Helicobacter pylori US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Helicobacter pylori. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Helicobacter pylori US Medical PG Question 1: A 45-year-old woman has a history of mild epigastric pain, which seems to have gotten worse over the last month. Her pain is most severe several hours after a meal and is somewhat relieved with over-the-counter antacids. The patient denies abnormal tastes in her mouth or radiating pain. She does not take any other over-the-counter medications. She denies bleeding, anemia, or unexplained weight loss, and denies a family history of gastrointestinal malignancy. Which of the following is the best next step in the management of this patient?
- A. Barium swallow
- B. Urease breath test (Correct Answer)
- C. Esophageal pH monitoring
- D. Empiric proton pump inhibitor therapy
- E. Upper endoscopy with biopsy of gastric mucosa
Helicobacter pylori Explanation: ***Urease breath test***
- The patient's symptoms of **epigastric pain** that is worse several hours after a meal and relieved by antacids are highly suggestive of a **peptic ulcer**.
- Given her age (45) and the absence of alarm symptoms (bleeding, weight loss, dysphagia), testing for **_H. pylori_ infection** with a non-invasive method like the **urease breath test** [1] is the most appropriate initial step.
- Identifying and eradicating _H. pylori_ is the cornerstone of therapy for peptic ulcers to relieve symptoms and prevent recurrence [1].
*Barium swallow*
- A **barium swallow** is primarily used to evaluate **structural abnormalities** of the esophagus, stomach, and duodenum.
- It is less effective for diagnosing **mucosal pathology** like peptic ulcers or _H. pylori_ infection compared to endoscopy or breath tests.
*Esophageal pH monitoring*
- **Esophageal pH monitoring** is the gold standard for diagnosing **gastroesophageal reflux disease (GERD)**.
- The patient's symptoms are more consistent with peptic ulcer disease, especially the pain pattern and relief with antacids, rather than typical GERD symptoms like heartburn or regurgitation.
*Empiric proton pump inhibitor therapy*
- While empiric PPI therapy can be considered for **GERD** or **dyspepsia**, it's generally not the first line when **_H. pylori_** is a strong possibility, especially in a patient with symptoms suggestive of a peptic ulcer.
- Identifying and eradicating _H. pylori_ is crucial for ulcer healing and preventing recurrence, and this would be missed with just empiric PPI therapy [1].
*Upper endoscopy with biopsy of gastric mucosa*
- **Upper endoscopy** is indicated when **alarm symptoms** (e.g., GI bleeding, unexplained weight loss, dysphagia, anemia) [2] are present, or in older patients (>60 years) with new-onset dyspepsia.
- For a 45-year-old with non-alarming symptoms, a **non-invasive _H. pylori_ test** is preferred initially before proceeding to endoscopy.
Helicobacter pylori US Medical PG Question 2: A 30-year-old man who recently emigrated from Southeast Asia presents with heartburn and a bad taste in his mouth. He says the symptoms have been present for the last 6 months and are much worse at night. He describes the pain as moderate to severe, burning in character, and localized to the epigastric region. He mentions that 1 month ago, he was tested for Helicobacter pylori back in his country and completed a course of multiple antibiotics, but there has been no improvement in his symptoms. Which of the following is the most likely diagnosis in this patient?
- A. Peptic ulcer disease
- B. Gastric MALT (mucosa-associated lymphoid tissue) lymphoma
- C. Duodenal ulcer disease
- D. Gastroesophageal reflux disease (Correct Answer)
- E. Gastric adenocarcinoma
Helicobacter pylori Explanation: ***Gastroesophageal reflux disease***
- The patient's symptoms of **heartburn**, a **bad taste in his mouth**, and worsening symptoms at **night** are classic presentations of **Gastroesophageal Reflux Disease (GERD)**.
- The failure of **H. pylori eradication therapy** to improve symptoms suggests that H. pylori infection was not the primary cause of his dyspepsia.
*Peptic ulcer disease*
- While **epigastric pain** can be seen in peptic ulcer disease (**PUD**), the prominent symptoms of **heartburn** and a **sour taste in the mouth** are more characteristic of GERD.
