Actinomyces and Nocardia US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Actinomyces and Nocardia. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Actinomyces and Nocardia US Medical PG Question 1: A medical technician is trying to isolate a pathogen from the sputum sample of a patient. The sample is heat fixed to a slide then covered with carbol fuchsin stain and heated again. After washing off the stain with clean water, the slide is covered with 1% sulfuric acid for decolorization. The sample is rinsed again and stained with methylene blue. Microscopic examination shows numerous red, branching filamentous organisms. Which of the following is the most likely isolated pathogen?
- A. Cryptococcus neoformans
- B. Tropheryma whipplei
- C. Nocardia asteroides (Correct Answer)
- D. Rickettsia rickettsii
- E. Staphylococcus aureus
Actinomyces and Nocardia Explanation: ***Nocardia asteroides***
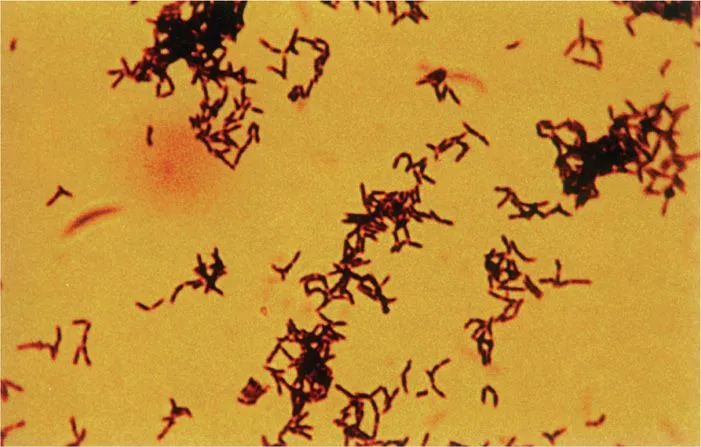
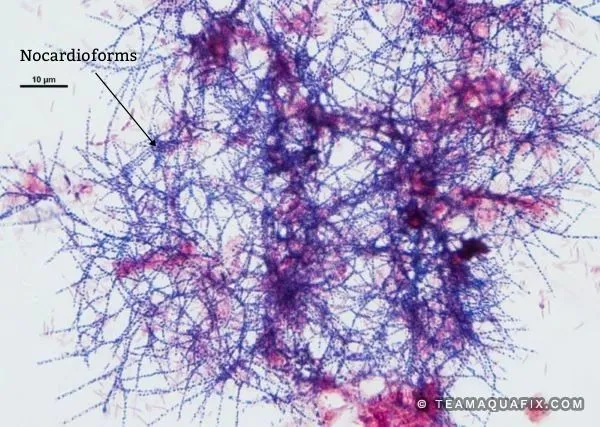
- The described staining procedure is a **modified acid-fast stain**, indicated by the use of **carbol fuchsin**, heating, and decolorization with **weak acid (1% sulfuric acid)**, followed by a counterstain with methylene blue.
- **Nocardia species** are **weakly acid-fast bacteria** that resist decolorization with weak acids (1-3% sulfuric acid), appearing as **red, branching filamentous organisms** under this staining method.
- The **modified acid-fast stain** uses weaker decolorizing agents compared to the standard Ziehl-Neelsen stain, making it suitable for detecting weakly acid-fast organisms like Nocardia.
- Nocardia are aerobic actinomycetes commonly found in soil and can cause pulmonary infections, especially in immunocompromised patients.
*Cryptococcus neoformans*
- This is a **yeast** that is typically identified using an **India ink stain** to visualize its polysaccharide capsule, or through fungal stains like Gomori methenamine silver (GMS).
- It would not appear as acid-fast red branching filaments with the described technique.
*Tropheryma whipplei*
- This bacterium is typically identified by **periodic acid-Schiff (PAS) stain** in tissue biopsies, which highlights its cell wall glycoproteins (appears magenta).
- It is not acid-fast and would not retain the carbol fuchsin after acid decolorization.
*Rickettsia rickettsii*
- This is an **obligate intracellular bacterium** that is difficult to culture and is often diagnosed by **serological tests** or **immunohistochemistry** on skin biopsy specimens.
