Escherichia coli US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Escherichia coli. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Escherichia coli US Medical PG Question 1: A 24-year-old man presents to the emergency department for bloody stools. The patient states that he has had bloody diarrhea for the past 3 days without improvement. He recently returned from a camping trip where he drank stream water and admits to eating undercooked meats which included beef, chicken, pork, and salmon. The patient's father died at age 40 due to colon cancer, and his mother died of breast cancer at the age of 52. The patient lives alone and drinks socially. The patient has unprotected sex with multiple male partners. His temperature is 98.3°F (36.8°C), blood pressure is 107/58 mmHg, pulse is 127/min, respirations are 12/min, and oxygen saturation is 99% on room air. Laboratory values are ordered as seen below.
Hemoglobin: 9.2 g/dL
Hematocrit: 29%
Leukocyte count: 9,500/mm^3 with normal differential
Platelet count: 87,000/mm^3
Lactate dehydrogenase: 327 IU/L
Haptoglobin: 5 mg/dL
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 5.9 mEq/L
HCO3-: 19 mEq/L
BUN: 39 mg/dL
Glucose: 99 mg/dL
Creatinine: 1.1 mg/dL
Ca2+: 10.2 mg/dL
Which of the following is the most likely cause of this patient's presentation?
- A. Entamoeba histolytica
- B. Campylobacter jejuni
- C. Giardia lamblia
- D. Colon cancer
- E. Escherichia coli (Correct Answer)
Escherichia coli Explanation: ***Escherichia coli***
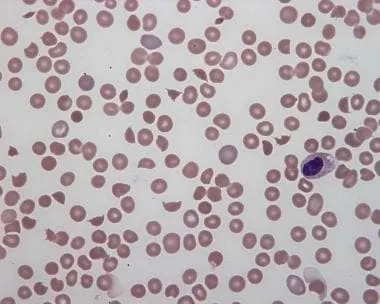
- The patient presents with **bloody diarrhea**, acute **kidney injury (elevated BUN)**, **thrombocytopenia**, and **microangiopathic hemolytic anemia** (indicated by low hemoglobin, low haptoglobin, and elevated LDH), which are classic signs of **hemolytic-uremic syndrome (HUS)**.
- HUS is most commonly caused by **Shiga toxin-producing *E. coli* (STEC)**, typically O157:H7, often acquired through consumption of **undercooked meat**.
*Entamoeba histolytica*
- This parasite causes **amoebic dysentery** (bloody diarrhea), but it typically does not lead to **hemolytic-uremic syndrome (HUS)**.
- While it can be acquired through contaminated water, the constellation of hematologic and renal findings (thrombocytopenia, AKI, hemolysis) points away from *E. histolytica*.
*Campylobacter jejuni*
- *Campylobacter jejuni* is a common cause of **bloody diarrhea** and can be acquired from undercooked poultry.
- However, it is more commonly associated with **Guillain-Barré syndrome** and **reactive arthritis**, rather than HUS.
*Giardia lamblia*
- *Giardia* typically causes **non-bloody, watery diarrhea**, often with **steatorrhea**, and is associated with camping and drinking untreated stream water.
- It does not cause bloody diarrhea, thrombocytopenia, hemolytic anemia, or acute kidney injury.
*Colon cancer*
- While colon cancer can cause **bloody stools** and the patient has a family history, his acute presentation with **severe, acute bloody diarrhea**, **thrombocytopenia**, and **renal injury** is not typical for the initial presentation of colon cancer.
- The findings are more indicative of an **acute infectious process** leading to HUS.
