Blastomyces dermatitidis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Blastomyces dermatitidis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Blastomyces dermatitidis US Medical PG Question 1: A 54-year-old woman comes to the physician because of a painful skin lesion on her right leg for 1 month. It initially started out as a small red spot but has rapidly increased in size during this period. She remembers an ant bite on her leg prior to the lesion occurring. She was treated for anterior uveitis 8 months ago with corticosteroids. She has Crohn's disease, type 2 diabetes mellitus, and hypertension. Current medications include insulin, mesalamine, enalapril, and aspirin. She returned from Wisconsin after visiting her son 2 months ago. Her temperature is 37.6°C (98°F), pulse is 98/min, and blood pressure is 126/88 mm Hg. Examination shows pitting pedal edema of the lower extremities. There is a 4-cm tender ulcerative lesion on the anterior right leg with a central necrotic base and purplish irregular borders. There are dilated tortuous veins in both lower legs. Femoral and pedal pulses are palpated bilaterally. Which of the following is the most likely diagnosis?
- A. Pyoderma gangrenosum (Correct Answer)
- B. Basal cell carcinoma
- C. Squamous cell carcinoma
- D. Ecthyma gangrenosum
- E. Blastomycosis
Blastomyces dermatitidis Explanation: ***Pyoderma gangrenosum***
- The patient's history of **Crohn's disease**, **anterior uveitis**, and a rapidly progressing, **tender ulcerative lesion** with a **necrotic base** and **purplish irregular borders** are highly characteristic of pyoderma gangrenosum.
- The phenomenon of **pathergy** (exacerbation of lesions after minor trauma like a bug bite) further supports this diagnosis.
*Basal cell carcinoma*
- Typically presents as a **slow-growing lesion** with **pearly borders** and **telangiectasias**, not a rapidly enlarging, tender ulcer with a necrotic base.
- It is often associated with sun exposure and rarely presents with the systemic associations seen in this case.
*Squamous cell carcinoma*
- Usually appears as a **scaly, erythematous patch** or an **indurated nodule** that may ulcerate, but it is generally a chronic lesion and less acutely painful or rapidly progressing.
- While it can be aggressive, the clinical presentation and rapid progression with a necrotic center and systemic associations point away from this diagnosis.
*Ecthyma gangrenosum*
- This condition is caused by **Pseudomonas aeruginosa bacteremia** and is characterized by a central necrotic area surrounded by an erythematous halo, typically in immunocompromised patients.
- While there is some overlap in appearance, ecthyma gangrenosum is usually associated with **sepsis** and systemic signs of infection, which are not prominent here.
*Blastomycosis*
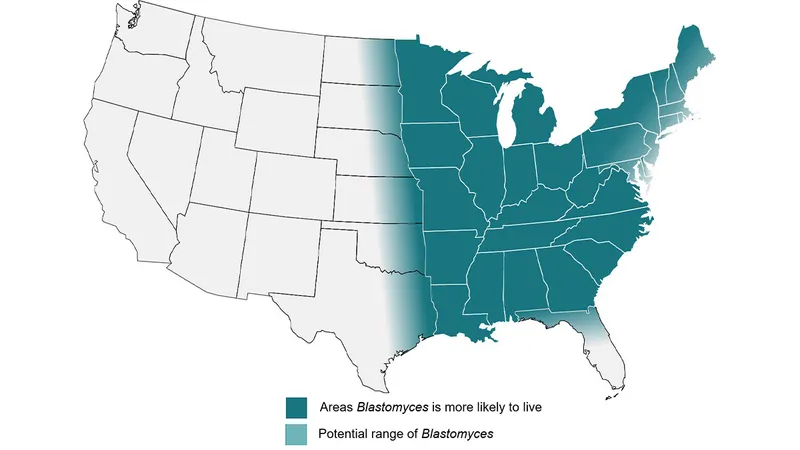
- A **fungal infection** endemic to the Great Lakes region (including Wisconsin), which can cause skin lesions that may be verrucous, ulcerative, or plaque-like.
