspirin, metoprolol, atorvastatin, and albuterol inhaler. Temperature is 37.2°C (99.0°F), blood pressure is 110/70 mm Hg, pulse is 92/min and respirations are 14/min. On physical examination, there are painless areas of hemorrhage on his palms and soles. Cardiac auscultation reveals a new pansystolic murmur over the apex. An echocardiogram shows echogenic endocardial vegetation on a leaflet of the mitral valve. Which of the following pathogens is most likely responsible for his condition?
- A. Staphylococcus aureus
- B. Enterococcus (Correct Answer)
- C. Pseudomonas aeruginosa
- D. Staphylococcus epidermidis
- E. Streptococcus gallolyticus
Enterococci Explanation: ***Enterococcus***
- The patient's history of recent **cystoscopy**, recurrent **cystitis**, and **pyelonephritis** suggests a genitourinary source of infection, making *Enterococcus* a likely pathogen for **infective endocarditis**.
- **Enterococci** are common causes of urinary tract infections, especially in elderly males and those undergoing urological procedures, and can subsequently cause endocarditis.
*Staphylococcus aureus*
- While *S. aureus* is a leading cause of infective endocarditis, particularly in intravenous drug users or those with central lines, there is no direct evidence here to suggest a **cutaneous** or **catheter-related** entry point.
- The patient's clinical presentation, specifically the preceding genitourinary procedure, points away from *S. aureus* as the most probable cause.
*Pseudomonas aeruginosa*
- *Pseudomonas aeruginosa* typically causes endocarditis in specific contexts such as **intravenous drug use** or in patients with **prosthetic valves** and healthcare-associated infections, none of which are strongly indicated.
- Despite the history of recent instrumentation, *Pseudomonas* is less common as a cause of endocarditis following cystoscopy compared to *Enterococcus*.
*Staphylococcus epidermidis*
- *S. epidermidis* is usually associated with **prosthetic valve endocarditis** or infection of **intravascular devices**, as it is a common skin commensal.
- The patient has no history of prosthetic valves, and the infection appears to be linked to a genitourinary procedure rather than a device-related contamination.
*Streptococcus gallolyticus*
- *Streptococcus gallolyticus* (**formerly *S. bovis***) is classically associated with **colorectal carcinoma** and gastrointestinal sources of bacteremia.
- Although it can cause endocarditis, the patient's presentation with a recent cystoscopy points towards a genitourinary pathogen rather than a gastrointestinal one.
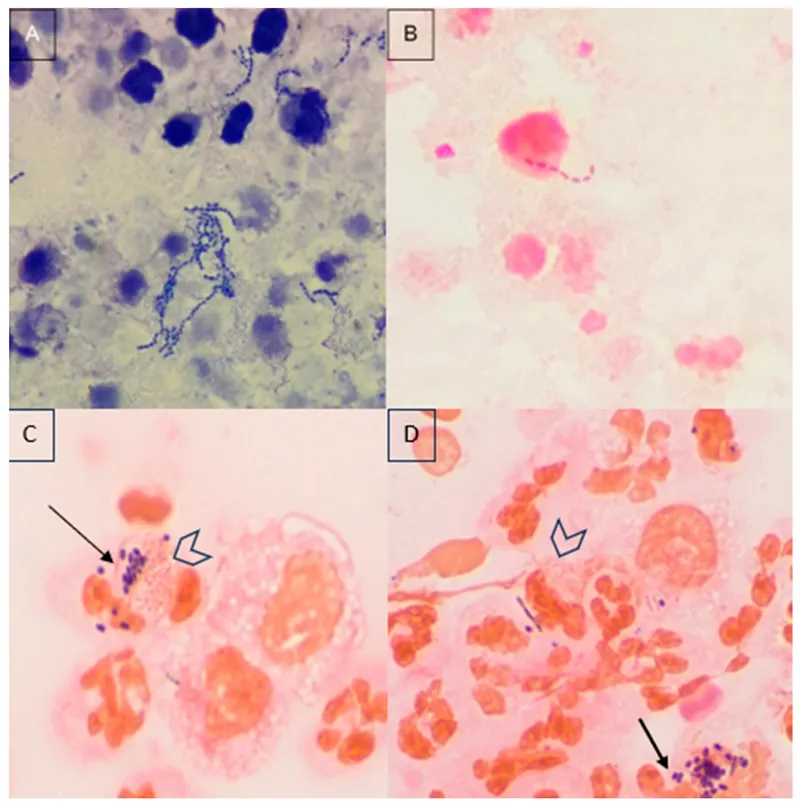
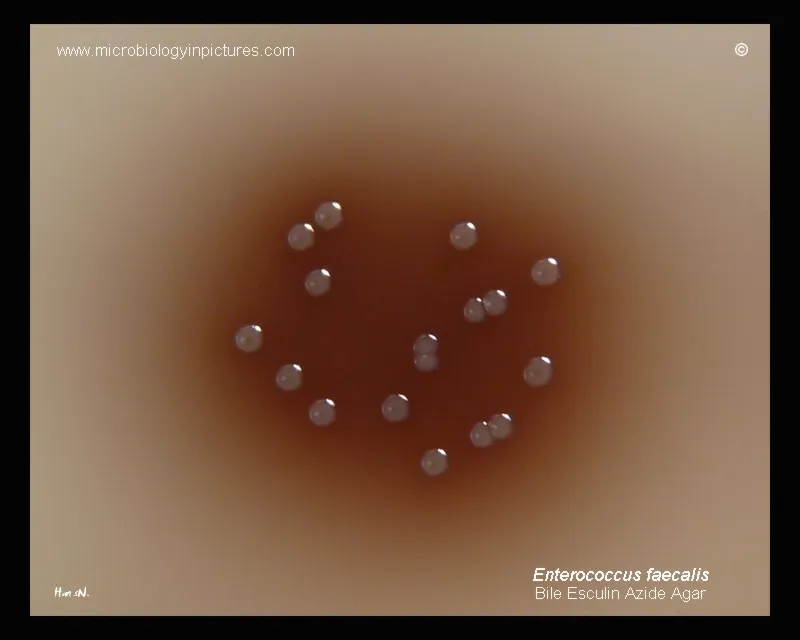
