Clostridium species US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Clostridium species. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Clostridium species US Medical PG Question 1: A 59-year-old woman comes to the emergency department because of abdominal pain and bloody diarrhea that began 12 hours ago. Three days ago, she ate undercooked chicken at a local restaurant. Blood cultures grow spiral and comma-shaped, oxidase-positive organisms at 42°C. This patient is at greatest risk for which of the following complications?
- A. Toxic megacolon
- B. Segmental myelin degeneration (Correct Answer)
- C. Peyer patch necrosis
- D. Seizures
- E. Erythema nodosum
Clostridium species Explanation: ***Segmental myelin degeneration***
- The description of the organism (spiral/comma-shaped, oxidase-positive, growing
at 42°C) combined with bloody diarrhea from undercooked chicken strongly
suggests **_Campylobacter jejuni_** infection.
- _Campylobacter jejuni_ infection is the most common antecedent infection
for **Guillain-Barré syndrome (GBS)**, which is characterized by **segmental
demyelination** of peripheral nerves.
*Toxic megacolon*
- This complication is more commonly associated with severe inflammatory bowel disease or
infections like **_Clostridium difficile_** or **_Entamoeba histolytica_**.
- While theoretically possible with any severe diarrheal illness, it is not the **greatest
risk** specifically linked to _Campylobacter_ in this context.
*Peyer patch necrosis*
- **Peyer patch necrosis** is a characteristic complication seen in **typhoid fever**, caused by
**_Salmonella Typhi_**, which would present differently (e.g., rose spots, bradycardia,
step-wise fever).
- _Campylobacter_ infection primarily causes inflammation of the
intestinal mucosa rather than necrosis of Peyer patches.
*Seizures*
- Seizures are not a typical or common direct complication of _Campylobacter
jejuni_ infection in adults, although severe electrolyte imbalances from any
diarrhea could rarely precipitate them.
- They are more commonly associated with direct CNS infections or severe systemic
inflammatory responses from other pathogens.
*Erythema nodosum*
- **Erythema nodosum** is a non-specific inflammatory condition that can be
associated with various infections, including streptococcal infections, tuberculosis,
and some fungal diseases, as well as inflammatory bowel disease.
- While it has been reported rarely with _Campylobacter_ infections, it is not the **most
significant or common complication** compared to GBS.
Clostridium species US Medical PG Question 2: A 26-year-old man with no past medical history is brought in to the trauma bay by ambulance after sustaining a motorcycle crash against a parked car. The patient is alert and oriented with no focal neurologic defects. The patient has a few lower extremity abrasions but is otherwise healthy and is discharged. One week later, the patient returns to the emergency department with a 2-day history of high fevers and redness on his left lower leg. On exam, his temperature is 102.0°F (38.9°C), blood pressure is 70/44 mmHg, pulse is 108/min, and respirations are 14/min. The patient appears toxic, and his left lower leg is tense, erythematous, and tender to palpation between the ankle and the knee. The exam is notable for tense bullae developing on the lateral calf. Palpation near the bullae is notable for crepitus. Which of the following toxins is likely responsible for this finding?
- A. Enterotoxin
- B. Cytotoxin
- C. Tetanospasmin
- D. Botulinum toxin
- E. Alpha toxin (Correct Answer)
Clostridium species Explanation: ***Alpha toxin***
- The patient's symptoms of **fever**, **hypotension**, **tachycardia**, and a **tense**, **erythematous**, **tender leg with bullae and crepitus** are characteristic of **necrotizing fasciitis**, likely caused by *Clostridium perfringens*.