- However, the description of a rapidly progressing, deeply ulcerative lesion with purplish, undermined borders and strong association with inflammatory bowel disease is more consistent with pyoderma gangrenosum.
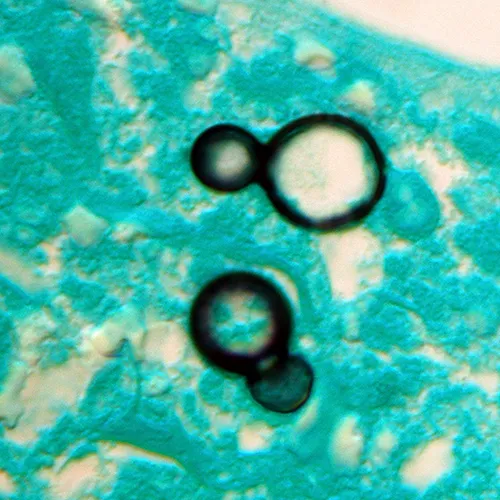
Blastomyces dermatitidis US Medical PG Question 2: A 44-year-old man comes to the physician because of a 3-week history of productive cough, fever, and lethargy. He also has several skin lesions over his body. His symptoms began 3 weeks after he returned from a camping trip in Kentucky. Three years ago, he underwent kidney transplantation for polycystic kidney disease. Current medications include sirolimus and prednisone. His temperature is 38°C (100.4°F). Diffuse crackles are heard over the lung fields. There are 4 white, verrucous skin patches over his chest and upper limbs. A photomicrograph of a skin biopsy specimen from one of the lesions is shown. Which of the following is the most likely diagnosis?
- A. Coccidioidomycosis
- B. Mucormycosis
- C. Blastomycosis (Correct Answer)
- D. Cryptococcosis
- E. Histoplasmosis
Blastomyces dermatitidis Explanation: ***Blastomycosis***
- The patient's history of **camping in Kentucky**, along with the presence of **pulmonary symptoms** (productive cough, fever, crackles) and **verrucous skin lesions**, are classic for blastomycosis.
- The photomicrograph showing **broad-based budding yeast** is pathognomonic for *Blastomyces dermatitidis*.
*Coccidioidomycosis*
- This is typical in the **Southwestern United States and parts of Mexico**, not Kentucky.
- Microscopic examination would reveal **spherules containing endospores**, which are not seen in the provided image.
*Mucormycosis*
- This infection is characterized by **irregular, broad, non-septate hyphae** with **wide-angle branching**, often invading blood vessels, leading to tissue necrosis.
- It primarily affects immunocompromised patients but typically presents as **rhinocerebral** or **pulmonary infection**, less commonly with verrucous skin lesions of this type.
*Cryptococcosis*
- Primarily affects the **lungs and central nervous system**, especially in immunocompromised individuals.
- Microscopy typically shows **encapsulated yeast** cells, which would be visible with India ink stain, and are not represented by the broad-based budding in the image.
*Histoplasmosis*
- Prevalent in the **Ohio and Mississippi River Valleys**, which includes Kentucky, and is often associated with **bird or bat droppings**.
- On microscopy, it presents as **small intracellular yeast** within macrophages, which is morphologically distinct from the large, broad-based budding yeast shown.
Blastomyces dermatitidis US Medical PG Question 3: A young woman from the Ohio River Valley in the United States currently on corticosteroid therapy for ulcerative colitis presented to a clinic complaining of fever, sweat, headache, nonproductive cough, malaise, and general weakness. A chest radiograph revealed patchy pneumonia in the lower lung fields, together with enlarged mediastinal and hilar lymph nodes. Skin changes suggestive of erythema nodosum (i.e. an acute erythematous eruption) were noted. Because the patient was from a region endemic for fungal infections associated with her symptoms and the patient was in close contact with a person presenting similar symptoms, the attending physician suspected that systemic fungal infection might be responsible for this woman’s illness. Which of the following laboratory tests can the physician use to ensure early detection of the disease, and also effectively monitor the treatment response?
