Host factors in dimorphic fungal infections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Host factors in dimorphic fungal infections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Host factors in dimorphic fungal infections US Medical PG Question 1: A 26-year-old man comes to the physician for a follow-up examination. He was diagnosed with HIV infection 2 weeks ago. His CD4+ T-lymphocyte count is 162/mm3 (N ≥ 500). An interferon-gamma release assay is negative. Prophylactic treatment against which of the following pathogens is most appropriate at this time?
- A. Cytomegalovirus
- B. Toxoplasma gondii
- C. Mycobacterium tuberculosis
- D. Aspergillus fumigatus
- E. Pneumocystis jirovecii (Correct Answer)
Host factors in dimorphic fungal infections Explanation: ***Pneumocystis jirovecii***
- This patient's **CD4+ T-lymphocyte count of 162/mm3** is below the threshold of 200/mm3, indicating a significant risk for **Pneumocystis pneumonia (PCP)**, an opportunistic infection in HIV.
- Prophylaxis with **trimethoprim-sulfamethoxazole (TMP-SMX)** is highly effective and recommended for HIV patients with CD4 counts less than 200/mm3.
*Cytomegalovirus*
- **CMV prophylaxis** is generally not recommended for all HIV patients, even with low CD4 counts, unless there is evidence of active disease or extremely low CD4 counts (e.g., <50/mm3) with high viral loads.
- While CMV can cause end-organ disease in advanced HIV, routine primary prophylaxis is not standard for this CD4 level.
*Toxoplasma gondii*
- **Toxoplasma prophylaxis** is indicated for HIV patients with **CD4 counts less than 100/mm3** who are also seropositive for *Toxoplasma gondii*.
- The patient's CD4 count is 162/mm3, and there's no mention of *Toxoplasma* serostatus, making it less appropriate than PCP prophylaxis.
*Mycobacterium tuberculosis*
- The patient's **interferon-gamma release assay (IGRA) is negative**, which suggests no **latent tuberculosis infection (LTBI)**, thus making primary prophylaxis unnecessary at this time.
- While HIV patients are at high risk for TB, prophylaxis is typically given for LTBI or as secondary prophylaxis for those who have completed treatment for active TB.
*Aspergillus fumigatus*
- **Aspergillus infections** are typically seen in patients with severe **neutropenia** or those receiving high-dose corticosteroids, not primarily in HIV patients based solely on CD4 count.
- Routine prophylaxis for Aspergillus is not recommended for HIV patients, even with low CD4 counts, unless there is a specific risk factor.
Host factors in dimorphic fungal infections US Medical PG Question 2: A 3-year-old recent immigrant is diagnosed with primary tuberculosis. Her body produces T cells that do not have IL-12 receptors on their surface, and she is noted to have impaired development of Th1 T-helper cells. Which of the following cytokines would benefit this patient?
- A. IL-4
- B. IL-22
- C. TGF-beta
- D. IL-17
- E. Interferon-gamma (Correct Answer)
Host factors in dimorphic fungal infections Explanation: ***Interferon-gamma***
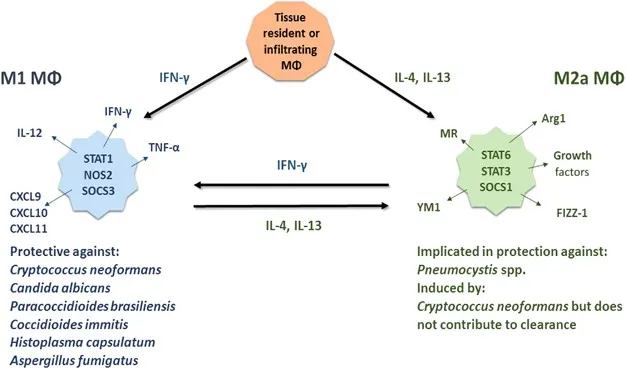
- This patient has an impaired **Th1 response**, which is crucial for controlling intracellular infections like **tuberculosis** by activating macrophages.
- **Interferon-gamma** is the primary cytokine produced by **Th1 cells** that activates macrophages, leading to enhanced phagocytosis and killing of intracellular pathogens.
*IL-4*
- **IL-4** is a key cytokine produced by **Th2 cells**, which primarily drive **humoral immunity** and allergic responses, not cellular immunity against intracellular bacteria.
