Diagnostic approaches for dimorphic fungi US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diagnostic approaches for dimorphic fungi. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diagnostic approaches for dimorphic fungi US Medical PG Question 1: The surgical equipment used during a craniectomy is sterilized using pressurized steam at 121°C for 15 minutes. Reuse of these instruments can cause transmission of which of the following pathogens?
- A. Non-enveloped viruses
- B. Sporulating bacteria
- C. Prions (Correct Answer)
- D. Enveloped viruses
- E. Yeasts
Diagnostic approaches for dimorphic fungi Explanation: ***Prions***
- Prions are **abnormally folded proteins** that are highly resistant to standard sterilization methods like steam autoclaving at 121°C, making them a risk for transmission through reused surgical instruments.
- They cause transmissible spongiform encephalopathies (TSEs) like **Creutzfeldt-Jakob disease**, where even trace amounts can be highly infectious.
*Non-enveloped viruses*
- Non-enveloped viruses are generally **more resistant to heat and disinfectants** than enveloped viruses but are typically inactivated by recommended steam sterilization protocols.
- Standard autoclaving conditions are effective in destroying most non-enveloped viruses.
*Sporulating bacteria*
- **Bacterial spores**, such as those from *Clostridium* or *Bacillus*, are known for their high resistance to heat and chemicals, but are usually **inactivated by steam sterilization at 121°C** for 15 minutes.
- This method is specifically designed to kill bacterial spores effectively.
*Enveloped viruses*
- Enveloped viruses are the **least resistant to heat and chemical disinfectants** due to their lipid envelope.
- They are readily **inactivated by standard steam sterilization** at 121°C.
*Yeasts*
- **Yeasts** are eukaryotic microorganisms that are typically **susceptible to heat sterilization**.
- They are effectively killed by typical steam autoclaving conditions used for surgical instruments.
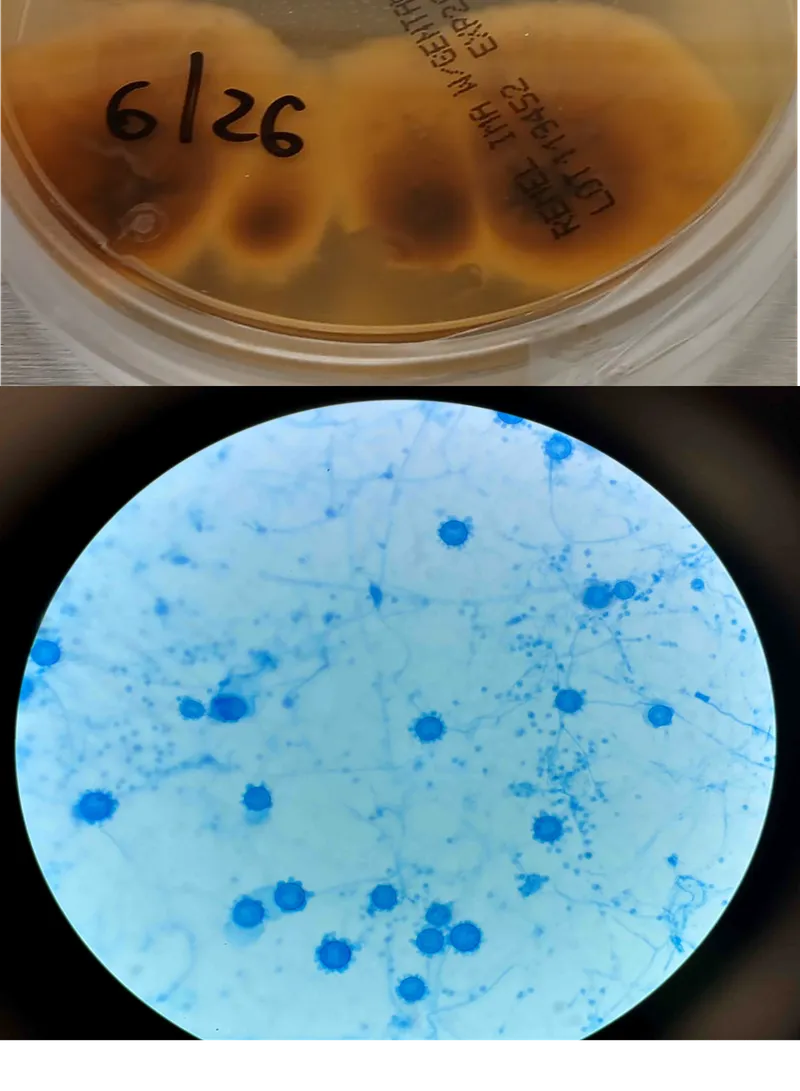
Diagnostic approaches for dimorphic fungi US Medical PG Question 2: A 44-year-old man comes to the physician because of a 3-week history of productive cough, fever, and lethargy. He also has several skin lesions over his body. His symptoms began 3 weeks after he returned from a camping trip in Kentucky. Three years ago, he underwent kidney transplantation for polycystic kidney disease. Current medications include sirolimus and prednisone. His temperature is 38°C (100.4°F). Diffuse crackles are heard over the lung fields. There are 4 white, verrucous skin patches over his chest and upper limbs. A photomicrograph of a skin biopsy specimen from one of the lesions is shown. Which of the following is the most likely diagnosis?