- A. Skin tests
- B. Fungal staining
- C. Antigen detection (Correct Answer)
- D. Culture method
- E. Antibody testing
Blastomyces dermatitidis Explanation: ***Antigen detection***
- **Antigen detection assays** (e.g., *Histoplasma galactomannan antigen*) are highly sensitive for **disseminated histoplasmosis**, especially in immunosuppressed patients like this one on corticosteroids.
- They provide **early diagnosis** and are effective for **monitoring treatment response**, as antigen levels typically decrease with successful therapy.
*Skin tests*
- **Skin tests** (e.g., *histoplasmin skin test*) indicate **prior exposure** to the fungus and are not useful for diagnosing active, acute infection.
- A positive skin test does not differentiate between past exposure and current disease, making it unsuitable for early detection or monitoring.
*Fungal staining*
- **Fungal staining** of patient samples (e.g., sputum, biopsy) can reveal fungal elements but has **limited sensitivity** and may not identify the specific pathogen.
- It often requires **invasive procedures** to obtain suitable specimens and is not ideal for routine monitoring of treatment response due to variability.
*Culture method*
- **Fungal cultures** are a **definitive diagnostic method** but can take **several weeks** to yield results, which is too slow for early detection in an acutely ill patient.
- While useful for species identification and susceptibility testing, the **delayed turnaround time** makes it impractical for monitoring rapid treatment changes.
*Antibody testing*
- **Antibody tests** for fungal infections can be useful but may show **false negatives in immunocompromised patients** (like this patient on corticosteroids) due to a blunted immune response.
- Seroconversion or a significant rise in antibody titers can indicate infection, but antibodies may **persist long after resolution**, making them less reliable for monitoring acute treatment efficacy.
Blastomyces dermatitidis US Medical PG Question 4: An investigator is studying growth patterns of various fungal pathogens. Incubation of an isolated fungus at 25°C shows branching hyphae with rosettes of conidia under light microscopy. After incubation at 37°C, microscopic examination of the same organism instead shows smooth, white colonies with rounded, elongated cells. Infection with the investigated pathogen is most likely to cause which of the following conditions?
- A. Pityriasis versicolor
- B. Candidiasis
- C. Cryptococcosis
- D. Sporotrichosis (Correct Answer)
- E. Coccidioidomycosis
Blastomyces dermatitidis Explanation: ***Sporotrichosis***
- The description of a fungal pathogen exhibiting **thermal dimorphism** (different forms at 25°C and 37°C) is characteristic of **Sporothrix schenckii**.
- At 25°C, it typically grows as **mold with branching hyphae and conidia in rosettes**, and at 37°C, it grows as **yeast-like cells (cigar-shaped bodies in tissue)**, which can appear rounded and elongated.
*Pityriasis versicolor*
- Caused by **Malassezia globosa**, which is a **lipophilic yeast** and does not exhibit thermal dimorphism described here.
- Characterized by **hypo- or hyperpigmented skin patches**, not deep tissue infection with dimorphic growth.
*Candidiasis*
- Caused by **Candida species**, which are **opportunistic yeasts** that can form pseudohyphae and true hyphae but do not display the specific dimorphism with rosettes of conidia at 25°C.
- Infections range from superficial mucocutaneous to systemic, but the fungal morphology described does not fit.
*Cryptococcosis*
- Caused by **Cryptococcus neoformans** or **Cryptococcus gattii**, which are **encapsulated yeasts** and do not exhibit dimorphism (mold at 25°C, yeast at 37°C).
- Primarily causes **meningoencephalitis** or pulmonary disease, and is identified by its capsule and yeast form.
*Coccidioidomycosis*
- Caused by **Coccidioides immitis** or **Coccidioides posadasii**, which are **thermally dimorphic fungi**, but their morphology differs from the description.
