Sporothrix schenckii complex US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Sporothrix schenckii complex. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Sporothrix schenckii complex US Medical PG Question 1: A previously healthy 52-year-old woman comes to the physician because of a 1-week history of productive cough, fevers, and malaise. She has smoked one pack of cigarettes daily for 35 years. Her temperature is 39°C (102.2°F). Diffuse inspiratory crackles are heard bilaterally. Her leukocyte count is 14,300/mm3. Sputum analysis shows numerous polymorphonuclear leukocytes and a few squamous epithelial cells. An x-ray of the chest shows bilateral patchy consolidations. Which of the following findings on sputum culture is most consistent with this patient's respiratory symptoms?
- A. Anaerobic gram-positive, branching, filamentous bacilli
- B. Gram-positive, alpha-hemolytic, optochin-resistant cocci in chains
- C. Encapsulated, pleomorphic, gram-negative coccobacilli (Correct Answer)
- D. Pseudohyphae with budding yeasts at 20°C
- E. Gram-positive, catalase-positive, coagulase-negative cocci in clusters
Sporothrix schenckii complex Explanation: ***Encapsulated, pleomorphic, gram-negative coccobacilli***
- This description is characteristic of ***Haemophilus influenzae***, a common cause of **community-acquired pneumonia**, especially in patients with a history of **smoking** and **COPD**.
- The clinical presentation with productive cough, fever, malaise, bilateral patchy consolidations, and leukocytosis is highly consistent with bacterial pneumonia caused by this organism.
*Anaerobic gram-positive, branching, filamentous bacilli*
- This describes organisms like ***Actinomyces***, which typically cause **abscesses**, **fistulas**, and granulomatous lesions, rather than acute community-acquired pneumonia.
- The patient's acute symptoms and diffuse infiltrates are not typical for **actinomycosis**.
*Gram-positive, alpha-hemolytic, optochin-resistant cocci in chains*
- This morphology (alpha-hemolytic, optochin-resistant cocci in chains) describes ***Streptococcus viridans***.
- While *S. viridans* can cause infections, it is not a primary cause of **community-acquired pneumonia**; it is more commonly associated with **endocarditis** or oral infections.
*Pseudohyphae with budding yeasts at 20°C*
- This describes a **fungal pathogen**, possibly *Candida albicans*, which forms **pseudohyphae** and **budding yeasts**.
- While *Candida* can cause lung infections, it is usually seen in **immunocompromised individuals** or those with prolonged antibiotic use, which is not suggested here.
*Gram-positive, catalase-positive, coagulase-negative cocci in clusters*
- This describes **coagulase-negative *Staphylococcus***, such as *Staphylococcus epidermidis*.
- These organisms are common **skin commensals** and typically cause infections related to **indwelling medical devices** or **bacteremia** in immunocompromised patients, not community-acquired pneumonia.
Sporothrix schenckii complex US Medical PG Question 2: A 34-year-old woman presents with multiple round, scaly patches on her chest and back. The lesions are hypopigmented and slightly pruritic. KOH preparation of skin scrapings shows short, angular hyphae. Which of the following best describes the causative organism's morphology in culture?
- A. Branching, septate hyphae with characteristic 'spaghetti and meatballs' appearance (Correct Answer)
- B. Non-septate hyphae with sporangiospores
- C. Branching, septate hyphae with tear-drop microconidia
- D. Pseudohyphae with blastoconidia
Sporothrix schenckii complex Explanation: ***Branching, septate hyphae with characteristic 'spaghetti and meatballs' appearance***
- The clinical presentation of **hypopigmented, scaly patches** on the trunk, especially with mild pruritus, is highly suggestive of **tinea versicolor**.
- A **KOH preparation** showing **short, angular hyphae** is characteristic of *Malassezia furfur*, which when cultured, displays both **mycelial elements (spaghetti)** and **yeast forms (meatballs)**.
*Non-septate hyphae with sporangiospores*
- This morphology is characteristic of **zygomycetes** (e.g., *Rhizopus*, *Mucor*), which cause diseases like mucormycosis, a much more severe and rapidly progressive infection, not tinea versicolor.
- **Zygomycetes** are typically associated with invasive infections in immunocompromised individuals.