- Its administration would promote a **Th2 response**, which is not beneficial for combating **tuberculosis** and might even suppress the desirable Th1 response.
*IL-22*
- **IL-22** is mainly involved in **epithelial cell proliferation**, host defense at mucosal surfaces, and tissue repair.
- While it has a role in host defense against certain pathogens, it is not the primary cytokine required to compensate for a deficient **Th1 response** in **tuberculosis**.
*TGF-beta*
- **TGF-beta** is a pleiotropic cytokine with roles in cell growth, differentiation, and immune regulation, often acting as an **immunosuppressant** or driving **Treg differentiation**.
- It would not directly compensate for a lack of **Th1 cell function** needed to activate macrophages against **tuberculosis**.
*IL-17*
- **IL-17** is the signature cytokine of **Th17 cells**, which are important for host defense against **extracellular bacteria** and fungi, primarily by recruiting neutrophils.
- While it plays a role in some immune responses, it is not the crucial cytokine to boost in a patient with impaired **Th1 development** against **intracellular M. tuberculosis**.
Host factors in dimorphic fungal infections US Medical PG Question 3: A 21-year-old woman comes to the physician because of a 1-week history of white discoloration of the tongue. She has had similar, recurrent episodes over the past 5 years. Examination shows white plaques on the tongue that easily scrape off and thick, cracked fingernails with white discoloration. KOH preparation of a tongue scraping shows budding yeasts with pseudohyphae. This patient's condition is most likely caused by decreased activity of which of the following?
- A. Neutrophils
- B. Complement C1–4
- C. B cells
- D. T cells (Correct Answer)
- E. Complement C5–9
Host factors in dimorphic fungal infections Explanation: ***T cells***
- The recurrent oral **candidiasis** with **pseudohyphae** (thrush) and **onychomycosis** (thick, cracked fingernails) suggests a defect in **cell-mediated immunity**, which is primarily mediated by **T cells**.
- **T cells** are crucial for controlling fungal infections, particularly *Candida* species, and their decreased activity makes individuals susceptible to **recurrent mucocutaneous candidiasis** (affecting skin, nails, and mucous membranes).
*Neutrophils*
- Defective **neutrophil** function would lead to **invasive or disseminated candidiasis** (bloodstream, deep tissues) rather than the chronic mucocutaneous pattern seen here.
- Neutrophil defects also cause recurrent **bacterial infections**, especially from *Staphylococcus* and *Pseudomonas* species.
*Complement C1–4*
- Deficiencies in early **complement components** (C1-C4) are associated with an increased risk of encapsulated **bacterial infections** and **immune complex disorders** like lupus.
- These deficiencies are not typically linked to recurrent fungal infections such as candidiasis.
*B cells*
- **B cells** are responsible for **humoral immunity** (antibody production), and their deficiency would lead to recurrent **bacterial and viral infections**, particularly those affecting the respiratory tract.
- While antibodies can play a supportive role, they are not the primary defense against localized candidal infections.
*Complement C5–9*
- Deficiencies in late **complement components** (C5-C9), part of the **membrane attack complex (MAC)**, primarily increase susceptibility to recurrent **Neisseria** infections (*N. meningitidis* and *N. gonorrhoeae*).
- These components are not directly involved in immunity against *Candida* infections.
Host factors in dimorphic fungal infections US Medical PG Question 4: A 43-year-old HIV positive male presents with signs and symptoms concerning for a fungal infection. He is currently not on antiretrovirals and his CD4 count is 98. Which of the following candidal infections could be seen in this patient but would be very rare in an immunocompetent host?
- A. Endocarditis
- B. Intertrigo
- C. Oral thrush
- D. Esophagitis (Correct Answer)
- E. Vaginitis
Host factors in dimorphic fungal infections Explanation: ***Esophagitis***
- **Candidal esophagitis** is an **AIDS-defining illness** and is highly suggestive of severe immunosuppression, making it rare in immunocompetent individuals.
- The patient's **CD4 count of 98** indicates advanced HIV disease, placing him at high risk for opportunistic infections like candidal esophagitis.
*Endocarditis*
- While fungal endocarditis can occur in immunocompromised patients, it is more commonly associated with intravenous drug use, prosthetic valves, or central venous catheters, rather than solely with a low CD4 count.
- It is not considered an AIDS-defining illness in the same way as candidal esophagitis.