- A. Coccidioidomycosis
- B. Mucormycosis
- C. Blastomycosis (Correct Answer)
- D. Cryptococcosis
- E. Histoplasmosis
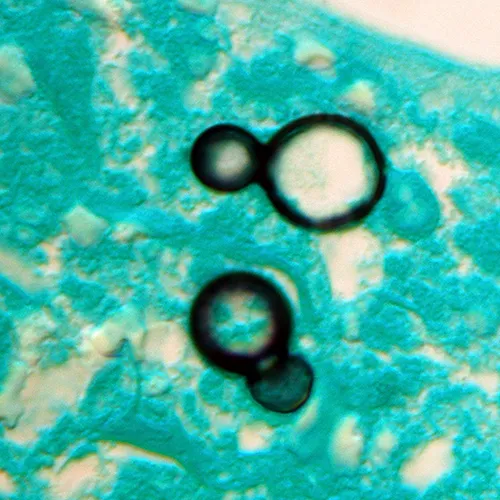
Diagnostic approaches for dimorphic fungi Explanation: ***Blastomycosis***
- The patient's history of **camping in Kentucky**, along with the presence of **pulmonary symptoms** (productive cough, fever, crackles) and **verrucous skin lesions**, are classic for blastomycosis.
- The photomicrograph showing **broad-based budding yeast** is pathognomonic for *Blastomyces dermatitidis*.
*Coccidioidomycosis*
- This is typical in the **Southwestern United States and parts of Mexico**, not Kentucky.
- Microscopic examination would reveal **spherules containing endospores**, which are not seen in the provided image.
*Mucormycosis*
- This infection is characterized by **irregular, broad, non-septate hyphae** with **wide-angle branching**, often invading blood vessels, leading to tissue necrosis.
- It primarily affects immunocompromised patients but typically presents as **rhinocerebral** or **pulmonary infection**, less commonly with verrucous skin lesions of this type.
*Cryptococcosis*
- Primarily affects the **lungs and central nervous system**, especially in immunocompromised individuals.
- Microscopy typically shows **encapsulated yeast** cells, which would be visible with India ink stain, and are not represented by the broad-based budding in the image.
*Histoplasmosis*
- Prevalent in the **Ohio and Mississippi River Valleys**, which includes Kentucky, and is often associated with **bird or bat droppings**.
- On microscopy, it presents as **small intracellular yeast** within macrophages, which is morphologically distinct from the large, broad-based budding yeast shown.
Diagnostic approaches for dimorphic fungi US Medical PG Question 3: A young woman from the Ohio River Valley in the United States currently on corticosteroid therapy for ulcerative colitis presented to a clinic complaining of fever, sweat, headache, nonproductive cough, malaise, and general weakness. A chest radiograph revealed patchy pneumonia in the lower lung fields, together with enlarged mediastinal and hilar lymph nodes. Skin changes suggestive of erythema nodosum (i.e. an acute erythematous eruption) were noted. Because the patient was from a region endemic for fungal infections associated with her symptoms and the patient was in close contact with a person presenting similar symptoms, the attending physician suspected that systemic fungal infection might be responsible for this woman’s illness. Which of the following laboratory tests can the physician use to ensure early detection of the disease, and also effectively monitor the treatment response?
