Coccidioides immitis/posadasii US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Coccidioides immitis/posadasii. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Coccidioides immitis/posadasii US Medical PG Question 1: A 44-year-old man comes to the physician because of a 3-week history of productive cough, fever, and lethargy. He also has several skin lesions over his body. His symptoms began 3 weeks after he returned from a camping trip in Kentucky. Three years ago, he underwent kidney transplantation for polycystic kidney disease. Current medications include sirolimus and prednisone. His temperature is 38°C (100.4°F). Diffuse crackles are heard over the lung fields. There are 4 white, verrucous skin patches over his chest and upper limbs. A photomicrograph of a skin biopsy specimen from one of the lesions is shown. Which of the following is the most likely diagnosis?
- A. Coccidioidomycosis
- B. Mucormycosis
- C. Blastomycosis (Correct Answer)
- D. Cryptococcosis
- E. Histoplasmosis
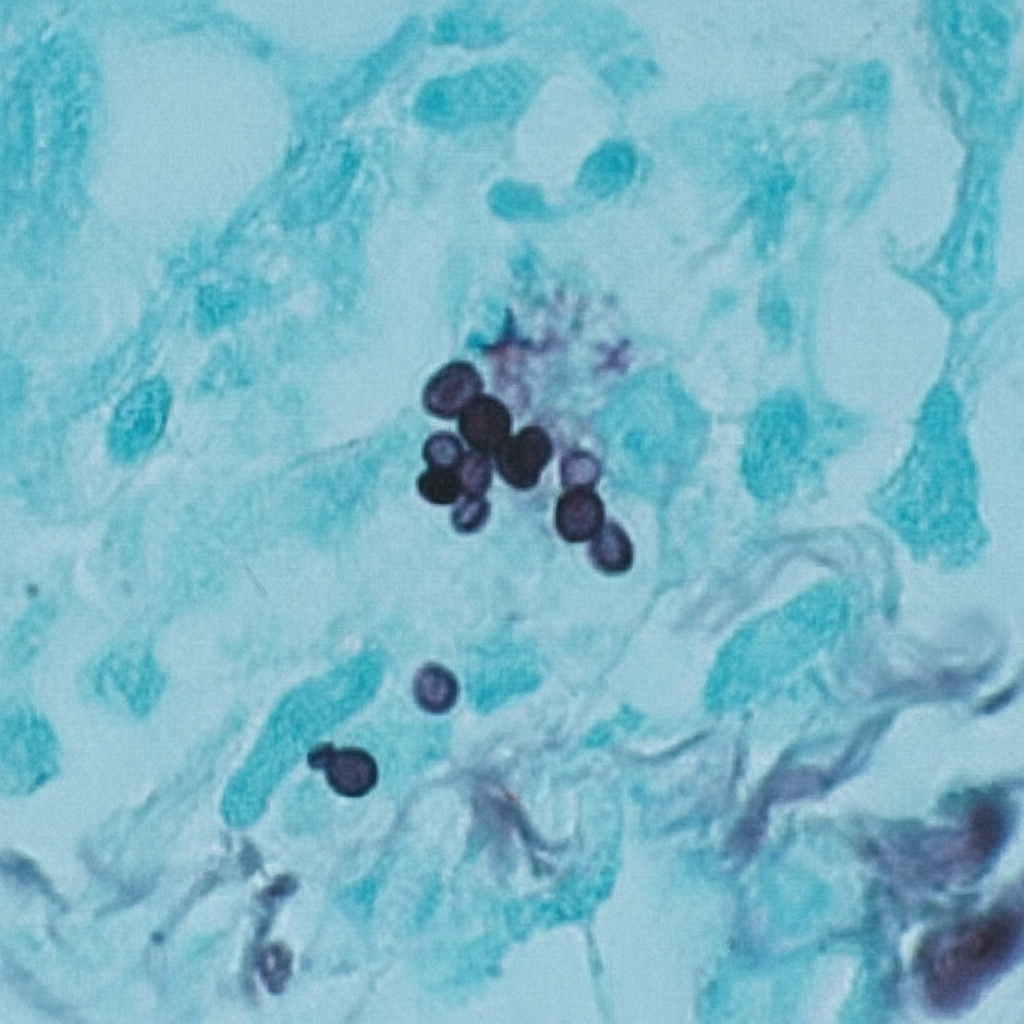
Coccidioides immitis/posadasii Explanation: ***Blastomycosis***
- The patient's history of **camping in Kentucky**, along with the presence of **pulmonary symptoms** (productive cough, fever, crackles) and **verrucous skin lesions**, are classic for blastomycosis.