*Intertrigo*
- **Candidal intertrigo** is a common skin infection that can occur in both immunocompetent and immunocompromised individuals, usually in skin folds where moisture accumulates.
- Its presence does not strongly suggest severe immunosuppression, although it may be more persistent or widespread in HIV patients.
*Oral thrush*
- **Oral candidiasis** is common in HIV-positive patients, especially with lower CD4 counts, but it can also occur in immunocompetent individuals (e.g., due to antibiotic use, steroid inhalers, or diabetes).
- While indicative of some degree of immunosuppression in an HIV patient, it is not as specific for severe immunosuppression as candidal esophagitis.
*Vaginitis*
- **Candidal vaginitis** is a very common infection in women, regardless of immune status, and is not a strong indicator of severe immunosuppression or an AIDS-defining illness.
- Although it can be more frequent or resistant to treatment in HIV-positive women, its mere presence does not signify a condition rare in immunocompetent hosts.
Host factors in dimorphic fungal infections US Medical PG Question 5: A 30-year-old man is admitted to the hospital with a presumed pneumonia and started on antibiotics. Two days later, the patient shows no improvement. Blood cultures reveal yeast with pseudophyphae. Which of the following cell types is most likely deficient or dysfunctional in this patient?
- A. Eosinophils
- B. Macrophages
- C. Neutrophils (Correct Answer)
- D. T-cells
- E. B-cells
Host factors in dimorphic fungal infections Explanation: ***Neutrophils***
- The presence of **yeast with pseudohyphae** in blood cultures, particularly *Candida*, indicates a fungal infection.
- **Neutrophils** are crucial for the host defense against *Candida* and other fungal pathogens, so their deficiency or dysfunction would predispose to candidemia.
- Neutropenia or neutrophil dysfunction (e.g., chronic granulomatous disease) significantly increases risk of invasive candidiasis.
*Eosinophils*
- **Eosinophils** are primarily involved in defense against **parasitic infections** and in allergic reactions.
- They play a minimal role in the immune response to systemic fungal infections like candidemia.
*Macrophages*
- **Macrophages** are phagocytic cells that contribute to antifungal immunity, particularly in tissue surveillance and chronic infection control.
- However, **neutrophils** are the primary and most critical defense against acute *Candida* bloodstream infections.
- Macrophage deficiency alone does not typically predispose to candidemia as severely as neutrophil deficiency.
*T-cells*
- **T-cells** are important for cell-mediated immunity, particularly against **intracellular pathogens** and viral infections.
- While they play a role in modulating antifungal responses, their deficiency typically leads to infections with *Pneumocystis jirovecii* or severe mucocutaneous candidiasis, rather than disseminated candidemia.
*B-cells*
- **B-cells** are responsible for **humoral immunity** through antibody production, which is primarily effective against extracellular bacteria and toxins.
- They are not the primary line of defense against fungal infections such as candidemia.
Host factors in dimorphic fungal infections US Medical PG Question 6: A 40-year-old farmer from Ohio seeks evaluation at a clinic with complaints of a chronic cough, fevers, and anorexia of several months duration. On examination, he has generalized lymphadenopathy with hepatosplenomegaly. A chest radiograph reveals local infiltrates and patchy opacities involving all lung fields. Fine needle aspiration of an enlarged lymph node shows the presence of intracellular yeast. A fungal culture shows the presence of smooth, thin-walled microconidia and tuberculate macroconidia. Which of the following is the most likely diagnosis?
- A. Coccidioidomycosis
- B. Blastomycosis
- C. Cryptococcosis
- D. Histoplasmosis (Correct Answer)
- E. Sporotrichosis
Host factors in dimorphic fungal infections Explanation: ***Histoplasmosis***
- **Histoplasmosis** is characterized by the presence of **intracellular yeast** in tissue samples and **tuberculate macroconidia** in fungal cultures, which are key diagnostic findings in this case.
- The patient's presentation with chronic cough, fevers, anorexia, generalized lymphadenopathy, hepatosplenomegaly, and lung infiltrates, along with geographic exposure in **Ohio** (part of the Ohio River Valley endemic area), is highly consistent with disseminated histoplasmosis.
*Coccidioidomycosis*
- While coccidioidomycosis can cause lung infiltrates, it is typically endemic to the **southwestern United States** and Mexico, not Ohio.