Enterococci US Medical PG Question 3: A scientist is studying the mechanisms by which bacteria become resistant to antibiotics. She begins by obtaining a culture of vancomycin-resistant Enterococcus faecalis and conducts replicate plating experiments. In these experiments, colonies are inoculated onto a membrane and smeared on 2 separate plates, 1 containing vancomycin and the other with no antibiotics. She finds that all of the bacterial colonies are vancomycin resistant because they grow on both plates. She then maintains the bacteria in liquid culture without vancomycin while she performs her other studies. Fifteen generations of bacteria later, she conducts replicate plating experiments again and finds that 20% of the colonies are now sensitive to vancomycin. Which of the following mechanisms is the most likely explanation for why these colonies have become vancomycin sensitive?
- A. Point mutation
- B. Gain of function mutation
- C. Viral infection
- D. Plasmid loss (Correct Answer)
- E. Loss of function mutation
Enterococci Explanation: ***Plasmid loss***
- The initial **vancomycin resistance** in *Enterococcus faecalis* is often mediated by genes located on **plasmids**, which are extrachromosomal DNA.
- In the absence of selective pressure (vancomycin), bacteria that lose the plasmid (and thus the resistance genes) have a **growth advantage** over those that retain the energetically costly plasmid, leading to an increase in sensitive colonies over generations.
*Point mutation*
- A **point mutation** typically involves a change in a single nucleotide and could lead to loss of resistance if it occurred in a gene conferring resistance.
- However, since there was no selective pressure for loss of resistance, it is less likely that 20% of the population would acquire such a specific point mutation to revert resistance.
*Gain of function mutation*
- A **gain of function mutation** would imply that the bacteria acquired a *new* advantageous trait, not the *loss* of resistance.
- This type of mutation would not explain why some colonies became sensitive to vancomycin after the drug was removed.
*Viral infection*
- **Viral infection** (bacteriophages) can transfer genes through transduction or cause bacterial lysis, but it's not the primary mechanism for a widespread reversion of resistance in the absence of antibiotic pressure.
- It would not explain the observed increase in vancomycin-sensitive colonies due to evolutionary pressure.
*Loss of function mutation*
- While a **loss of function mutation** in a gene conferring resistance could lead to sensitivity, it's generally less likely to explain a 20% shift without selective pressure than **plasmid loss**.