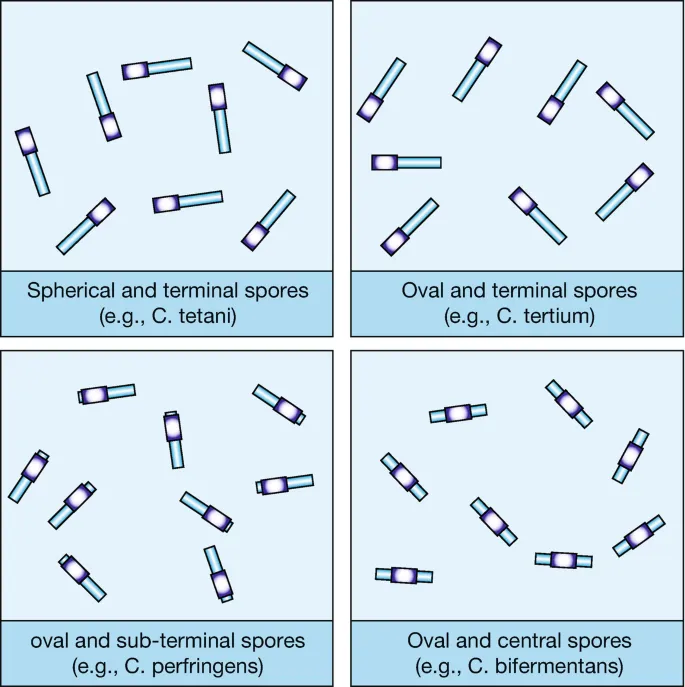
- *Clostridium perfringens* produces an **alpha toxin** (phospholipase C) that is a potent **lecithinase**, causing widespread cell membrane destruction, hemolysis, tissue necrosis, and gas gangrene.
*Enterotoxin*
- **Enterotoxins** are typically associated with **food poisoning** or **diarrheal illnesses** and primarily affect the gastrointestinal tract.
- They do not typically cause the **severe local tissue destruction with crepitus** observed in this patient.
*Cytotoxin*
- **Cytotoxins** are a broad class of toxins that can kill cells, but in the context of bacterial infections, "cytotoxin" alone does not specify the typical clinical picture.
- While *Clostridium perfringens* toxins are cytotoxic, the term "cytotoxin" is too general and less specific than **alpha toxin** for this clinical presentation.
*Tetanospasmin*
- **Tetanospasmin** is produced by *Clostridium tetani* and causes **spastic paralysis** and **muscle rigidity** (e.g., lockjaw) by blocking inhibitory neurotransmitters.
- It does not cause diffuse tissue necrosis, gas formation, or the systemic signs of **septic shock** seen in this patient.
*Botulinum toxin*
- **Botulinum toxin**, produced by *Clostridium botulinum*, causes **flaccid paralysis** by inhibiting acetylcholine release at the neuromuscular junction.
- This symptom is distinct from the **acute necrotizing infection** with systemic inflammatory response syndrome (SIRS) symptoms described.
Clostridium species US Medical PG Question 3: A 20-week-old infant is brought to an urgent care clinic by her mother because she has not been eating well for the past 2 days. The mother said her daughter has also been "floppy" since yesterday morning and has been unable to move or open her eyes since the afternoon of the same day. The child has recently started solid foods, like cereals sweetened with honey. There is no history of loose, watery stools. On examination, the child is lethargic with lax muscle tone. She does not have a fever or apparent respiratory distress. What is the most likely mode of transmission of the pathogen responsible for this patient’s condition?
- A. Vertical transmission
- B. Vector-borne disease
- C. Direct contact
- D. Contaminated food (Correct Answer)
- E. Airborne transmission
Clostridium species Explanation: ***Contaminated food***
- The infant's symptoms of **lethargy**, widespread **flaccid paralysis** (floppy, unable to move or open eyes), and recent ingestion of **honey** (a known source of **Clostridium botulinum** spores) strongly suggest **infant botulism**.
- **Infant botulism** is acquired through the ingestion of **Clostridium botulinum spores**, typically from environmental sources or contaminated food like honey, which then germinate in the infant's immature gut.
*Vertical transmission*
- **Vertical transmission** refers to the passage of a pathogen from mother to offspring during pregnancy, birth, or breastfeeding.
- The clinical picture of **flaccid paralysis** and association with **honey ingestion** in this case does not align with typical vertically transmitted infections.
*Vector-borne disease*
- **Vector-borne diseases** are transmitted by an arthropod vector, such as mosquitoes or ticks.
- There is no clinical or epidemiological evidence in the scenario to suggest an **arthropod vector** as the source of this infant's illness.