- At 25°C, they grow as molds with **arthroconidia**, and at 37°C, they form **spherules containing endospores** in tissue, not smooth, white colonies with rounded, elongated cells.
Blastomyces dermatitidis US Medical PG Question 5: A 27-year-old female presents to her primary care physician because she is concerned about lighter colored patches on her skin. She recently went sunbathing and noticed that these areas also did not tan. Her doctor explains that she has a fungal infection of the skin that damages melanocytes by producing acids. She is prescribed selenium sulfide and told to follow-up in one month. Which of the following describes the appearance of the most likely infectious organism under microscopy?
- A. Broad based budding yeast
- B. "Captain's wheel" yeast
- C. Germ tube forming fungus
- D. Branching septate hyphae
- E. "Spaghetti and meatballs" fungus (Correct Answer)
Blastomyces dermatitidis Explanation: ***"Spaghetti and meatballs" fungus***
- The "spaghetti and meatballs" appearance on microscopy, referring to a mixture of short, septate hyphae and spherical yeast forms, is characteristic of **Malassezia globosa** or other *Malassezia* species, which cause **tinea versicolor**.
- **Tinea versicolor** presents as hypopigmented patches, especially after sun exposure, because the fungus produces **azelaic acid** that inhibits melanin synthesis.
*Broad based budding yeast*
- This description is characteristic of **Blastomyces dermatitidis**, which causes **blastomycosis**, a deep fungal infection.
- Blastomycosis typically manifests as pulmonary disease or disseminated lesions, not superficial hypopigmented skin patches.
*"Captain's wheel" yeast*
- The "captain's wheel" or multi-budding yeast appearance is characteristic of **Paracoccidioides brasiliensis**, the causative agent of **paracoccidioidomycosis**.
- This is a systemic mycosis primarily affecting the lungs and mucocutaneous areas, not a superficial skin infection like tinea versicolor.
*Germ tube forming fungus*
- The formation of **germ tubes** when incubated in serum at 37°C is a characteristic feature used to identify **Candida albicans**.
- *Candida* most commonly causes mucocutaneous candidiasis (e.g., thrush, vaginitis) or invasive infections, not hypopigmented skin patches that fail to tan.
*Branching septate hyphae*
- **Branching septate hyphae** are a general microscopic feature seen in many filamentous fungi, including dermatophytes like *Trichophyton* and *Microsporum*, which cause **tinea corporis** or **tinea pedis**.
- While dermatophytes cause skin infections, they typically result in erythematous, scaly, and often pruritic lesions and do not usually present as hypopigmented patches that fail to tan due to melanin inhibition, as seen in tinea versicolor.
Blastomyces dermatitidis US Medical PG Question 6: A 40-year-old farmer from Ohio seeks evaluation at a clinic with complaints of a chronic cough, fevers, and anorexia of several months duration. On examination, he has generalized lymphadenopathy with hepatosplenomegaly. A chest radiograph reveals local infiltrates and patchy opacities involving all lung fields. Fine needle aspiration of an enlarged lymph node shows the presence of intracellular yeast. A fungal culture shows the presence of smooth, thin-walled microconidia and tuberculate macroconidia. Which of the following is the most likely diagnosis?
- A. Coccidioidomycosis
- B. Blastomycosis
- C. Cryptococcosis
- D. Histoplasmosis (Correct Answer)
- E. Sporotrichosis
Blastomyces dermatitidis Explanation: ***Histoplasmosis***
- **Histoplasmosis** is characterized by the presence of **intracellular yeast** in tissue samples and **tuberculate macroconidia** in fungal cultures, which are key diagnostic findings in this case.
- The patient's presentation with chronic cough, fevers, anorexia, generalized lymphadenopathy, hepatosplenomegaly, and lung infiltrates, along with geographic exposure in **Ohio** (part of the Ohio River Valley endemic area), is highly consistent with disseminated histoplasmosis.