- Plasmids are often unstable and are easily lost in the absence of selection, whereas a specific gene mutation causing loss of function would need to arise and become prevalent in the population.
Enterococci US Medical PG Question 4: A 47-year-old woman comes to the physician because of a 6-week history of fatigue and low-grade fever. She has no history of serious illness except for a bicuspid aortic valve, diagnosed 10 years ago. She does not use illicit drugs. Her temperature is 37.7°C (99.9°F). Physical examination shows petechiae under the fingernails and multiple tender, red nodules on the fingers. A new grade 2/6 diastolic murmur is heard at the right second intercostal space. Which of the following is the most likely causal organism?
- A. Staphylococcus epidermidis
- B. Streptococcus pyogenes
- C. Streptococcus sanguinis (Correct Answer)
- D. Streptococcus pneumoniae
- E. Enterococcus faecalis
Enterococci Explanation: ***Streptococcus sanguinis***
- The patient's presentation with **fatigue, low-grade fever, petechiae, tender nodules (Osler nodes)**, and a **new diastolic murmur** in a patient with a **bicuspid aortic valve** is highly suggestive of **infective endocarditis**.
- **Streptococcus sanguinis** (and other viridans streptococci) are common causes of subacute bacterial endocarditis, often associated with **oral flora** and pre-existing valvular heart disease.
*Staphylococcus epidermidis*
- This organism is a common cause of **prosthetic valve endocarditis** and **nosocomial infections** but is less likely to cause endocarditis in a native valve without a history of recent surgery or intravenous lines.
- While it can cause endocarditis, the clinical features here, especially the lack of recent medical interventions, point away from *S. epidermidis* as the primary cause.
*Streptococcus pyogenes*
- **Streptococcus pyogenes** is primarily known for causing **strep throat, scarlet fever, and rheumatic fever**, which can lead to rheumatic heart disease but rarely causes acute or subacute infective endocarditis directly.
- It typically causes more acute and severe infections, which doesn't align with the 6-week history of low-grade fever and fatigue.
*Streptococcus pneumoniae*
- **Streptococcus pneumoniae** is a common cause of **pneumonia, meningitis, and otitis media** but is an uncommon cause of infective endocarditis, accounting for a very small percentage of cases.
- Endocarditis due to *S. pneumoniae* tends to be **acute and fulminant**, often associated with severe systemic illness, which is not fully consistent with the subacute presentation here.
*Enterococcus faecalis*
- **Enterococcus faecalis** is a common cause of **nosocomial urinary tract infections** and can cause endocarditis, especially in older patients or those with gastrointestinal or genitourinary procedures.
- While it's a possibility for endocarditis, the oral flora association with viridans streptococci (like *S. sanguinis*) in the context of a bicuspid aortic valve makes it a more direct fit.
Enterococci US Medical PG Question 5: A 22-year-old man presents to clinic with a chief concern about a painless ulcer on his penis that he noticed 4 weeks ago and resolved one week ago. He denies any pain on urination or changes in urinary patterns. He admits to having multiple sexual partners in the past 3 months and inconsistent use of barrier protection. His vitals are within normal limits and his physical exam is unremarkable. He is given the appropriate antibiotic for this condition and sent home. What molecular structure is mimicked by the antibiotic most likely prescribed in this case?
- A. D-Ala-D-Ala (Correct Answer)
- B. Retinoic acid
- C. Uracil
- D. Adenine
- E. Folate intermediates
Enterococci Explanation: ***D-Ala-D-Ala***
- The patient's presentation of a **painless penile ulcer** (chancre) that resolves spontaneously, along with high-risk sexual behavior, is highly suggestive of **primary syphilis**.
- The standard treatment for primary syphilis is **penicillin G**, a beta-lactam antibiotic that targets bacterial cell wall synthesis by mimicking the **D-Ala-D-Ala** terminus of peptidoglycan precursors.
- Penicillin binds to penicillin-binding proteins (transpeptidases) that normally recognize D-Ala-D-Ala, thereby inhibiting cell wall synthesis.
*Retinoic acid*
- **Retinoic acid** is a derivative of vitamin A involved in cell growth and differentiation.
- It is not a molecular structure mimicked by antibiotics used to treat bacterial infections like syphilis.
*Uracil*
- **Uracil** is a pyrimidine base found in RNA.