Escherichia coli US Medical PG Question 2: A 34-year-old, previously healthy woman is admitted to the hospital with abdominal pain and bloody diarrhea. She reports consuming undercooked beef a day before the onset of her symptoms. Her medical history is unremarkable. Vital signs include: blood pressure 100/70 mm Hg, pulse rate 70/min, respiratory rate 16/min, and temperature 36.6℃ (97.9℉). Physical examination shows paleness, face and leg edema, and abdominal tenderness in the lower right quadrant. Laboratory investigation shows the following findings:
Erythrocytes 3 x 106/mm3
Hemoglobin 9.4 g/dL
Hematocrit 0.45 (45%)
Corrected reticulocyte count 5.5%
Platelet count 18,000/mm3
Leukocytes 11,750/mm3
Total bilirubin 2.33 mg/dL (39.8 µmol/L)
Direct bilirubin 0.2 mg/dL (3.4 µmol/L)
Serum creatinine 4.5 mg/dL (397.8 µmol/L)
Blood urea nitrogen 35.4 mg/dL (12.6 mmol/L)
E. coli O157: H7 was identified in the patient’s stool. Which toxin is likely responsible for her symptoms?
- A. Erythrogenic toxin
- B. Shiga toxin (Correct Answer)
- C. Enterotoxin type B
- D. α-hemolysin
- E. Exotoxin A
Escherichia coli Explanation: ***Shiga toxin***
- The clinical presentation of **abdominal pain, bloody diarrhea, thrombocytopenia, microangiopathic hemolytic anemia** (indicated by low hemoglobin, elevated reticulocyte count, and elevated indirect bilirubin), and **acute kidney injury** (elevated creatinine and BUN with edema) strongly suggests **hemolytic uremic syndrome (HUS)**.
- ***E. coli* O157:H7** is a common cause of HUS, and it produces **Shiga toxins** (Stx1 and Stx2, also known as verotoxins), which cause endothelial damage leading to the characteristic features of HUS.
- Shiga toxins inhibit protein synthesis by cleaving ribosomal RNA, resulting in **endothelial cell damage, thrombotic microangiopathy**, and the classic triad of HUS.
*Erythrogenic toxin*
- This toxin is produced by **_Streptococcus pyogenes_** and is responsible for the rash seen in **scarlet fever**.
- It is not associated with **_E. coli_ O157:H7 infection** or the development of HUS.
*Enterotoxin type B*
- **Enterotoxin type B** is typically associated with **_Staphylococcus aureus_** and acts as a **superantigen** causing food poisoning with symptoms like vomiting and diarrhea.
- It does not cause HUS or the specific hematological and renal manifestations described in the patient.
*α-hemolysin*
- **Alpha-hemolysin** is a pore-forming cytolytic toxin produced by various bacteria, including **_Staphylococcus aureus_** and **_E. coli_**.
- While some *E. coli* strains produce alpha-hemolysin, it is not the primary toxin responsible for HUS caused by **_E. coli_ O157:H7**.
*Exotoxin A*
- **Exotoxin A** is produced by **_Pseudomonas aeruginosa_** and inhibits protein synthesis by ADP-ribosylation of elongation factor-2 (EF-2).
- It is not produced by *E. coli* O157:H7 and is not associated with HUS or the clinical presentation in this patient.
Escherichia coli US Medical PG Question 3: A 25-year-old woman has dysuria, pyuria, increased frequency of urination, and fever of 1-day duration. She is sexually active. Urine cultures show gram-positive bacteria in clusters that are catalase-positive and coagulase-negative. The patient is started on trimethoprim-sulfamethoxazole. Which of the following characteristics is used to identify the offending organism?
- A. Resistance to bacitracin
- B. Beta hemolysis
- C. Sensitivity to novobiocin
- D. Resistance to novobiocin (Correct Answer)
- E. Sensitivity to bacitracin
Escherichia coli Explanation: ***Resistance to novobiocin***
- The patient's symptoms (dysuria, pyuria, frequency, fever) and urine culture results (gram-positive cocci in clusters, catalase-positive, coagulase-negative) are highly suggestive of a **Staphylococcus saprophyticus** urinary tract infection (UTI).
