Neisseria species (meningitidis, gonorrhoeae) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Neisseria species (meningitidis, gonorrhoeae). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Neisseria species (meningitidis, gonorrhoeae) US Medical PG Question 1: An 18-year-old male in his first year of college presents to the emergency room with a fever and a severe headache. He reports having unprotected sex with several partners over the past few weeks. Upon examination, the male demonstrates nuchal rigidity and photophobia. His past medical history is notable for a lack of vaccinations beginning from infancy due to his parents' belief that vaccinations may cause autism. The bacteria causing these symptoms would most likely demonstrate which of the following?
- A. Negative catalase test
- B. Gram-negative bacteria (Correct Answer)
- C. Urease positive
- D. Positive quellung reaction
- E. Lactose fermentation
Neisseria species (meningitidis, gonorrhoeae) Explanation: ***Gram-negative bacteria***
- The clinical picture of fever, severe headache, **nuchal rigidity**, and photophobia in an unvaccinated 18-year-old college student strongly suggests **bacterial meningitis** caused by *Neisseria meningitidis*.
- *Neisseria meningitidis* is a **Gram-negative diplococcus**, which is the most definitive laboratory characteristic for identifying this organism.
- College dormitory settings and unvaccinated status are major risk factors for **meningococcal meningitis**, and Gram stain is typically the first diagnostic step showing Gram-negative diplococci in CSF.
*Positive quellung reaction*
- The Quellung reaction (capsular swelling) is classically associated with **Streptococcus pneumoniae**, not *Neisseria meningitidis*.
- While *N. meningitidis* does have a polysaccharide capsule, the Quellung test is not the standard identification method for this organism.
- *S. pneumoniae* would be more common in older adults or those with specific risk factors like asplenia.
*Negative catalase test*
- *Neisseria meningitidis* is **catalase-positive**, so a negative catalase test would rule out this organism.
- Catalase-negative organisms include Streptococcus and Enterococcus species, which have different clinical presentations.
*Lactose fermentation*
- *Neisseria meningitidis* is a **non-lactose fermenter** and does not utilize lactose fermentation for energy.
- Lactose fermentation is characteristic of enteric Gram-negative bacteria like *E. coli* and *Klebsiella*, not Neisseria species.
- *N. meningitidis* ferments **maltose and glucose**, which distinguishes it from *N. gonorrhoeae* (glucose only).
*Urease positive*
- *Neisseria meningitidis* is **urease-negative**, so urease positivity would rule out this organism.
- Urease-positive bacteria include *Helicobacter pylori*, *Proteus* species, and *Klebsiella*, none of which typically cause meningitis in this clinical setting.
Neisseria species (meningitidis, gonorrhoeae) US Medical PG Question 2: A medical technician is trying to isolate a pathogen from the sputum sample of a patient. The sample is heat fixed to a slide then covered with carbol fuchsin stain and heated again. After washing off the stain with clean water, the slide is covered with 1% sulfuric acid for decolorization. The sample is rinsed again and stained with methylene blue. Microscopic examination shows numerous red, branching filamentous organisms. Which of the following is the most likely isolated pathogen?
- A. Cryptococcus neoformans
- B. Tropheryma whipplei
- C. Nocardia asteroides (Correct Answer)
- D. Rickettsia rickettsii
- E. Staphylococcus aureus
Neisseria species (meningitidis, gonorrhoeae) Explanation: ***Nocardia asteroides***
- The described staining procedure is a **modified acid-fast stain**, indicated by the use of **carbol fuchsin**, heating, and decolorization with **weak acid (1% sulfuric acid)**, followed by a counterstain with methylene blue.
- **Nocardia species** are **weakly acid-fast bacteria** that resist decolorization with weak acids (1-3% sulfuric acid), appearing as **red, branching filamentous organisms** under this staining method.
- The **modified acid-fast stain** uses weaker decolorizing agents compared to the standard Ziehl-Neelsen stain, making it suitable for detecting weakly acid-fast organisms like Nocardia.
