Bacillus species US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Bacillus species. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Bacillus species US Medical PG Question 1: A 32-year-old woman comes to the emergency department with a 2-day history of abdominal pain and diarrhea. She has had about 8 voluminous stools per day, some of which were bloody. She visited an international food festival three days ago. She takes no medications. Her temperature is 39.5°C (103.1°F), pulse is 90/min, and blood pressure is 110/65 mm Hg. Examination shows a tender abdomen, increased bowel sounds, and dry mucous membranes. Microscopic examination of the stool shows polymorphonuclear leukocytes. Stool culture results are pending. Which of the following most likely caused the patient's symptoms?
- A. Home-canned vegetables
- B. Yogurt dip
- C. Reheated rice
- D. Toxic mushrooms
- E. Omelette (Correct Answer)
Bacillus species Explanation: **Omelette**
- The symptoms, including **bloody diarrhea**, fever, and exposure to an international food festival suggest a **bacterial infection**, likely from contaminated eggs (e.g., **Salmonella**).
- The presence of **polymorphonuclear leukocytes** in the stool indicates an **invasive bacterial infection**, consistent with salmonellosis.
*Home-canned vegetables*
- Poorly preserved home-canned vegetables are a classic cause of **botulism**, which presents with **neurological symptoms** (e.g., flaccid paralysis) and is not characterized by bloody diarrhea or fever.
- While it can cause gastrointestinal upset, bloody stools are not typical, and the primary concern is neurotoxicity due to **Clostridium botulinum toxin**.
*Yogurt dip*
- Yogurt is a dairy product, and contamination typically leads to **non-bloody diarrhea** and vomiting, often caused by bacteria like *Staphylococcus aureus* or *Bacillus cereus* producing enterotoxins.
- The symptoms would likely be less severe and lack the invasive features (bloody stools, fever, PMNs) seen in this patient.
*Reheated rice*
- Reheated rice is commonly associated with **Bacillus cereus** food poisoning, which typically causes either an emetic (vomiting) or diarrheal syndrome.
- The diarrhea caused by *Bacillus cereus* is usually **watery and non-bloody**, and it rarely presents with significant fever or invasive features like polymorphonuclear leukocytes in stool.
*Toxic mushrooms*
- Mushroom poisoning can present with a wide range of symptoms, including gastrointestinal distress (vomiting, diarrhea), but the presentation varies greatly depending on the mushroom species.
- **Bloody diarrhea** with fever and polymorphonuclear leukocytes in stool is not a typical hallmark of common toxic mushroom ingestions, which often involve hepatotoxicity or neurotoxicity.
Bacillus species US Medical PG Question 2: A 12-year-old boy presents to the emergency room with difficulty breathing after several days of severe sore throat. Further history reveals that his family immigrated recently from Eastern Europe and he has never previously seen a doctor. Physical exam shows cervical lymphadenopathy with extensive neck edema as well as the finding shown in the image provided. You suspect a bacteria that causes the disease by producing an AB type exotoxin. Which of the following is the proper medium to culture the most likely cause of this infection?
- A. Thayer-Martin Agar
- B. Charcoal Yeast Agar
- C. Tellurite Agar (Correct Answer)
- D. Eaton's Agar
- E. Bordet-Gengou Agar
Bacillus species Explanation: ***Tellurite Agar***
- The clinical picture (sore throat, neck edema, cervical lymphadenopathy, difficulty breathing, recent immigration from Eastern Europe, unvaccinated) is highly suggestive of **diphtheria**, caused by *Corynebacterium diphtheriae*.
- **Tellurite agar** (e.g., cysteine-tellurite blood agar or Tinsdale medium) is the selective medium used to isolate *Corynebacterium diphtheriae*, which forms characteristic **gray-black colonies** due to the reduction of tellurite.
*Thayer-Martin Agar*
- This is a selective medium primarily used for the isolation of **Neisseria gonorrhoeae** and **Neisseria meningitidis**.
- It contains antibiotics to inhibit the growth of other bacteria and fungi, which would not be appropriate for *Corynebacterium diphtheriae*.
*Charcoal Yeast Agar*
- **Buffered Charcoal Yeast Extract (BCYE) agar** is the specific medium used for the isolation of **Legionella species**, particularly *Legionella pneumophila*.
- *Legionella* requires **L-cysteine** and **iron salts** for growth, which are provided in BCYE agar.
*Bordet-Gengou Agar*
- This medium is specifically designed for the isolation of **Bordetella pertussis**, the causative agent of **whooping cough**.
