Treatment of dimorphic fungal infections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Treatment of dimorphic fungal infections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
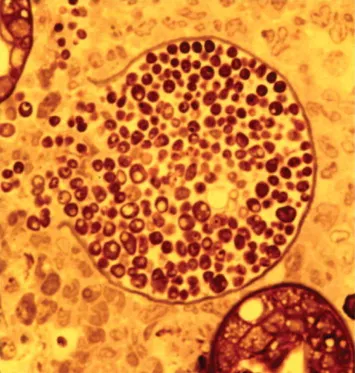
Treatment of dimorphic fungal infections US Medical PG Question 1: A 44-year-old man comes to the physician because of a 3-week history of productive cough, fever, and lethargy. He also has several skin lesions over his body. His symptoms began 3 weeks after he returned from a camping trip in Kentucky. Three years ago, he underwent kidney transplantation for polycystic kidney disease. Current medications include sirolimus and prednisone. His temperature is 38°C (100.4°F). Diffuse crackles are heard over the lung fields. There are 4 white, verrucous skin patches over his chest and upper limbs. A photomicrograph of a skin biopsy specimen from one of the lesions is shown. Which of the following is the most likely diagnosis?
- A. Coccidioidomycosis
- B. Mucormycosis
- C. Blastomycosis (Correct Answer)
- D. Cryptococcosis
- E. Histoplasmosis
Treatment of dimorphic fungal infections Explanation: ***Blastomycosis***
- The patient's history of **camping in Kentucky**, along with the presence of **pulmonary symptoms** (productive cough, fever, crackles) and **verrucous skin lesions**, are classic for blastomycosis.
- The photomicrograph showing **broad-based budding yeast** is pathognomonic for *Blastomyces dermatitidis*.
*Coccidioidomycosis*
- This is typical in the **Southwestern United States and parts of Mexico**, not Kentucky.
- Microscopic examination would reveal **spherules containing endospores**, which are not seen in the provided image.
*Mucormycosis*
- This infection is characterized by **irregular, broad, non-septate hyphae** with **wide-angle branching**, often invading blood vessels, leading to tissue necrosis.
- It primarily affects immunocompromised patients but typically presents as **rhinocerebral** or **pulmonary infection**, less commonly with verrucous skin lesions of this type.
*Cryptococcosis*
- Primarily affects the **lungs and central nervous system**, especially in immunocompromised individuals.
- Microscopy typically shows **encapsulated yeast** cells, which would be visible with India ink stain, and are not represented by the broad-based budding in the image.