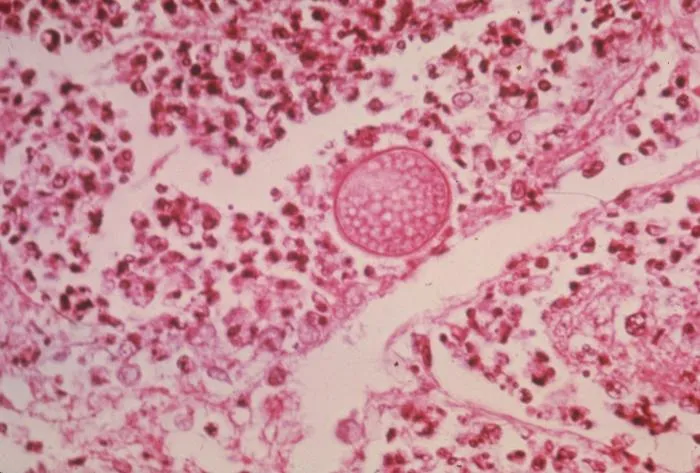
- The photomicrograph showing **broad-based budding yeast** is pathognomonic for *Blastomyces dermatitidis*.
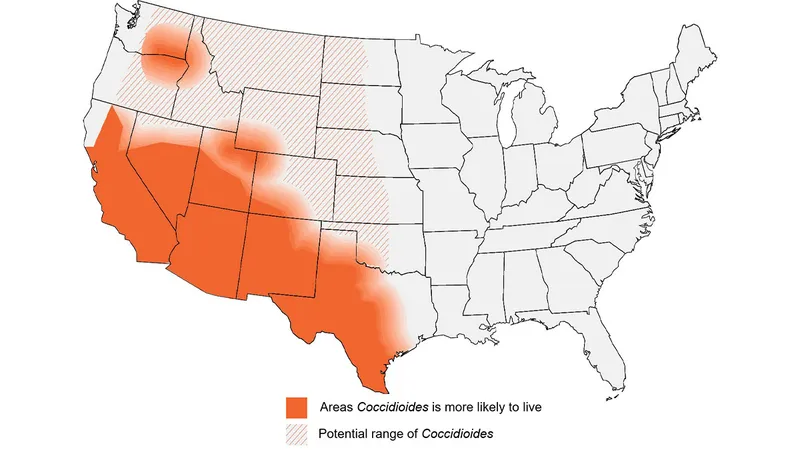
*Coccidioidomycosis*
- This is typical in the **Southwestern United States and parts of Mexico**, not Kentucky.
- Microscopic examination would reveal **spherules containing endospores**, which are not seen in the provided image.
*Mucormycosis*
- This infection is characterized by **irregular, broad, non-septate hyphae** with **wide-angle branching**, often invading blood vessels, leading to tissue necrosis.
- It primarily affects immunocompromised patients but typically presents as **rhinocerebral** or **pulmonary infection**, less commonly with verrucous skin lesions of this type.
*Cryptococcosis*
- Primarily affects the **lungs and central nervous system**, especially in immunocompromised individuals.
- Microscopy typically shows **encapsulated yeast** cells, which would be visible with India ink stain, and are not represented by the broad-based budding in the image.
*Histoplasmosis*
- Prevalent in the **Ohio and Mississippi River Valleys**, which includes Kentucky, and is often associated with **bird or bat droppings**.
- On microscopy, it presents as **small intracellular yeast** within macrophages, which is morphologically distinct from the large, broad-based budding yeast shown.