- Nocardia are aerobic actinomycetes commonly found in soil and can cause pulmonary infections, especially in immunocompromised patients.
*Cryptococcus neoformans*
- This is a **yeast** that is typically identified using an **India ink stain** to visualize its polysaccharide capsule, or through fungal stains like Gomori methenamine silver (GMS).
- It would not appear as acid-fast red branching filaments with the described technique.
*Tropheryma whipplei*
- This bacterium is typically identified by **periodic acid-Schiff (PAS) stain** in tissue biopsies, which highlights its cell wall glycoproteins (appears magenta).
- It is not acid-fast and would not retain the carbol fuchsin after acid decolorization.
*Rickettsia rickettsii*
- This is an **obligate intracellular bacterium** that is difficult to culture and is often diagnosed by **serological tests** or **immunohistochemistry** on skin biopsy specimens.
- It is not acid-fast and would not be detected by this staining technique.
*Staphylococcus aureus*
- This is a **Gram-positive coccus** that would be stained **purple** by a Gram stain as it retains crystal violet.
- It is not acid-fast and would be completely decolorized by sulfuric acid in the described procedure, appearing blue (counterstain color) rather than red.
Neisseria species (meningitidis, gonorrhoeae) US Medical PG Question 3: An 18-year-old female college student is brought to the emergency department by ambulance for a headache and altered mental status. The patient lives with her boyfriend who is with her currently. He states she had not been feeling well for the past day and has vomited several times in the past 12 hours. Lumbar puncture is performed in the emergency room and demonstrates an increased cell count with a neutrophil predominance and gram-negative diplococci on Gram stain. The patient is started on vancomycin and ceftriaxone. Which of the following is the best next step in management?
- A. Treat boyfriend with rifampin (Correct Answer)
- B. Add ampicillin to treatment regimen
- C. Add ampicillin, dexamethasone, and rifampin to treatment regimen
- D. Add dexamethasone to treatment regimen
- E. Treat boyfriend with ceftriaxone and vancomycin
Neisseria species (meningitidis, gonorrhoeae) Explanation: ***Treat boyfriend with rifampin***
- The patient's presentation with headache, altered mental status, neutrophilic pleocytosis, and **Gram-negative diplococci** on CSF Gram stain is highly suggestive of **Neisseria meningitidis** meningitis.
- The patient is already on appropriate empiric antibiotic therapy (vancomycin and ceftriaxone), so the **immediate priority** is to prevent secondary cases through **post-exposure prophylaxis** for close contacts.
- Close contacts, including household members like the boyfriend, are at high risk of contracting the infection and should receive prophylaxis within **24 hours** of case identification, with **rifampin**, **ciprofloxacin**, or **IM ceftriaxone** being standard options.
*Add ampicillin to treatment regimen*
- Ampicillin provides coverage for **Listeria monocytogenes**, but the Gram stain demonstrating **Gram-negative diplococci** makes Listeria (Gram-positive rod) unlikely in this otherwise healthy young adult without specific risk factors for Listeria.
- The current regimen of vancomycin and ceftriaxone provides adequate empiric coverage for acute bacterial meningitis, targeting common pathogens like **S. pneumoniae** and **N. meningitidis**.
*Add ampicillin, dexamethasone, and rifampin to treatment regimen*
- While providing rifampin prophylaxis to the boyfriend is appropriate, adding it to the **patient's** treatment regimen is not indicated for her active infection.
- **Dexamethasone** is often added to reduce inflammation and neurological sequelae but should be given **prior to or concurrently** with the first dose of antibiotics; adding it later in the course may not be as beneficial.
- This option conflates treatment of the patient with prophylaxis of contacts.
*Add dexamethasone to treatment regimen*
- Dexamethasone is recommended in adults with suspected pneumococcal meningitis to reduce mortality and neurological sequelae, but ideal administration is **prior to or with the first dose of antibiotics**.