*Histoplasmosis*
- Prevalent in the **Ohio and Mississippi River Valleys**, which includes Kentucky, and is often associated with **bird or bat droppings**.
- On microscopy, it presents as **small intracellular yeast** within macrophages, which is morphologically distinct from the large, broad-based budding yeast shown.
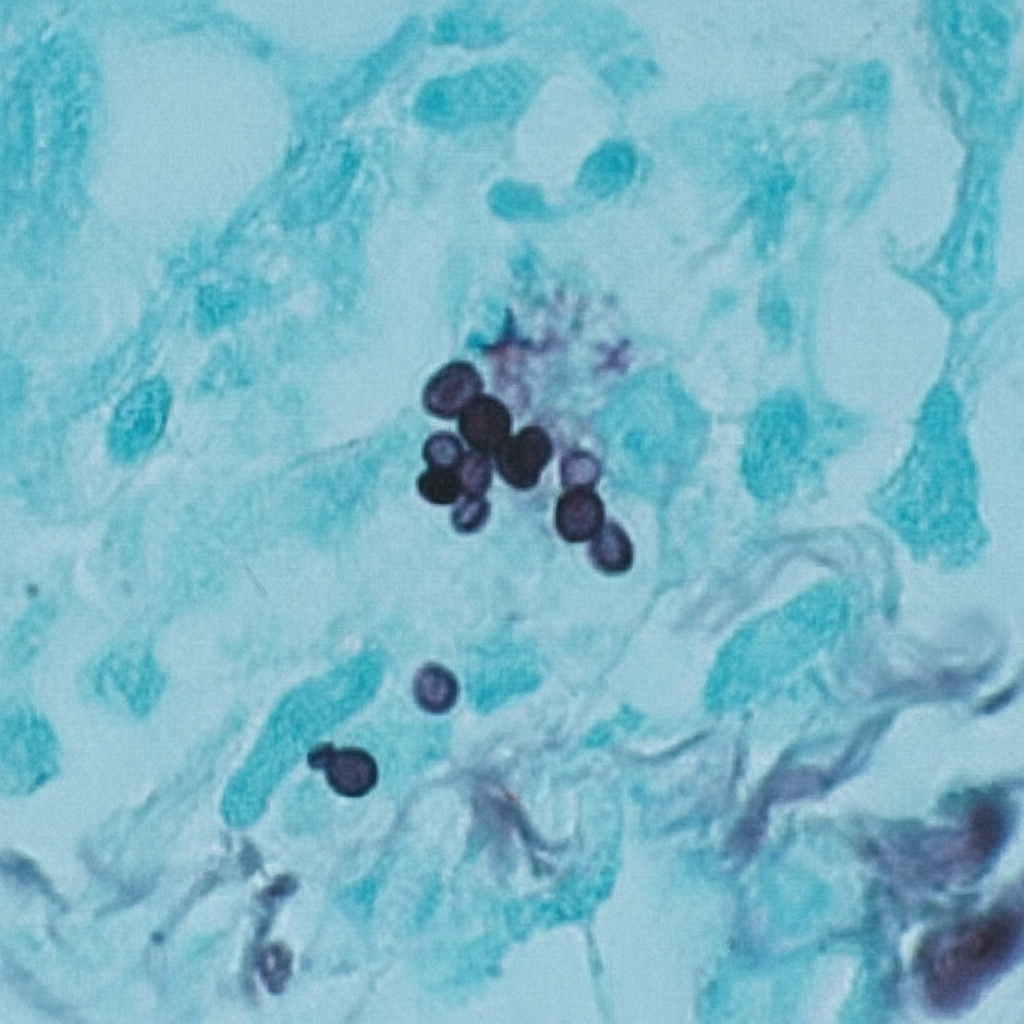
Treatment of dimorphic fungal infections US Medical PG Question 2: A 52-year-old man comes to the physician because of a 4-day history of a productive cough, shortness of breath, and low-grade fever. He works as a farmer in southern Arizona. Physical examination shows multiple skin lesions with a dark blue center, pale intermediate zone, and red peripheral rim on the upper and lower extremities. There are diffuse crackles on the left side of the chest. An x-ray of the chest shows left basilar consolidation and left hilar lymphadenopathy. A photomicrograph of tissue obtained from a biopsy of the lung is shown. Which of the following is the most likely causal pathogen?
- A. Coccidioides immitis (Correct Answer)
- B. Paracoccidioides brasiliensis
- C. Candida albicans
- D. Blastomyces dermatitidis
- E. Aspergillus fumigatus
Treatment of dimorphic fungal infections Explanation: ***Coccidioides immitis***
- The patient's presentation with **respiratory symptoms**, **skin lesions** (erythema multiforme-like), and **hilar lymphadenopathy** in a farmer from **southern Arizona** is highly characteristic of coccidioidomycosis. The image shows **spherules** containing **endospores**, which are diagnostic of *Coccidioides*.
- *Coccidioides immitis* is a **dimorphic fungus** endemic to the **Southwestern United States** (including Arizona) and parts of Mexico and Central/South America, commonly causing **valley fever**.
*Paracoccidioides brasiliensis*
- This fungus is associated with **Paracoccidioidomycosis**, which is primarily found in **Latin America** (excluding the US Southwest).
- Microscopically, it presents as a **captain's wheel** appearance with multiple buds, which is not seen here.
*Candida albicans*
- *Candida albicans* is a **yeast** that typically causes **mucocutaneous infections** (e.g., thrush, vaginitis) and can cause systemic candidiasis in immunocompromised individuals.