- A key distinguishing characteristic of **Staphylococcus saprophyticus** from other coagulase-negative staphylococci (especially *Staphylococcus epidermidis*) is its **resistance to novobiocin**.
*Resistance to bacitracin*
- This characteristic is used to differentiate Group A Streptococcus (Streptococcus pyogenes), which is sensitive to bacitracin, from other beta-hemolytic streptococci.
- However, in this case, the organism is described as gram-positive cocci in clusters and catalase-positive, indicating Staphylococcus, not Streptococcus.
*Beta hemolysis*
- While beta hemolysis is a characteristic of certain bacteria, such as *Streptococcus pyogenes* or *Staphylococcus aureus*, it is not the primary diagnostic feature for the coagulase-negative, catalase-positive staphylococcus described here.
- Furthermore, *Staphylococcus saprophyticus* is typically non-hemolytic or weakly hemolytic.
*Sensitivity to novobiocin*
- **Sensitivity to novobiocin** is a characteristic of *Staphylococcus epidermidis* and other coagulase-negative staphylococci, but not *Staphylococcus saprophyticus*.
- Since the clinical picture points strongly to *Staphylococcus saprophyticus* in a young, sexually active female with a UTI, novobiocin resistance is the expected finding.
*Sensitivity to bacitracin*
- **Sensitivity to bacitracin** is a key characteristic used to identify *Streptococcus pyogenes* (Group A Strep).
- The organism in this scenario is a gram-positive cocci in clusters and catalase-positive, indicating a Staphylococcus species, not Streptococcus.
Escherichia coli US Medical PG Question 4: A 32-year-old man presents with a history of diarrhea several days after eating a hot dog at a neighborhood barbeque. He notes that the diarrhea is visibly bloody, but he has not experienced a fever. He adds that several other people from his neighborhood had similar complaints, many of which required hospitalization after eating food at the same barbeque. His temperature is 37°C (98.6°F ), respiratory rate is 16/min, pulse is 77/min, and blood pressure is 100/88 mm Hg. A physical examination is performed and is within normal limits. Blood is drawn for laboratory testing. The results are as follows:
Hb%: 12 gm/dL
Total count (WBC): 13,100/mm3
Differential count:
Neutrophils: 80%
Lymphocytes: 15%
Monocytes: 5%
ESR: 10 mm/hr
Glucose, Serum: 90 mg/dL
BUN: 21 mg/dL
Creatinine, Serum: 1.96 mg/dL
Sodium, Serum: 138 mmol/L
Potassium, Serum: 5.2 mmol/L
Chloride, Serum: 103 mmol/L
Bilirubin, Total: 2.5 mg/dL
Alkaline Phosphatase, Serum: 66 IU/L
Aspartate aminotransferase (AST): 32 IU/L
Alanine aminotransferase (ALT): 34 IU/L
Urinalysis is normal except for RBC casts. What is the most concerning possible complication?
- A. Disseminated intravascular coagulation
- B. Guillain-Barré syndrome
- C. Hemolytic uremic syndrome (Correct Answer)
- D. Plummer-Vinson syndrome
- E. Rotatory nystagmus
Escherichia coli Explanation: ***Hemolytic uremic syndrome***
- The patient presents with **bloody diarrhea** following suspected food poisoning (likely *E. coli O157:H7* from undercooked hot dog), elevated creatinine (1.96 mg/dL) and BUN indicating **acute kidney injury**, elevated total bilirubin (2.5 mg/dL) suggesting **hemolysis**, and **RBC casts in the urine**, which are pathognomonic for glomerular disease.
- HUS is characterized by a triad of **microangiopathic hemolytic anemia**, **thrombocytopenia**, and **acute kidney injury**. While platelet count is not provided in this case, the combination of bloody diarrhea following food exposure, evidence of hemolysis (elevated bilirubin with normal liver enzymes), acute renal failure, and RBC casts strongly suggests HUS.
- HUS is the most serious complication of **Shiga toxin-producing E. coli** infection and can lead to permanent renal damage or death if untreated.