*Coccidioidomycosis*
- While coccidioidomycosis can cause lung infiltrates, it is typically endemic to the **southwestern United States** and Mexico, not Ohio.
- Microscopic examination would reveal **spherules** containing endospores, not intracellular yeast with tuberculate macroconidia.
*Blastomycosis*
- Blastomycosis is also endemic to the Ohio River Valley, but it is characterized by **broad-based budding yeast** in tissue, and its cultures typically do not show tuberculate macroconidia.
- While it causes pulmonary and disseminated disease, the specific microscopic and culture findings differentiate it from histoplasmosis.
*Cryptococcosis*
- Cryptococcosis primarily affects immunocompromised individuals and is characterized by encapsulated yeast, which would be visible with India ink stain.
- It typically presents as **meningitis** or pneumonia, and its culture morphology does not include tuberculate macroconidia.
*Sporotrichosis*
- Sporotrichosis is commonly associated with **cutaneous lesions** following traumatic inoculation of spores from soil or vegetation, and it rarely causes disseminated disease with extensive systemic symptoms like those described.
- The yeast forms in tissue are typically smaller and cigar-shaped, and the culture morphology differs significantly from what is described.
Blastomyces dermatitidis US Medical PG Question 7: A 4-month-old boy is brought to the physician by his father because of a progressively worsening rash on his buttocks for the last week. He cries during diaper changes and is more fussy than usual. Physical examination of the boy shows erythematous papules and plaques in the bilateral inguinal creases, on the scrotum, and in the gluteal cleft. Small areas of maceration are also present. A diagnosis is made, and treatment with topical clotrimazole is initiated. Microscopic examination of skin scrapings from this patient's rash is most likely to show which of the following findings?
- A. Round yeast surrounded by budding yeast cells
- B. Oval, budding yeast with pseudohyphae (Correct Answer)
- C. Broad-based budding yeast
- D. Fruiting bodies with septate, acute-angle hyphae
- E. Narrow budding, encapsulated yeast
Blastomyces dermatitidis Explanation: ***Oval, budding yeast with pseudohyphae***
- This morphology is characteristic of *Candida albicans*, which commonly causes **diaper rash** due to the warm, moist environment in the diaper area.
- The rash described, with **erythematous papules and plaques** in the inguinal creases, scrotum, and gluteal cleft, along with **maceration**, is typical of candidal diaper dermatitis.
*Round yeast surrounded by budding yeast cells*
- This description ("wagon wheel" appearance) is characteristic of *Malasseella globosa*, the causative agent of **tinea versicolor**.
- Tinea versicolor typically presents with hypo- or hyperpigmented patches, not the erythematous, macerated rash seen in this infant.
*Broad-based budding yeast*
- This morphology is characteristic of **Blastomycosis**, caused by *Blastomyces dermatitidis*.
- This infection typically causes **pulmonary disease** or **cutaneous lesions** that are often verrucous or ulcerative, not a diaper rash.
*Fruiting bodies with septate, acute-angle hyphae*
- This describes the microscopic appearance of *Aspergillus* species.
- *Aspergillus* typically causes **invasive pulmonary disease** in immunocompromised individuals or **allergic bronchopulmonary aspergillosis**, not diaper dermatitis.
*Narrow budding, encapsulated yeast*
- This is the characteristic microscopic appearance of *Cryptococcus neoformans*.
- *Cryptococcus* commonly causes **meningitis** or **pulmonary infections**, particularly in immunocompromised patients, and is not associated with diaper rash.
Blastomyces dermatitidis US Medical PG Question 8: A 3-month-old girl is brought to the emergency department because of a 2-day history of progressive difficulty breathing and a dry cough. Five weeks ago, she was diagnosed with diffuse hemangiomas involving the intrathoracic cavity and started treatment with prednisolone. She appears uncomfortable and in moderate respiratory distress. Her temperature is 38°C (100.4°F), pulse is 150/min, respirations are 50/min, and blood pressure is 88/50 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 87%. Oral examination shows a white plaque covering the tongue that bleeds when scraped. Chest examination shows subcostal and intercostal retractions. Scattered fine crackles and rhonchi are heard throughout both lung fields. Laboratory studies show a leukocyte count of 21,000/mm3 and an increased serum beta-D-glucan concentration. An x-ray of the chest shows symmetrical, diffuse interstitial infiltrates. Which of the following is most likely to confirm the diagnosis?