- It contains potato extract, glycerol, and blood, which are necessary for the fastidious *Bordetella pertussis* to grow.
*Eaton's Agar*
- **Eaton's agar** is a specialized liquid or semi-solid medium used for the cultivation of **Mycoplasma pneumoniae**.
- *Mycoplasma pneumoniae* is a common cause of **atypical pneumonia** and lacks a cell wall, making it difficult to culture on standard media.
Bacillus species US Medical PG Question 3: A 30-year-old woman comes to the emergency department because of fever, watery diarrhea, and abdominal cramping for the past 24 hours. She recently went to an international food fair. Her temperature is 39°C (102.2°F). Physical examination shows increased bowel sounds. Stool cultures grow gram-positive, spore-forming, anaerobic rods that produce alpha toxin. The responsible organism also causes which of the following physical examination findings?
- A. Diffuse, flaccid bullae
- B. Subcutaneous crepitus (Correct Answer)
- C. Facial paralysis
- D. Rose spots
- E. Petechial rash
Bacillus species Explanation: ***Subcutaneous crepitus***
- The description of gram-positive, spore-forming, anaerobic rods producing alpha toxin is characteristic of *Clostridium perfringens*.
- This organism causes **two main clinical syndromes**: (1) **food poisoning** with diarrhea (as in this patient), and (2) **gas gangrene** (clostridial myonecrosis).
- **Gas gangrene** is characterized by muscle necrosis, gas production in tissues (leading to **crepitus** on palpation), and rapid tissue destruction.
*Diffuse, flaccid bullae*
- This finding is more commonly associated with **staphylococcal scalded skin syndrome (SSSS)** caused by *Staphylococcus aureus* exfoliative toxins.
- *Clostridium perfringens* infections typically lead to **gas formation** and tissue necrosis rather than superficial bullae.
*Facial paralysis*
- **Facial paralysis** is characteristic of *Clostridium botulinum* (botulism), which produces neurotoxins that block acetylcholine release.
- *Clostridium perfringens* does not produce neurotoxins that cause paralysis; its pathogenicity is due to **alpha toxin** (phospholipase C) causing tissue destruction.
*Rose spots*
- **Rose spots** are characteristic of **typhoid fever**, caused by *Salmonella Typhi*.
- They are faint, salmon-colored maculopapular lesions on the trunk that blanch with pressure.
*Petechial rash*
- A **petechial rash** is often seen in conditions like **meningococcemia** (*Neisseria meningitidis*), **Rocky Mountain spotted fever**, or bacterial **endocarditis** due to vascular damage.
- While *Clostridium perfringens* can cause severe sepsis, a petechial rash is not its classic presentation.
Bacillus species US Medical PG Question 4: A 50-year-old farmer presents to a physician with painless, black, severely swollen pustules on the left hand. Examination reveals extensive swelling around the wound. Microscopy reveals gram-positive bacilli with a bamboo stick appearance. Culture shows large, gray, non-hemolytic colonies with irregular borders. Which of the following is the most likely diagnosis?
- A. Anthrax (Correct Answer)
- B. Tularemia
- C. Brucellosis
- D. Erysipeloid
- E. Listeriosis
Bacillus species Explanation: ***Anthrax***
- The combination of **painless, black, severely swollen pustules** (eschar and edema) on the hand of a **farmer** is pathognomonic for **cutaneous anthrax**.
- **Gram-positive bacilli with a bamboo stick appearance** and **large, gray, non-hemolytic colonies with irregular borders** on culture are characteristic features of *Bacillus anthracis*.
*Tularemia*
- While tularemia can present with an **ulceroglandular lesion** at the site of inoculation, it is typically accompanied by **highly painful regional lymphadenopathy**.
- The causative agent, *Francisella tularensis*, is a **small, gram-negative coccobacillus**, not a large gram-positive bacillus.
*Brucellosis*
- This zoonotic infection is primarily associated with **fever, sweats, malaise**, and **arthralgia**, often linked to consumption of unpasteurized dairy or contact with infected animals.
- It does not present with characteristic skin lesions like the **black pustules** described, and **Brucella species** are **gram-negative coccobacilli**.
*Erysipeloid*
- Erysipeloid is a skin infection caused by *Erysipelothrix rhusiopathiae*, characterized by a **reddish-purple, elevated migratory lesion with sharply defined borders**, often on the hands or fingers.