Coccidioides immitis/posadasii US Medical PG Question 2: A 58-year-old woman visits a physician because of fever, chills, dry cough, and a few enlarging masses on her cheeks and neck. Wart-like lesions are present on the nose as shown in the photograph. She reports that she visited the Mississippi area a few months before on a business trip. Her temperature is 38.1°C (100.6°F), the pulse is 80/min, and the blood pressure is 121/78 mm Hg. A fine needle aspirate of the lymph node is sent for pathological investigation. Culture growth shows white colonies on Sabouraud glucose agar (SGA). Which of the following is the most likely causal organism?
- A. Histoplasma capsulatum
- B. Malassezia furfur
- C. Blastomyces dermatitidis (Correct Answer)
- D. Coccidioides immitis
- E. Aspergillus fumigatus
Coccidioides immitis/posadasii Explanation: ***Blastomyces dermatitidis***
- The patient's symptoms, including **fever, chills, dry cough, enlarging masses on cheeks and neck, and wart-like lesions on the nose**, along with a history of travel to the **Mississippi area**, are highly characteristic of **blastomycosis**.
- **_Blastomyces dermatitidis_** is a dimorphic fungus endemic to the **Ohio and Mississippi River valleys** and the Great Lakes region, often causing pulmonary disease that can disseminate to the skin, bones, and other organs, producing lesions such as those described.
*Histoplasma capsulatum*
- This fungus is also endemic to the **Ohio and Mississippi River valleys** but typically causes **histoplasmosis**, which often presents with asymptomatic lung infection, or in severe cases, disseminated disease with **hepatosplenomegaly** and **oral ulcers**, rather than aggressive cutaneous **wart-like lesions**.
- While it can cause pulmonary symptoms, the prominent **skin lesions** and masses described are less typical for disseminated histoplasmosis compared to **blastomycosis**.
*Malassezia furfur*
- **_Malassezia furfur_** is associated with superficial fungal infections like **tinea versicolor** (pityriasis versicolor), which presents as hypopigmented or hyperpigmented patches on the skin, mainly on the trunk and upper extremities.
- It does not typically cause **deep-seated infections** with systemic symptoms (fever, chills, cough) or **wart-like lesions** on the nose and neck masses.
*Coccidioides immitis*
- **_Coccidioides immitis_** is endemic to the **southwestern United States** (e.g., California, Arizona) and is the causative agent of **Coccidioidomycosis** (Valley Fever).
- While it can cause pulmonary symptoms and disseminate, the classic dermatological manifestations are often **erythema nodosum** or **erythema multiforme**, not the wart-like, verrucous lesions described in this case, and its endemic region does not fit the patient's travel history to Mississippi.
*Aspergillus fumigatus*
- **_Aspergillus fumigatus_** is an opportunistic mold that primarily causes allergic bronchopulmonary aspergillosis (ABPA), aspergilloma (fungus ball in pre-existing lung cavities), or invasive aspergillosis in **immunocompromised individuals**.
- It is not typically associated with cutaneous **wart-like lesions** or the specific endemic pattern and systemic symptoms described in an otherwise seemingly immunocompetent individual in the Mississippi region.
Coccidioides immitis/posadasii US Medical PG Question 3: A young woman from the Ohio River Valley in the United States currently on corticosteroid therapy for ulcerative colitis presented to a clinic complaining of fever, sweat, headache, nonproductive cough, malaise, and general weakness. A chest radiograph revealed patchy pneumonia in the lower lung fields, together with enlarged mediastinal and hilar lymph nodes. Skin changes suggestive of erythema nodosum (i.e. an acute erythematous eruption) were noted. Because the patient was from a region endemic for fungal infections associated with her symptoms and the patient was in close contact with a person presenting similar symptoms, the attending physician suspected that systemic fungal infection might be responsible for this woman’s illness. Which of the following laboratory tests can the physician use to ensure early detection of the disease, and also effectively monitor the treatment response?
- A. Skin tests
- B. Fungal staining
- C. Antigen detection (Correct Answer)
- D. Culture method
- E. Antibody testing
Coccidioides immitis/posadasii Explanation: ***Antigen detection***
- **Antigen detection assays** (e.g., *Histoplasma galactomannan antigen*) are highly sensitive for **disseminated histoplasmosis**, especially in immunosuppressed patients like this one on corticosteroids.