- While some antibiotics target nucleic acid synthesis, they do not specifically mimic uracil as their mechanism of action.
*Adenine*
- **Adenine** is a purine base found in both DNA and RNA.
- Antibiotics do not mimic adenine to exert their antibacterial effects.
*Folate intermediates*
- Some antibiotics, such as **sulfonamides**, do structurally mimic **PABA (para-aminobenzoic acid)**, which is a folate pathway intermediate.
- However, these antibiotics are not used to treat syphilis, and penicillin (the correct treatment) does not mimic folate intermediates.
Enterococci US Medical PG Question 6: A 24-year-old woman presents to her primary care physician with a 3 day history of pain with urination. She says that this pain has been accompanied by abdominal pain as well as a feeling like she always needs to use the restroom. She has no past medical history and no family history that she can recall. She is currently sexually active with a new partner but has tested negative for sexually transmitted infections. Physical exam reveals suprapubic tenderness and urine culture reveals gram-positive cocci. Which of the following best describes the organism that is most likely causing this patient's symptoms?
- A. Catalase negative and beta-hemolytic
- B. Catalase negative and alpha-hemolytic
- C. Catalase positive and coagulase positive
- D. Coagulase negative and novobiocin sensitive
- E. Coagulase negative and novobiocin resistant (Correct Answer)
Enterococci Explanation: ***Coagulase negative and novobiocin resistant***
- The patient's symptoms (dysuria, abdominal pain, urinary urgency) combined with gram-positive cocci in the urine culture, especially in a sexually active young woman, are highly suggestive of a **Staphylococcus saprophyticus** urinary tract infection (UTI).
- *Staphylococcus saprophyticus* is characteristically **coagulase-negative** and naturally **resistant to novobiocin**.
*Catalase negative and beta-hemolytic*
- This describes organisms like **Streptococcus pyogenes**, which typically causes pharyngitis or skin infections, not UTIs with these characteristics.
- While *Streptococcus pyogenes* is gram-positive cocci, it is **catalase-negative**, differentiating it from *Staphylococcus* species.
*Catalase negative and alpha-hemolytic*
- This description fits **Streptococcus pneumoniae** or **viridans streptococci**.
- These organisms are generally associated with pneumonia, otitis media, or endocarditis, not commonly with UTIs presenting in this manner.
*Catalase positive and coagulase positive*
- This describes **Staphylococcus aureus**, which is a significant pathogen but less likely to cause uncomplicated UTIs in this demographic and presentation.
- While *Staphylococcus aureus* can cause UTIs, it's typically associated with a different clinical context or more severe infections.
*Coagulase negative and novobiocin sensitive*
- This describes **Staphylococcus epidermidis** and other common coagulase-negative staphylococci.
- While present on the skin, *Staphylococcus epidermidis* is usually a contaminant in urine cultures or causes UTIs in catheterized patients, and it is **novobiocin sensitive**, unlike *Staphylococcus saprophyticus*.
Enterococci US Medical PG Question 7: While testing various strains of Streptococcus pneumoniae, a researcher discovers that a certain strain of this bacteria is unable to cause disease in mice when deposited in their lungs. What physiological test would most likely deviate from normal in this strain of bacteria as opposed to a typical strain?
- A. Quellung reaction (Correct Answer)
- B. Hemolytic reaction when grown on sheep blood agar
- C. Bile solubility
- D. Optochin sensitivity
- E. Motility
Enterococci Explanation: ***Quellung reaction***
- The **Quellung reaction** tests for the presence of the **polysaccharide capsule**, which is the primary virulence factor of *S. pneumoniae*.
- An **avirulent strain** that cannot cause disease would most likely lack the capsule and show a **negative Quellung reaction** (no capsular swelling), deviating from the **positive reaction** seen in typical encapsulated pathogenic strains.
- The capsule enables *S. pneumoniae* to evade phagocytosis and complement-mediated killing, which is essential for establishing infection in the lungs.
*Hemolytic reaction when grown on sheep blood agar*
- Both virulent and avirulent strains of *S. pneumoniae* typically exhibit **alpha-hemolysis** (partial hemolysis, producing a greenish discoloration) on sheep blood agar due to the production of pneumolysin.
- This characteristic does not differentiate between pathogenic and non-pathogenic strains in terms of disease-causing ability.