- Microscopic examination would reveal **spherules** containing endospores, not intracellular yeast with tuberculate macroconidia.
*Blastomycosis*
- Blastomycosis is also endemic to the Ohio River Valley, but it is characterized by **broad-based budding yeast** in tissue, and its cultures typically do not show tuberculate macroconidia.
- While it causes pulmonary and disseminated disease, the specific microscopic and culture findings differentiate it from histoplasmosis.
*Cryptococcosis*
- Cryptococcosis primarily affects immunocompromised individuals and is characterized by encapsulated yeast, which would be visible with India ink stain.
- It typically presents as **meningitis** or pneumonia, and its culture morphology does not include tuberculate macroconidia.
*Sporotrichosis*
- Sporotrichosis is commonly associated with **cutaneous lesions** following traumatic inoculation of spores from soil or vegetation, and it rarely causes disseminated disease with extensive systemic symptoms like those described.
- The yeast forms in tissue are typically smaller and cigar-shaped, and the culture morphology differs significantly from what is described.
Host factors in dimorphic fungal infections US Medical PG Question 7: A 58-year-old man presents with a high-grade fever, throbbing left-sided headache, vision loss, and left orbital pain. He says that his symptoms started acutely 2 days ago with painful left-sided mid-facial swelling and a rash, which progressively worsened. Today, he woke up with complete vision loss in his left eye. His past medical history is significant for type 2 diabetes mellitus, diagnosed 5 years ago. He was started on an oral hypoglycemic agent which he discontinued after a year. His temperature is 38.9°C (102.0°F), blood pressure is 120/80 mm Hg, pulse is 120/min, and respiratory rate is 20/min. On examination, there is purulent discharge from the left eye and swelling of the left half of his face including the orbit. Oral examination reveals extensive necrosis of the palate with a black necrotic eschar and purulent discharge. Ophthalmic examination is significant for left-sided ptosis, proptosis, and an absence of the pupillary light reflex. Laboratory findings are significant for a blood glucose level of 388 mg/dL and a white blood cell count of 19,000 cells/mm³. Urinary ketone bodies are positive. Fungal elements are found on a KOH mount of the discharge. Which of the following statements best describes the organism responsible for this patient’s condition?
- A. It appears as a narrow-based budding yeast with a thick capsule
- B. Histopathological examination shows non-septate branching hyphae (Correct Answer)
- C. It produces conidiospores
- D. It has budding and filamentous forms
- E. Histopathological examination shows acute angle branching hyphae
Host factors in dimorphic fungal infections Explanation: ***Histopathological examination shows non-septate branching hyphae***
- The patient's presentation with **diabetic ketoacidosis**, orbital pain, vision loss, facial swelling, necrotic palatal eschar, and high fever strongly suggests **mucormycosis**, a severe fungal infection.
- Mucormycosis is caused by fungi belonging to **Mucorales order** (e.g., *Rhizopus*, *Mucor*, *Lichtheimia*), which are characterized by **broad, ribbon-like, non-septate hyphae with irregular, wide-angle branching**.
*It appears as a narrow-based budding yeast with a thick capsule*
- This description is characteristic of **Cryptococcus neoformans**, which causes cryptococcosis, often presenting with meningoencephalitis and lung involvement.
- The clinical picture and *KOH mount* findings in this patient are inconsistent with cryptococcosis.
*It produces conidiospores*
- **Conidiospores are asexual spores** produced by many fungi, including *Aspergillus* and *Penicillium*, but this is a general characteristic and not specific enough to definitively identify the pathogen responsible for mucormycosis.
- The *histopathological features* (non-septate hyphae) are the key identifier in mucormycosis.
*It has budding and filamentous forms*
- This description generally refers to **dimorphic fungi** (e.g., *Histoplasma*, *Blastomyces*, *Coccidioides*), which exhibit yeast forms in tissue and mold forms in culture.
- Mucorales are typically **molds** in both environments and are not considered dimorphic, nor do they commonly present with budding forms.
*Histopathological examination shows acute angle branching hyphae*
- This morphological description is characteristic of **Aspergillus species**, which cause aspergillosis, another opportunistic fungal infection.
- *Aspergillus* hyphae are typically **septate** and branch at acute angles (around 45 degrees), unlike the broad, non-septate, wide-angle branching hyphae of Mucorales.