- They provide **early diagnosis** and are effective for **monitoring treatment response**, as antigen levels typically decrease with successful therapy.
*Skin tests*
- **Skin tests** (e.g., *histoplasmin skin test*) indicate **prior exposure** to the fungus and are not useful for diagnosing active, acute infection.
- A positive skin test does not differentiate between past exposure and current disease, making it unsuitable for early detection or monitoring.
*Fungal staining*
- **Fungal staining** of patient samples (e.g., sputum, biopsy) can reveal fungal elements but has **limited sensitivity** and may not identify the specific pathogen.
- It often requires **invasive procedures** to obtain suitable specimens and is not ideal for routine monitoring of treatment response due to variability.
*Culture method*
- **Fungal cultures** are a **definitive diagnostic method** but can take **several weeks** to yield results, which is too slow for early detection in an acutely ill patient.
- While useful for species identification and susceptibility testing, the **delayed turnaround time** makes it impractical for monitoring rapid treatment changes.
*Antibody testing*
- **Antibody tests** for fungal infections can be useful but may show **false negatives in immunocompromised patients** (like this patient on corticosteroids) due to a blunted immune response.
- Seroconversion or a significant rise in antibody titers can indicate infection, but antibodies may **persist long after resolution**, making them less reliable for monitoring acute treatment efficacy.
Coccidioides immitis/posadasii US Medical PG Question 4: An investigator is studying growth patterns of various fungal pathogens. Incubation of an isolated fungus at 25°C shows branching hyphae with rosettes of conidia under light microscopy. After incubation at 37°C, microscopic examination of the same organism instead shows smooth, white colonies with rounded, elongated cells. Infection with the investigated pathogen is most likely to cause which of the following conditions?
- A. Pityriasis versicolor
- B. Candidiasis
- C. Cryptococcosis
- D. Sporotrichosis (Correct Answer)
- E. Coccidioidomycosis
Coccidioides immitis/posadasii Explanation: ***Sporotrichosis***
- The description of a fungal pathogen exhibiting **thermal dimorphism** (different forms at 25°C and 37°C) is characteristic of **Sporothrix schenckii**.
- At 25°C, it typically grows as **mold with branching hyphae and conidia in rosettes**, and at 37°C, it grows as **yeast-like cells (cigar-shaped bodies in tissue)**, which can appear rounded and elongated.
*Pityriasis versicolor*
- Caused by **Malassezia globosa**, which is a **lipophilic yeast** and does not exhibit thermal dimorphism described here.
- Characterized by **hypo- or hyperpigmented skin patches**, not deep tissue infection with dimorphic growth.
*Candidiasis*
- Caused by **Candida species**, which are **opportunistic yeasts** that can form pseudohyphae and true hyphae but do not display the specific dimorphism with rosettes of conidia at 25°C.
- Infections range from superficial mucocutaneous to systemic, but the fungal morphology described does not fit.
*Cryptococcosis*
- Caused by **Cryptococcus neoformans** or **Cryptococcus gattii**, which are **encapsulated yeasts** and do not exhibit dimorphism (mold at 25°C, yeast at 37°C).
- Primarily causes **meningoencephalitis** or pulmonary disease, and is identified by its capsule and yeast form.
*Coccidioidomycosis*
- Caused by **Coccidioides immitis** or **Coccidioides posadasii**, which are **thermally dimorphic fungi**, but their morphology differs from the description.
- At 25°C, they grow as molds with **arthroconidia**, and at 37°C, they form **spherules containing endospores** in tissue, not smooth, white colonies with rounded, elongated cells.
Coccidioides immitis/posadasii US Medical PG Question 5: A 47-year-old woman comes to the physician because of a 3-day history of fever, fatigue, loss of appetite, cough, and chest pain. Physical examination shows diffuse inspiratory crackles over the left lung field. An x-ray of the chest shows hilar lymphadenopathy and well-defined nodules with central calcifications. Urine studies show the presence of a polysaccharide antigen. A biopsy specimen of the lung shows cells with basophilic, crescent-shaped nuclei and pericellular halos located within macrophages. This patient's history is most likely to show which of the following?