- It forms **pseudohyphae and budding yeasts** microscopically, which are distinct from the spherules seen in the image.
*Blastomyces dermatitidis*
- **Blastomycosis** is endemic to the **Great Lakes region and Ohio/Mississippi River valleys** and usually presents with pneumonia and skin lesions.
- Microscopic examination reveals **broad-based budding yeasts**, which are different from the features shown in the image.
*Aspergillus fumigatus*
- *Aspergillus fumigatus* causes various conditions, including allergic bronchopulmonary aspergillosis (ABPA), aspergilloma, and invasive aspergillosis, particularly in **immunocompromised patients**.
- Microscopically, it is characterized by **acute-angle branching septate hyphae**, which is not consistent with the image provided.
Treatment of dimorphic fungal infections US Medical PG Question 3: A 25-year-old nulligravid female presents to clinic complaining of abnormal vaginal discharge and vaginal pruritis. The patient's past medical history is unremarkable and she does not take any medications. She is sexually active with 3 male partners and does not use condoms. Pelvic examination is notable for a thick, odorless, white discharge. There is marked erythema and edema of the vulva. Vaginal pH is normal. Microscopic viewing of the discharge shows pseudohyphae and white blood cells. Which of the following is the most appropriate treatment plan?
- A. Oral fluconazole for the patient (Correct Answer)
- B. Topical metronidazole
- C. Oral clindamycin for the patient
- D. Oral fluconazole for the patient and her partner
- E. Oral clindamycin for the patient and her partner
Treatment of dimorphic fungal infections Explanation: ***Oral fluconazole for the patient***
- The symptoms of **thick, odorless, white discharge**, **marked vulvar erythema and edema**, **normal vaginal pH**, and most importantly, the presence of **pseudohyphae** on microscopic examination are all characteristic findings of **vulvovaginal candidiasis**.
- **Oral fluconazole** is a first-line treatment for uncomplicated vulvovaginal candidiasis, effectively targeting the fungal overgrowth.
*Topical metronidazole*
- **Metronidazole** is an antibiotic primarily used to treat **bacterial vaginosis** and **trichomoniasis**.
- Microscopic examination showing **pseudohyphae** rules out bacterial vaginosis and trichomoniasis, making metronidazole an ineffective treatment for candidiasis.
*Oral clindamycin for the patient*
- **Clindamycin** is an antibiotic effective against certain bacterial infections, including **bacterial vaginosis**.
- It is not effective against **fungal infections** like candidiasis.
*Oral fluconazole for the patient and her partner*
- While **oral fluconazole** is appropriate for the patient, routine treatment of male sexual partners for **vulvovaginal candidiasis** is **not typically recommended** unless the partner also exhibits symptoms of balanitis or the patient experiences recurrent infections.
- **Candidiasis is not considered a sexually transmitted infection (STI)** because it often occurs in sexually inactive women and successful treatment does not depend on partner treatment.
*Oral clindamycin for the patient and her partner*
- **Clindamycin** is not effective against **fungal infections**.
- Furthermore, routine partner treatment for vaginal candidiasis with any medication is generally **not indicated**.
Treatment of dimorphic fungal infections US Medical PG Question 4: A 29-year-old woman comes to the military physician because of a 2-day history of fever, joint pain, dry cough, chest pain, and a painful red rash on her lower legs. Two weeks ago, she returned from military training in Southern California. She appears ill. Her temperature is 39°C (102.1°F). Physical examination shows diffuse inspiratory crackles over all lung fields and multiple tender erythematous nodules over the anterior aspect of both legs. A biopsy specimen of this patient's lungs is most likely to show which of the following?
- A. Septate hyphae with acute-angle branching
- B. Spherules filled with endospores (Correct Answer)
- C. Broad-based budding yeast
- D. Encapsulated yeast with narrow-based budding
- E. Oval, budding yeast with pseudohyphae
Treatment of dimorphic fungal infections Explanation: **Spherules filled with endospores**
- The patient's symptoms (fever, joint pain, dry cough, chest pain, erythema nodosum on legs) combined with her travel history to **Southern California** are highly suggestive of **Coccidioidomycosis** ("Valley Fever").