- It is not acid-fast and would not be detected by this staining technique.
*Staphylococcus aureus*
- This is a **Gram-positive coccus** that would be stained **purple** by a Gram stain as it retains crystal violet.
- It is not acid-fast and would be completely decolorized by sulfuric acid in the described procedure, appearing blue (counterstain color) rather than red.
Actinomyces and Nocardia US Medical PG Question 2: An investigator is studying the growth of an organism in different media. The organism is inoculated on a petri dish that contains heated sheep blood, vancomycin, nystatin, trimethoprim, and colistin. The resulting growth medium is incubated at 37°C. Numerous small, white colonies are seen after incubation for 48 hours. This organism is most likely to cause which of the following conditions?
- A. Pontiac fever
- B. Pseudomembranous colitis
- C. Hemolytic uremic syndrome
- D. Oral thrush
- E. Gonorrhea (Correct Answer)
Actinomyces and Nocardia Explanation: ***Gonorrhea***
- The growth medium described is **Thayer-Martin agar**, a selective medium containing **heated sheep blood** (supplies NAD+), **vancomycin** (inhibits Gram-positives), **colistin** (inhibits Gram-negatives), **nystatin** (inhibits fungi), and **trimethoprim** (inhibits Proteus). This medium is specifically designed for the isolation of *Neisseria gonorrhoeae* from polymicrobial samples.
- *Neisseria gonorrhoeae* typically grows as **small, translucent-to-white colonies** on selective media like Thayer-Martin agar, and incubation at 37°C in CO2 (not explicitly mentioned but often required) for 24-48 hours yields visible growth, causing **gonorrhea**.
*Pontiac fever*
- Pontiac fever is a mild, self-limiting form of **legionellosis**, caused by *Legionella pneumophila*.
- *Legionella* requires a specialized medium such as **buffered charcoal yeast extract (BCYE) agar** for growth, not Thayer-Martin agar.
*Pseudomembranous colitis*
- This condition is caused by **toxin-producing *Clostridioides difficile***, often after antibiotic use.
- *C. difficile* is an obligate anaerobe and requires **anaerobic conditions** and specific selective media (e.g., CCFA agar) for isolation, not Thayer-Martin agar under aerobic conditions.
*Hemolytic uremic syndrome*
- Hemolytic uremic syndrome (HUS) is often caused by **Shiga toxin-producing *Escherichia coli* (STEC)**, particularly O157:H7.
- STEC can be isolated on media like **sorbitol MacConkey agar (SMAC)**, where O157:H7 appears as non-sorbitol fermenting colonies, distinct from the growth seen on Thayer-Martin.
*Oral thrush*
- Oral thrush is caused by *Candida albicans*, a yeast.
- *Candida* would be inhibited by **nystatin** in the Thayer-Martin medium, which is an antifungal agent.
Actinomyces and Nocardia US Medical PG Question 3: Blood cultures are sent to the laboratory and empiric treatment with intravenous vancomycin is started. Blood cultures grow gram-negative bacilli identified as Cardiobacterium hominis. Which of the following is the most appropriate next step in management?
- A. Switch to intravenous gentamicin
- B. Switch to intravenous ampicillin
- C. Switch to intravenous ceftriaxone (Correct Answer)
- D. Switch to intravenous cefazolin
- E. Add intravenous rifampin
Actinomyces and Nocardia Explanation: ***Switch to intravenous ceftriaxone***
- **Cardiobacterium hominis** is part of the **HACEK group** of bacteria, which are known for causing **endocarditis**.
- These organisms are typically susceptible to **beta-lactam antibiotics**, with **third-generation cephalosporins** like ceftriaxone being the drug of choice due to their excellent activity and good penetration.
*Switch to intravenous gentamicin*
- While **aminoglycosides** like gentamicin can be used in combination regimens for serious infections, they are generally **not monotherapy** for HACEK endocarditis and are associated with **nephrotoxicity** and **ototoxicity**.
- The primary treatment for HACEK endocarditis is a **beta-lactam antibiotic**, not an aminoglycoside alone.