*Branching, septate hyphae with tear-drop microconidia*
- This describes the typical dermatophyte, *Trichophyton rubrum*, which causes conditions like tinea pedis, tinea cruris, and tinea corporis, usually presenting with **erythematous, annular lesions** with active borders, different from tinea versicolor.
- While it also has septate hyphae, the distinct microconidia morphology differentiates it from *Malassezia*.
*Pseudohyphae with blastoconidia*
- This morphology is typical of **Candida species**, which cause conditions like candidiasis (e.g., thrush, diaper rash, vulvovaginitis).
- Though *Candida* can cause skin infections, the hypopigmentation and characteristic KOH findings of short, angular hyphae are inconsistent with *Malassezia*.
Sporothrix schenckii complex US Medical PG Question 3: A previously healthy 5-year-old boy is brought to the physician because of a 2-day history of itchy rash and swelling on his left lower leg. His mother says the boy complained of an insect bite while playing outdoors 3 days before the onset of the lesion. His immunizations are up-to-date. He is at the 50th percentile for height and the 85th percentile for weight. He has no known allergies. His temperature is 38.5°C (101.3°F), pulse is 120/min, and blood pressure is 95/60 mm Hg. The lower left leg is swollen and tender with erythema that has sharply defined borders. There is also a narrow red line with a raised border that extends from the lower leg to the groin. The remainder of the examination shows no abnormalities. Which of the following is the most likely cause of these findings?
- A. Streptococcus pyogenes infection (Correct Answer)
- B. Sporothrix schenckii infection
- C. Contact dermatitis
- D. Staphylococcus aureus infection
- E. Vasculitis
Sporothrix schenckii complex Explanation: ***Streptococcus pyogenes infection***
- The presentation of a rapidly spreading **erythema with sharply defined borders** and a **red streak (lymphangitis)** extending to the groin is characteristic of **cellulitis or erysipelas**, commonly caused by *Streptococcus pyogenes*.
- A **recent insect bite** or minor trauma provides a portal of entry for this bacterial infection, especially in active children.
*Sporothrix schenckii infection*
- This typically causes **sporotrichosis**, characterized by a **papule or nodule at the site of inoculation** (e.g., from thorns or sphagnum moss) that slowly ulcerates and can spread along lymphatic channels, forming secondary nodules.
- While it can cause lymphatic spread, the rapid onset, fever, and classic erysipelas-like appearance are less typical for *Sporothrix schenckii*.
*Contact dermatitis*
- This is an **inflammatory skin reaction** to an allergen or irritant, presenting with a pruritic rash, erythema, and sometimes vesicles or blisters, but it usually **lacks systemic symptoms** like fever and rarely presents with distinct **lymphangitic streaking**.
- The sharply defined, rapidly spreading erythema more strongly suggests an infectious process than an allergic reaction.
*Staphylococcus aureus infection*
- While *Staphylococcus aureus* is a common cause of skin infections, it typically presents as **folliculitis, furuncles, carbuncles, or abscesses**, often with **purulent drainage** and less commonly with the rapidly spreading, well-demarcated erythema characteristic of erysipelas caused by *Streptococcus pyogenes*.
- Although it can cause cellulitis, the strong lymphatic streaking and erysipelas-like appearance point more towards streptococcal involvement.
*Vasculitis*
- Vasculitis involves **inflammation of blood vessels** and can manifest with a variety of skin lesions, such as **purpura, livedo reticularis, or nodules**, but it **does not typically present with a red streaking pattern of lymphangitis** or the rapidly progressive, sharply bordered erythema seen in this case.
- Systemic vasculitis would also likely involve other organ systems.
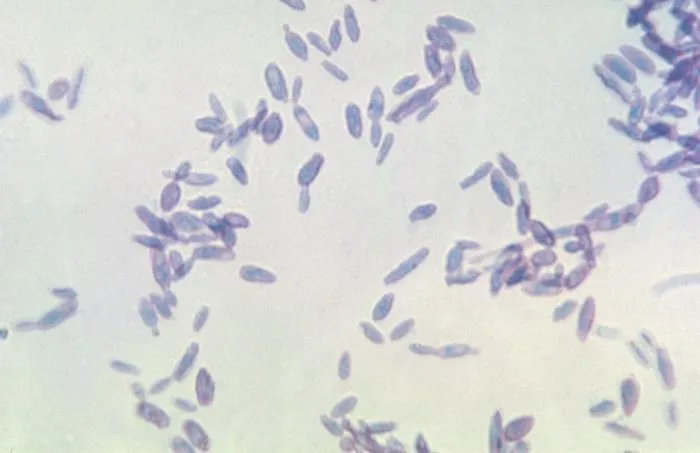
Sporothrix schenckii complex US Medical PG Question 4: An investigator is studying growth patterns of various fungal pathogens. Incubation of an isolated fungus at 25°C shows branching hyphae with rosettes of conidia under light microscopy. After incubation at 37°C, microscopic examination of the same organism instead shows smooth, white colonies with rounded, elongated cells. Infection with the investigated pathogen is most likely to cause which of the following conditions?