- It does not produce **black pustules** or the specific microscopic and cultural features described for *Bacillus anthracis*.
*Listeriosis*
- Listeriosis, caused by *Listeria monocytogenes*, typically presents as **meningitis, sepsis**, or **gastroenteritis**, particularly in immunocompromised individuals, pregnant women, and neonates.
- While *Listeria* is a **gram-positive rod**, it does not cause the distinct skin lesions seen in the patient, nor does it form large, non-hemolytic colonies with irregular borders.
Bacillus species US Medical PG Question 5: A 55-year-old woman with type 2 diabetes mellitus is admitted to the hospital because of a 2-day history of fever, breathlessness, and cough productive of large quantities of green sputum. She drinks 8 beers daily. Her temperature is 39°C (102.2°F), pulse is 110/min, respirations are 28/min, and blood pressure is 100/60 mm Hg. Blood and sputum cultures grow gram-negative, catalase-positive, capsulated bacilli. Which of the following components of the causal organism is the most likely cause of this patient's hypotension?
- A. Poly-D-glutamate
- B. Teichoic acid
- C. Lipid A (Correct Answer)
- D. Lecithinase
- E. Lipooligosaccharide
Bacillus species Explanation: ***Lipid A***
- The patient's presentation with **fever**, **hypotension**, and gram-negative bacterial infection suggests **sepsis** and **septic shock**.
- **Lipid A** is the endotoxic component of **lipopolysaccharide (LPS)** found in the outer membrane of gram-negative bacteria, directly responsible for mediating the systemic inflammatory response and hypotension in septic shock.
- Lipid A is recognized by **TLR4** on immune cells, triggering the release of **TNF-α**, **IL-1**, and other cytokines that cause vasodilation, increased vascular permeability, and shock.
*Poly-D-glutamate*
- This is a component of the **capsule of *Bacillus anthracis***, which is a gram-positive rod, not the gram-negative, catalase-positive, capsulated organism described.
- While it contributes to virulence by inhibiting phagocytosis, it does not directly cause the profound hemodynamic changes seen in sepsis from gram-negative bacteria.
*Teichoic acid*
- **Teichoic acids** are components of the **cell wall of gram-positive bacteria** (e.g., *Staphylococcus*, *Streptococcus*) and are not found in gram-negative bacteria.
- While they can stimulate an inflammatory response, they are not the primary cause of septic shock in gram-negative infections.
*Lecithinase*
- **Lecithinase** (also known as **alpha-toxin** or **phospholipase C**) is an **exotoxin** produced by various bacteria, notably *Clostridium perfringens*.
- While it can cause tissue damage and contribute to virulence, it is not an integral structural component of the bacterial cell wall responsible for generalized vasodilation and hypotension in gram-negative sepsis.
*Lipooligosaccharide*
- **Lipooligosaccharide (LOS)** is a structural variant of LPS found in certain gram-negative bacteria (particularly **Neisseriaceae** like *N. meningitidis* and *N. gonorrhoeae*), consisting of **Lipid A** plus a short oligosaccharide core without the O-antigen repeats.
- While **Lipid A within LOS** is endotoxic, the question asks for the specific **component** causing hypotension, which is **Lipid A itself**, not the larger LOS molecule.
- The likely pathogen here (*Klebsiella pneumoniae* given clinical context) contains **LPS**, not LOS, making Lipid A the most precise answer.
Bacillus species US Medical PG Question 6: A 35-year-old patient with no significant past medical history arrives to the ED with abdominal cramps, nausea, and vomiting. He has had no recent travel or chemical exposures; however, three other members of his family also arrived concurrently to the ED with abdominal cramps, nausea, and vomiting. When asked about their recent activities, they recall that they had shared a lunch of leftover fried rice and soft boiled eggs about 5 hours earlier. The patients are otherwise afebrile and deny any history of diarrhea. Which of the following toxins is the most likely to have caused these symptoms?
- A. Shiga toxin
- B. Cereulide (Correct Answer)
- C. Endotoxin
- D. Exotoxin A
- E. Toxin B
Bacillus species Explanation: ***Cereulide***
- The rapid onset (within 5 hours) of gastrointestinal symptoms (nausea, vomiting, abdominal cramps) after consuming **fried rice** and **boiled eggs** is characteristic of intoxication by **cereulide**.
- This preformed toxin is produced by *Bacillus cereus* in improperly stored starchy foods like rice, leading to emetic-type food poisoning.