*Switch to intravenous ampicillin*
- **Ampicillin** is a beta-lactam, but it may not consistently provide optimal coverage for all HACEK organisms, and some strains may have reduced susceptibility.
- **Third-generation cephalosporins** are preferred due to their broader and more consistent activity against this group.
*Switch to intravenous cefazolin*
- **Cefazolin** is a first-generation cephalosporin and typically has **limited activity** against gram-negative bacilli, especially those like Cardiobacterium hominis which require broader-spectrum beta-lactams.
- Its spectrum of activity is primarily against **gram-positive bacteria** and some **gram-negative cocci**.
*Add intravenous rifampin*
- **Rifampin** is primarily used for **mycobacterial infections** and in combination regimens for specific bacterial infections (e.g., bone and joint infections, prosthetic device infections) often due to resistant staphylococci.
- It is **not a first-line agent** for Cardiobacterium hominis infections and there's no indication for its use here with an organism susceptible to ceftriaxone.
Actinomyces and Nocardia US Medical PG Question 4: A 28-year-old man presents with a draining abscess on his left jaw. The patient states that he had a “bad tooth” a few weeks ago which has progressed to his current condition. His vital signs include: blood pressure 110/80 mm Hg, heart rate 85/min, and temperature 37.9°C (100.3°F). On physical examination, the patient has a 4 cm abscess on the left maxillary line that is draining a granulous, purulent material. Which of the following is the most likely causative organism of this abscess?
- A. Gram-positive cocci in clusters
- B. Gram-positive cocci in chains
- C. Enveloped, double stranded DNA virus
- D. Gram-positive, branching rod (Correct Answer)
- E. Aerobic gram-negative rod
Actinomyces and Nocardia Explanation: ***Gram-positive, branching rod***
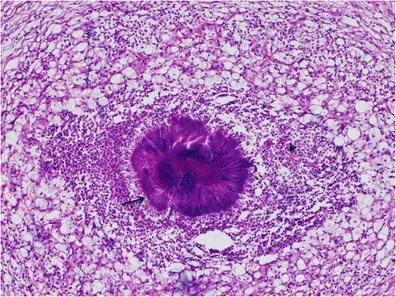
- The description of a **draining abscess** on the jaw originating from a "bad tooth," with **granulous, purulent material**, is highly suggestive of **actinomycosis**.
- *Actinomyces israelii*, the most common causative agent, is a **Gram-positive, branching rod** that forms characteristic **sulfur granules** in pus, which are macroscopic colonies of bacteria and calcium phosphate.
*Gram-positive cocci in clusters*
- This description typically refers to **Staphylococcus aureus**, which causes abscesses, but they are usually **acute, painful, and rapidly developing**, without the characteristic "sulfur granules" seen in actinomycosis.
- While *S. aureus* can certainly infect the oral cavity, the **chronic nature** and **"granulous" discharge** point away from a typical staphylococcal infection.
*Gram-positive cocci in chains*
- This typically describes **Streptococcus species**, which are common oral flora and can cause dental infections and cellulitis.
- However, they do not typically form the **granulous, draining abscesses** or **sulfur granules** associated with actinomycosis.
*Enveloped, double stranded DNA virus*
- This category includes viruses such as herpesviruses or poxviruses; viruses do not cause **bacterial abscesses** with purulent, granulous material.
- Viral infections present with different clinical manifestations, such as **vesicles, ulcers**, or systemic disease, not a chronic draining abscess.
*Aerobic gram-negative rod*
- While some **aerobic Gram-negative rods** (e.g., *Pseudomonas*, *E. coli*) can cause abscesses, especially in immunocompromised individuals or hospital settings, they are less common causes of **odontogenic abscesses** in healthy patients.
- These bacteria do not produce the **sulfur granules** characteristic of actinomycosis.
Actinomyces and Nocardia US Medical PG Question 5: A 50-year-old HIV-positive male presents to the ER with a two-day history of fever and hemoptysis. Chest radiograph shows a fibrocavitary lesion in the right middle lobe. Biopsy of the afflicted area demonstrates septate hyphae that branch at acute angles. Which of the following is the most likely causal organism?