- A. Pityriasis versicolor
- B. Candidiasis
- C. Cryptococcosis
- D. Sporotrichosis (Correct Answer)
- E. Coccidioidomycosis
Sporothrix schenckii complex Explanation: ***Sporotrichosis***
- The description of a fungal pathogen exhibiting **thermal dimorphism** (different forms at 25°C and 37°C) is characteristic of **Sporothrix schenckii**.
- At 25°C, it typically grows as **mold with branching hyphae and conidia in rosettes**, and at 37°C, it grows as **yeast-like cells (cigar-shaped bodies in tissue)**, which can appear rounded and elongated.
*Pityriasis versicolor*
- Caused by **Malassezia globosa**, which is a **lipophilic yeast** and does not exhibit thermal dimorphism described here.
- Characterized by **hypo- or hyperpigmented skin patches**, not deep tissue infection with dimorphic growth.
*Candidiasis*
- Caused by **Candida species**, which are **opportunistic yeasts** that can form pseudohyphae and true hyphae but do not display the specific dimorphism with rosettes of conidia at 25°C.
- Infections range from superficial mucocutaneous to systemic, but the fungal morphology described does not fit.
*Cryptococcosis*
- Caused by **Cryptococcus neoformans** or **Cryptococcus gattii**, which are **encapsulated yeasts** and do not exhibit dimorphism (mold at 25°C, yeast at 37°C).
- Primarily causes **meningoencephalitis** or pulmonary disease, and is identified by its capsule and yeast form.
*Coccidioidomycosis*
- Caused by **Coccidioides immitis** or **Coccidioides posadasii**, which are **thermally dimorphic fungi**, but their morphology differs from the description.
- At 25°C, they grow as molds with **arthroconidia**, and at 37°C, they form **spherules containing endospores** in tissue, not smooth, white colonies with rounded, elongated cells.
Sporothrix schenckii complex US Medical PG Question 5: A 37-year-old woman with a history of systemic lupus erythematosus, on prednisone and methotrexate, presents to the dermatology clinic with three weeks of a diffuse, itchy rash. Physical exam is remarkable for small red papules in her bilateral axillae and groin and thin reddish-brown lines in her interdigital spaces. The following skin biopsy is obtained. Which of the following is the most appropriate treatment?
- A. Capsaicin cream
- B. Ketoconazole cream
- C. Permethrin cream (Correct Answer)
- D. Hydrocortisone cream
- E. Nystatin cream
Sporothrix schenckii complex Explanation: ***Permethrin cream***
- The patient's presentation with **diffuse itchy rash**, small red papules in the axillae and groin, and **reddish-brown lines in interdigital spaces (burrows)** is classic for **scabies**.
- **Permethrin 5% cream** is the **first-line treatment** for scabies due to its efficacy as a **scabicidal agent** by disrupting the parasite's nervous system.
- The patient's **immunocompromised status** (on prednisone and methotrexate) increases risk for **crusted (Norwegian) scabies**, but permethrin remains the primary topical treatment; severe cases may require addition of oral ivermectin.
*Capsaicin cream*
- Capsaicin cream is used for **neuropathic pain** and often causes a burning sensation, making it unsuitable for a pruritic rash caused by mites.
- It does not have any **antiparasitic properties** and would not treat the underlying cause of scabies.
*Ketoconazole cream*
- Ketoconazole is an **antifungal agent** used to treat conditions like candidiasis or tinea infections.
- The clinical presentation is not suggestive of a fungal infection, and ketoconazole would be ineffective against scabies mites.
*Hydrocortisone cream*
- Hydrocortisone is a **topical corticosteroid** used to reduce inflammation and itching associated with various dermatoses.
- While it may temporarily relieve itching, it would not eradicate the **scabies mites** and their eggs, leading to recurrence.