- A. Skin tests
- B. Fungal staining
- C. Antigen detection (Correct Answer)
- D. Culture method
- E. Antibody testing
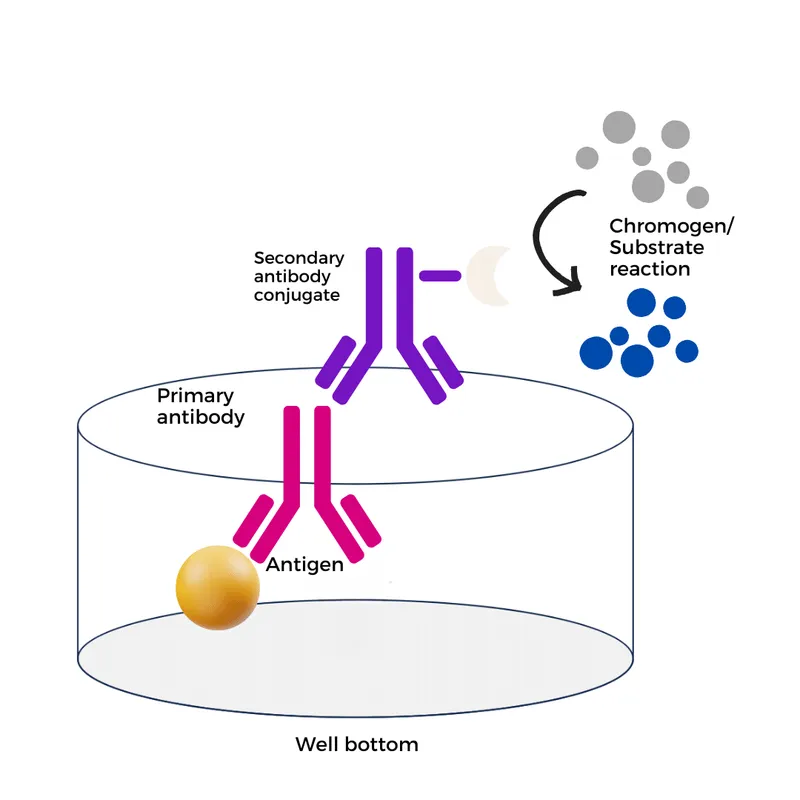
Diagnostic approaches for dimorphic fungi Explanation: ***Antigen detection***
- **Antigen detection assays** (e.g., *Histoplasma galactomannan antigen*) are highly sensitive for **disseminated histoplasmosis**, especially in immunosuppressed patients like this one on corticosteroids.
- They provide **early diagnosis** and are effective for **monitoring treatment response**, as antigen levels typically decrease with successful therapy.
*Skin tests*
- **Skin tests** (e.g., *histoplasmin skin test*) indicate **prior exposure** to the fungus and are not useful for diagnosing active, acute infection.
- A positive skin test does not differentiate between past exposure and current disease, making it unsuitable for early detection or monitoring.
*Fungal staining*
- **Fungal staining** of patient samples (e.g., sputum, biopsy) can reveal fungal elements but has **limited sensitivity** and may not identify the specific pathogen.
- It often requires **invasive procedures** to obtain suitable specimens and is not ideal for routine monitoring of treatment response due to variability.
*Culture method*
- **Fungal cultures** are a **definitive diagnostic method** but can take **several weeks** to yield results, which is too slow for early detection in an acutely ill patient.
- While useful for species identification and susceptibility testing, the **delayed turnaround time** makes it impractical for monitoring rapid treatment changes.
*Antibody testing*
- **Antibody tests** for fungal infections can be useful but may show **false negatives in immunocompromised patients** (like this patient on corticosteroids) due to a blunted immune response.
- Seroconversion or a significant rise in antibody titers can indicate infection, but antibodies may **persist long after resolution**, making them less reliable for monitoring acute treatment efficacy.