- While it might still be considered, the priority given the **Gram-negative diplococci** (suggesting N. meningitidis rather than S. pneumoniae) is **contact prophylaxis** to prevent further spread, and the timing for optimal dexamethasone benefit has likely passed.
*Treat boyfriend with ceftriaxone and vancomycin*
- Ceftriaxone and vancomycin are appropriate for treating the patient's active meningitis, but they are not the standard or preferred agents for **post-exposure prophylaxis** in contacts.
- Post-exposure prophylaxis typically involves a short course of agents like **rifampin**, **ciprofloxacin**, or a single dose of **intramuscular ceftriaxone**, primarily to eradicate nasopharyngeal carriage and prevent transmission.
Neisseria species (meningitidis, gonorrhoeae) US Medical PG Question 4: A 22-year-old female with no past medical history presents to her primary care physician with a 3-day history of knee pain. She denies any recent injury or trauma. On physical examination her knee is warm, erythematous, and has diminished range of movement. The patient reports having multiple sexual partners over the last year and does not use protection regularly. Her blood pressure is 124/85 mmHg, heart rate is 76/min, and temperature is 38.3℃ (101.0℉). A joint aspiration is performed and a growth of gram-negative diplococci is noted on bacterial culture. What is the treatment of choice for this patient's condition?
- A. Vancomycin monotherapy
- B. Fluoroquinolones
- C. Nafcillin monotherapy and joint aspiration
- D. Oxacillin and ceftriaxone
- E. Ceftriaxone monotherapy and joint aspiration (Correct Answer)
Neisseria species (meningitidis, gonorrhoeae) Explanation: ***Ceftriaxone monotherapy and joint aspiration***
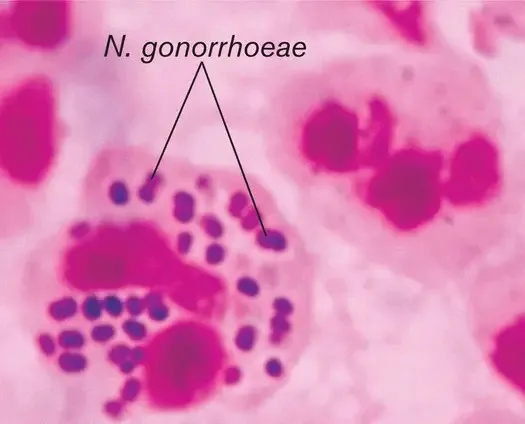
- The patient's presentation with **acute monoarthritis**, fever, and **gram-negative diplococci** on joint culture is highly suggestive of **gonococcal arthritis**. Intravenous ceftriaxone is the treatment of choice for disseminated gonococcal infection.
- While joint aspiration confirms the diagnosis and can relieve pressure, definitive treatment requires systemic antibiotics to clear the infection.
*Vancomycin monotherapy*
- **Vancomycin** is primarily effective against **gram-positive bacteria**, particularly MRSA, and would not adequately cover the gram-negative diplococci found in this case.
- Using vancomycin alone would leave the patient's gonococcal infection untreated, potentially leading to worsening of symptoms or complications.
*Fluoroquinolones*
- While some fluoroquinolones have activity against *Neisseria gonorrhoeae*, **widespread resistance** to this class of antibiotics has emerged, making them an unreliable choice for empiric or first-line treatment of gonococcal infections.
- The CDC no longer recommends fluoroquinolones for gonococcal infections due to high rates of resistance.
*Nafcillin monotherapy and joint aspiration*
- **Nafcillin** is a narrow-spectrum penicillin effective primarily against **methicillin-sensitive *Staphylococcus aureus*** and other gram-positive organisms.
- It would not provide appropriate coverage for the **gram-negative diplococci** identified in this patient's joint fluid.
*Oxacillin and ceftriaxone*
- While **ceftriaxone** is appropriate, the addition of **oxacillin** (another anti-staphylococcal penicillin) would be unnecessary.