*Direct contact*
- Diseases transmitted by **direct contact** typically require close physical interaction with an infected individual or their body fluids.
- The onset of **neurological symptoms** and the specific history of **honey ingestion** do not point to direct contact as the mode of transmission for botulism.
*Airborne transmission*
- **Airborne transmission** occurs when pathogens are spread through respiratory droplets or aerosols.
- The symptoms of **flaccid paralysis** and the history of recent **honey ingestion** are not consistent with an airborne pathogen.
Clostridium species US Medical PG Question 4: A 9-month-old baby boy is brought to his pediatrician due to poor feeding and fewer bowel movements. His father notes that he has been less active and is having difficulty with movements such as rolling over. Vital signs are normal, and physical exam is notable for weak sucking reflex, ptosis, and decreased eye movements. In addition, the baby has generalized weakness and flushed skin. Stool samples are collected, treatment is started immediately, and the baby’s condition improves. The results of the stool studies return several days later and show gram-positive, anaerobic rods. The toxin most likely responsible for this baby’s condition acts through which mechanism?
- A. Impairment of phagocytosis
- B. Increased chloride secretion within the gut
- C. Inhibition of protein synthesis
- D. Inhibition of neurotransmitter release (Correct Answer)
- E. Degradation of the cell membrane
Clostridium species Explanation: ***Inhibition of neurotransmitter release***
- The baby's symptoms of **generalized weakness**, **weak sucking reflex**, **ptosis**, and **decreased eye movements** are characteristic of **infant botulism**, caused by *Clostridium botulinum* toxins.
- These toxins, specifically the **botulinum neurotoxin**, block the release of **acetylcholine** at the **neuromuscular junction**, leading to flaccid paralysis.
*Impairment of phagocytosis*
- This mechanism is not directly related to the symptoms of **flaccid paralysis** seen in infant botulism.
- Phagocytosis is primarily involved in immune responses and pathogen clearance, not nerve transmission.
*Increased chloride secretion within the gut*
- While some bacterial toxins, like **cholera toxin**, cause increased chloride secretion leading to watery diarrhea, this is not the mechanism of botulinum toxin.
- The baby's symptoms point to neurological impairment, not excessive fluid loss in the gut.
*Inhibition of protein synthesis*
- Toxins such as **diphtheria toxin** or **Shiga toxin** inhibit protein synthesis, leading to cell death and specific clinical manifestations different from those presented here.
- The symptoms described are due to a highly specific blockage of neurotransmission rather than general cellular dysfunction.
*Degradation of the cell membrane*
- This mechanism is characteristic of toxins that form **pores** or enzymes that directly **damage cell membranes**, leading to cell lysis.
- Examples include alpha-toxin of *Clostridium perfringens*, but it does not align with the neurological symptoms of infant botulism.
Clostridium species US Medical PG Question 5: An otherwise healthy 7-year-old boy is brought to the emergency department because of a 1-day history of involuntary muscle contractions and pain in his back and neck. Two weeks ago, he fell while playing in the sandbox and scraped both his knees. He has not received any vaccinations since birth. His temperature is 38.5°C (101.3°F). He is diaphoretic. Examination shows inability to open his mouth beyond 1 cm. There is hyperextension of the lumbar spine and resistance to neck flexion. Administration of which of the following would most likely have prevented this patient's current condition?
- A. Chemically-inactivated virus
- B. Denatured bacterial product (Correct Answer)
- C. Viable but weakened microorganism
- D. Human immunoglobulin against a viral protein
- E. Capsular polysaccharides
Clostridium species Explanation: ***Denatured bacterial product***
- This describes a **toxoid vaccine**, specifically the **tetanus toxoid vaccine**, which is a denatured form of the bacterial toxin.
- The patient's symptoms (trismus, back and neck pain, muscle contractions, **opisthotonus**) are classic for **tetanus**, and his unvaccinated status and recent wound increase his risk.
*Chemically-inactivated virus*
- This refers to an **inactivated viral vaccine**, which is effective against viral infections, not bacterial toxins.
- Tetanus is caused by a bacterial toxin, not a virus, making this vaccine type irrelevant to preventing the described condition.