Diagnostic approaches for dimorphic fungi US Medical PG Question 4: A 29-year-old woman comes to the military physician because of a 2-day history of fever, joint pain, dry cough, chest pain, and a painful red rash on her lower legs. Two weeks ago, she returned from military training in Southern California. She appears ill. Her temperature is 39°C (102.1°F). Physical examination shows diffuse inspiratory crackles over all lung fields and multiple tender erythematous nodules over the anterior aspect of both legs. A biopsy specimen of this patient's lungs is most likely to show which of the following?
- A. Septate hyphae with acute-angle branching
- B. Spherules filled with endospores (Correct Answer)
- C. Broad-based budding yeast
- D. Encapsulated yeast with narrow-based budding
- E. Oval, budding yeast with pseudohyphae
Diagnostic approaches for dimorphic fungi Explanation: **Spherules filled with endospores**
- The patient's symptoms (fever, joint pain, dry cough, chest pain, erythema nodosum on legs) combined with her travel history to **Southern California** are highly suggestive of **Coccidioidomycosis** ("Valley Fever").
- A biopsy of affected lung tissue in coccidioidomycosis typically reveals **spherules** (thick-walled structures) containing numerous **endospores**, which are characteristic of the tissue phase of *Coccidioides immitis/posadasii*.
*Septate hyphae with acute-angle branching*
- This morphology is characteristic of **Aspergillus** species, which can cause opportunistic infections, especially in immunocompromised individuals.
- While it can cause lung infections, the clinical presentation and geographic exposure do not point towards aspergillosis as the most likely diagnosis.
*Broad-based budding yeast*
- This describes the characteristic morphology of *Blastomyces dermatitidis*, the causative agent of **Blastomycosis**.
- **Blastomycosis** is typically found in the Great Lakes region, Ohio, Mississippi River valleys, and southeastern United States, not Southern California.
*Encapsulated yeast with narrow-based budding*
- This describes **Cryptococcus neoformans**, which appears as an encapsulated yeast with narrow-based budding in tissue.
- While it can cause pulmonary disease, the classic presentation (erythema nodosum, acute illness after Southern California exposure) is not consistent with **cryptococcosis**, which typically presents subacutely in immunocompromised patients.
*Oval, budding yeast with pseudohyphae*
- This morphology is characteristic of *Candida albicans*, which commonly causes mucocutaneous infections and can cause systemic candidiasis, particularly in immunocompromised patients.
- The clinical picture of a healthy young woman with exposure in Southern California does not fit with a typical **Candida** infection.
Diagnostic approaches for dimorphic fungi US Medical PG Question 5: A 27-year-old female presents to her primary care physician because she is concerned about lighter colored patches on her skin. She recently went sunbathing and noticed that these areas also did not tan. Her doctor explains that she has a fungal infection of the skin that damages melanocytes by producing acids. She is prescribed selenium sulfide and told to follow-up in one month. Which of the following describes the appearance of the most likely infectious organism under microscopy?
- A. Broad based budding yeast
- B. "Captain's wheel" yeast
- C. Germ tube forming fungus
- D. Branching septate hyphae
- E. "Spaghetti and meatballs" fungus (Correct Answer)
Diagnostic approaches for dimorphic fungi Explanation: ***"Spaghetti and meatballs" fungus***
- The "spaghetti and meatballs" appearance on microscopy, referring to a mixture of short, septate hyphae and spherical yeast forms, is characteristic of **Malassezia globosa** or other *Malassezia* species, which cause **tinea versicolor**.
- **Tinea versicolor** presents as hypopigmented patches, especially after sun exposure, because the fungus produces **azelaic acid** that inhibits melanin synthesis.
*Broad based budding yeast*
- This description is characteristic of **Blastomyces dermatitidis**, which causes **blastomycosis**, a deep fungal infection.
- Blastomycosis typically manifests as pulmonary disease or disseminated lesions, not superficial hypopigmented skin patches.
*"Captain's wheel" yeast*
- The "captain's wheel" or multi-budding yeast appearance is characteristic of **Paracoccidioides brasiliensis**, the causative agent of **paracoccidioidomycosis**.
- This is a systemic mycosis primarily affecting the lungs and mucocutaneous areas, not a superficial skin infection like tinea versicolor.
*Germ tube forming fungus*
- The formation of **germ tubes** when incubated in serum at 37°C is a characteristic feature used to identify **Candida albicans**.