- The lack of specific relief with food or worsening with particular food types (common in PUD) makes it less likely, and the failure of H. pylori treatment points away from most common PUD etiologies.
*Gastric MALT (mucosa-associated lymphoid tissue) lymphoma*
- **Gastric MALT lymphoma** is often associated with chronic **H. pylori infection**, but its symptoms are typically more vague, such as **weight loss**, **anorexia**, or **nausea**, and less specifically tied to heartburn and acid reflux.
- The prompt response to H. pylori eradication is often seen in early-stage MALT lymphoma, but the patient's symptoms persisted despite antibiotic treatment.
*Duodenal ulcer disease*
- Similar to peptic ulcer disease, **duodenal ulcers** typically present with **epigastric pain** that often improves with food and worsens 2-3 hours after meals or at night.
- The description of **heartburn** and a **sour taste** makes GERD a more direct fit than duodenal ulcer disease.
*Gastric adenocarcinoma*
- **Gastric adenocarcinoma** presents with symptoms like **weight loss**, **early satiety**, **dysphagia**, or **anemia**, which are not reported in this patient.
- While it can cause epigastric pain, the specific reflux symptoms and absence of "alarm features" like weight loss make it less likely in this young patient.
Helicobacter pylori US Medical PG Question 3: A 28-year-old graduate student visits the university health clinic for 3-weeks of epigastric pain that worsens with meals, associated with retrosternal pain, early satiety, and bloating. She denies vomiting blood or blood in her stool. She has been consuming large volumes of caffeinated-drinks and fast-food for a month, as she has been studying for her tests. Her family and personal history are unremarkable with no history of gastrointestinal cancer. Her vital signs are within normal limits. Physical examination is only positive for a mild epigastric tenderness. Which of the following is the most appropriate approach in this case?
- A. Treatment with metoclopramide
- B. Upper endoscopy
- C. Fecal antigen testing for Helicobacter pylori (Correct Answer)
- D. Treatment with omeprazole
- E. Barium swallow radiograph
Helicobacter pylori Explanation: ***Fecal antigen testing for Helicobacter pylori***
- The patient presents with **dyspeptic symptoms** (epigastric pain, early satiety, bloating) and no **alarm symptoms** (e.g., GI bleeding, unexplained weight loss, dysphagia).
- Given her age (< 60 years) and lack of alarm symptoms, a "test-and-treat" strategy for **Helicobacter pylori** is recommended, with fecal antigen testing being a non-invasive and accurate option.
*Treatment with metoclopramide*
- Metoclopramide is a **prokinetic agent** used for conditions like gastroparesis, not primarily for initial management of undiagnosed dyspepsia.
- While she has early satiety, the primary approach should be to rule out common causes of dyspepsia like **H. pylori** before considering symptomatic treatments for motility issues.
*Upper endoscopy*
- An **upper endoscopy** is indicated if the patient is older (typically > 60 years) or has **alarm symptoms** (e.g., GI bleeding, unexplained weight loss, dysphagia, persistent vomiting).
- This 28-year-old patient lacks any alarm symptoms and is below the age threshold for an immediate endoscopic evaluation for dyspepsia.
*Treatment with omeprazole*
- While a **proton pump inhibitor (PPI)** like omeprazole can treat dyspeptic symptoms, it is not the most appropriate *initial* approach without first testing for **H. pylori**.
- Empiric PPI therapy can **mask H. pylori infection**, potentially delaying appropriate eradication therapy if the test-and-treat strategy is not followed.
*Barium swallow radiograph*
- A **barium swallow** is primarily used to evaluate structural abnormalities of the **esophagus**, such as strictures, diverticula, or achalasia, and is less effective for diagnosing mucosal diseases of the stomach or duodenum.
- It is not the preferred diagnostic test for evaluating dyspepsia or identifying **H. pylori** infection.