- A. Mycobacterium tuberculosis
- B. Pneumocystis jirovecii
- C. Aspergillus fumigatus (Correct Answer)
- D. Candida albicans
- E. Mucor species
Actinomyces and Nocardia Explanation: ***Aspergillus fumigatus***
- The combination of **fever**, **hemoptysis**, a **fibrocavitary lesion** in an **HIV-positive** patient, and the presence of **septate hyphae branching at acute angles** on biopsy are classic findings for invasive **aspergillosis**.
- **Aspergillus** specifically targets individuals with compromised immune systems, and the pathological description of the hyphae is highly characteristic of this fungus.
*Mycobacterium tuberculosis*
- While **Mycobacterium tuberculosis** can cause **fever**, **hemoptysis**, and **cavitary lesions** in HIV-positive patients, the microscopic description of **septate hyphae branching at acute angles** is not consistent with bacterial infection.
- Tuberculosis is characterized by **acid-fast bacilli** and granulomatous inflammation, not fungal hyphae.
*Mucor species*
- **Mucor** (along with Rhizopus) causes **mucormycosis**, an invasive fungal infection that can affect immunocompromised patients and present with pulmonary involvement and cavitary lesions.
- However, mucormycosis is characterized by **non-septate (aseptate) hyphae branching at right (90-degree) angles**, not septate hyphae at acute angles, making it distinguishable from Aspergillus.
*Pneumocystis jirovecii*
- **Pneumocystis jirovecii** is a common cause of pneumonia in HIV-positive patients, typically presenting as **diffuse interstitial infiltrates** rather than cavitary lesions.
- Microscopic examination would reveal **cysts** and **trophozoites**, not septate hyphae, making it inconsistent with the biopsy findings.
*Candida albicans*
- While **Candida albicans** can cause infections in immunocompromised individuals, it typically presents as **oral thrush**, esophagitis, or disseminated candidiasis.
- Pulmonary involvement is less common and usually manifests as **pneumonitis** rather than cavitary lesions, and its hyphae are typically **pseudohyphae** or budding yeasts, not septate hyphae branching at acute angles.
Actinomyces and Nocardia US Medical PG Question 6: A 15-year-old boy presents with his father to the urgent care department with a 5-day history of frequent diarrhea, occasionally mixed with streaks of blood. Stool cultures are pending, but preliminary stool samples demonstrate fecal leukocytes and erythrocytes. The patient's vital signs are within normal limits, and he is started on outpatient therapy for presumed Shigella infection. Which of the following was the young man most likely started on?
- A. Oral vancomycin
- B. Oral erythromycin
- C. Oral metronidazole
- D. An oral quinolone
- E. Oral trimethoprim-sulfamethoxazole (TMP-SMX) (Correct Answer)
Actinomyces and Nocardia Explanation: **Oral trimethoprim-sulfamethoxazole (TMP-SMX)**
- **TMP-SMX** is a traditional first-line treatment for **Shigella infection** in settings where susceptibility is expected or confirmed.
- The patient's presentation with **bloody diarrhea**, **fecal leukocytes**, and **erythrocytes** is classic for **Shigella dysentery**.
- While **resistance rates vary by region**, TMP-SMX remains an appropriate choice when local susceptibility patterns support its use.
- It is cost-effective, well-tolerated, and appropriate for outpatient management of uncomplicated cases.
*Oral vancomycin*
- Vancomycin is specifically used for **Clostridioides difficile infection** and does not treat Shigella.
- It has **poor oral absorption** and no activity against Gram-negative enteric pathogens like Shigella.
*Oral erythromycin*
- Erythromycin is primarily effective against **Campylobacter jejuni** and respiratory pathogens.
- It has **limited activity against Shigella** and resistance rates are high, making it an inappropriate choice.
*Oral metronidazole*
- Metronidazole treats **anaerobic bacteria** and protozoal infections (*Giardia*, *Entamoeba histolytica*).
- It has **no significant activity against Shigella**, a facultative anaerobic Gram-negative bacillus.
*An oral quinolone*
- **Fluoroquinolones** (e.g., ciprofloxacin) are highly effective against Shigella and often used as first-line therapy, particularly in areas with high TMP-SMX resistance.