- *Candida* most commonly causes mucocutaneous candidiasis (e.g., thrush, vaginitis) or invasive infections, not hypopigmented skin patches that fail to tan.
*Branching septate hyphae*
- **Branching septate hyphae** are a general microscopic feature seen in many filamentous fungi, including dermatophytes like *Trichophyton* and *Microsporum*, which cause **tinea corporis** or **tinea pedis**.
- While dermatophytes cause skin infections, they typically result in erythematous, scaly, and often pruritic lesions and do not usually present as hypopigmented patches that fail to tan due to melanin inhibition, as seen in tinea versicolor.
Diagnostic approaches for dimorphic fungi US Medical PG Question 6: A 31-year-old female undergoing treatment for leukemia is found to have a frontal lobe abscess accompanied by paranasal swelling. She additionally complains of headache, facial pain, and nasal discharge. Biopsy of the infected tissue would most likely reveal which of the following?
- A. Yeast with pseudohyphae
- B. Septate hyphae
- C. Irregular non-septate hyphae (Correct Answer)
- D. Spherules containing endospores
- E. Budding yeast with a narrow base
Diagnostic approaches for dimorphic fungi Explanation: ***Irregular non-septate hyphae***
- The clinical presentation of a **leukemic patient** with a **frontal lobe abscess** and **paranasal swelling**, along with headache, facial pain, and nasal discharge, strongly suggests **mucormycosis**.
- Mucormycosis is characterized by **broad, ribbon-like, irregular non-septate hyphae** with **right-angle branching** on tissue biopsy, making this the most likely finding.
*Yeast with pseudohyphae*
- This morphology is characteristic of **Candida species**, which can cause opportunistic infections but typically manifest as candidemia, esophagitis, or vulvovaginitis in immunocompromised patients, not usually a frontal lobe abscess with paranasal involvement.
- While Candida can cause severe systemic infections, the specific combination of a frontal lobe abscess and paranasal swelling points away from Candida as the primary cause in this context.
*Septate hyphae*
- **Septate hyphae** are typical of **Aspergillus species**, which can cause invasive aspergillosis, including sinopulmonary infections and CNS involvement in immunocompromised hosts.
- However, Aspergillus hyphae are typically **narrow (3-6 µm)** with **acute-angle (45-degree) branching**, differentiating them from the broad, irregular hyphae seen in mucormycosis.
*Spherules containing endospores*
- This morphology is characteristic of **Coccidioides immitis**, the causative agent of coccidioidomycosis.
- Coccidioidomycosis is geographically restricted to endemic areas (e.g., southwestern US) and typically presents with pulmonary symptoms, disseminated disease, or meningitis, which does not fit the described paranasal and frontal lobe presentation.
*Budding yeast with a narrow base*
- This morphology is characteristic of **Cryptococcus neoformans**, an encapsulated yeast that commonly causes **meningitis** and **pneumonia** in immunocompromised individuals.
- While Cryptococcus can cause CNS infections, the presence of paranasal swelling and the specific description of a frontal lobe abscess make mucormycosis a more fitting diagnosis.
Diagnostic approaches for dimorphic fungi US Medical PG Question 7: You are seeing an otherwise healthy 66-year-old male in clinic who is complaining of localized back pain and a new rash. On physical exam, his vital signs are within normal limits. You note a vesicular rash restricted to the upper left side of his back. In order to confirm your suspected diagnosis, you perform a diagnostic test. What would you expect to find on the diagnostic test that was performed?
- A. Gram negative bacilli
- B. Branching pseudohyphae
- C. Pear shaped motile cells
- D. Multinucleated giant cells (Correct Answer)
- E. Gram positive cocci
Diagnostic approaches for dimorphic fungi Explanation: ***Multinucleated giant cells***
- The patient's presentation of a **unilateral, vesicular rash** in an older adult, along with localized back pain, is highly suggestive of **herpes zoster (shingles)**.
- A Tzanck smear, a common diagnostic test for vesicular lesions, would reveal **multinucleated giant cells** and **intranuclear inclusions**, characteristic cytopathic effects of herpesviruses like VZV.