*Viable but weakened microorganism*
- This describes a **live-attenuated vaccine**, which typically induces a strong immune response against the live pathogen itself.
- Tetanus prevention targets the toxin produced by *Clostridium tetani*, not the microorganism directly via an attenuated form.
*Human immunoglobulin against a viral protein*
- This describes **passive immunization** using antibodies against a viral protein, usually for viral infections or post-exposure prophylaxis.
- While passive immunization with tetanus immune globulin can *treat* tetanus, a vaccine is needed for *prevention*, and the target here is a bacterial toxin, not a viral protein.
*Capsular polysaccharides*
- This describes a component of **polysaccharide vaccines** used against encapsulated bacteria (e.g., *Streptococcus pneumoniae*, *Haemophilus influenzae type b*).
- *Clostridium tetani* is not an encapsulated bacterium, and its pathogenicity stems from its toxin, not its capsule.
Clostridium species US Medical PG Question 6: A 47-year-old man comes to the physician because of abdominal pain and foul-smelling, watery diarrhea for several days. He has not had nausea, vomiting, or blood in the stool. He has a history of alcohol use disorder and recently completed a 7-day course of clindamycin for pneumonia. He has not traveled out of the United States. Which of the following toxins is most likely to be involved in the pathogenesis of this patient's symptoms?
- A. Cereulide toxin
- B. Cholera toxin
- C. Clostridioides difficile cytotoxin (Correct Answer)
- D. Shiga toxin
- E. Alpha toxin
Clostridium species Explanation: ***Clostridioides difficile cytotoxin***
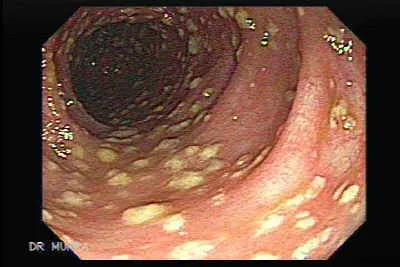
- The patient's history of recent **clindamycin** use, followed by **abdominal pain** and **foul-smelling, watery diarrhea**, is highly suggestive of *Clostridioides difficile* infection.
- *C. difficile* produces **cytotoxin (TcdB)** and **enterotoxin (TcdA)**, which lead to colitis and diarrhea, often after antimicrobial therapy.
*Cereulide toxin*
- This preformed toxin is produced by *Bacillus cereus* and typically causes a **short-incubation** emetic type of food poisoning, characterized by **nausea and vomiting**.
- The patient's symptoms are primarily diarrhea, and nausea/vomiting are absent, making this less likely.
*Cholera toxin*
- Produced by *Vibrio cholerae*, this toxin causes profuse, **"rice-water" diarrhea** with rapid dehydration.
- The patient has not traveled to endemic areas, and there is no mention of the characteristic severe dehydration or "rice-water" stool.
*Shiga toxin*
- This toxin, produced by *Shigella dysenteriae* and enterohemorrhagic *E. coli* (EHEC), typically causes **bloody diarrhea** and can lead to **hemolytic uremic syndrome (HUS)**.
- The patient's diarrhea is watery and explicitly stated to be without blood, ruling out Shiga toxin as the cause.
*Alpha toxin*
- This toxin is produced by *Clostridium perfringens* and is primarily associated with **gas gangrene** (myonecrosis) and some forms of food poisoning.
- While *C. perfringens* can cause diarrhea, it's typically mild and self-limiting, and the clinical picture in this patient, especially with recent antibiotic use, points more strongly to *C. difficile*.
Clostridium species US Medical PG Question 7: A 55-year-old man presents to the physician with complaints of 5 days of watery diarrhea, fever, and bloating. He has not noticed any blood in his stool. He states that his diet has not changed recently, and his family has been spared from diarrhea symptoms despite eating the same foods that he has been cooking at home. He has no history of recent travel outside the United States. His only medication is high-dose omeprazole, which he has been taking daily for the past few months to alleviate his gastroesophageal reflux disease (GERD). Which of the following is the most appropriate initial test to work up this patient’s symptoms?