*Disseminated intravascular coagulation*
- While DIC involves widespread clotting and bleeding, it typically presents with more severe systemic symptoms like **petechiae**, **purpura**, fever, and significant derangements in coagulation tests (e.g., prolonged PT/aPTT, decreased fibrinogen, elevated D-dimer), which are not described here.
- The localized presentation with primarily renal involvement and absence of systemic coagulopathy makes HUS more likely than DIC.
*Guillain-Barré syndrome*
- GBS is an **autoimmune disorder** affecting the peripheral nervous system, characterized by **ascending paralysis** and areflexia, usually following an infection (often *Campylobacter jejuni*).
- There are no neurological symptoms such as weakness, paresthesias, or paralysis mentioned in this patient's presentation, and the prominent renal findings point away from GBS.
*Plummer-Vinson syndrome*
- Plummer-Vinson syndrome is a rare condition characterized by **iron deficiency anemia**, **dysphagia** due to esophageal webs, and glossitis.
- This patient presents with acute GI infection and acute kidney injury, not chronic iron deficiency anemia features or dysphagia. This option is not relevant to the clinical scenario.
*Rotatory nystagmus*
- **Rotatory nystagmus** is an involuntary eye movement pattern, usually indicating a vestibular or central nervous system disorder.
- This is a physical examination finding, not a complication or syndrome. There is no mention of visual disturbances or neurological deficits in this patient's presentation.
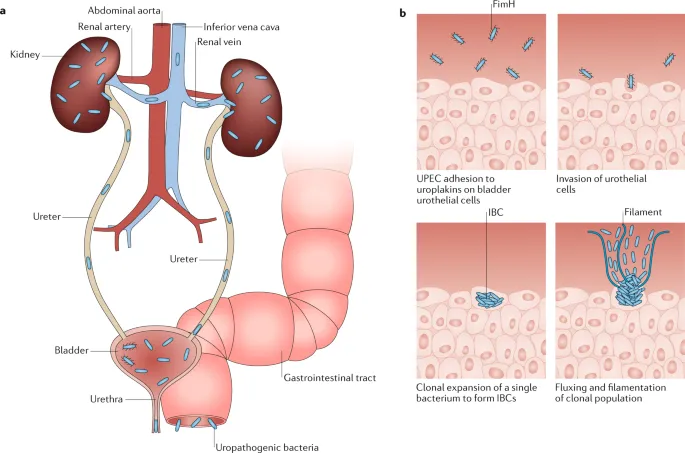
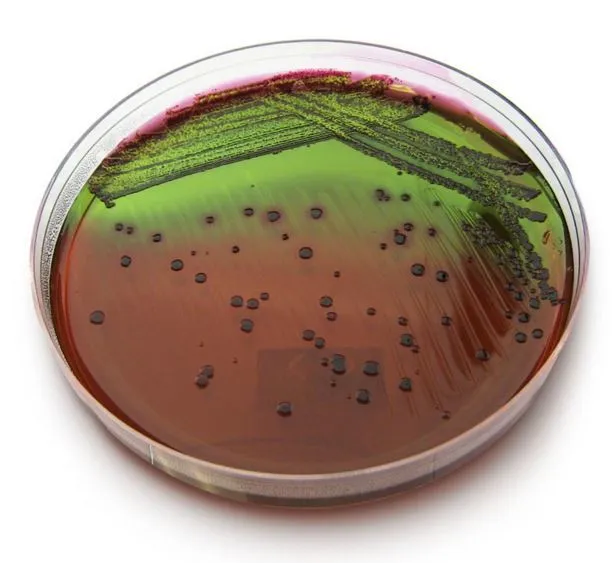
Escherichia coli US Medical PG Question 5: A previously healthy 26-year-old woman comes to the physician because of a 2-day history of pain with urination. She has been sexually active with two partners over the past year. She uses condoms for contraception. Vital signs are within normal limits. Physical examination shows suprapubic tenderness. Urinalysis shows neutrophils and a positive nitrite test. Urine culture grows gram-negative, oxidase-negative rods that form greenish colonies on eosin-methylene blue agar. Which of the following virulence factors of the causal organism increases the risk of infection in this patient?