*Gram negative bacilli*
- This finding would suggest a **bacterial infection**, typically not associated with vesicular rashes like shingles.
- Gram-negative bacilli are often implicated in conditions such as **urinary tract infections** or **sepsis**, not dermatological viral infections.
*Branching pseudohyphae*
- This microscopic feature is characteristic of **fungal infections**, specifically **Candida species**, which present as a candidiasis rash, not a dermatomal vesicular rash.
- Fungal rashes are typically erythematous and can be pruritic but do not usually form discrete vesicles in a dermatomal distribution.
*Pear shaped motile cells*
- This describes **Trichomonas vaginalis**, a parasite causing sexually transmitted infections, primarily **vaginitis** or **urethritis**.
- This finding would be completely unrelated to a vesicular skin rash or the suspected diagnosis of shingles.
*Gram positive cocci*
- This finding is indicative of a **bacterial infection**, such as those caused by **Staphylococcus aureus** or **Streptococcus pyogenes**.
- While these bacteria can cause skin infections (e.g., impetigo, cellulitis), they do not produce the classic unilateral vesicular rash of shingles and would not involve multinucleated giant cells on microscopy.
Diagnostic approaches for dimorphic fungi US Medical PG Question 8: A 40-year-old farmer from Ohio seeks evaluation at a clinic with complaints of a chronic cough, fevers, and anorexia of several months duration. On examination, he has generalized lymphadenopathy with hepatosplenomegaly. A chest radiograph reveals local infiltrates and patchy opacities involving all lung fields. Fine needle aspiration of an enlarged lymph node shows the presence of intracellular yeast. A fungal culture shows the presence of smooth, thin-walled microconidia and tuberculate macroconidia. Which of the following is the most likely diagnosis?
- A. Coccidioidomycosis
- B. Blastomycosis
- C. Cryptococcosis
- D. Histoplasmosis (Correct Answer)
- E. Sporotrichosis
Diagnostic approaches for dimorphic fungi Explanation: ***Histoplasmosis***
- **Histoplasmosis** is characterized by the presence of **intracellular yeast** in tissue samples and **tuberculate macroconidia** in fungal cultures, which are key diagnostic findings in this case.
- The patient's presentation with chronic cough, fevers, anorexia, generalized lymphadenopathy, hepatosplenomegaly, and lung infiltrates, along with geographic exposure in **Ohio** (part of the Ohio River Valley endemic area), is highly consistent with disseminated histoplasmosis.
*Coccidioidomycosis*
- While coccidioidomycosis can cause lung infiltrates, it is typically endemic to the **southwestern United States** and Mexico, not Ohio.
- Microscopic examination would reveal **spherules** containing endospores, not intracellular yeast with tuberculate macroconidia.
*Blastomycosis*
- Blastomycosis is also endemic to the Ohio River Valley, but it is characterized by **broad-based budding yeast** in tissue, and its cultures typically do not show tuberculate macroconidia.
- While it causes pulmonary and disseminated disease, the specific microscopic and culture findings differentiate it from histoplasmosis.
*Cryptococcosis*
- Cryptococcosis primarily affects immunocompromised individuals and is characterized by encapsulated yeast, which would be visible with India ink stain.
- It typically presents as **meningitis** or pneumonia, and its culture morphology does not include tuberculate macroconidia.
*Sporotrichosis*
- Sporotrichosis is commonly associated with **cutaneous lesions** following traumatic inoculation of spores from soil or vegetation, and it rarely causes disseminated disease with extensive systemic symptoms like those described.
- The yeast forms in tissue are typically smaller and cigar-shaped, and the culture morphology differs significantly from what is described.
Diagnostic approaches for dimorphic fungi US Medical PG Question 9: An investigator is studying growth patterns of various fungal pathogens. Incubation of an isolated fungus at 25°C shows branching hyphae with rosettes of conidia under light microscopy. After incubation at 37°C, microscopic examination of the same organism instead shows smooth, white colonies with rounded, elongated cells. Infection with the investigated pathogen is most likely to cause which of the following conditions?