- They are increasingly preferred in current guidelines due to rising resistance to TMP-SMX.
- However, in the context of empiric outpatient treatment where susceptibility is presumed, **TMP-SMX** may still be chosen initially as a narrower-spectrum, cost-effective option, with fluoroquinolones reserved based on culture results or treatment failure.
Actinomyces and Nocardia US Medical PG Question 7: A 20-year-old woman presents for a follow-up visit with her physician. She has a history of cystic fibrosis and is currently under treatment. She has recently been struggling with recurrent bouts of cough and foul-smelling, mucopurulent sputum over the past year. Each episode lasts for about a week or so and then subsides. She does not have a fever or chills during these episodes. She has been hospitalized several times for pneumonia as a child and continues to struggle with diarrhea. Physically she appears to be underweight and in distress. Auscultation reveals reduced breath sounds on the lower lung fields with prominent rhonchi. Which of the following infectious agents is most likely associated with the recurrent symptoms this patient is experiencing?
- A. Mycobacterium avium
- B. Pseudomonas (Correct Answer)
- C. Histoplasma
- D. Pneumococcus
- E. Listeria
Actinomyces and Nocardia Explanation: ***Pseudomonas***
- **Pseudomonas aeruginosa** is a common and opportunistic pathogen in patients with **cystic fibrosis** due to altered mucus secretion and impaired mucociliary clearance.
- Recurrent cough, foul-smelling, and **mucopurulent sputum** are classic symptoms of **Pseudomonas** lung infections in CF patients, often leading to chronic colonization and bronchiectasis.
*Mycobacterium avium*
- While *Mycobacterium avium complex* (MAC) can infect patients with cystic fibrosis, it typically causes a **more indolent and chronic lung disease** rather than recurrent, self-limiting bouts of cough and sputum.
- MAC infections are often associated with **nodular or cavitary lesions** on imaging and may require prolonged multidrug therapy.
*Histoplasmosis*
- **Histoplasmosis** is a fungal infection endemic to certain geographic regions (e.g., Ohio and Mississippi River valleys) and is acquired by inhaling spores.
- It's **not a typical or recurrent pathogen** in cystic fibrosis patients in the way bacterial infections are, and its presentation often includes fever, chills, and disseminated disease in immunocompromised individuals.
*Pneumococcus*
- *Streptococcus pneumoniae* (**Pneumococcus**) is a common cause of **acute bacterial pneumonia** in the general population, including young children.
- While CF patients can get pneumococcal infections, the pattern of **recurrent bouts of foul-smelling mucopurulent sputum** without fever and the chronic nature of the lung disease point away from typical acute pneumococcal infection and more towards a chronic colonizer like *Pseudomonas*.
*Listeria*
- *Listeria monocytogenes* is primarily a cause of **foodborne illness**, leading to gastroenteritis, meningitis, or sepsis, particularly in immunocompromised individuals, pregnant women, and neonates.
- It is **not a common respiratory pathogen**, and its presentation does not align with the described recurrent pulmonary symptoms in a cystic fibrosis patient.
Actinomyces and Nocardia US Medical PG Question 8: A 54-year-old woman comes to the physician because of lower back pain, night sweats, and a 5-kg (11-lb) weight loss during the past 4 weeks. She has rheumatoid arthritis treated with adalimumab. Her temperature is 38°C (100.4°F). Physical examination shows tenderness over the T10 and L1 spinous processes. Passive extension of the right hip causes pain in the right lower quadrant. The patient's symptoms are most likely caused by an organism with which of the following virulence factors?
- A. Proteins that bind to the Fc region of immunoglobulin G
- B. Protease that cleaves immunoglobulin A
- C. Polysaccharide capsule that prevents phagocytosis
- D. Surface glycolipids that prevent phagolysosome fusion (Correct Answer)
- E. Polypeptides that inactivate elongation factor 2
Actinomyces and Nocardia Explanation: ***Surface glycolipids that prevent phagolysosome fusion***
- The patient's symptoms (low back pain, night sweats, weight loss, fever, spinal tenderness, and hip pain) in a patient on **adalimumab** (a TNF-alpha inhibitor) suggest **disseminated tuberculosis** (Pott disease).