- Oxacillin is primarily used for gram-positive infections and would not add benefit against **gonococcal arthritis**, increasing the risk of adverse effects without improving efficacy.
Neisseria species (meningitidis, gonorrhoeae) US Medical PG Question 5: A 15-year-old boy is brought to the Emergency department by ambulance from school. He started the day with some body aches and joint pain but then had several episodes of vomiting and started complaining of a terrible headache. The school nurse called for emergency services. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. Past medical history is noncontributory. He is a good student and enjoys sports. At the hospital, his blood pressure is 120/80 mm Hg, heart rate is 105/min, respiratory rate is 21/min, and his temperature is 38.9°C (102.0°F). On physical exam, he appears drowsy with neck stiffness and sensitivity to light. Kernig’s sign is positive. An ophthalmic exam is performed followed by a lumbar puncture. An aliquot of cerebrospinal fluid is sent to microbiology. A gram stain shows gram-negative diplococci. A smear is prepared on blood agar and grows round, smooth, convex colonies with clearly defined edges. Which of the following would identify the described pathogen?
- A. Oxidase-positive and ferments glucose and maltose (Correct Answer)
- B. Oxidase-positive test and ferments glucose only
- C. Catalase-negative and oxidase-positive
- D. No growth on Thayer-Martin medium
- E. Growth in anaerobic conditions
Neisseria species (meningitidis, gonorrhoeae) Explanation: ***Oxidase-positive and ferments glucose and maltose***
- The patient's symptoms (fever, headache, neck stiffness, sensitivity to light, positive Kernig's sign) are classic for **meningitis**, and the CSF showing **gram-negative diplococci** points to *Neisseria meningitidis*.
- *Neisseria meningitidis* is identified by its positive **oxidase test** and its ability to ferment both **glucose and maltose**.
*Oxidase-positive test and ferments glucose only*
- This description corresponds to *Neisseria gonorrhoeae*, which primarily causes **gonorrhea** and occasionally meningitis due to disseminated infection but is less common in this age group and presentation.
- While *Neisseria gonorrhoeae* is also an **oxidase-positive gram-negative diplococcus**, it specifically ferments only *glucose*, not maltose.
*Catalase-negative and oxidase-positive*
- While *Neisseria meningitidis* is **oxidase-positive**, stating it is "catalase-negative" is incorrect; *Neisseria* species are actually **catalase-positive**.
- This option incorrectly describes a general metabolic property that would rule out *Neisseria meningitidis*.
*No growth on Thayer-Martin medium*
- Thayer-Martin medium is a **selective medium** specifically designed to isolate pathogenic *Neisseria species* by inhibiting the growth of commensal bacteria and fungi.
- Therefore, *Neisseria meningitidis* would **grow well** on Thayer-Martin medium, making "no growth" an incorrect identifier.
*Growth in anaerobic conditions*
- *Neisseria meningitidis* is an **obligate aerobe**, meaning it requires oxygen for growth.
- It would **not grow** in anaerobic conditions, making this statement false for identifying the described pathogen.
Neisseria species (meningitidis, gonorrhoeae) US Medical PG Question 6: A 25-year-old man with no significant past medical history is brought in by ambulance after a witnessed seizure at home. On physical exam, temperature is 102.3 deg F (39.1 deg C), blood pressure is 90/62 mmHg, pulse is 118/min, and respirations are 25/min. He is unable to touch his chin to his chest and spontaneously flexes his hips with passive neck flexion. Appropriate empiric treatment is begun. CT head is unremarkable, and a lumbar puncture sample is obtained. Gram stain of the cerebrospinal fluid (CSF) reveals gram-positive diplococci. Which of the following would you expect to see on CSF studies?