- A. Pityriasis versicolor
- B. Candidiasis
- C. Cryptococcosis
- D. Sporotrichosis (Correct Answer)
- E. Coccidioidomycosis
Diagnostic approaches for dimorphic fungi Explanation: ***Sporotrichosis***
- The description of a fungal pathogen exhibiting **thermal dimorphism** (different forms at 25°C and 37°C) is characteristic of **Sporothrix schenckii**.
- At 25°C, it typically grows as **mold with branching hyphae and conidia in rosettes**, and at 37°C, it grows as **yeast-like cells (cigar-shaped bodies in tissue)**, which can appear rounded and elongated.
*Pityriasis versicolor*
- Caused by **Malassezia globosa**, which is a **lipophilic yeast** and does not exhibit thermal dimorphism described here.
- Characterized by **hypo- or hyperpigmented skin patches**, not deep tissue infection with dimorphic growth.
*Candidiasis*
- Caused by **Candida species**, which are **opportunistic yeasts** that can form pseudohyphae and true hyphae but do not display the specific dimorphism with rosettes of conidia at 25°C.
- Infections range from superficial mucocutaneous to systemic, but the fungal morphology described does not fit.
*Cryptococcosis*
- Caused by **Cryptococcus neoformans** or **Cryptococcus gattii**, which are **encapsulated yeasts** and do not exhibit dimorphism (mold at 25°C, yeast at 37°C).
- Primarily causes **meningoencephalitis** or pulmonary disease, and is identified by its capsule and yeast form.
*Coccidioidomycosis*
- Caused by **Coccidioides immitis** or **Coccidioides posadasii**, which are **thermally dimorphic fungi**, but their morphology differs from the description.
- At 25°C, they grow as molds with **arthroconidia**, and at 37°C, they form **spherules containing endospores** in tissue, not smooth, white colonies with rounded, elongated cells.
Diagnostic approaches for dimorphic fungi US Medical PG Question 10: A 16-year-old boy presents to his pediatrician because he has noticed white plaques forming on his tongue over the last 5 days. He recently returned from a boy scout trip where he traveled across the country and hiked through the woods. His past medical history is significant for asthma for which he uses an inhaler as needed. He says that during the trip he felt short of breath several times and had to use the inhaler. He also says that several of his friends appeared to get sick on the same trip and were coughing a lot. He has not experienced any other symptoms since returning from the trip. On presentation, he is found to have white plaques on the tongue that can be scraped off. Which of the following is a characteristic of the most likely cause of this patient's disease?
- A. Acute angle branching
- B. Spherules containing endospores
- C. Germ tube formation (Correct Answer)
- D. Latex agglutination
- E. Broad-based budding
Diagnostic approaches for dimorphic fungi Explanation: ***Germ tube formation***
- This patient presents with **oral thrush (candidiasis)**, characterized by **white plaques on the tongue that can be scraped off**. His history of **asthma and inhaler use** (likely corticosteroids) is a risk factor.
- **Germ tube formation** is a rapid diagnostic test for *Candida albicans*, the most common cause of oral thrush, where yeast cells produce filament-like extensions when incubated in serum.
*Acute angle branching*
- This is characteristic of **Aspergillus species**, which typically cause invasive mold infections in immunocompromised individuals, or allergic bronchopulmonary aspergillosis, not oral thrush.
- *Aspergillus* infections are not typically associated with easily scraped-off oral plaques.
*Spherules containing endospores*
- **Spherules containing endospores** are the characteristic tissue form of **Coccidioides immitis/posadasii**, a dimorphic fungus causing coccidioidomycosis (Valley fever), typically presenting as a pulmonary infection.
- This feature is not associated with *Candida albicans* or oral thrush, though the patient's travel history could suggest dimorphic fungal exposure.
*Latex agglutination*
- **Latex agglutination** is a serological test primarily used for detecting **cryptococcal capsular antigen** in cerebrospinal fluid or serum, indicating cryptococcosis.
- It is not a characteristic feature or primary diagnostic method for *Candida* infections like oral thrush.
*Broad-based budding*
- **Broad-based budding** is a microscopic characteristic of **Blastomyces dermatitidis**, a dimorphic fungus causing blastomycosis, typically a pulmonary infection that can disseminate to skin, bone, or other organs.
- This feature is not associated with *Candida albicans* or oral thrush.
More Diagnostic approaches for dimorphic fungi US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.