- A biopsy of affected lung tissue in coccidioidomycosis typically reveals **spherules** (thick-walled structures) containing numerous **endospores**, which are characteristic of the tissue phase of *Coccidioides immitis/posadasii*.
*Septate hyphae with acute-angle branching*
- This morphology is characteristic of **Aspergillus** species, which can cause opportunistic infections, especially in immunocompromised individuals.
- While it can cause lung infections, the clinical presentation and geographic exposure do not point towards aspergillosis as the most likely diagnosis.
*Broad-based budding yeast*
- This describes the characteristic morphology of *Blastomyces dermatitidis*, the causative agent of **Blastomycosis**.
- **Blastomycosis** is typically found in the Great Lakes region, Ohio, Mississippi River valleys, and southeastern United States, not Southern California.
*Encapsulated yeast with narrow-based budding*
- This describes **Cryptococcus neoformans**, which appears as an encapsulated yeast with narrow-based budding in tissue.
- While it can cause pulmonary disease, the classic presentation (erythema nodosum, acute illness after Southern California exposure) is not consistent with **cryptococcosis**, which typically presents subacutely in immunocompromised patients.
*Oval, budding yeast with pseudohyphae*
- This morphology is characteristic of *Candida albicans*, which commonly causes mucocutaneous infections and can cause systemic candidiasis, particularly in immunocompromised patients.
- The clinical picture of a healthy young woman with exposure in Southern California does not fit with a typical **Candida** infection.
Treatment of dimorphic fungal infections US Medical PG Question 5: A 73-year-old man presents to the office, complaining of “weird blisters” on his right hand, which appeared 2 weeks ago. The patient says that he initially had a rash, which progressed to blisters. He denies any trauma or known contact with sick people. He is worried because he hasn’t been able to garden since the rash appeared, and he was planning on entering his roses into an annual competition this month. His vital signs are stable. On physical exam, the patient has multiple bullae accompanied by red, papular lesions on his right hand, which progress to his forearm. The right axillary lymph nodes are swollen and tender. What is the treatment for the most likely diagnosis of this patient?
- A. Itraconazole (Correct Answer)
- B. Azithromycin
- C. Topical corticosteroids
- D. Doxycycline
- E. Potassium iodide solution
Treatment of dimorphic fungal infections Explanation: ***Itraconazole***
- This patient likely has **sporotrichosis**, a subcutaneous fungal infection, given the history of **gardening** (exposure to soil/plants), **papular lesions progressing to blisters**, and **lymphatic spread** (swollen axillary lymph nodes).
- **Itraconazole** is the **first-line treatment** for cutaneous and lymphocutaneous sporotrichosis.
*Azithromycin*
- **Azithromycin** is an **antibiotic** used to treat bacterial infections, not fungal infections like sporotrichosis.
- It is often used for respiratory tract infections, sexually transmitted infections, and some skin infections.
*Topical corticosteroids*
- **Topical corticosteroids** are anti-inflammatory agents that would likely worsen a fungal infection by suppressing the immune response.
- They are used for inflammatory dermatoses like eczema or psoriasis and would not be effective against sporotrichosis.
*Doxycycline*
- **Doxycycline** is a broad-spectrum **antibiotic**, effective against a variety of bacterial infections, including some atypical pathogens.
- It has no antifungal activity and would not be an appropriate treatment for sporotrichosis.
*Potassium iodide solution*
- While traditionally used for sporotrichosis, **potassium iodide (KI) solution** is now considered a **second-line treatment** due to its side effects and the availability of more effective and safer antifungals like itraconazole.
- It is used only in cases where itraconazole is contraindicated or ineffective.