- Using corticosteroids alone in an **already immunocompromised patient** could worsen the infestation.
*Nystatin cream*
- Nystatin is another **antifungal medication** primarily used for cutaneous candidiasis.
- It has no activity against parasitic infestations such as scabies and would therefore be an inappropriate treatment.
Sporothrix schenckii complex US Medical PG Question 6: A 40-year-old farmer from Ohio seeks evaluation at a clinic with complaints of a chronic cough, fevers, and anorexia of several months duration. On examination, he has generalized lymphadenopathy with hepatosplenomegaly. A chest radiograph reveals local infiltrates and patchy opacities involving all lung fields. Fine needle aspiration of an enlarged lymph node shows the presence of intracellular yeast. A fungal culture shows the presence of smooth, thin-walled microconidia and tuberculate macroconidia. Which of the following is the most likely diagnosis?
- A. Coccidioidomycosis
- B. Blastomycosis
- C. Cryptococcosis
- D. Histoplasmosis (Correct Answer)
- E. Sporotrichosis
Sporothrix schenckii complex Explanation: ***Histoplasmosis***
- **Histoplasmosis** is characterized by the presence of **intracellular yeast** in tissue samples and **tuberculate macroconidia** in fungal cultures, which are key diagnostic findings in this case.
- The patient's presentation with chronic cough, fevers, anorexia, generalized lymphadenopathy, hepatosplenomegaly, and lung infiltrates, along with geographic exposure in **Ohio** (part of the Ohio River Valley endemic area), is highly consistent with disseminated histoplasmosis.
*Coccidioidomycosis*
- While coccidioidomycosis can cause lung infiltrates, it is typically endemic to the **southwestern United States** and Mexico, not Ohio.
- Microscopic examination would reveal **spherules** containing endospores, not intracellular yeast with tuberculate macroconidia.
*Blastomycosis*
- Blastomycosis is also endemic to the Ohio River Valley, but it is characterized by **broad-based budding yeast** in tissue, and its cultures typically do not show tuberculate macroconidia.
- While it causes pulmonary and disseminated disease, the specific microscopic and culture findings differentiate it from histoplasmosis.
*Cryptococcosis*
- Cryptococcosis primarily affects immunocompromised individuals and is characterized by encapsulated yeast, which would be visible with India ink stain.
- It typically presents as **meningitis** or pneumonia, and its culture morphology does not include tuberculate macroconidia.
*Sporotrichosis*
- Sporotrichosis is commonly associated with **cutaneous lesions** following traumatic inoculation of spores from soil or vegetation, and it rarely causes disseminated disease with extensive systemic symptoms like those described.
- The yeast forms in tissue are typically smaller and cigar-shaped, and the culture morphology differs significantly from what is described.
Sporothrix schenckii complex US Medical PG Question 7: A 31-year-old female undergoing treatment for leukemia is found to have a frontal lobe abscess accompanied by paranasal swelling. She additionally complains of headache, facial pain, and nasal discharge. Biopsy of the infected tissue would most likely reveal which of the following?
- A. Yeast with pseudohyphae
- B. Septate hyphae
- C. Irregular non-septate hyphae (Correct Answer)
- D. Spherules containing endospores
- E. Budding yeast with a narrow base
Sporothrix schenckii complex Explanation: ***Irregular non-septate hyphae***
- The clinical presentation of a **leukemic patient** with a **frontal lobe abscess** and **paranasal swelling**, along with headache, facial pain, and nasal discharge, strongly suggests **mucormycosis**.
- Mucormycosis is characterized by **broad, ribbon-like, irregular non-septate hyphae** with **right-angle branching** on tissue biopsy, making this the most likely finding.
*Yeast with pseudohyphae*
- This morphology is characteristic of **Candida species**, which can cause opportunistic infections but typically manifest as candidemia, esophagitis, or vulvovaginitis in immunocompromised patients, not usually a frontal lobe abscess with paranasal involvement.
- While Candida can cause severe systemic infections, the specific combination of a frontal lobe abscess and paranasal swelling points away from Candida as the primary cause in this context.
*Septate hyphae*
- **Septate hyphae** are typical of **Aspergillus species**, which can cause invasive aspergillosis, including sinopulmonary infections and CNS involvement in immunocompromised hosts.