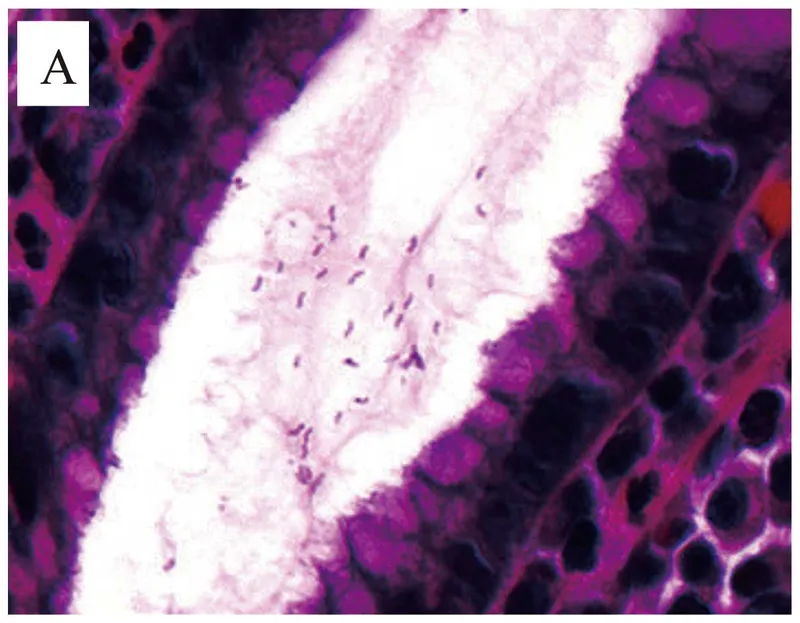
Helicobacter pylori US Medical PG Question 4: A 49-year-old male complains of abdominal discomfort that worsens following meals. A gastric biopsy reveals a 2 cm gastric ulcer, and immunohistochemical staining demonstrates the presence of a rod-shaped bacterium in the gastric mucosa. Which of the following is used by the infiltrating pathogen to neutralize gastric acidity?
- A. Mucinase
- B. LT toxin
- C. Flagella
- D. Bismuth
- E. Urease (Correct Answer)
Helicobacter pylori Explanation: ***Urease***
- The presence of a rod-shaped bacterium in the gastric mucosa causing ulcers points to **Helicobacter pylori**.
- **H. pylori** produces **urease**, an enzyme that converts urea into ammonia and carbon dioxide, creating a more alkaline environment around the bacterium, thus neutralizing gastric acid and allowing its survival.
*Mucinase*
- **Mucinase** is an enzyme produced by some bacteria that breaks down the protective mucus layer, contributing to mucosal damage.
- While contributing to pathogenesis, mucinase does not directly neutralize gastric acidity.
*LT toxin*
- **LT toxin** (heat-labile toxin) is primarily associated with **enterotoxigenic Escherichia coli (ETEC)** and causes watery diarrhea by increasing cAMP.
- This toxin is not produced by **H. pylori** and does not play a role in neutralizing gastric acid.
*Flagella*
- **Flagella** are **locomotor appendages** that allow **H. pylori** to move through the gastric mucus layer and colonize the gastric epithelium.
- While crucial for host colonization, flagella do not directly neutralize gastric acid.
*Bismuth*
- **Bismuth** is a component of some multi-drug regimens used to treat **H. pylori** infection, acting as an antimicrobial and mucosal protectant.
- It is not produced by the bacterium but is a medication given to the patient.
Helicobacter pylori US Medical PG Question 5: A 52-year-old man comes to the physician because of a 3-month history of upper abdominal pain and nausea that occurs about 3 hours after eating and at night. These symptoms improve with eating. After eating, he often has a feeling of fullness and bloating. He has had several episodes of dark stools over the past month. He has smoked one pack of cigarettes daily for 40 years and drinks 2 alcoholic beverages daily. He takes no medications. His temperature is 36.4°C (97.5°F), pulse is 80/min, and blood pressure is 110/70 mm Hg. Abdominal examination shows epigastric tenderness with no guarding or rebound. Bowel sounds are normal. Which of the following treatments is most appropriate to prevent further complications of the disease in this patient?