Treatment of dimorphic fungal infections US Medical PG Question 6: A 74-year-old man is admitted to the medical ward after he developed a fungal infection. He has aplastic anemia. The most recent absolute neutrophil count was 450/µL. An anti-fungal agent is administered that inhibits the fungal enzyme, (1→3)-β-D-glucan synthase, and thereby disrupts the integrity of the fungal cell wall. He responds well to the treatment. Although amphotericin B is more efficacious for his condition, it was not used because of the side effect profile. What was the most likely infection?
- A. Invasive aspergillosis
- B. Mucormycosis
- C. Histoplasmosis
- D. Paracoccidioidomycosis
- E. Candidemia (Correct Answer)
Treatment of dimorphic fungal infections Explanation: ***Candidemia***
- The patient's **neutropenia** (absolute neutrophil count of 450/µL) due to aplastic anemia is a major risk factor for invasive candidiasis, including candidemia.
- The antifungal agent's mechanism of action, targeting **(1→3)-β-D-glucan synthase**, is characteristic of **echinocandins**, which are first-line agents for candidemia, especially in critically ill or neutropenic patients, and often preferred over amphotericin B due to a better side effect profile.
*Invasive aspergillosis*
- While neutropenia is a significant risk factor for invasive aspergillosis, the primary antifungal drugs for this condition are typically **voriconazole** or **isavuconazole**, although echinocandins may be used as salvage therapy or in combination.
- The description of the drug's mechanism specifically targeting **(1→3)-β-D-glucan synthase** does not make aspergillosis the *most likely* infection, as some Aspergillus species may have less β-D-glucan in their cell walls compared to *Candida*.
*Mucormycosis*
- This aggressive fungal infection is often seen in immunocompromised patients, particularly those with **diabetes** or profound neutropenia, but the primary treatment is usually **amphotericin B**.
- Mucorales fungi typically **lack ergosterol** and their cell walls do not contain **(1→3)-β-D-glucan**, making echinocandins ineffective.
*Histoplasmosis*
- This is a dimorphic fungal infection endemic to certain geographic regions, primarily affecting the lungs and disseminating in immunocompromised individuals.
- The drug of choice for severe or disseminated histoplasmosis is **amphotericin B**, followed by azoles; echinocandins are generally not active against *Histoplasma*.
*Paracoccidioidomycosis*
- This is a chronic systemic mycosis found in Latin America, primarily affecting the lungs, skin, and lymph nodes.
- Treatment for severe forms typically involves **amphotericin B**, followed by sulfonamides or azoles for maintenance; echinocandins are not effective against *Paracoccidioides*.
Treatment of dimorphic fungal infections US Medical PG Question 7: A 32-year-old woman presents with three-days of vaginal burning, itching, and pain with intercourse. She is in a monogamous relationship with her husband and has an intrauterine device for contraception. Her past medical history is unremarkable, except for recently being treated with antibiotics for sinusitis. Pelvic exam is remarkable for vulvar excoriations, vaginal wall edema, and thick, white discharge in the vault. Wet mount with KOH staining reveals budding filaments with pseudohyphae and hyphae. Which of the following is the most appropriate treatment?
- A. Voriconazole
- B. Posaconazole
- C. Metronidazole
- D. Itraconazole
- E. Fluconazole (Correct Answer)
Treatment of dimorphic fungal infections Explanation: ***Fluconazole***
- The patient's symptoms (vaginal burning, itching, pain with intercourse, thick, white discharge) and **wet mount findings (budding filaments with pseudohyphae and hyphae)** are classic for **vulvovaginal candidiasis (VVC)**, often precipitated by recent antibiotic use.
- **Fluconazole** is a highly effective and commonly prescribed oral antifungal for uncomplicated VVC due to its convenience and excellent therapeutic profile.
*Voriconazole*
- **Voriconazole** is a broad-spectrum triazole antifungal primarily used for invasive fungal infections, such as **invasive aspergillosis** and candidemia, and is not a first-line treatment for uncomplicated VVC.
- Its use is typically reserved for more severe or refractory systemic fungal infections, and it has a more significant side effect profile than fluconazole.