- A. Tuberculin skin test
- B. Urine antigen test
- C. CT scan of the chest
- D. Bronchoalveolar lavage (Correct Answer)
- E. DNA test for CFTR mutation
Blastomyces dermatitidis Explanation: ***Bronchoalveolar lavage***
- The patient, an infant on **prednisolone** (immunosuppression) with **diffuse interstitial infiltrates**, **uncomfortable appearance**, **respiratory distress**, and **oral thrush (white plaque that bleeds when scraped)**, points to **Pneumocystis pneumonia (PCP)**.
- **Bronchoalveolar lavage (BAL)** is the gold standard for diagnosing PCP by identifying **Pneumocystis jirovecii cysts** or **trophozoites** using special stains (e.g., Giemsa, methenamine silver).
*Tuberculin skin test*
- The **tuberculin skin test** is used to diagnose **tuberculosis**, which typically presents with **granulomas** and **cavitary lesions** on chest X-ray, not diffuse interstitial infiltrates.
- While tuberculosis can cause respiratory symptoms, the presence of oral thrush and immunosuppression suggests an opportunistic fungal infection like PCP rather than TB.
*Urine antigen test*
- A **urine antigen test** is commonly used for diagnosing **Legionnaires' disease** or **pneumococcal pneumonia** in adults, and is not applicable for PCP.
- It does not detect *Pneumocystis jirovecii*, which is the suspected pathogen in this immunosuppressed infant.
*CT scan of the chest*
- A **CT scan of the chest** would show **diffuse ground-glass opacities** characteristic of PCP but is a **radiological finding**, not a definitive diagnostic test for the pathogen itself.
- While it can further characterize the pulmonary findings, it cannot identify the causative organism, which is crucial for targeted treatment.
*DNA test for CFTR mutation*
- A **DNA test for CFTR mutation** is used to diagnose **cystic fibrosis**, a genetic disorder affecting mucus production, and is not relevant in this acute presentation of respiratory distress and immunosuppression.
- Cystic fibrosis typically presents with recurrent respiratory infections, pancreatic insufficiency, and failure to thrive, not primarily with opportunistic infections like PCP.
Blastomyces dermatitidis US Medical PG Question 9: A 45-year-old HIV-positive patient (CD4 count 180 cells/µL) from San Joaquin Valley presents with erythema nodosum, arthralgias, and bilateral hilar adenopathy. Coccidioides serology shows IgM positive, IgG negative. He is asymptomatic except for joint pain and skin lesions. He is on antiretroviral therapy with undetectable viral load. Evaluate the clinical presentation and synthesize the appropriate management decision considering immune status and disease manifestations.
- A. Immediate amphotericin B therapy for 6 weeks
- B. Fluconazole 400 mg daily for 12 months as he has HIV
- C. Observation with serial serologies, treat only if progressive disease develops (Correct Answer)
- D. Oral itraconazole for 3-6 months
- E. Increase antiretroviral therapy intensity and observe
Blastomyces dermatitidis Explanation: ***Observation with serial serologies, treat only if progressive disease develops***
- The presence of **erythema nodosum** and **arthralgias** (Valley Fever) indicates a vigorous **host immune response**, which is often associated with a self-limited clinical course and a good prognosis.
- In HIV patients with CD4 counts >150-250 cells/µL on stable **ART** with a suppressed viral load, primary pulmonary coccidioidomycosis can often be managed with observation rather than immediate **antifungal therapy**.
*Immediate amphotericin B therapy for 6 weeks*
- This aggressive intravenous treatment is reserved for **disseminated** or life-threatening **meningeal coccidioidomycosis**, not for uncomplicated primary infection.