- A. Intravenous vitamin B12 supplementation
- B. Truncal vagotomy
- C. Amoxicillin, clarithromycin, and omeprazole (Correct Answer)
- D. Fundoplication, hiatoplasty, and gastropexy
- E. Distal gastrectomy with gastroduodenostomy
Helicobacter pylori Explanation: ***Amoxicillin, clarithromycin, and omeprazole***
- This patient's symptoms (epigastric pain 3 hours after eating and at night, improvement with eating, dark stools) are highly suggestive of a **duodenal ulcer complicated by upper gastrointestinal bleeding**. The most common cause of duodenal ulcers is *H. pylori* infection.
- The recommended first-line treatment for *H. pylori* infection involves a triple therapy regimen, including two antibiotics (like **amoxicillin and clarithromycin**) to eradicate the bacteria and a **proton pump inhibitor (omeprazole)** to reduce acid production and promote ulcer healing.
*Intravenous vitamin B12 supplementation*
- This treatment is appropriate for **vitamin B12 deficiency**, which can occur in conditions like atrophic gastritis, pernicious anemia, or following gastric resections, but is not indicated for acute peptic ulcer disease and wouldn't address the primary pathology.
- There is no clinical indication in the patient's presentation (e.g., neurological symptoms, macrocytic anemia) to suggest a deficiency in vitamin B12.
*Truncal vagotomy*
- **Truncal vagotomy** is a surgical procedure that was historically performed to reduce gastric acid secretion by cutting the vagus nerve. It is rarely used now due to the effectiveness of medical therapies for peptic ulcer disease.
- This invasive surgical option is generally reserved for refractory cases of peptic ulcer disease not responsive to medical management, or when complications like uncontrolled bleeding or perforation necessitate surgical intervention.
*Fundoplication, hiatoplasty, and gastropexy*
- These surgical procedures are primarily used to treat **gastroesophageal reflux disease (GERD)** and **hiatal hernia**, not peptic ulcer disease.
- Fundoplication wraps the stomach fundus around the lower esophagus to reinforce the lower esophageal sphincter, addressing reflux symptoms which are not the primary complaint here.
*Distal gastrectomy with gastroduodenostomy*
- **Distal gastrectomy** is a major surgical procedure involving the removal of the distal part of the stomach. It is typically reserved for severe complications of peptic ulcer disease (e.g., perforation, obstruction, recurrent bleeding unresponsive to other treatments) or gastric cancer.
- While it might be considered in extreme cases of complicated peptic ulcer, it is not the initial or most appropriate treatment for preventing further complications in a patient who has yet to receive standard anti-*H. pylori* therapy.
Helicobacter pylori US Medical PG Question 6: A previously healthy 37-year-old man comes to the physician for the evaluation of an 8-week history of intermittent burning epigastric pain. During this period, he has also felt bloated and uncomfortable after meals. He has not had weight loss or a change in bowel habits. He has no personal or family history of serious illness. He takes no medications. He does not smoke. He drinks 1–3 beers per week. Vital signs are within normal limits. Abdominal examination shows mild epigastric tenderness on palpation without guarding or rebound tenderness. Bowel sounds are normal. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Urea breath test (Correct Answer)
- B. Helicobacter pylori eradication therapy
- C. Helicobacter pylori serum IgG
- D. Upper gastrointestinal endoscopy
- E. Proton pump inhibitors
Helicobacter pylori Explanation: ***Urea breath test***
- The patient presents with classic symptoms of **dyspepsia**, and given his age (<60 years) and absence of **alarm symptoms** (e.g., weight loss, dysphagia, GI bleeding), an initial non-invasive test for **_Helicobacter pylori_** is appropriate.
- A **urea breath test** is a highly sensitive and specific non-invasive method to detect active _H. pylori_ infection.
*Helicobacter pylori eradication therapy*
- This therapy should only be initiated after a confirmed diagnosis of **_H. pylori_ infection**.
- Treating empirically without confirmation can lead to **antibiotic resistance** and unnecessary side effects.
*Helicobacter pylori serum IgG*
- A serum IgG test indicates only **prior exposure** to _H. pylori_ and does not distinguish between active and past infection.
- Therefore, it is **not suitable for diagnosing current active infection** or for confirming eradication.