*Shiga toxin*
- **Shiga toxin** is produced by *Shigella dysenteriae* and Shiga toxin-producing *E. coli* (STEC), typically causing **bloody diarrhea** and **hemolytic uremic syndrome (HUS)**, which are not present here.
- The incubation period for Shiga toxin-mediated illness is usually longer, ranging from 1 to 8 days, making a rapid onset of symptoms unlikely.
*Endotoxin*
- **Endotoxin** (lipopolysaccharide or LPS) is a component of the outer membrane of **Gram-negative bacteria** and causes systemic symptoms like fever, shock, and organ dysfunction when released during bacterial lysis.
- While it can cause some gastrointestinal effects, the rapid onset of isolated emetic symptoms in a food poisoning cluster is not typical for endotoxin as the primary cause.
*Exotoxin A*
- **Exotoxin A** is a virulence factor produced by *Pseudomonas aeruginosa* and is associated with severe infections in immunocompromised patients, not typically foodborne illness.
- Its mechanism of action involves inhibiting protein synthesis, leading to tissue damage in specific infections, not acute emetic food poisoning.
*Toxin B*
- **Toxin B** is produced by *Clostridioides difficile* and is a major cause of **antibiotic-associated colitis** and **pseudomembranous colitis**, characterized by diarrhea and abdominal pain.
- The patient's presentation of acute onset nausea, vomiting, and abdominal cramps without diarrhea and no history of antibiotic use does not align with *C. difficile* infection.
Bacillus species US Medical PG Question 7: A 73-year-old man is brought to the emergency department because of fever, headaches, and confusion for the past 24 hours. Three years ago, he underwent heart transplantation because of congestive heart failure. His temperature is 38.1°C (100.5°F). He is oriented only to person. Physical examination shows nuchal rigidity. A cerebrospinal fluid culture on blood agar grows colonies of a gram-positive bacillus surrounded by a narrow transparent rim. Administration of which of the following antibiotics is most likely to be effective in the treatment of this patient's condition?
- A. Ampicillin (Correct Answer)
- B. Doxycycline
- C. Chloramphenicol
- D. Erythromycin
- E. Vancomycin
Bacillus species Explanation: ***Ampicillin***
- This patient presents with symptoms of **meningitis** (fever, headache, confusion, nuchal rigidity) and is immunocompromised due to a **heart transplant**. The CSF culture revealing a **gram-positive bacillus** with a narrow transparent rim on blood agar strongly suggests **Listeria monocytogenes**.
- **Ampicillin** is the first-line treatment for **Listeria meningitis**, as it is bactericidal and effectively penetrates the central nervous system.
*Doxycycline*
- Doxycycline is a **tetracycline antibiotic** that is effective against a broad range of bacteria, including some gram-positive organisms, but it is not the drug of choice for **Listeria meningitis**.
- It is primarily **bacteriostatic**, and for serious infections like bacterial meningitis, a bactericidal agent is preferred, especially in immunocompromised patients.
*Chloramphenicol*
- Chloramphenicol is a broad-spectrum antibiotic that can be effective against some gram-positive bacteria, but its use is limited due to significant side effects like **bone marrow suppression** (aplastic anemia).
- It is not considered a first-line agent for **Listeria meningitis** due to the availability of safer and equally effective alternatives like ampicillin.
*Erythromycin*
- Erythromycin is a **macrolide antibiotic** primarily used for respiratory tract infections and certain skin and soft tissue infections.
- While it has activity against some gram-positive bacteria, it is generally **not effective against Listeria monocytogenes** and does not adequately penetrate the central nervous system for meningitis treatment.
*Vancomycin*
- Vancomycin is a glycopeptide antibiotic primarily used for serious infections caused by **methicillin-resistant Staphylococcus aureus (MRSA)** and other resistant gram-positive bacteria.
- Although it is effective against many gram-positive organisms, **Listeria monocytogenes is inherently resistant to vancomycin**, making it an ineffective treatment choice for this patient's condition.
Bacillus species US Medical PG Question 8: A 71-year-old woman presents with high-grade fever and chills, difficulty breathing, and a productive cough with rust-colored sputum. She complains of a sharp left-sided chest pain. Physical examination reveals increased fremitus, dullness to percussion, and bronchial breath sounds on the lower left side. A chest X-ray shows left lower lobe consolidation. The offending organism that was cultured from the sputum was catalase-negative and had a positive Quellung reaction. The organism will show which gram stain results?