- *Mycobacterium tuberculosis* uses **mycolic acids** and other surface glycolipids to prevent phagolysosome fusion, allowing it to survive and replicate within macrophages.
*Proteins that bind to the Fc region of immunoglobulin G*
- This virulence factor is characteristic of bacteria like *Staphylococcus aureus* (Protein A) and *Streptococcus pyogenes* (Protein G), which is not consistent with the clinical picture.
- These proteins interfere with opsonization and antibody-mediated immunity, but are not the primary mechanism of *Mycobacterium tuberculosis* survival within macrophages.
*Protease that cleaves immunoglobulin A*
- **IgA protease** is a virulence factor for bacteria such as *Neisseria gonorrhoeae*, *Neisseria meningitidis*, and *Streptococcus pneumoniae*, which colonize mucosal surfaces.
- This mechanism helps these bacteria evade mucosal immunity, but it is not relevant to the pathogenesis of tuberculosis.
*Polysaccharide capsule that prevents phagocytosis*
- A polysaccharide capsule is a major virulence factor for many encapsulated bacteria (e.g., *Streptococcus pneumoniae*, *Haemophilus influenzae*, *Neisseria meningitidis*) that helps them evade phagocytosis.
- However, *Mycobacterium tuberculosis* is not primarily characterized by a polysaccharide capsule for immune evasion; its internal survival within macrophages is more critical.
*Polypeptides that inactivate elongation factor 2*
- Toxins that inactivate **elongation factor 2** are associated with *Corynebacterium diphtheriae* (**diphtheria toxin**) and *Pseudomonas aeruginosa* (**exotoxin A**), leading to inhibition of protein synthesis.
- This mechanism is not involved in the pathogenesis of *Mycobacterium tuberculosis* infection or its ability to cause disseminated disease.
Actinomyces and Nocardia US Medical PG Question 9: A 35-year-old man from Thailand presents with low-grade fever, chronic cough, and night sweats for 3 months. He describes the cough as productive and producing white sputum that is sometimes streaked with blood. He also says he has lost 10 lb in the last 3 months. Past medical history is unremarkable. The patient denies any smoking history, alcohol, or recreational drug use. The vital signs include blood pressure 115/75 mm Hg, heart rate 120/min, respiratory rate 20/min, and temperature 36.6℃ (97.8℉). On physical examination, the patient is ill-looking and thin with no pallor or jaundice. Cardiopulmonary auscultation reveals some fine crackles in the right upper lobe. A chest radiograph reveals a right upper lobe homogeneous density. Which of the following tests would be most helpful in making a definitive diagnosis of active infection in this patient?
- A. PPD test
- B. Silver stain
- C. Ziehl-Neelsen stain (Correct Answer)
- D. Gram stain
- E. Interferon-gamma assay
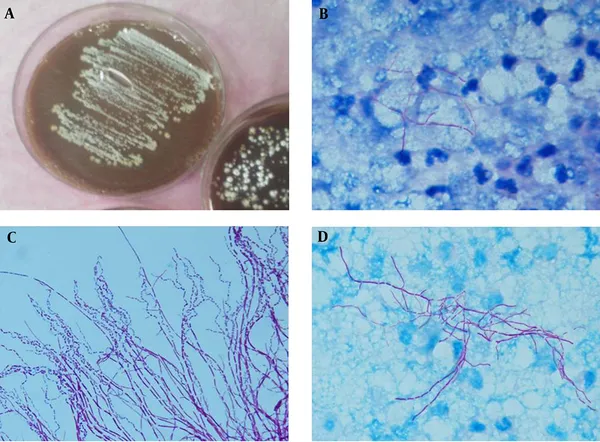
Actinomyces and Nocardia Explanation: ***Ziehl-Neelsen stain***
- The patient's symptoms (low-grade fever, chronic cough with white/bloody sputum, night sweats, weight loss) and chest X-ray findings (right upper lobe homogeneous density) are highly suggestive of **active tuberculosis (TB)**, especially given his origin from Thailand (a country with a high TB burden).