- A. Stool toxin assay (Correct Answer)
- B. Colonoscopy
- C. Fecal occult blood test
- D. Stool culture
- E. Stool ova and parasite
Clostridium species Explanation: ***Stool toxin assay***
- The patient's presentation of **watery diarrhea** and fever, especially with a history of **high-dose omeprazole use**, strongly suggests **Clostridioides difficile infection**.
- **Omeprazole** (a proton pump inhibitor) reduces stomach acid, which can disrupt the normal gut flora and increase susceptibility to *C. difficile*; a **stool toxin assay** is the most direct diagnostic test for this infection.
*Colonoscopy*
- While a colonoscopy can visualize pseudomembranes associated with severe *C. difficile* colitis, it is an **invasive procedure** and not the initial diagnostic test of choice for suspected infectious diarrhea.
- It is usually reserved for cases with atypical presentations, suspected complications, or when other diagnostic tests are inconclusive.
*Fecal occult blood test*
- The patient describes **watery diarrhea** and specifically states he has **not noticed any blood in his stool**, making a fecal occult blood test unlikely to be helpful in this acute setting.
- This test is primarily used for screening **colorectal cancer** or identifying chronic gastrointestinal bleeding.
*Stool culture*
- A stool culture primarily identifies bacterial pathogens like *Salmonella*, *Shigella*, or *Campylobacter*, which typically cause diarrheal illnesses that may include **bloody stools** or have specific epidemiological links (e.g., foodborne outbreaks).
- Given the history of **omeprazole use** and the absence of blood, *C. difficile* is more likely than these common bacterial enteritides, and a stool culture does not detect *C. difficile* itself.
*Stool ova and parasite*
- This test is used to detect **parasitic infections** (e.g., Giardia, Cryptosporidium), which can cause watery diarrhea and bloating.
- However, given the specific risk factor of **omeprazole use**, **Clostridioides difficile** infection is a more probable diagnosis, making the stool toxin assay the more appropriate initial test.
Clostridium species US Medical PG Question 8: A 48-year-old woman comes to the physician for a follow-up examination. Six months ago, she was diagnosed with overactive bladder syndrome and began treatment with oxybutynin. She continues to have involuntary loss of urine with sudden episodes of significant bladder discomfort that is only relieved by voiding. A substance is injected into the detrusor muscle to treat her symptoms. The physician informs the patient that she will have transitory relief for several months before symptoms return and will require repeated treatment. The injected substance is most likely produced by an organism with which of the following microbiological properties?
- A. Gram-negative, encapsulated diplococcus
- B. Gram-negative, comma-shaped rod
- C. Gram-positive, club-shaped rod
- D. Gram-negative, aerobic coccobacillus
- E. Gram-positive, spore-forming rod (Correct Answer)
Clostridium species Explanation: ***Gram-positive, spore-forming rod***
- The patient's symptoms of **overactive bladder** are being treated with a substance injected into the detrusor muscle, providing temporary relief, which is characteristic of **botulinum toxin**.
- **Botulinum toxin** is produced by *Clostridium botulinum*, a **Gram-positive, spore-forming anaerobic rod** known for producing potent neurotoxins.
*Gram-negative, encapsulated diplococcus*
- This describes organisms like *Neisseria meningitidis*, which causes **meningitis** and **sepsis**, not conditions treated with muscle relaxants.
- The clinical presentation and treatment are inconsistent with infections caused by such bacteria.
*Gram-negative, comma-shaped rod*
- This morphology is characteristic of *Vibrio cholerae*, which causes **cholera**, an acute diarrheal illness.
- There is no clinical relevance of *Vibrio cholerae* toxins in the treatment of overactive bladder.
*Gram-positive, club-shaped rod*
- This describes *Corynebacterium diphtheriae*, the causative agent of **diphtheria**, a respiratory illness.
- The diphtheria toxin causes tissue damage and systemic effects, but it is not used therapeutically for muscle relaxation.
*Gram-negative, aerobic coccobacillus*
- This describes bacteria such as *Bordetella pertussis*, which causes **pertussis (whooping cough),** and *Haemophilus influenzae*.
- Toxins from these organisms are not used for therapeutic detrusor muscle relaxation.