- A. Gram-negative diplococci
- B. Cannot be seen with gram staining since the organism lacks a cell wall
- C. Gram-positive cocci in clusters
- D. Gram-negative rod
- E. Gram-positive diplococci (Correct Answer)
Bacillus species Explanation: ***Gram-positive diplococci***
- The clinical presentation (high fever, chills, productive cough with **rust-colored sputum**, sharp chest pain, signs of **consolidation**) is classic for **pneumococcal pneumonia**.
- The organism responsible for pneumococcal pneumonia, *Streptococcus pneumoniae*, is a **Gram-positive, catalase-negative diplococcus** that exhibits a **positive Quellung reaction** due to its polysaccharide capsule.
*Gram-negative diplococci*
- This describes organisms such as **Neisseria meningitidis** or **Neisseria gonorrhoeae**, which cause meningitis or gonorrhea, respectively, not typical pneumonia.
- While *Moraxella catarrhalis* is a Gram-negative diplococcus that can cause respiratory infections, it typically causes otitis media or sinusitis and less commonly severe pneumonia with rust-colored sputum.
*Cannot be seen with gram staining since the organism lacks a cell wall*
- This description typically refers to **Mycoplasma pneumoniae**, which causes **atypical pneumonia** and lacks a cell wall, rendering it unstainable by Gram stain.
- Mycoplasma pneumonia usually presents with a more indolent course, a non-productive cough, and rarely causes rust-colored sputum or lobar consolidation seen on X-ray.
*Gram-positive cocci in clusters*
- This morphology is characteristic of **staphylococci**, such as *Staphylococcus aureus*, which can cause pneumonia, often in immunocompromised individuals or as a complication of influenza.
- However, *Staphylococcus aureus* is **catalase-positive**, and its pneumonia presentation can be more fulminant, often leading to abscess formation, differing from the typical presentation of pneumococcal pneumonia.
*Gram-negative rod*
- This morphology is characteristic of various bacteria including **Klebsiella pneumoniae**, **Pseudomonas aeruginosa**, or **Haemophilus influenzae**.
- **Klebsiella pneumoniae** can cause severe pneumonia with **currant jelly sputum** but is a Gram-negative rod and would not exhibit a Quellung reaction in the same manner as *S. pneumoniae*.
Bacillus species US Medical PG Question 9: A 29-year-old woman comes to the military physician because of a 2-day history of fever, joint pain, dry cough, chest pain, and a painful red rash on her lower legs. Two weeks ago, she returned from military training in Southern California. She appears ill. Her temperature is 39°C (102.1°F). Physical examination shows diffuse inspiratory crackles over all lung fields and multiple tender erythematous nodules over the anterior aspect of both legs. A biopsy specimen of this patient's lungs is most likely to show which of the following?
- A. Septate hyphae with acute-angle branching
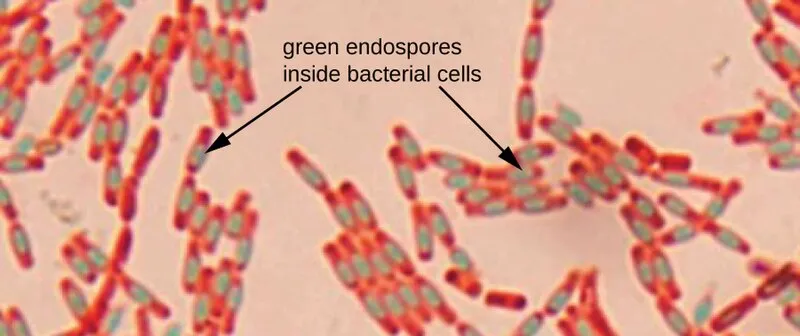
- B. Spherules filled with endospores (Correct Answer)
- C. Broad-based budding yeast
- D. Encapsulated yeast with narrow-based budding
- E. Oval, budding yeast with pseudohyphae
Bacillus species Explanation: **Spherules filled with endospores**
- The patient's symptoms (fever, joint pain, dry cough, chest pain, erythema nodosum on legs) combined with her travel history to **Southern California** are highly suggestive of **Coccidioidomycosis** ("Valley Fever").
- A biopsy of affected lung tissue in coccidioidomycosis typically reveals **spherules** (thick-walled structures) containing numerous **endospores**, which are characteristic of the tissue phase of *Coccidioides immitis/posadasii*.
*Septate hyphae with acute-angle branching*
- This morphology is characteristic of **Aspergillus** species, which can cause opportunistic infections, especially in immunocompromised individuals.