*Upper gastrointestinal endoscopy*
- **Upper GI endoscopy** is indicated for patients over 60 with new-onset dyspepsia, or for those younger than 60 who present with **alarm symptoms** (e.g., weight loss, dysphagia, recurrent vomiting, GI bleeding, anemia).
- This patient currently has no alarm symptoms, making endoscopy an overly aggressive initial approach.
*Proton pump inhibitors*
- While **PPIs** are effective for symptom relief in dyspepsia, they can mask underlying _H. pylori_ infection or other serious conditions if used empirically without proper investigation.
- Furthermore, PPIs can cause **false-negative results** for _H. pylori_ tests like the urea breath test, so they should ideally be stopped for 1-2 weeks before testing.
Helicobacter pylori US Medical PG Question 7: A 33-year-old man living in the United States recently consumed a meal mostly consisting of raw shellfish that his girlfriend brought on her trip to Asia. After 2 days, he experienced a sudden onset of diarrhea and vomiting with severe abdominal cramps while his girlfriend developed mild diarrhea just several hours later. The diarrhea was profuse, looked like rice water, and had a pungent fishy odor. He soon started to experience muscle cramps and weakness, together with a deep labored breathing pattern. They called an ambulance and were transported to a local hospital. Based on the symptoms and blue hue to the skin, the attending physician hospitalized the male patient, started an intravenous infusion, and sent a stool specimen to the clinical microbiology laboratory for analysis. The next day, yellow bacterial colonies were observed on thiosulfate-citrate-bile salts-sucrose agar (as shown on the image). If you were the microbiologist on call, what kind of bacterial morphology would you expect to see during microscopic evaluation of a gram-stain slide made from those bacterial colonies?
- A. Seagull-shaped rods
- B. Club-shaped rods
- C. Corkscrew-shaped rods
- D. Spiral-shaped rods
- E. Comma-shaped rods (Correct Answer)
Helicobacter pylori Explanation: ***Comma-shaped rods***
- The clinical presentation of **profuse, rice-water diarrhea** with a **fishy odor** after consuming **raw shellfish** imported from Asia is highly characteristic of **cholera**, caused by *Vibrio cholerae*.
- *Vibrio cholerae* are gram-negative, **curved, or comma-shaped rods** that grow well on **thiosulfate-citrate-bile salts-sucrose (TCBS) agar**, forming specific colonies that, when gram-stained, reveal this distinct morphology.
- The yellow colonies on TCBS indicate sucrose fermentation, which is typical of *V. cholerae*, and the severe dehydration with blue hue (cyanosis) reflects the massive fluid loss caused by cholera toxin.
*Seagull-shaped rods*
- This morphology is characteristic of *Campylobacter jejuni*, which typically causes acute **gastroenteritis** with bloody diarrhea but not the classic "rice-water" stool associated with cholera.
- While *Campylobacter* can be acquired from contaminated food, the stool characteristics and rapid, severe dehydration point away from it.
*Club-shaped rods*
- **Club-shaped rods** are typical of *Corynebacterium diphtheriae*, the causative agent of **diphtheria**, which manifests as an upper respiratory tract infection with a pseudomembrane and systemic toxicity, not severe diarrheal disease.
- Their growth requirements and clinical presentation are completely different from what is described in the case.
*Corkscrew-shaped rods*
- This describes the morphology of **spirochetes**, such as *Treponema pallidum* (syphilis) or *Leptospira* species (leptospirosis), which cause diseases unrelated to acute diarrheal illness from shellfish.
- Spirochetes are typically visualized using darkfield microscopy and do not grow on TCBS agar.
*Spiral-shaped rods*
- **Spiral-shaped rods** can broadly describe several bacteria, including *Helicobacter pylori* (gastrointestinal ulcers) or some *Campylobacter* species.
- While *Helicobacter* is spiral, it's not associated with acute, severe cholera-like diarrhea, and *Campylobacter* is more specifically "seagull-shaped" or S-shaped.