- A. Fimbriae (Correct Answer)
- B. Lecithinase
- C. IgA protease
- D. Biofilm production
- E. Lipoteichoic acid
Escherichia coli Explanation: ***Fimbriae***
- The patient's symptoms (dysuria, suprapubic tenderness), urinalysis findings (neutrophils, positive nitrite), and culture results (gram-negative, oxidase-negative rods, greenish colonies on EMB agar) are highly suggestive of a **urinary tract infection (UTI)** caused by **Escherichia coli**.
- **P-fimbriae (pili)** are crucial virulence factors for *E. coli* in UTIs, enabling the bacteria to **adhere to uroepithelial cells** and colonize the urinary tract.
*Lecithinase*
- **Lecithinase (alpha-toxin)** is a virulence factor primarily associated with bacteria like *Clostridium perfringens*, causing gas gangrene, and some *Bacillus cereus* strains.
- It is not a significant virulence factor for *E. coli* in the context of UTIs.
*IgA protease*
- **IgA protease** is an enzyme produced by bacteria such as *Neisseria gonorrhoeae*, *Neisseria meningitidis*, and *Haemophilus influenzae*.
- It cleaves IgA antibodies, preventing their protective effects at mucosal surfaces, but it is not a primary virulence factor for *E. coli* in UTIs.
*Biofilm production*
- While *E. coli* can form biofilms, particularly in chronic infections or on catheters, **biofilm production** is not the primary mechanism that increases the **initial risk** of acquiring an acute uncomplicated UTI in a healthy individual.
- The *initial* adherence to uroepithelium, facilitated by fimbriae, is key for colonization and infection establishment.
*Lipoteichoic acid*
- **Lipoteichoic acid** is a major component of the cell wall in **Gram-positive bacteria** and contributes to their immune stimulation and adherence properties.
- The causative organism in this case is a **Gram-negative rod**, making lipoteichoic acid an irrelevant virulence factor.
Escherichia coli US Medical PG Question 6: A previously healthy 29-year-old man comes to the emergency department for a 2-day history of abdominal pain, vomiting, and watery diarrhea. Bowel movements occur every 3 hours and are non-bloody. He recently returned from a backpacking trip in Central America. He does not take any medications. Stool culture shows gram-negative, rod-shaped bacteria that ferment lactose. Which of the following toxins is most likely to be involved in the pathogenesis of this patient's symptoms?
- A. Enterotoxin B
- B. Cereulide
- C. Toxin A
- D. Heat-labile toxin (Correct Answer)
- E. Shiga toxin
Escherichia coli Explanation: ***Heat-labile toxin***
- The patient's symptoms (non-bloody watery diarrhea, vomiting) following travel to Central America are consistent with **traveler's diarrhea** caused by **enterotoxigenic Escherichia coli (ETEC)**.
- ETEC produces **heat-labile toxin (LT)**, which acts similarly to cholera toxin by activating **adenylate cyclase**, increasing **cAMP**, and leading to electrolyte and water secretion into the bowel lumen.
*Enterotoxin B*
- **Enterotoxin B** is a superantigen produced by **Staphylococcus aureus** and is primarily associated with **staphylococcal food poisoning**, characterized by rapid-onset nausea, vomiting, and non-bloody diarrhea.
- While it causes gastrointestinal symptoms, the stool culture showing a gram-negative, lactose-fermenting rod points away from **S. aureus** (a gram-positive coccus).
*Cereulide*
- **Cereulide** is a toxin produced by **Bacillus cereus**, typically associated with rapid-onset vomiting after consuming contaminated rice.