- The **Ziehl-Neelsen stain** (acid-fast stain) directly visualizes **acid-fast bacilli** (AFB) like *Mycobacterium tuberculosis* in sputum, providing a rapid and definitive diagnosis of active infection.
*PPD test*
- A **PPD test** (tuberculin skin test) indicates exposure to *Mycobacterium tuberculosis* but cannot differentiate between **latent TB infection** and **active disease**.
- A positive PPD can occur in individuals previously exposed or vaccinated with BCG, offering no direct evidence of current active infection.
*Silver stain*
- **Silver stain** (e.g., Gomori methenamine silver) is used to identify fungal organisms like *Pneumocystis jirovecii* or certain bacteria, such as *Legionella pneumophila*.
- It is not the primary stain for diagnosing tuberculosis, which requires detection of acid-fast bacilli.
*Gram stain*
- **Gram stain** is used to classify bacteria based on their cell wall properties (Gram-positive or Gram-negative).
- *Mycobacterium tuberculosis* has a unique **mycolic acid-rich cell wall** that makes it resistant to Gram staining and requires acid-fast staining for visualization.
*Interferon-gamma assay*
- An **interferon-gamma release assay (IGRA)**, like the Quantiferon-TB Gold test, detects exposure to *Mycobacterium tuberculosis* and is used to diagnose **latent TB infection**.
- Similar to the PPD test, it cannot distinguish between latent infection and **active disease**, and a positive result requires further investigation for active TB.
Actinomyces and Nocardia US Medical PG Question 10: A 45-year-old man comes to the physician because of a 1-month history of fever and poor appetite. Five weeks ago, he underwent molar extraction for dental caries. His temperature is 38°C (100.4°F). Cardiac examination shows a grade 2/6 holosystolic murmur heard best at the apex. A blood culture shows gram-positive, catalase-negative cocci. Transesophageal echocardiography shows a small vegetation on the mitral valve with mild regurgitation. The causal organism most likely has which of the following characteristics?
- A. Production of dextrans (Correct Answer)
- B. Production of CAMP factor
- C. Conversion of fibrinogen to fibrin
- D. Formation of germ tubes at body temperature
- E. Replication in host macrophages
Actinomyces and Nocardia Explanation: **Production of dextrans**
- The clinical picture of **fever**, **poor appetite**, a **holosystolic murmur**, and **mitral valve vegetation** following a dental procedure (molar extraction) strongly points to **infective endocarditis** caused by **Viridans streptococci**.
- **Viridans streptococci**, commonly found in the oral cavity, produce **dextrans**, which allow them to adhere to damaged heart valves and fibrin-platelet aggregates, initiating vegetation formation.
*Production of CAMP factor*
- **CAMP factor** is a characteristic of **Group B Streptococcus (Streptococcus agalactiae)**, which primarily causes infections in neonates and immunocompromised adults, not typically infective endocarditis post-dental procedure.
- *Streptococcus agalactiae* is also catalase-negative and gram-positive but is rarely associated with endocarditis arising from oral flora.
*Conversion of fibrinogen to fibrin*
- The ability to convert **fibrinogen to fibrin** is characteristic of **coagulase-positive organisms**, such as *Staphylococcus aureus*, which is a catalase-positive organism.
- The blood culture in this case specifically states **catalase-negative cocci**, ruling out *Staphylococcus aureus* as the causative agent.
*Formation of germ tubes at body temperature*
- **Germ tube formation** at body temperature is a distinguishing characteristic of *Candida albicans*, a **fungus**, not a gram-positive, catalase-negative coccus.
- While *Candida* can cause endocarditis, the microbiological findings described do not align with a fungal infection.
*Replication in host macrophages*
- **Intracellular replication in host macrophages** is characteristic of certain bacteria like *Mycobacterium tuberculosis*, *Listeria monocytogenes*, or *Salmonella typhi*, which typically cause systemic infections
- This characteristic is not associated with the gram-positive, catalase-negative cocci responsible for subacute bacterial endocarditis following dental procedures.
More Actinomyces and Nocardia US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.