*Bile solubility*
- *S. pneumoniae* is characteristically **bile-soluble** due to the presence of autolysin enzymes that are activated by bile salts, leading to cellular lysis.
- This property is a **species characteristic** present in both virulent and avirulent strains, thus it would not explain the inability to cause disease.
*Optochin sensitivity*
- *S. pneumoniae* is universally **sensitive to optochin**, a chemical agent that inhibits its growth and is used for laboratory identification.
- This characteristic is used for **species identification** but does not correlate with strain virulence or disease-causing ability.
*Motility*
- *Streptococcus pneumoniae* is a **non-motile** bacterium; it lacks flagella.
- This characteristic is consistent across all strains and is not a virulence factor for this species.
Enterococci US Medical PG Question 8: A 51-year-old man is admitted to the hospital because of a 2-day history of fever, nausea, and abdominal pain. His temperature is 39.4°C (102.9°F) and pulse is 106/min. Physical examination shows tenderness in the right upper quadrant. Blood cultures grow nonhemolytic, gram-positive cocci that grow in hypertonic saline. Antibiotic sensitivity testing of the isolated organism shows that gentamicin has a minimum inhibitory concentration (MIC) of 16 μg/mL. The addition of ampicillin, which has an MIC of 2 μg/mL alone, decreases the MIC of gentamicin to 0.85 μg/mL. The decrease in the MIC of gentamicin with the addition of ampicillin is most likely due to which of the following mechanisms?
- A. Increase in the intracellular uptake of gentamicin (Correct Answer)
- B. Sequential block of essential micronutrient synthesis
- C. Inhibition of the acetylation of gentamicin
- D. Additive bacteriostatic effect of ampicillin
- E. Stabilization of gentamicin binding at the target site
Enterococci Explanation: ***Increase in the intracellular uptake of gentamicin***
- This scenario describes **synergism**, where ampicillin (a cell wall synthesis inhibitor) damages the bacterial cell wall, allowing better penetration of gentamicin (an aminoglycoside) into the cell. Aminoglycosides require **active transport** across the bacterial cell membrane, which is enhanced by cell wall disruption.
- The significant reduction in gentamicin's MIC when combined with ampicillin demonstrates that ampicillin facilitates gentamicin's access to its **ribosomal target**, leading to a more potent bactericidal effect.
*Sequential block of essential micronutrient synthesis*
- **Sequential block** typically refers to the synergistic action of drugs like trimethoprim and sulfamethoxazole, which inhibit different steps in the **folic acid synthesis pathway**.
- This mechanism is not directly applicable to the combination of a cell wall inhibitor and an aminoglycoside, which target different cellular processes.
*Inhibition of the acetylation of gentamicin*
- **Acetylation** is a common mechanism of aminoglycoside inactivation by bacterial enzymes (aminoglycoside-modifying enzymes).
- Ampicillin does not primarily work by inhibiting these enzymes; its main action is on **peptidoglycan synthesis** in the bacterial cell wall.
*Additive bacteriostatic effect of ampicillin*
- Ampicillin is a **bactericidal antibiotic** that works by inhibiting cell wall synthesis, not typically bacteriostatic in its primary action, especially against susceptible organisms.
- The dramatic drop in gentamicin's MIC suggests more than just an additive bacteriostatic effect; it indicates a **synergistic interaction** leading to enhanced bactericidal activity.
*Stabilization of gentamicin binding at the target site*
- Gentamicin binds to the bacterial **30S ribosomal subunit**, inhibiting protein synthesis.
- Ampicillin's mechanism of action is on the **bacterial cell wall**, and it does not directly stabilize the binding of gentamicin to the ribosome. Its role is to facilitate gentamicin's entry into the cell.
Enterococci US Medical PG Question 9: A 45-year-old man comes to the physician because of a 1-month history of fever and poor appetite. Five weeks ago, he underwent molar extraction for dental caries. His temperature is 38°C (100.4°F). Cardiac examination shows a grade 2/6 holosystolic murmur heard best at the apex. A blood culture shows gram-positive, catalase-negative cocci. Transesophageal echocardiography shows a small vegetation on the mitral valve with mild regurgitation. The causal organism most likely has which of the following characteristics?