- The symptoms are more acute and the causative organism (gram-positive rod) does not match the stool culture findings.
*Toxin A*
- **Toxin A** (and Toxin B) are produced by **Clostridioides difficile** and are responsible for **pseudomembranous colitis**, characterized by severe watery diarrhea, abdominal pain, and sometimes fever, often following antibiotic use.
- The patient's presentation and the stool culture for a gram-negative, lactose-fermenting rod do not fit **C. difficile** infection.
*Shiga toxin*
- **Shiga toxin** is produced by **Shiga toxin-producing E. coli (STEC)**, including E. coli O157:H7, and **Shigella dysenteriae**.
- It typically causes **bloody diarrhea** (dysentery) and is associated with complications like **hemolytic uremic syndrome (HUS)**, which is not described in this patient's non-bloody diarrhea.
Escherichia coli US Medical PG Question 7: An investigator is studying a strain of bacteria that retains a blue color after crystal violet dye and acetone are applied. The bacteria are inoculated in a petri dish containing hypotonic saline. After the addition of an antibiotic, the bacteria swell and rupture. This antibiotic most likely belongs to which of the following classes?
- A. Macrolide
- B. Cephalosporin (Correct Answer)
- C. Sulfonamide
- D. Fluoroquinolone
- E. Tetracycline
Escherichia coli Explanation: ***Cephalosporin***
- This scenario describes a **Gram-positive bacterium** (retains blue color) which, after antibiotic treatment, swells and lyses in a hypotonic solution. This indicates a defect in the **peptidoglycan cell wall**.
- **Cephalosporins** are **β-lactam antibiotics** that inhibit bacterial cell wall synthesis by interfering with **peptidoglycan cross-linking**, leading to osmotic lysis in hypotonic environments.
*Macrolide*
- Macrolides like **azithromycin** and **erythromycin** inhibit bacterial **protein synthesis** by binding to the 50S ribosomal subunit.
- They do not directly target the cell wall, so they would not cause immediate osmotic lysis in this manner.
*Sulfonamide*
- Sulfonamides inhibit bacterial **folic acid synthesis** by acting as a competitive inhibitor of dihydropteroate synthase, disrupting DNA and RNA production.
- Their mechanism of action does not involve direct cell wall disruption or osmotic lysis.
*Fluoroquinolone*
- Fluoroquinolones interfere with bacterial **DNA replication and transcription** by inhibiting **DNA gyrase** and **topoisomerase IV**.
- This class of antibiotics does not primarily target the cell wall, and therefore would not lead to prompt osmotic swelling and rupture.
*Tetracycline*
- Tetracyclines inhibit bacterial **protein synthesis** by binding to the 30S ribosomal subunit, preventing the attachment of aminoacyl-tRNA.
- They do not affect the cell wall, so they would not cause the observed osmotic lysis.
Escherichia coli US Medical PG Question 8: A 59-year-old man comes to the physician because of urinary frequency and perineal pain for the past 3 days. During this time, he has also had pain with defecation. He is sexually active with his wife only. His temperature is 39.1°C (102.3°F). His penis and scrotum appear normal. Digital rectal examination shows a swollen, exquisitely tender prostate. His leukocyte count is 13,400/mm3. A urine culture obtained prior to initiating treatment is most likely to show which of the following?