- A. Elevated opening pressure, elevated protein, normal glucose
- B. Normal opening pressure, normal protein, normal glucose
- C. Elevated opening pressure, elevated protein, elevated glucose
- D. Normal opening pressure, elevated protein, normal glucose
- E. Elevated opening pressure, elevated protein, low glucose (Correct Answer)
Neisseria species (meningitidis, gonorrhoeae) Explanation: ***Elevated opening pressure, elevated protein, low glucose***
- **Bacterial meningitis** typically presents with an **elevated opening pressure** due to inflammation and increased intracranial pressure.
- The inflammatory response leads to increased vascular permeability, causing **elevated protein** in the CSF and **low glucose** due to bacterial consumption.
*Elevated opening pressure, elevated protein, normal glucose*
- While **elevated opening pressure** and **elevated protein** can be seen in inflammatory conditions, **normal CSF glucose** is more characteristic of viral meningitis or non-infectious inflammatory conditions, not bacterial.
- In bacterial meningitis, bacteria metabolize glucose, leading to a **decreased CSF glucose level**.
*Normal opening pressure, normal protein, normal glucose*
- This profile is typical for a **normal CSF study** or certain chronic neurological conditions, not acute bacterial meningitis.
- The patient's severe symptoms, including fever, seizure, and meningismus, contradict a normal CSF profile.
*Elevated opening pressure, elevated protein, elevated glucose*
- While **elevated opening pressure** and **elevated protein** can occur, **elevated CSF glucose** is inconsistent with any common form of meningitis.
- An elevated CSF glucose is rare and would suggest systemic hyperglycemia without impaired glucose transport into the CSF.
*Normal opening pressure, elevated protein, normal glucose*
- A **normal opening pressure** would be unusual in a patient with bacterial meningitis, given the inflammation and potential for increased intracranial pressure.
- While **elevated protein** and **normal glucose** can occur in certain conditions (e.g., Guillain-Barré syndrome), it does not fit the clinical picture of acute bacterial meningitis with fever and meningismus.
Neisseria species (meningitidis, gonorrhoeae) US Medical PG Question 7: A 22-year-old female is brought to the emergency department by her roommate with a one day history of fever and malaise. She did not feel well after class the previous night and has been in her room since then. She has not been eating or drinking due to severe nausea. Her roommate checked on her one hour ago and was alarmed to find a fever of 102°F (38.9°C). On physical exam temperature is 103°F (40°C), blood pressure is 110/66 mmHg, pulse is 110/min, respirations are 23/min, and pulse oximetry is 98% on room air. She refuses to move her neck and has a rash on her trunk. You perform a lumbar puncture and the CSF analysis is shown below.
Appearance: Cloudy
Opening pressure: 180 mm H2O
WBC count: 150 cells/µL (93% PMN)
Glucose level: < 40 mg/dL
Protein level: 50 mg/dL
Gram stain: gram-negative diplococci
Based on this patient's clinical presentation, which of the following should most likely be administered?
- A. Ceftriaxone (Correct Answer)
- B. Dexamethasone
- C. Rifampin
- D. Acyclovir
- E. Erythromycin
Neisseria species (meningitidis, gonorrhoeae) Explanation: ***Ceftriaxone***
- The patient presents with classic signs of **bacterial meningitis** (fever, neck stiffness, rash, altered mental status) and CSF analysis confirms, showing **cloudy appearance**, **elevated opening pressure**, **high WBC count with PMN predominance**, **low glucose**, and **gram-negative diplococci** on Gram stain, typical for *Neisseria meningitidis*.
- **Ceftriaxone** is a third-generation cephalosporin, a first-line antibiotic for treating bacterial meningitis, particularly effective against *Neisseria meningitidis*.
*Dexamethasone*
- While **dexamethasone** can be used as an adjunct in bacterial meningitis, particularly when caused by *Streptococcus pneumoniae*, it's administered *before or with* the first dose of antibiotics to mitigate inflammation.
- It is not the primary treatment to *eradicate* the infection and is less critical than immediate antibiotic therapy.