*Posaconazole*
- **Posaconazole** is another extended-spectrum triazole antifungal primarily used for the prophylaxis and treatment of **invasive fungal infections** in immunocompromised patients, particularly those unresponsive to other antifungals.
- It is not indicated for the treatment of uncomplicated vulvovaginal candidiasis.
*Metronidazole*
- **Metronidazole** is an antibiotic and antiprotozoal agent used to treat bacterial vaginosis and trichomoniasis, both of which are common causes of vaginitis.
- It is **ineffective against fungal infections**, and the patient's symptoms and wet mount findings rule out bacterial vaginosis and trichomoniasis.
*Itraconazole*
- **Itraconazole** is an antifungal drug effective against superficial and systemic fungal infections, but it is typically used for more severe or recurrent VVC, or in cases of non-albicans Candida species.
- While effective, **fluconazole** is generally preferred as the first-line oral treatment for uncomplicated VVC due to its single-dose efficacy and established safety profile for this indication.
Treatment of dimorphic fungal infections US Medical PG Question 8: A 40-year-old farmer from Ohio seeks evaluation at a clinic with complaints of a chronic cough, fevers, and anorexia of several months duration. On examination, he has generalized lymphadenopathy with hepatosplenomegaly. A chest radiograph reveals local infiltrates and patchy opacities involving all lung fields. Fine needle aspiration of an enlarged lymph node shows the presence of intracellular yeast. A fungal culture shows the presence of smooth, thin-walled microconidia and tuberculate macroconidia. Which of the following is the most likely diagnosis?
- A. Coccidioidomycosis
- B. Blastomycosis
- C. Cryptococcosis
- D. Histoplasmosis (Correct Answer)
- E. Sporotrichosis
Treatment of dimorphic fungal infections Explanation: ***Histoplasmosis***
- **Histoplasmosis** is characterized by the presence of **intracellular yeast** in tissue samples and **tuberculate macroconidia** in fungal cultures, which are key diagnostic findings in this case.
- The patient's presentation with chronic cough, fevers, anorexia, generalized lymphadenopathy, hepatosplenomegaly, and lung infiltrates, along with geographic exposure in **Ohio** (part of the Ohio River Valley endemic area), is highly consistent with disseminated histoplasmosis.
*Coccidioidomycosis*
- While coccidioidomycosis can cause lung infiltrates, it is typically endemic to the **southwestern United States** and Mexico, not Ohio.
- Microscopic examination would reveal **spherules** containing endospores, not intracellular yeast with tuberculate macroconidia.
*Blastomycosis*
- Blastomycosis is also endemic to the Ohio River Valley, but it is characterized by **broad-based budding yeast** in tissue, and its cultures typically do not show tuberculate macroconidia.
- While it causes pulmonary and disseminated disease, the specific microscopic and culture findings differentiate it from histoplasmosis.
*Cryptococcosis*
- Cryptococcosis primarily affects immunocompromised individuals and is characterized by encapsulated yeast, which would be visible with India ink stain.
- It typically presents as **meningitis** or pneumonia, and its culture morphology does not include tuberculate macroconidia.
*Sporotrichosis*
- Sporotrichosis is commonly associated with **cutaneous lesions** following traumatic inoculation of spores from soil or vegetation, and it rarely causes disseminated disease with extensive systemic symptoms like those described.
- The yeast forms in tissue are typically smaller and cigar-shaped, and the culture morphology differs significantly from what is described.
Treatment of dimorphic fungal infections US Medical PG Question 9: A 62-year-old man is brought to the emergency department from a senior-care facility after he was found with a decreased level of consciousness and fever. His personal history is relevant for colorectal cancer that was managed with surgical excision of the tumor. Upon admission, he is found to have a blood pressure of 130/80 mm Hg, a pulse of 102/min, a respiratory rate of 20/min, and a body temperature 38.8°C (101.8°F). There is no rash on physical examination; he is found to have neck rigidity, confusion, and photophobia. There are no focal neurological deficits. A head CT is normal without mass or hydrocephalus. A lumbar puncture was performed and cerebrospinal fluid (CSF) is sent to analysis while ceftriaxone and vancomycin are started. Which of the following additional antimicrobials should be added in the management of this patient?