- While it can cause lung infections, the clinical presentation and geographic exposure do not point towards aspergillosis as the most likely diagnosis.
*Broad-based budding yeast*
- This describes the characteristic morphology of *Blastomyces dermatitidis*, the causative agent of **Blastomycosis**.
- **Blastomycosis** is typically found in the Great Lakes region, Ohio, Mississippi River valleys, and southeastern United States, not Southern California.
*Encapsulated yeast with narrow-based budding*
- This describes **Cryptococcus neoformans**, which appears as an encapsulated yeast with narrow-based budding in tissue.
- While it can cause pulmonary disease, the classic presentation (erythema nodosum, acute illness after Southern California exposure) is not consistent with **cryptococcosis**, which typically presents subacutely in immunocompromised patients.
*Oval, budding yeast with pseudohyphae*
- This morphology is characteristic of *Candida albicans*, which commonly causes mucocutaneous infections and can cause systemic candidiasis, particularly in immunocompromised patients.
- The clinical picture of a healthy young woman with exposure in Southern California does not fit with a typical **Candida** infection.
Bacillus species US Medical PG Question 10: An 11-year-old boy presents with a sore throat, fever, chills, and difficulty swallowing for the past 3 days. The patient’s mother says that last night he was short of breath and had a headache. Past medical history is unremarkable. The patient has not been vaccinated as his mother thinks it is "unnecessary". His temperature is 38.3°C (101.0°F), blood pressure is 120/70 mm Hg, pulse is 110/min, and respiratory rate is 18/min. On physical examination, the patient is ill-appearing and dehydrated. A grayish-white membrane and pharyngeal erythema are present in the oropharynx. Significant cervical lymphadenopathy is also present. A throat swab is taken and gram staining shows gram-positive club-shaped bacilli along with few neutrophils. Which of the following would most likely be the result of the bacterial culture of the throat swab in this patient?
- A. Hemolytic black colonies on blood agar
- B. Metallic green colonies on eosin-methylene blue agar
- C. Greyish-white colonies on Thayer-Martin agar
- D. Small black colonies on tellurite agar (Correct Answer)
- E. Creamy white colonies on Loeffler's serum
Bacillus species Explanation: ***Small black colonies on tellurite agar***
- The clinical presentation, including **sore throat**, **fever**, **grayish-white membrane** in the oropharynx, and **cervical lymphadenopathy** in an **unvaccinated child**, strongly suggests **diphtheria** caused by *Corynebacterium diphtheriae*.
- *Corynebacterium diphtheriae* produces **small gray-black colonies** on **potassium tellurite agar** (e.g., Blood Tellurite Agar or Tinsdale agar) due to the reduction of tellurite to elemental tellurium within the bacterial cells.
- This is the **definitive culture characteristic** used for laboratory diagnosis of diphtheria.
*Hemolytic black colonies on blood agar*
- **Hemolytic black colonies** are not characteristic of *Corynebacterium diphtheriae*.
- *C. diphtheriae* may show minimal or no hemolysis on blood agar, and does not produce black colonies on this medium.
- Black colonies with hemolysis might suggest other organisms but are not typical for diphtheria diagnosis.
*Metallic green colonies on eosin-methylene blue agar*
- **Metallic green colonies** on **eosin-methylene blue (EMB) agar** are characteristic of **lactose-fermenting bacteria**, particularly *Escherichia coli*.
- This finding is associated with **Gram-negative enteric bacteria**, not the Gram-positive club-shaped bacilli seen in this patient.
*Greyish-white colonies on Thayer-Martin agar*
- **Greyish-white colonies** on **Thayer-Martin agar** are typically seen with **fastidious Gram-negative diplococci**, such as *Neisseria gonorrhoeae* or *Neisseria meningitidis*.
- This medium is selective for *Neisseria* species and would not be used for isolating *Corynebacterium diphtheriae*, which is a Gram-positive rod.
*Creamy white colonies on Loeffler's serum*
- **Loeffler's serum medium** is indeed used to enhance the growth of *Corynebacterium diphtheriae*, and the organism produces **creamy white to grayish colonies** on this medium.
- However, Loeffler's medium is primarily used to demonstrate the characteristic **metachromatic granules** (Babes-Ernst bodies) on microscopy, not for definitive culture identification.
- **Tellurite agar**, not Loeffler's medium, is the **gold standard** for culture diagnosis because the black colony appearance is pathognomonic for *C. diphtheriae*.
More Bacillus species US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.