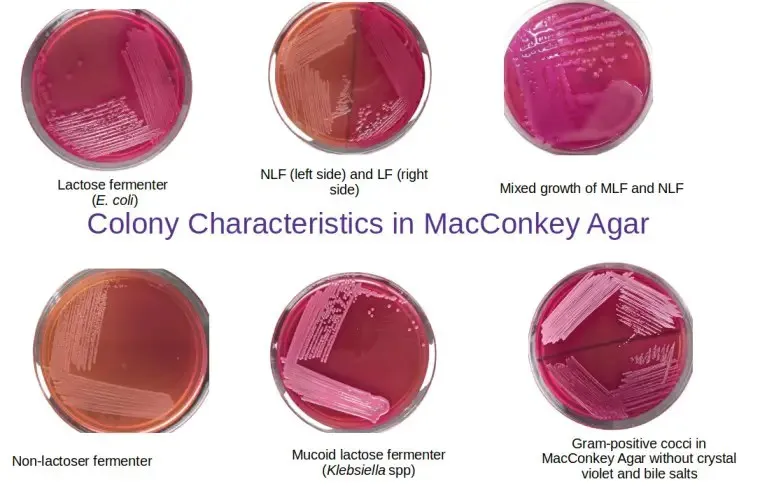
- A. Gram-negative, lactose-fermenting rods in pink colonies (Correct Answer)
- B. Gram-negative, oxidase-positive rods in green colonies
- C. Gram-negative, encapsulated rods in mucoid colonies
- D. Gram-negative, aerobic, intracellular diplococci
- E. Weakly staining, obligate intracellular bacilli
Escherichia coli Explanation: ***Gram-negative, lactose-fermenting rods in pink colonies***
- The patient's symptoms (urinary frequency, perineal pain, fever, tender prostate) are highly suggestive of **acute bacterial prostatitis**.
- **Uropathogenic Escherichia coli** (a Gram-negative, lactose-fermenting rod) is the most common cause of acute bacterial prostatitis and UTIs, typically producing pink colonies on **MacConkey agar**.
*Gram-negative, oxidase-positive rods in green colonies*
- This description typically fits *Pseudomonas aeruginosa*, which can cause UTIs but is less common in uncomplicated acute prostatitis and often produces a characteristic **green pigment** and fruity odor.
- *Pseudomonas* infections are more frequently seen in **hospital-acquired infections** or in patients with indwelling catheters or immunocompromise.
*Gram-negative, encapsulated rods in mucoid colonies*
- This describes organisms like **Klebsiella pneumoniae**, which can cause UTIs and prostatitis, often presenting with **mucoid colonies** due to their prominent capsule.
- While possible, *Klebsiella* is less common than *E. coli* in uncomplicated community-acquired prostatitis.
*Gram-negative, aerobic, intracellular diplococci*
- This description refers to **Neisseria gonorrhoeae**, which causes **gonorrhea**, a sexually transmitted infection.
- While it can cause urethritis, it is not a typical cause of acute bacterial prostatitis in a patient described as exclusively sexually active with his wife and without urethral discharge.
- *N. gonorrhoeae* requires **specialized culture media** (Thayer-Martin agar) and is not routinely detected on standard urine culture media; modern diagnosis typically uses NAAT/PCR testing.
*Weakly staining, obligate intracellular bacilli*
- This description refers to organisms like **Chlamydia trachomatis** or **Rickettsia** species.
- *Chlamydia* can cause urethritis and, less commonly, epididymitis, but it typically causes a more subacute prostatitis if involved and requires specialized non-culture-based testing (e.g., PCR) for detection due to its obligate intracellular nature.
Escherichia coli US Medical PG Question 9: An investigator is studying the immune response and the spleen in a mouse model infected with Escherichia coli. Which of the following anatomical sites in the spleen is important for the secondary maturation and affinity maturation of B cells that will ultimately target Escherichia coli?
- A. Sinusoids
- B. Periarteriolar lymphatic sheaths
- C. Marginal zone
- D. Red pulp
- E. Germinal center (Correct Answer)
Escherichia coli Explanation: ***Germinal center***
- The **germinal centers** are the primary sites within secondary lymphoid organs, including the spleen, where B cells undergo **proliferation**, **somatic hypermutation**, and **affinity maturation** following antigen exposure.
- This process is crucial for generating high-affinity antibodies capable of effectively targeting pathogens like *Escherichia coli*.
*Sinusoids*
- **Sinusoids** are specialized vascular channels found throughout the spleen, particularly in the red pulp, responsible for filtering blood and removing old or damaged red blood cells.