Host factors in dimorphic fungal infections US Medical PG Question 8: A 3-month-old girl is brought to the emergency department because of a 2-day history of progressive difficulty breathing and a dry cough. Five weeks ago, she was diagnosed with diffuse hemangiomas involving the intrathoracic cavity and started treatment with prednisolone. She appears uncomfortable and in moderate respiratory distress. Her temperature is 38°C (100.4°F), pulse is 150/min, respirations are 50/min, and blood pressure is 88/50 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 87%. Oral examination shows a white plaque covering the tongue that bleeds when scraped. Chest examination shows subcostal and intercostal retractions. Scattered fine crackles and rhonchi are heard throughout both lung fields. Laboratory studies show a leukocyte count of 21,000/mm3 and an increased serum beta-D-glucan concentration. An x-ray of the chest shows symmetrical, diffuse interstitial infiltrates. Which of the following is most likely to confirm the diagnosis?
- A. Tuberculin skin test
- B. Urine antigen test
- C. CT scan of the chest
- D. Bronchoalveolar lavage (Correct Answer)
- E. DNA test for CFTR mutation
Host factors in dimorphic fungal infections Explanation: ***Bronchoalveolar lavage***
- The patient, an infant on **prednisolone** (immunosuppression) with **diffuse interstitial infiltrates**, **uncomfortable appearance**, **respiratory distress**, and **oral thrush (white plaque that bleeds when scraped)**, points to **Pneumocystis pneumonia (PCP)**.
- **Bronchoalveolar lavage (BAL)** is the gold standard for diagnosing PCP by identifying **Pneumocystis jirovecii cysts** or **trophozoites** using special stains (e.g., Giemsa, methenamine silver).
*Tuberculin skin test*
- The **tuberculin skin test** is used to diagnose **tuberculosis**, which typically presents with **granulomas** and **cavitary lesions** on chest X-ray, not diffuse interstitial infiltrates.
- While tuberculosis can cause respiratory symptoms, the presence of oral thrush and immunosuppression suggests an opportunistic fungal infection like PCP rather than TB.
*Urine antigen test*
- A **urine antigen test** is commonly used for diagnosing **Legionnaires' disease** or **pneumococcal pneumonia** in adults, and is not applicable for PCP.
- It does not detect *Pneumocystis jirovecii*, which is the suspected pathogen in this immunosuppressed infant.
*CT scan of the chest*
- A **CT scan of the chest** would show **diffuse ground-glass opacities** characteristic of PCP but is a **radiological finding**, not a definitive diagnostic test for the pathogen itself.
- While it can further characterize the pulmonary findings, it cannot identify the causative organism, which is crucial for targeted treatment.
*DNA test for CFTR mutation*
- A **DNA test for CFTR mutation** is used to diagnose **cystic fibrosis**, a genetic disorder affecting mucus production, and is not relevant in this acute presentation of respiratory distress and immunosuppression.
- Cystic fibrosis typically presents with recurrent respiratory infections, pancreatic insufficiency, and failure to thrive, not primarily with opportunistic infections like PCP.
Host factors in dimorphic fungal infections US Medical PG Question 9: A 29-year-old woman comes to the military physician because of a 2-day history of fever, joint pain, dry cough, chest pain, and a painful red rash on her lower legs. Two weeks ago, she returned from military training in Southern California. She appears ill. Her temperature is 39°C (102.1°F). Physical examination shows diffuse inspiratory crackles over all lung fields and multiple tender erythematous nodules over the anterior aspect of both legs. A biopsy specimen of this patient's lungs is most likely to show which of the following?
- A. Septate hyphae with acute-angle branching
- B. Spherules filled with endospores (Correct Answer)
- C. Broad-based budding yeast
- D. Encapsulated yeast with narrow-based budding
- E. Oval, budding yeast with pseudohyphae
Host factors in dimorphic fungal infections Explanation: **Spherules filled with endospores**
- The patient's symptoms (fever, joint pain, dry cough, chest pain, erythema nodosum on legs) combined with her travel history to **Southern California** are highly suggestive of **Coccidioidomycosis** ("Valley Fever").
- A biopsy of affected lung tissue in coccidioidomycosis typically reveals **spherules** (thick-walled structures) containing numerous **endospores**, which are characteristic of the tissue phase of *Coccidioides immitis/posadasii*.