- A. Visit to Arizona desert
- B. Recent trip to Brazil
- C. Previous mycobacterial infection
- D. Exposure to bat droppings (Correct Answer)
- E. Treatment with inhaled glucocorticoids
Coccidioides immitis/posadasii Explanation: ***Exposure to bat droppings***
- The clinical presentation, including fever, cough, chest pain, **hilar lymphadenopathy**, **nodules with central calcifications**, and **intracellular encapsulated yeasts** in macrophages, is classic for **histoplasmosis**.
- **Histoplasma capsulatum** is endemic to the Ohio and Mississippi River valleys and is transmitted through inhalation of spores from soil contaminated with **bat or bird droppings**.
*Visit to Arizona desert*
- Exposure in the **Arizona desert** is associated with **coccidioidomycosis** (Valley Fever), which presents with similar pulmonary symptoms but is caused by Coccidioides immitis/posadasii, characterized by **spherules** containing endospores.
- While it can cause hilar lymphadenopathy and nodules, the characteristic intracellular budding yeasts within macrophages and the polysaccharide antigen in urine point away from coccidioidomycosis.
*Recent trip to Brazil*
- A trip to **Brazil** might suggest diseases like **Paracoccidioidomycosis**, which presents with chronic mucocutaneous or disseminated lesions, or various tropical infections, but is not typically characterized by the specific pulmonary and microscopic findings described here.
- The histopathological findings of **intracellular yeasts with pericellular halos** (consistent with Histoplasma) would not be the primary finding for paracoccidioidomycosis, which generally shows characteristic **"pilot wheel"** or multiple budding yeasts.
*Previous mycobacterial infection*
- A previous **mycobacterial infection** would lead to tuberculosis, characterized by **acid-fast bacilli** and granulomas with **caseating necrosis**, which is different from the described intracellular yeasts and polysaccharide antigen.
- While tuberculosis can cause hilar lymphadenopathy and pulmonary nodules, the given microscopic description of cells with basophilic nuclei and pericellular halos within macrophages does not fit Mycobacterium tuberculosis.
*Treatment with inhaled glucocorticoids*
- Inhaled glucocorticoids are used to treat conditions like asthma or COPD and, while prolonged use can rarely predispose to **opportunistic fungal infections** (e.g., aspergillosis, candidiasis), they are not a cause of this specific clinical presentation or the microbiological findings of histoplasmosis.
- The use of inhaled steroids would not explain the geographic exposure, hilar lymphadenopathy, or the specific appearance of the fungal elements within macrophages described.
Coccidioides immitis/posadasii US Medical PG Question 6: A 73-year-old man presents to the office, complaining of “weird blisters” on his right hand, which appeared 2 weeks ago. The patient says that he initially had a rash, which progressed to blisters. He denies any trauma or known contact with sick people. He is worried because he hasn’t been able to garden since the rash appeared, and he was planning on entering his roses into an annual competition this month. His vital signs are stable. On physical exam, the patient has multiple bullae accompanied by red, papular lesions on his right hand, which progress to his forearm. The right axillary lymph nodes are swollen and tender. What is the treatment for the most likely diagnosis of this patient?
- A. Itraconazole (Correct Answer)
- B. Azithromycin
- C. Topical corticosteroids
- D. Doxycycline
- E. Potassium iodide solution
Coccidioides immitis/posadasii Explanation: ***Itraconazole***
- This patient likely has **sporotrichosis**, a subcutaneous fungal infection, given the history of **gardening** (exposure to soil/plants), **papular lesions progressing to blisters**, and **lymphatic spread** (swollen axillary lymph nodes).
- **Itraconazole** is the **first-line treatment** for cutaneous and lymphocutaneous sporotrichosis.
*Azithromycin*
- **Azithromycin** is an **antibiotic** used to treat bacterial infections, not fungal infections like sporotrichosis.
- It is often used for respiratory tract infections, sexually transmitted infections, and some skin infections.
*Topical corticosteroids*
- **Topical corticosteroids** are anti-inflammatory agents that would likely worsen a fungal infection by suppressing the immune response.