- They are not directly involved in the secondary maturation or affinity maturation of B cells.
*Periarteriolar lymphatic sheaths*
- The **periarteriolar lymphatic sheaths (PALS)** are T-cell rich areas in the white pulp of the spleen, surrounding central arterioles.
- While important for T-cell activation, the main site for B-cell affinity maturation is the germinal center, which forms within B cell follicles adjacent to the PALS.
*Marginal zone*
- The **marginal zone** is a specialized area at the periphery of the white pulp, rich in unique B cell populations that respond rapidly to T-cell independent antigens.
- While it plays a role in initial immune responses, it is not the primary site for the secondary maturation and affinity maturation of B cells.
*Red pulp*
- The **red pulp** makes up the majority of the spleen and is primarily involved in filtering blood, removing old red blood cells, and storing platelets.
- While it contains macrophages and other immune cells, it is not the main site for B-cell secondary maturation and affinity maturation, which occurs in the white pulp's germinal centers.
Escherichia coli US Medical PG Question 10: An 87-year-old woman is brought to the emergency department from her nursing home because of increasing confusion and lethargy for 12 hours. The nursing home aide says she did not want to get out of bed this morning and seemed less responsive than usual. She has Alzheimer's disease, hypertension, and a history of nephrolithiasis. She has chronic, intractable urinary incontinence, for which she has an indwelling urinary catheter. Current medications include galantamine, memantine, and ramipril. Her temperature is 38.5°C (101.3°F), pulse is 112/min, respiratory rate is 16/min, and blood pressure is 108/76 mm Hg. Physical examination shows mild tenderness to palpation of the lower abdomen. On mental status examination, she is oriented only to person. Laboratory studies show:
Hemoglobin 12.4 g/dL
Leukocyte count 9,000/mm3
Platelet count 355,000/mm3
Urine
pH 8.2
Glucose 1+
Protein 2+
Ketones negative
RBC 5/hpf
WBC 35/hpf
Bacteria moderate
Nitrites positive
Which of the following is the most likely causal organism?
- A. Enterococcus faecalis
- B. Klebsiella pneumoniae
- C. Staphylococcus saprophyticus
- D. Escherichia coli
- E. Proteus mirabilis (Correct Answer)
Escherichia coli Explanation: ***Proteus mirabilis***
- The high urine pH (8.2), positive nitrites, and moderate bacteria, along with signs of infection in an elderly catheterized patient, are highly suggestive of a **urea-splitting organism**.
- **Proteus mirabilis** is a common cause of catheter-associated UTIs and produces urease, leading to alkaline urine and the formation of struvite stones, consistent with the patient's history of nephrolithiasis.
*Enterococcus faecalis*
- While *Enterococcus faecalis* can cause UTIs, it typically does not produce urease and therefore would not cause such a **markedly elevated urine pH** (above 7.5).
- Although it can cause positive nitrites, the absence of a strong alkali pH makes it less likely than *Proteus mirabilis*.
*Klebsiella pneumoniae*
- *Klebsiella pneumoniae* can cause UTIs and produce nitrites, but it is not typically a strong **urease producer** to the extent that would cause an alkaline urine pH of 8.2.
- It is more commonly associated with nosocomial infections, but the highly alkaline urine points away from it as the most likely cause here.
*Staphylococcus saprophyticus*
- *Staphylococcus saprophyticus* is a common cause of UTIs in young, sexually active women, but it is **rare in elderly, catheterized patients**.
- It is also not typically associated with such a high urine pH as seen in this case.
*Escherichia coli*
- *Escherichia coli* is the most common cause of UTIs, but it is a **non-urease-producing** bacterium and would typically result in acidic urine, or at least a less alkaline pH than 8.2.
- While it would cause positive nitrites and moderate bacteria, the elevated pH makes it less likely than *Proteus mirabilis* in this context.
More Escherichia coli US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.