Clostridium species US Medical PG Question 9: A 24-year-old college student consumed a container of canned vegetables for dinner. Fourteen hours later, he presents to the E.R. complaining of difficulty swallowing and double-vision. The bacterium leading to these symptoms is:
- A. Rod-shaped (Correct Answer)
- B. An obligate aerobe
- C. Gram-negative
- D. Non-spore forming
- E. Cocci-shaped
Clostridium species Explanation: ***Rod-shaped***
- The symptoms of **difficulty swallowing (dysphagia)** and **double vision (diplopia)**, following consumption of canned food, are highly indicative of **botulism**, caused by *Clostridium botulinum*.
- *Clostridium botulinum* is a **rod-shaped (bacillus)** bacterium, which is a key morphological characteristic.
*An obligate aerobe*
- *Clostridium botulinum* is actually an **obligate anaerobe**, meaning it thrives in environments without oxygen, such as sealed cans.
- An obligate aerobe requires oxygen for growth; therefore, this statement is incorrect.
*Gram-negative*
- *Clostridium botulinum* is a **Gram-positive bacterium**, specifically a Gram-positive rod.
- Gram-negative bacteria have a different cell wall structure and stain pink/red, unlike the purple of Gram-positive bacteria.
*Non-spore forming*
- *Clostridium botulinum* is a **spore-forming bacterium**, and its spores are famously heat-resistant, allowing them to survive inadequate canning processes.
- The formation of spores is crucial for its survival and persistence in various environments.
*Cocci-shaped*
- **Cocci-shaped** bacteria are spherical, but *Clostridium botulinum* is explicitly **rod-shaped (bacillus)**.
- This morphological description does not match the causative agent of botulism.
Clostridium species US Medical PG Question 10: A 2-year-old girl who emigrated from Pakistan 2 weeks ago is brought to the emergency department because of lower limb weakness for one-day. One week ago, she had a 3-day episode of flu-like symptoms that resolved without treatment. She has not yet received any routine childhood vaccinations. Deep tendon reflexes are 1+ in the right lower extremity and absent in the left lower extremity. Analysis of cerebrospinal fluid shows a leukocyte count of 38 cells/mm3 (68% lymphocytes), a protein concentration of 49 mg/dL, and a glucose concentration of 60 mg/dL. Which of the following is the most likely diagnosis in this patient?
- A. Poliomyelitis (Correct Answer)
- B. Tetanus
- C. Guillain-Barre syndrome
- D. Botulism
- E. HSV encephalitis
Clostridium species Explanation: ***Poliomyelitis***
- The patient's presentation with **acute flaccid paralysis** (lower limb weakness with absent reflexes), recent emigration from a region with potential **endemic polio** (Pakistan), and **lack of vaccination** are highly suggestive of poliomyelitis.
- The **CSF findings** (mild pleocytosis with lymphocytic predominance and normal glucose) are consistent with a viral infection of the central nervous system, which is characteristic of polio.
*Tetanus*
- Tetanus typically presents with **spastic paralysis**, muscle rigidity, and **lockjaw**, not flaccid paralysis.
- The onset of symptoms is also usually preceded by a wound contamination, which is not mentioned in this case.
*Guillain-Barre syndrome*
- While GBS can cause **flaccid paralysis** and is often preceded by a viral illness, it typically presents with **ascending paralysis** and the CSF classically shows **albumino-cytological dissociation** (high protein with normal or low cell count), which is not fully consistent with the CSF findings here.
- The rapid onset of significant asymmetry in reflexes is also less typical for GBS.
*Botulism*
- Botulism causes **descending flaccid paralysis**, often starting with cranial nerve palsies (e.g., ptosis, diplopia), and is typically associated with ingestion of contaminated food or honey in infants.
- The patient's symptoms are more focused on lower limb weakness without initial cranial nerve involvement, and the CSF findings are usually normal in botulism.
*HSV encephalitis*
- HSV encephalitis typically presents with **fever, seizures, altered mental status, and focal neurological deficits**, not primarily acute flaccid paralysis.
- While it is a viral encephalitis, the predominant symptom pattern and the specific lower limb weakness are not characteristic of HSV encephalitis.
More Clostridium species US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.