*Rifampin*
- **Rifampin** is primarily used for chemoprophylaxis in close contacts of individuals with meningococcal meningitis, or as part of a multi-drug regimen for tuberculosis.
- It is not the recommended first-line monotherapy for acute bacterial meningitis.
*Acyclovir*
- **Acyclovir** is an antiviral medication used to treat herpes simplex virus (HSV) meningitis or encephalitis.
- The CSF analysis showing **gram-negative diplococci** clearly indicates a bacterial etiology, not viral, making acyclovir inappropriate.
*Erythromycin*
- **Erythromycin** is a macrolide antibiotic with a narrower spectrum of activity and is not typically used as first-line treatment for bacterial meningitis, especially not for *Neisseria meningitidis*.
- Its use is often limited by resistance and side effects compared to third-generation cephalosporins.
Neisseria species (meningitidis, gonorrhoeae) US Medical PG Question 8: An endocervical swab is performed and nucleic acid amplification testing via polymerase chain reaction is conducted. It is positive for Chlamydia trachomatis and negative for Neisseria gonorrhoeae. Which of the following is the most appropriate pharmacotherapy?
- A. Oral azithromycin (Correct Answer)
- B. Intramuscular ceftriaxone plus oral azithromycin
- C. Oral doxycycline
- D. Intramuscular ceftriaxone
- E. Intravenous cefoxitin plus oral doxycycline
Neisseria species (meningitidis, gonorrhoeae) Explanation: ***Oral azithromycin***
- A single 1-gram oral dose of **azithromycin** is a highly effective and convenient first-line treatment for uncomplicated **Chlamydia trachomatis** infections.
- Its long half-life allows for once-daily dosing, improving patient adherence.
*Intramuscular ceftriaxone plus oral azithromycin*
- This combination therapy is primarily used for suspected or confirmed **gonorrhea** and chlamydia coinfection, particularly if N. gonorrhoeae cannot be ruled out.
- Since **Neisseria gonorrhoeae** was explicitly negative, the ceftriaxone component is unnecessary.
*Oral doxycycline*
- **Doxycycline** (100 mg twice daily for 7 days) is an alternative first-line treatment for **Chlamydia trachomatis** infections and is highly effective.
- However, azithromycin is often preferred for its single-dose regimen which can improve treatment adherence, especially in asymptomatic patients.
*Intramuscular ceftriaxone*
- **Ceftriaxone** is the primary treatment for **Neisseria gonorrhoeae** infections.
- As the test for **N. gonorrhoeae** was negative, this treatment is not indicated for the current patient's diagnosis.
*Intravenous cefoxitin plus oral doxycycline*
- This regimen is typically reserved for more severe infections, such as **pelvic inflammatory disease (PID)**, often requiring hospitalization, which is not indicated by the simple positive chlamydia swab.
- Administering **IV cefoxitin** is an escalation beyond what is necessary for uncomplicated chlamydial cervicitis.
Neisseria species (meningitidis, gonorrhoeae) US Medical PG Question 9: A 71-year-old woman presents with high-grade fever and chills, difficulty breathing, and a productive cough with rust-colored sputum. She complains of a sharp left-sided chest pain. Physical examination reveals increased fremitus, dullness to percussion, and bronchial breath sounds on the lower left side. A chest X-ray shows left lower lobe consolidation. The offending organism that was cultured from the sputum was catalase-negative and had a positive Quellung reaction. The organism will show which gram stain results?
- A. Gram-negative diplococci
- B. Cannot be seen with gram staining since the organism lacks a cell wall
- C. Gram-positive cocci in clusters
- D. Gram-negative rod
- E. Gram-positive diplococci (Correct Answer)
Neisseria species (meningitidis, gonorrhoeae) Explanation: ***Gram-positive diplococci***
- The clinical presentation (high fever, chills, productive cough with **rust-colored sputum**, sharp chest pain, signs of **consolidation**) is classic for **pneumococcal pneumonia**.