- They are used for inflammatory dermatoses like eczema or psoriasis and would not be effective against sporotrichosis.
*Doxycycline*
- **Doxycycline** is a broad-spectrum **antibiotic**, effective against a variety of bacterial infections, including some atypical pathogens.
- It has no antifungal activity and would not be an appropriate treatment for sporotrichosis.
*Potassium iodide solution*
- While traditionally used for sporotrichosis, **potassium iodide (KI) solution** is now considered a **second-line treatment** due to its side effects and the availability of more effective and safer antifungals like itraconazole.
- It is used only in cases where itraconazole is contraindicated or ineffective.
Coccidioides immitis/posadasii US Medical PG Question 7: A 40-year-old farmer from Ohio seeks evaluation at a clinic with complaints of a chronic cough, fevers, and anorexia of several months duration. On examination, he has generalized lymphadenopathy with hepatosplenomegaly. A chest radiograph reveals local infiltrates and patchy opacities involving all lung fields. Fine needle aspiration of an enlarged lymph node shows the presence of intracellular yeast. A fungal culture shows the presence of smooth, thin-walled microconidia and tuberculate macroconidia. Which of the following is the most likely diagnosis?
- A. Coccidioidomycosis
- B. Blastomycosis
- C. Cryptococcosis
- D. Histoplasmosis (Correct Answer)
- E. Sporotrichosis
Coccidioides immitis/posadasii Explanation: ***Histoplasmosis***
- **Histoplasmosis** is characterized by the presence of **intracellular yeast** in tissue samples and **tuberculate macroconidia** in fungal cultures, which are key diagnostic findings in this case.
- The patient's presentation with chronic cough, fevers, anorexia, generalized lymphadenopathy, hepatosplenomegaly, and lung infiltrates, along with geographic exposure in **Ohio** (part of the Ohio River Valley endemic area), is highly consistent with disseminated histoplasmosis.
*Coccidioidomycosis*
- While coccidioidomycosis can cause lung infiltrates, it is typically endemic to the **southwestern United States** and Mexico, not Ohio.
- Microscopic examination would reveal **spherules** containing endospores, not intracellular yeast with tuberculate macroconidia.
*Blastomycosis*
- Blastomycosis is also endemic to the Ohio River Valley, but it is characterized by **broad-based budding yeast** in tissue, and its cultures typically do not show tuberculate macroconidia.
- While it causes pulmonary and disseminated disease, the specific microscopic and culture findings differentiate it from histoplasmosis.
*Cryptococcosis*
- Cryptococcosis primarily affects immunocompromised individuals and is characterized by encapsulated yeast, which would be visible with India ink stain.
- It typically presents as **meningitis** or pneumonia, and its culture morphology does not include tuberculate macroconidia.
*Sporotrichosis*
- Sporotrichosis is commonly associated with **cutaneous lesions** following traumatic inoculation of spores from soil or vegetation, and it rarely causes disseminated disease with extensive systemic symptoms like those described.
- The yeast forms in tissue are typically smaller and cigar-shaped, and the culture morphology differs significantly from what is described.
Coccidioides immitis/posadasii US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Coccidioides immitis/posadasii Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Coccidioides immitis/posadasii US Medical PG Question 9: A 52-year-old man comes to the physician because of a 4-day history of a productive cough, shortness of breath, and low-grade fever. He works as a farmer in southern Arizona. Physical examination shows multiple skin lesions with a dark blue center, pale intermediate zone, and red peripheral rim on the upper and lower extremities. There are diffuse crackles on the left side of the chest. An x-ray of the chest shows left basilar consolidation and left hilar lymphadenopathy. A photomicrograph of tissue obtained from a biopsy of the lung is shown. Which of the following is the most likely causal pathogen?
- A. Coccidioides immitis (Correct Answer)
- B. Paracoccidioides brasiliensis
- C. Candida albicans
- D. Blastomyces dermatitidis
- E. Aspergillus fumigatus
Coccidioides immitis/posadasii Explanation: ***Coccidioides immitis***
- The patient's presentation with **respiratory symptoms**, **skin lesions** (erythema multiforme-like), and **hilar lymphadenopathy** in a farmer from **southern Arizona** is highly characteristic of coccidioidomycosis. The image shows **spherules** containing **endospores**, which are diagnostic of *Coccidioides*.