- However, Aspergillus hyphae are typically **narrow (3-6 µm)** with **acute-angle (45-degree) branching**, differentiating them from the broad, irregular hyphae seen in mucormycosis.
*Spherules containing endospores*
- This morphology is characteristic of **Coccidioides immitis**, the causative agent of coccidioidomycosis.
- Coccidioidomycosis is geographically restricted to endemic areas (e.g., southwestern US) and typically presents with pulmonary symptoms, disseminated disease, or meningitis, which does not fit the described paranasal and frontal lobe presentation.
*Budding yeast with a narrow base*
- This morphology is characteristic of **Cryptococcus neoformans**, an encapsulated yeast that commonly causes **meningitis** and **pneumonia** in immunocompromised individuals.
- While Cryptococcus can cause CNS infections, the presence of paranasal swelling and the specific description of a frontal lobe abscess make mucormycosis a more fitting diagnosis.
Sporothrix schenckii complex US Medical PG Question 8: A previously healthy 48-year-old man comes to the physician because of a 2-week history of a nonpruritic rash on his right forearm. The rash began as pustules and progressed to form nodules and ulcers. He works as a gardener. Physical examination shows right axillary lymphadenopathy and the findings in the photograph. Which of the following is the most likely causal organism?
- A. Bartonella henselae
- B. Sporothrix schenckii (Correct Answer)
- C. Pasteurella multocida
- D. Blastomyces dermatitidis
- E. Pseudomonas aeruginosa
Sporothrix schenckii complex Explanation: ***Sporothrix schenckii***
- The patient's occupation as a **gardener** and the description of a rash progressing from **pustules to nodules and ulcers**, associated with **axillary lymphadenopathy** along a lymphatic chain, are classic findings of **sporotrichosis** (rose gardener's disease), caused by *Sporothrix schenckii*.
- This fungus is found in soil and on plants, and infection typically occurs via **traumatic inoculation** (e.g., thorn prick).
*Bartonella henselae*
- This bacterium causes **cat-scratch disease**, characterized by a papule or pustule at the inoculation site and regional lymphadenopathy.
- While it causes lymphadenopathy, the skin lesions typically do not progress to the chronic **ulcerative and nodular pattern along lymphatic drainage** seen here, and there's no history of cat exposure.
*Pasteurella multocida*
- *Pasteurella multocida* is a common cause of **wound infections after animal bites or scratches**, particularly from cats and dogs.
- Infections typically manifest as rapid onset of **erythema, swelling, and pain** at the bite site, often with cellulitis, rather than the described pustular-to-nodular-to-ulcerative progression along lymphatic channels.
*Blastomyces dermatitidis*
- *Blastomyces dermatitidis* causes **blastomycosis**, a systemic fungal infection that can present with cutaneous lesions, often **papules, pustules, or ulcers**, but these are typically associated with **pulmonary involvement** and occur after inhalation of spores, not directly from skin inoculation with lymphatic spread in a gardener.
- The skin lesions of blastomycosis are often described as **verrucous** with sharply demarcated borders.
*Pseudomonas aeruginosa*
- *Pseudomonas aeruginosa* can cause various skin infections, especially in immunocompromised individuals, those with burns, or associated with water exposure (e.g., **"hot tub folliculitis"**).
- While it can cause pustules, it does not typically produce the **lymphocutaneous spread** of nodules and ulcers observed in this patient's presentation.
Sporothrix schenckii complex US Medical PG Question 9: A 16-year-old boy is brought to the physician by his host parents for evaluation of a progressively pruritic rash over his shoulders and buttocks for the past 6 months. He recently came to the United States from Nigeria to attend a year of high school. He reports that it has been increasingly difficult for him to read the whiteboard during classes. Physical examination shows symmetrically distributed papules 4–8 mm in diameter, excoriation marks, and patchy hyperpigmentation over his shoulders, waist, and buttocks. There is nontender inguinal lymphadenopathy and several firm, nontender subcutaneous nodules along the right iliac crest. Six skin snip biopsies are taken from the pelvic girdle, buttocks, and thigh, and are then incubated in saline. After 24 hours, microscopic examination shows motile microfilariae. Which of the following is the most likely diagnosis?