- The organism responsible for pneumococcal pneumonia, *Streptococcus pneumoniae*, is a **Gram-positive, catalase-negative diplococcus** that exhibits a **positive Quellung reaction** due to its polysaccharide capsule.
*Gram-negative diplococci*
- This describes organisms such as **Neisseria meningitidis** or **Neisseria gonorrhoeae**, which cause meningitis or gonorrhea, respectively, not typical pneumonia.
- While *Moraxella catarrhalis* is a Gram-negative diplococcus that can cause respiratory infections, it typically causes otitis media or sinusitis and less commonly severe pneumonia with rust-colored sputum.
*Cannot be seen with gram staining since the organism lacks a cell wall*
- This description typically refers to **Mycoplasma pneumoniae**, which causes **atypical pneumonia** and lacks a cell wall, rendering it unstainable by Gram stain.
- Mycoplasma pneumonia usually presents with a more indolent course, a non-productive cough, and rarely causes rust-colored sputum or lobar consolidation seen on X-ray.
*Gram-positive cocci in clusters*
- This morphology is characteristic of **staphylococci**, such as *Staphylococcus aureus*, which can cause pneumonia, often in immunocompromised individuals or as a complication of influenza.
- However, *Staphylococcus aureus* is **catalase-positive**, and its pneumonia presentation can be more fulminant, often leading to abscess formation, differing from the typical presentation of pneumococcal pneumonia.
*Gram-negative rod*
- This morphology is characteristic of various bacteria including **Klebsiella pneumoniae**, **Pseudomonas aeruginosa**, or **Haemophilus influenzae**.
- **Klebsiella pneumoniae** can cause severe pneumonia with **currant jelly sputum** but is a Gram-negative rod and would not exhibit a Quellung reaction in the same manner as *S. pneumoniae*.
Neisseria species (meningitidis, gonorrhoeae) US Medical PG Question 10: A 19-year-old male is found to have Neisseria gonorrhoeae bacteremia. This bacterium produces an IgA protease capable of cleaving the hinge region of IgA antibodies. What is the most likely physiological consequence of such a protease?
- A. Membrane attack complex formation is impaired
- B. Impaired antibody binding to mast cells
- C. Opsonization and phagocytosis of pathogen cannot occur
- D. Impaired adaptive immune system memory
- E. Impaired mucosal immune protection (Correct Answer)
Neisseria species (meningitidis, gonorrhoeae) Explanation: ***Impaired mucosal immune protection***
- **IgA** is the primary antibody mediating **mucosal immunity**, protecting surfaces like the urogenital tract from pathogens.
- Cleavage of IgA by a protease directly compromises its ability to bind to and neutralize pathogens at these mucosal surfaces, facilitating infection.
*Membrane attack complex formation is impaired*
- The **membrane attack complex (MAC)** is primarily formed by components of the **complement system (C5b-C9)**, which is activated by IgG and IgM, not IgA.
- While IgA can activate the alternative pathway of complement, its primary role is not in MAC formation.
*Impaired antibody binding to mast cells*
- **Mast cells** primarily bind **IgE antibodies** via their Fc receptors, leading to degranulation upon allergen binding.
- IgA does not typically bind to mast cells, so IgA protease activity would not directly impact this process.
*Opsonization and phagocytosis of pathogen cannot occur*
- **Opsonization** leading to phagocytosis is predominantly mediated by **IgG antibodies** and **complement proteins (e.g., C3b)**.
- While IgA can contribute to opsonization to some extent, it is not the primary mediator, and its impairment would not completely prevent all opsonization.
*Impaired adaptive immune system memory*
- **Adaptive immune system memory** is largely mediated by **memory B cells** and **memory T cells**, which produce and respond to various antibody isotypes (IgG, IgA, IgM, IgE).
- The cleavage of existing IgA antibodies does not directly impair the generation or function of memory lymphocytes, although it might lead to more frequent infections requiring a new immune response.
More Neisseria species (meningitidis, gonorrhoeae) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.