- *Coccidioides immitis* is a **dimorphic fungus** endemic to the **Southwestern United States** (including Arizona) and parts of Mexico and Central/South America, commonly causing **valley fever**.
*Paracoccidioides brasiliensis*
- This fungus is associated with **Paracoccidioidomycosis**, which is primarily found in **Latin America** (excluding the US Southwest).
- Microscopically, it presents as a **captain's wheel** appearance with multiple buds, which is not seen here.
*Candida albicans*
- *Candida albicans* is a **yeast** that typically causes **mucocutaneous infections** (e.g., thrush, vaginitis) and can cause systemic candidiasis in immunocompromised individuals.
- It forms **pseudohyphae and budding yeasts** microscopically, which are distinct from the spherules seen in the image.
*Blastomyces dermatitidis*
- **Blastomycosis** is endemic to the **Great Lakes region and Ohio/Mississippi River valleys** and usually presents with pneumonia and skin lesions.
- Microscopic examination reveals **broad-based budding yeasts**, which are different from the features shown in the image.
*Aspergillus fumigatus*
- *Aspergillus fumigatus* causes various conditions, including allergic bronchopulmonary aspergillosis (ABPA), aspergilloma, and invasive aspergillosis, particularly in **immunocompromised patients**.
- Microscopically, it is characterized by **acute-angle branching septate hyphae**, which is not consistent with the image provided.
Coccidioides immitis/posadasii US Medical PG Question 10: A 29-year-old woman comes to the military physician because of a 2-day history of fever, joint pain, dry cough, chest pain, and a painful red rash on her lower legs. Two weeks ago, she returned from military training in Southern California. She appears ill. Her temperature is 39°C (102.1°F). Physical examination shows diffuse inspiratory crackles over all lung fields and multiple tender erythematous nodules over the anterior aspect of both legs. A biopsy specimen of this patient's lungs is most likely to show which of the following?
- A. Septate hyphae with acute-angle branching
- B. Spherules filled with endospores (Correct Answer)
- C. Broad-based budding yeast
- D. Encapsulated yeast with narrow-based budding
- E. Oval, budding yeast with pseudohyphae
Coccidioides immitis/posadasii Explanation: **Spherules filled with endospores**
- The patient's symptoms (fever, joint pain, dry cough, chest pain, erythema nodosum on legs) combined with her travel history to **Southern California** are highly suggestive of **Coccidioidomycosis** ("Valley Fever").
- A biopsy of affected lung tissue in coccidioidomycosis typically reveals **spherules** (thick-walled structures) containing numerous **endospores**, which are characteristic of the tissue phase of *Coccidioides immitis/posadasii*.
*Septate hyphae with acute-angle branching*
- This morphology is characteristic of **Aspergillus** species, which can cause opportunistic infections, especially in immunocompromised individuals.
- While it can cause lung infections, the clinical presentation and geographic exposure do not point towards aspergillosis as the most likely diagnosis.
*Broad-based budding yeast*
- This describes the characteristic morphology of *Blastomyces dermatitidis*, the causative agent of **Blastomycosis**.
- **Blastomycosis** is typically found in the Great Lakes region, Ohio, Mississippi River valleys, and southeastern United States, not Southern California.
*Encapsulated yeast with narrow-based budding*
- This describes **Cryptococcus neoformans**, which appears as an encapsulated yeast with narrow-based budding in tissue.
- While it can cause pulmonary disease, the classic presentation (erythema nodosum, acute illness after Southern California exposure) is not consistent with **cryptococcosis**, which typically presents subacutely in immunocompromised patients.
*Oval, budding yeast with pseudohyphae*
- This morphology is characteristic of *Candida albicans*, which commonly causes mucocutaneous infections and can cause systemic candidiasis, particularly in immunocompromised patients.
- The clinical picture of a healthy young woman with exposure in Southern California does not fit with a typical **Candida** infection.
More Coccidioides immitis/posadasii US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.