- A. Production of dextrans (Correct Answer)
- B. Production of CAMP factor
- C. Conversion of fibrinogen to fibrin
- D. Formation of germ tubes at body temperature
- E. Replication in host macrophages
Enterococci Explanation: **Production of dextrans**
- The clinical picture of **fever**, **poor appetite**, a **holosystolic murmur**, and **mitral valve vegetation** following a dental procedure (molar extraction) strongly points to **infective endocarditis** caused by **Viridans streptococci**.
- **Viridans streptococci**, commonly found in the oral cavity, produce **dextrans**, which allow them to adhere to damaged heart valves and fibrin-platelet aggregates, initiating vegetation formation.
*Production of CAMP factor*
- **CAMP factor** is a characteristic of **Group B Streptococcus (Streptococcus agalactiae)**, which primarily causes infections in neonates and immunocompromised adults, not typically infective endocarditis post-dental procedure.
- *Streptococcus agalactiae* is also catalase-negative and gram-positive but is rarely associated with endocarditis arising from oral flora.
*Conversion of fibrinogen to fibrin*
- The ability to convert **fibrinogen to fibrin** is characteristic of **coagulase-positive organisms**, such as *Staphylococcus aureus*, which is a catalase-positive organism.
- The blood culture in this case specifically states **catalase-negative cocci**, ruling out *Staphylococcus aureus* as the causative agent.
*Formation of germ tubes at body temperature*
- **Germ tube formation** at body temperature is a distinguishing characteristic of *Candida albicans*, a **fungus**, not a gram-positive, catalase-negative coccus.
- While *Candida* can cause endocarditis, the microbiological findings described do not align with a fungal infection.
*Replication in host macrophages*
- **Intracellular replication in host macrophages** is characteristic of certain bacteria like *Mycobacterium tuberculosis*, *Listeria monocytogenes*, or *Salmonella typhi*, which typically cause systemic infections
- This characteristic is not associated with the gram-positive, catalase-negative cocci responsible for subacute bacterial endocarditis following dental procedures.
Enterococci US Medical PG Question 10: A previously healthy 24-year-old woman comes to the physician because of a 1-day history of nausea and weakness. She is sexually active with 2 male partners and uses an oral contraceptive; she uses condoms inconsistently. Her last menstrual period was 4 days ago. Her temperature is 38.4°C (101°F). Physical examination shows right costovertebral angle tenderness. Pelvic examination is normal. Which of the following is the most likely cause of this patient's condition?
- A. Noninfectious inflammation of the bladder
- B. Ascending bacteria from the endocervix
- C. Decreased renal calcium reabsorption
- D. Decreased urinary pH
- E. Ascending bacteria from the bladder (Correct Answer)
Enterococci Explanation: ***Ascending bacteria from the bladder***
- The patient presents with **fever**, **nausea**, **weakness**, and **right costovertebral angle (CVA) tenderness**, which are classic symptoms of **acute pyelonephritis**.
- **Pyelonephritis** most commonly results from an **ascending urinary tract infection**, where bacteria (typically *E. coli*) from the bladder travel up the ureters to infect the kidneys.
- This accounts for approximately **95% of pyelonephritis cases** in young women.
*Noninfectious inflammation of the bladder*
- **Noninfectious cystitis** (interstitial cystitis) would not typically present with systemic symptoms like **fever** and **nausea**, or with **CVA tenderness**, which indicates kidney involvement.
- Bladder inflammation typically causes dysuria and frequency without systemic signs of infection.
*Ascending bacteria from the endocervix*
- **Ascending bacteria from the endocervix** can cause **pelvic inflammatory disease (PID)**, which presents with lower abdominal pain, cervical motion tenderness, and vaginal discharge.
- While PID can cause fever, the **normal pelvic examination** in this patient rules out this diagnosis, and PID **does not typically cause CVA tenderness**.
*Decreased renal calcium reabsorption*
- **Decreased renal calcium reabsorption** is associated with **hypercalciuria** and **nephrolithiasis** (kidney stones), which can present with acute flank pain if obstruction occurs.
- However, this condition does not explain the **fever** and systemic symptoms characteristic of an acute infectious process.
*Decreased urinary pH*
- **Decreased urinary pH** (acidic urine) can predispose to certain types of kidney stone formation but is not a direct cause of **pyelonephritis**.
- It does not explain the presence of **fever**, **CVA tenderness**, and systemic symptoms indicative of a bacterial kidney infection.
More Enterococci US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.