- A. Trimethoprim-sulfamethoxazole (TMP-SMX)
- B. Ampicillin (Correct Answer)
- C. Amphotericin
- D. Meropenem
- E. Clindamycin
Treatment of dimorphic fungal infections Explanation: ***Ampicillin***
- This patient is a 62-year-old, indicating an increased risk for **Listeria monocytogenes** meningitis, which is typically susceptible to ampicillin.
- Given his age and presentation with **meningeal signs** and fever, empirical coverage for Listeria with ampicillin is crucial, especially before CSF culture results are known.
*Trimethoprim-sulfamethoxazole (TMP-SMX)*
- While TMP-SMX can cover Listeria, it is generally considered a **second-line agent** for severe infections like meningitis due to slower bactericidal activity and potential for higher rates of treatment failure compared to ampicillin.
- Ampicillin is the **preferred first-line treatment** for Listeria meningitis unless there is a specific contraindication.
*Amphotericin*
- Amphotericin is an **antifungal agent** used for fungal meningitis.
- Although fungemia can occur in immunocompromised individuals or those with indwelling catheters, the initial presentation with bacterial meningitis symptoms and absence of specific risk factors for fungal infection do not support its empirical use.
*Meropenem*
- Meropenem is a **carbapenem** with a broad spectrum of activity, including many gram-negative and gram-positive bacteria, and some anaerobes.
- While it has good CNS penetration and could cover some organisms like penicillin-resistant S. pneumoniae or gram-negative rods, it is not the primary empirical choice specifically for **Listeria monocytogenes**, and there's no indication for its broad-spectrum coverage over standard empirical therapy currently.
*Clindamycin*
- Clindamycin is primarily active against **gram-positive bacteria**, especially anaerobes and some staphylococci and streptococci.
- It has **poor penetration into the CNS** and is therefore not effective for meningitis treatment, especially for common bacterial pathogens or Listeria.
Treatment of dimorphic fungal infections US Medical PG Question 10: A 30-year-old man is admitted to the hospital with a presumed pneumonia and started on antibiotics. Two days later, the patient shows no improvement. Blood cultures reveal yeast with pseudophyphae. Which of the following cell types is most likely deficient or dysfunctional in this patient?
- A. Eosinophils
- B. Macrophages
- C. Neutrophils (Correct Answer)
- D. T-cells
- E. B-cells
Treatment of dimorphic fungal infections Explanation: ***Neutrophils***
- The presence of **yeast with pseudohyphae** in blood cultures, particularly *Candida*, indicates a fungal infection.
- **Neutrophils** are crucial for the host defense against *Candida* and other fungal pathogens, so their deficiency or dysfunction would predispose to candidemia.
- Neutropenia or neutrophil dysfunction (e.g., chronic granulomatous disease) significantly increases risk of invasive candidiasis.
*Eosinophils*
- **Eosinophils** are primarily involved in defense against **parasitic infections** and in allergic reactions.
- They play a minimal role in the immune response to systemic fungal infections like candidemia.
*Macrophages*
- **Macrophages** are phagocytic cells that contribute to antifungal immunity, particularly in tissue surveillance and chronic infection control.
- However, **neutrophils** are the primary and most critical defense against acute *Candida* bloodstream infections.
- Macrophage deficiency alone does not typically predispose to candidemia as severely as neutrophil deficiency.
*T-cells*
- **T-cells** are important for cell-mediated immunity, particularly against **intracellular pathogens** and viral infections.
- While they play a role in modulating antifungal responses, their deficiency typically leads to infections with *Pneumocystis jirovecii* or severe mucocutaneous candidiasis, rather than disseminated candidemia.
*B-cells*
- **B-cells** are responsible for **humoral immunity** through antibody production, which is primarily effective against extracellular bacteria and toxins.
- They are not the primary line of defense against fungal infections such as candidemia.
More Treatment of dimorphic fungal infections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.