Helicobacter pylori US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Helicobacter pylori Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Helicobacter pylori US Medical PG Question 9: A 30-year-old woman who is 24-weeks pregnant presents to the emergency department with fever, painful urination, and headache. The patient's blood pressure is 111/67 mm Hg, the pulse is 95/min, the respiratory rate is 16/min, and the temperature is 38.3°C (101.1°F). Physical examination reveals bilateral tender inguinal lymphadenopathy and painful genital lesions. On closer inspection, the patient’s genital lesions contain clear fluid and measure 5–6 mm in diameter. What is the appropriate description of these lesions?
- A. Pustule
- B. Ulcer
- C. Papule
- D. Bulla
- E. Vesicle (Correct Answer)
Helicobacter pylori Explanation: ***Vesicle***
- A **vesicle** is defined as a **circumscribed, elevated lesion** (macule/papule) containing **clear fluid** and measuring less than 1 cm in diameter.
- The patient's lesions, which are 5-6 mm in diameter and contain clear fluid, perfectly fit the description of vesicles, characteristic of **herpes simplex virus (HSV)** infection.
*Pustule*
- A **pustule** is a small, elevated lesion similar to a vesicle but filled with **pus**, not clear fluid.
- Examples include acne or folliculitis, which are typically opaque and yellowish, unlike the described lesions.
*Ulcer*
- An **ulcer** is a defect or excavation of the skin past the **epidermis**, resulting in the loss of tissue.
- The patient's lesions are described as fluid-filled and elevated, not as an open wound with tissue loss.
*Papule*
- A **papule** is a **solid, elevated lesion** measuring less than 1 cm in diameter.
- While elevated and small, a papule does **not contain fluid**, which is a key characteristic of the described lesions.
*Bulla*
- A **bulla** is a **fluid-filled lesion** that is **larger than 1 cm** in diameter.
- The lesions described are 5-6 mm, making them smaller than the definition of a bulla.
Helicobacter pylori US Medical PG Question 10: A 27-year-old previously healthy man presents to the clinic complaining of bloody diarrhea and abdominal pain. Sexual history reveals that he has sex with men and women and uses protection most of the time. He is febrile with all other vital signs within normal limits. Physical exam demonstrates tenderness to palpation of the right upper quadrant. Subsequent ultrasound shows a uniform cyst in the liver. In addition to draining the potential abscess and sending it for culture, appropriate medical therapy would involve which of the following?
- A. Supportive therapy
- B. Metronidazole and iodoquinol (Correct Answer)
- C. Sulfadiazine and pyrimethamine
- D. Nifurtimox
- E. Amphotericin
Helicobacter pylori Explanation: ***Metronidazole and iodoquinol***
- The patient's symptoms (bloody diarrhea, abdominal pain, fever, liver cyst) and risk factors (sexual activity with men and women) are highly suggestive of an **amoebic liver abscess** caused by *Entamoeba histolytica*.
- **Metronidazole** is the drug of choice for invasive amoebiasis (including liver abscess), while **iodoquinol** (or paromomycin) treats the intestinal luminal cysts to prevent recurrence and transmission.
*Supportive therapy*
- While supportive care is important for managing symptoms like fever and dehydration, it does not address the underlying **amoebic infection** or the liver abscess.
- Delaying specific antimicrobial therapy can lead to worsening of the abscess, potential rupture, and increased morbidity.
*Sulfadiazine and pyrimethamine*
- This combination is the standard treatment for **toxoplasmosis**, a protozoal infection that typically affects immunocompromised individuals and can cause encephalitis or disseminated disease.
- It is not effective against *Entamoeba histolytica* and would not resolve an amoebic liver abscess.
*Nifurtimox*
- **Nifurtimox** is an antiparasitic medication specifically used to treat **Chagas disease**, caused by *Trypanosoma cruzi*.
- Chagas disease presents with different clinical manifestations and is transmitted by blood-sucking triatomine bugs, which does not fit the patient's presentation.
*Amphotericin*
- **Amphotericin B** is a broad-spectrum **antifungal agent** used to treat severe systemic fungal infections.
- It has no activity against *Entamoeba histolytica* or other protozoal infections causing similar symptoms.
More Helicobacter pylori US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.