- A. Cysticercosis
- B. Onchocerciasis (Correct Answer)
- C. Lymphatic filariasis
- D. Cutaneous larva migrans
- E. Trichuriasis
Sporothrix schenckii complex Explanation: ***Onchocerciasis***
- The presentation of **pruritic rash with papules**, **subcutaneous nodules** (onchocercomas), and **visual difficulties** (river blindness) in an individual from an endemic area (Nigeria) is classic for **onchocerciasis**.
- The presence of **motile microfilariae in skin snips** after saline incubation is a diagnostic hallmark of this condition, caused by *Onchocerca volvulus*.
*Cysticercosis*
- This condition is caused by the larval stage of *Taenia solium* and typically presents with **calcified lesions** in the muscle and brain (neurocysticercosis), which can lead to seizures.
- It does not typically cause the generalized pruritic rash, subcutaneous nodules, or ocular symptoms described, nor would **motile microfilariae** be found in skin snips.
*Lymphatic filariasis*
- Caused by *Wuchereria bancrofti* or *Brugia malayi*, this disease is characterized by **lymphedema** and **hydrocele**, eventually leading to **elephantiasis**.
- While it involves filarial worms and can cause lymphadenopathy, it does not typically manifest with the described rash, vision problems, or **subcutaneous nodules** (onchocercomas).
*Cutaneous larva migrans*
- This condition, caused by hookworm larvae (e.g., *Ancylostoma braziliense*), presents as a **serpiginous, intensely pruritic eruption** where the larvae migrate under the skin.
- It does not cause subcutaneous nodules, generalized papular rash, or ocular involvement, and skin snips would not show **microfilariae**.
*Trichuriasis*
- Caused by the **whipworm** (*Trichuris trichiura*), this is an intestinal nematode infection that can lead to **abdominal pain**, **diarrhea**, **rectal prolapse**, and **anemia**.
- It does not present with skin lesions, subcutaneous nodules, or visual impairment, and diagnosis is typically made by finding **ova in stool samples**, not microfilariae in skin snips.
Sporothrix schenckii complex US Medical PG Question 10: A previously healthy 24-year-old woman comes to the physician because of a 1-day history of nausea and weakness. She is sexually active with 2 male partners and uses an oral contraceptive; she uses condoms inconsistently. Her last menstrual period was 4 days ago. Her temperature is 38.4°C (101°F). Physical examination shows right costovertebral angle tenderness. Pelvic examination is normal. Which of the following is the most likely cause of this patient's condition?
- A. Noninfectious inflammation of the bladder
- B. Ascending bacteria from the endocervix
- C. Decreased renal calcium reabsorption
- D. Decreased urinary pH
- E. Ascending bacteria from the bladder (Correct Answer)
Sporothrix schenckii complex Explanation: ***Ascending bacteria from the bladder***
- The patient presents with **fever**, **nausea**, **weakness**, and **right costovertebral angle (CVA) tenderness**, which are classic symptoms of **acute pyelonephritis**.
- **Pyelonephritis** most commonly results from an **ascending urinary tract infection**, where bacteria (typically *E. coli*) from the bladder travel up the ureters to infect the kidneys.
- This accounts for approximately **95% of pyelonephritis cases** in young women.
*Noninfectious inflammation of the bladder*
- **Noninfectious cystitis** (interstitial cystitis) would not typically present with systemic symptoms like **fever** and **nausea**, or with **CVA tenderness**, which indicates kidney involvement.
- Bladder inflammation typically causes dysuria and frequency without systemic signs of infection.
*Ascending bacteria from the endocervix*
- **Ascending bacteria from the endocervix** can cause **pelvic inflammatory disease (PID)**, which presents with lower abdominal pain, cervical motion tenderness, and vaginal discharge.
- While PID can cause fever, the **normal pelvic examination** in this patient rules out this diagnosis, and PID **does not typically cause CVA tenderness**.
*Decreased renal calcium reabsorption*
- **Decreased renal calcium reabsorption** is associated with **hypercalciuria** and **nephrolithiasis** (kidney stones), which can present with acute flank pain if obstruction occurs.
- However, this condition does not explain the **fever** and systemic symptoms characteristic of an acute infectious process.
*Decreased urinary pH*
- **Decreased urinary pH** (acidic urine) can predispose to certain types of kidney stone formation but is not a direct cause of **pyelonephritis**.
- It does not explain the presence of **fever**, **CVA tenderness**, and systemic symptoms indicative of a bacterial kidney infection.
More Sporothrix schenckii complex US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.