- The patient's localized findings and **immunologic markers** (erythema nodosum) do not justify the toxicity of amphotericin B.
*Fluconazole 400 mg daily for 12 months as he has HIV*
- HIV status alone does not mandate long-term treatment if the patient is **immunologically stable** (CD4 >150) and asymptomatic/mildly symptomatic.
- Chronic suppressive therapy is typically reserved for those with **CD4 counts <150** or those who have completed treatment for disseminated disease.
*Oral itraconazole for 3-6 months*
- **Itraconazole** is an alternative to fluconazole for symptomatic pulmonary disease, but the patient's current symptoms are **immunologic reactions** rather than persistent fungal pneumonia.
- Treatment is not required for primary infection in a patient who is currently stable and showing signs of an effective **immune response**.
*Increase antiretroviral therapy intensity and observe*
- The patient already has an **undetectable viral load**, indicating that his current **ART regimen** is fully effective.
- Increasing the intensity of ART would not target the fungal infection and could lead to unnecessary **drug-drug interactions** and side effects.
Blastomyces dermatitidis US Medical PG Question 10: A 58-year-old man with acute myeloid leukemia presents with breakthrough fungal infection while on fluconazole prophylaxis. Blood cultures grow yeast that forms germ tubes. Chest CT shows new pulmonary nodules. He has neutropenia (ANC 200/µL) and is 2 weeks post-chemotherapy. His serum creatinine is 2.8 mg/dL. Evaluate and synthesize the optimal therapeutic strategy considering drug resistance, organ dysfunction, and underlying malignancy.
- A. Increase fluconazole dose to 800 mg daily
- B. Switch to liposomal amphotericin B with close renal monitoring
- C. Voriconazole with therapeutic drug monitoring and hold chemotherapy
- D. Echinocandin therapy (micafungin) with continuation of oncologic treatment plan (Correct Answer)
- E. Combination therapy with amphotericin B plus flucytosine
Blastomyces dermatitidis Explanation: ***Echinocandin therapy (micafungin) with continuation of oncologic treatment plan***
- **Echinocandins** are the preferred first-line treatment for invasive candidiasis in **neutropenic patients** and have an excellent safety profile with **no dosage adjustment** required for renal impairment.
- This strategy effectively targets **Candida albicans** (suggested by germ tube positivity) while minimizing **drug-drug interactions** with chemotherapy and avoiding further nephrotoxicity.
*Increase fluconazole dose to 800 mg daily*
- Increasing the dose is inappropriate for a **breakthrough infection**, as it suggests the fungal strain has developed **resistance** or reduced susceptibility to the current triazole therapy.
- Fluconazole is primarily **fungistatic** and may not provide the rapid biocidal action needed in a **critically ill, neutropenic** patient.
*Switch to liposomal amphotericin B with close renal monitoring*
- While effective against most fungi, **liposomal amphotericin B** carries a high risk of worsening the patient's existing **renal dysfunction** (creatinine 2.8 mg/dL).
- It is generally reserved as a second-line option when **echinocandins** are unavailable or contraindicated due to its significant **nephrotoxic potential**.
*Voriconazole with therapeutic drug monitoring and hold chemotherapy*
- **Voriconazole** is the treatment of choice for invasive aspergillosis, but for **Candida** bloodstream infections, echinocandins are superior in the setting of **neutropenia**.
- Azoles like voriconazole have extensive **CYP450 interactions** with chemotherapy agents and require **renal adjustment** of the intravenous vehicle (SBECD), making it less ideal here.
*Combination therapy with amphotericin B plus flucytosine*
- This combination is the gold standard for **cryptococcal meningitis**, but it is not indicated for initial therapy of **invasive candidiasis**.
- Both drugs are highly **nephrotoxic**, and flucytosine can cause significant **bone marrow suppression**, which would worsen the patient's existing **neutropenia**.
More Blastomyces dermatitidis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.