*Septate hyphae with acute-angle branching*
- This morphology is characteristic of **Aspergillus** species, which can cause opportunistic infections, especially in immunocompromised individuals.
- While it can cause lung infections, the clinical presentation and geographic exposure do not point towards aspergillosis as the most likely diagnosis.
*Broad-based budding yeast*
- This describes the characteristic morphology of *Blastomyces dermatitidis*, the causative agent of **Blastomycosis**.
- **Blastomycosis** is typically found in the Great Lakes region, Ohio, Mississippi River valleys, and southeastern United States, not Southern California.
*Encapsulated yeast with narrow-based budding*
- This describes **Cryptococcus neoformans**, which appears as an encapsulated yeast with narrow-based budding in tissue.
- While it can cause pulmonary disease, the classic presentation (erythema nodosum, acute illness after Southern California exposure) is not consistent with **cryptococcosis**, which typically presents subacutely in immunocompromised patients.
*Oval, budding yeast with pseudohyphae*
- This morphology is characteristic of *Candida albicans*, which commonly causes mucocutaneous infections and can cause systemic candidiasis, particularly in immunocompromised patients.
- The clinical picture of a healthy young woman with exposure in Southern California does not fit with a typical **Candida** infection.
Host factors in dimorphic fungal infections US Medical PG Question 10: A 47-year-old woman comes to the physician because of a 3-day history of fever, fatigue, loss of appetite, cough, and chest pain. Physical examination shows diffuse inspiratory crackles over the left lung field. An x-ray of the chest shows hilar lymphadenopathy and well-defined nodules with central calcifications. Urine studies show the presence of a polysaccharide antigen. A biopsy specimen of the lung shows cells with basophilic, crescent-shaped nuclei and pericellular halos located within macrophages. This patient's history is most likely to show which of the following?
- A. Visit to Arizona desert
- B. Recent trip to Brazil
- C. Previous mycobacterial infection
- D. Exposure to bat droppings (Correct Answer)
- E. Treatment with inhaled glucocorticoids
Host factors in dimorphic fungal infections Explanation: ***Exposure to bat droppings***
- The clinical presentation, including fever, cough, chest pain, **hilar lymphadenopathy**, **nodules with central calcifications**, and **intracellular encapsulated yeasts** in macrophages, is classic for **histoplasmosis**.
- **Histoplasma capsulatum** is endemic to the Ohio and Mississippi River valleys and is transmitted through inhalation of spores from soil contaminated with **bat or bird droppings**.
*Visit to Arizona desert*
- Exposure in the **Arizona desert** is associated with **coccidioidomycosis** (Valley Fever), which presents with similar pulmonary symptoms but is caused by Coccidioides immitis/posadasii, characterized by **spherules** containing endospores.
- While it can cause hilar lymphadenopathy and nodules, the characteristic intracellular budding yeasts within macrophages and the polysaccharide antigen in urine point away from coccidioidomycosis.
*Recent trip to Brazil*
- A trip to **Brazil** might suggest diseases like **Paracoccidioidomycosis**, which presents with chronic mucocutaneous or disseminated lesions, or various tropical infections, but is not typically characterized by the specific pulmonary and microscopic findings described here.
- The histopathological findings of **intracellular yeasts with pericellular halos** (consistent with Histoplasma) would not be the primary finding for paracoccidioidomycosis, which generally shows characteristic **"pilot wheel"** or multiple budding yeasts.
*Previous mycobacterial infection*
- A previous **mycobacterial infection** would lead to tuberculosis, characterized by **acid-fast bacilli** and granulomas with **caseating necrosis**, which is different from the described intracellular yeasts and polysaccharide antigen.
- While tuberculosis can cause hilar lymphadenopathy and pulmonary nodules, the given microscopic description of cells with basophilic nuclei and pericellular halos within macrophages does not fit Mycobacterium tuberculosis.
*Treatment with inhaled glucocorticoids*
- Inhaled glucocorticoids are used to treat conditions like asthma or COPD and, while prolonged use can rarely predispose to **opportunistic fungal infections** (e.g., aspergillosis, candidiasis), they are not a cause of this specific clinical presentation or the microbiological findings of histoplasmosis.
- The use of inhaled steroids would not explain the geographic exposure, hilar lymphadenopathy, or the specific appearance of the fungal elements within macrophages described.
More Host factors in dimorphic fungal infections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.