Prevention of biofilm formation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Prevention of biofilm formation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Prevention of biofilm formation US Medical PG Question 1: The surgical equipment used during a craniectomy is sterilized using pressurized steam at 121°C for 15 minutes. Reuse of these instruments can cause transmission of which of the following pathogens?
- A. Non-enveloped viruses
- B. Sporulating bacteria
- C. Prions (Correct Answer)
- D. Enveloped viruses
- E. Yeasts
Prevention of biofilm formation Explanation: ***Prions***
- Prions are **abnormally folded proteins** that are highly resistant to standard sterilization methods like steam autoclaving at 121°C, making them a risk for transmission through reused surgical instruments.
- They cause transmissible spongiform encephalopathies (TSEs) like **Creutzfeldt-Jakob disease**, where even trace amounts can be highly infectious.
*Non-enveloped viruses*
- Non-enveloped viruses are generally **more resistant to heat and disinfectants** than enveloped viruses but are typically inactivated by recommended steam sterilization protocols.
- Standard autoclaving conditions are effective in destroying most non-enveloped viruses.
*Sporulating bacteria*
- **Bacterial spores**, such as those from *Clostridium* or *Bacillus*, are known for their high resistance to heat and chemicals, but are usually **inactivated by steam sterilization at 121°C** for 15 minutes.
- This method is specifically designed to kill bacterial spores effectively.
*Enveloped viruses*
- Enveloped viruses are the **least resistant to heat and chemical disinfectants** due to their lipid envelope.
- They are readily **inactivated by standard steam sterilization** at 121°C.
*Yeasts*
- **Yeasts** are eukaryotic microorganisms that are typically **susceptible to heat sterilization**.
- They are effectively killed by typical steam autoclaving conditions used for surgical instruments.
Prevention of biofilm formation US Medical PG Question 2: An 8-year-old girl is brought to the emergency room for a 6-hour history of fever, sore throat, and difficulty swallowing. Physical examination shows pooling of oral secretions and inspiratory stridor. Lateral x-ray of the neck shows thickening of the epiglottis and aryepiglottic folds. Throat culture with chocolate agar shows small, gram-negative coccobacilli. The patient's brother is started on the recommended antibiotic for chemoprophylaxis. Which of the following is the primary mechanism of action of this drug?
- A. Inhibition of the 50S ribosomal subunit
- B. Inhibition of prokaryotic topoisomerase II
- C. Inhibition of DNA-dependent RNA-polymerase (Correct Answer)
- D. Inhibition of the 30S ribosomal subunit
- E. Inhibition of peptidoglycan crosslinking
Prevention of biofilm formation Explanation: ***Inhibition of DNA-dependent RNA-polymerase***
- The clinical picture strongly suggests **epiglottitis** caused by *Haemophilus influenzae type b* (Hib), characterized by **fever, sore throat, difficulty swallowing, pooling of oral secretions, inspiratory stridor**, and **epiglottic thickening** on X-ray.
- **Rifampin** is the recommended antibiotic for chemoprophylaxis in close contacts of Hib patients; its primary mechanism of action is to inhibit bacterial **DNA-dependent RNA polymerase**, thereby preventing **mRNA synthesis**.
*Inhibition of the 50S ribosomal subunit*
- This mechanism is characteristic of **macrolides** (e.g., azithromycin, erythromycin) and **clindamycin**, which are not the primary choice for Hib chemoprophylaxis.
- These drugs prevent **protein synthesis** by interfering with translocation or peptide bond formation on the larger ribosomal subunit.
*Inhibition of prokaryotic topoisomerase II*
- This is the mechanism of action for **fluoroquinolones** (e.g., ciprofloxacin), which are typically reserved for specific infections due to potential side effects in children.
- Fluoroquinolones interfere with **DNA replication** and **transcription** by preventing DNA unwinding and supercoiling.
*Inhibition of the 30S ribosomal subunit*
- This mechanism is associated with **tetracyclines** and **aminoglycosides** (e.g., doxycycline, gentamicin).
- These antibiotics block **protein synthesis** by preventing tRNA attachment or causing misreading of mRNA.
*Inhibition of peptidoglycan crosslinking*
- This describes the mechanism of **beta-lactam antibiotics** (e.g., penicillin, amoxicillin, cephalosporins), which inhibit bacterial **cell wall synthesis**.
- While some beta-lactams are used to treat Hib infections, they are not the primary drug for **chemoprophylaxis**.
Prevention of biofilm formation US Medical PG Question 3: A stool sample was taken from a 19-year-old male who presented with profuse watery diarrhea. He recently returned from a trip to Central America. A microbiologist identified the causative agent as a gram-negative, oxidase-positive, comma-shaped bacteria that is able to grow well in a pH > 8. Which of the following is a mechanism of action of the toxin produced by this bacteria?
- A. Overactivation of adenylate cyclase by inhibition of Gi subunit by ADP-ribosylation
- B. Inactivation of the 60S ribosomal subunit by cleaving an adenine from the 28S rRNA
- C. Overactivation of guanylate cyclase
- D. Overactivation of adenylate cyclase by activation of Gs subunit by ADP-ribosylation (Correct Answer)
- E. Degradation of cell membranes by hydrolysis of the phospholipids
Prevention of biofilm formation Explanation: ***Overactivation of adenylate cyclase by activation of Gs subunit by ADP-ribosylation***
- The description of the bacterium as **gram-negative, oxidase-positive, comma-shaped, growing well in pH > 8**, and causing **profuse watery diarrhea** after travel to Central America points to *Vibrio cholerae*.
- **Cholera toxin** (CTX) produced by *V. cholerae* is an A-B toxin that **ADP-ribosylates the Gs α-subunit**, permanently activating **adenylate cyclase**. This leads to increased cAMP levels, causing secretion of water and electrolytes into the intestinal lumen.
*Overactivation of adenylate cyclase by inhibition of Gi subunit by ADP-ribosylation*
- This mechanism describes the action of **pertussis toxin** from *Bordetella pertussis*, which ADP-ribosylates and **inhibits the Gi subunit**, preventing adenylate cyclase inhibition.
- While both ultimately increase cAMP, the specific target and mechanism (inhibition of Gi vs. activation of Gs) differ from cholera toxin.
*Inactivation of the 60S ribosomal subunit by cleaving an adenine from the 28S rRNA*
- This mechanism is characteristic of **Shiga toxin** produced by *Shigella dysenteriae* and Shiga-like toxins (verotoxins) produced by **enterohemorrhagic *E. coli*** (EHEC).
- These toxins inhibit protein synthesis, leading to cell death and often bloody diarrhea and hemolytic uremic syndrome, which is not described here.
*Overactivation of guanylate cyclase*
- **Heat-stable enterotoxins (ST)** produced by **enterotoxigenic *E. coli*** (ETEC) activate **guanylate cyclase**, leading to increased cGMP and subsequent fluid secretion.
- While ETEC can cause watery diarrhea, the bacterial characteristics provided (oxidase-positive, comma-shaped) do not fit *E. coli*.
*Degradation of cell membranes by hydrolysis of the phospholipids*
- This mechanism is associated with toxins like **phospholipases** or **lecithinases** (e.g., alpha-toxin of *Clostridium perfringens*).
- These toxins cause direct cell lysis and tissue damage, which is not the primary mechanism of action for the watery diarrhea seen in cholera.
Prevention of biofilm formation US Medical PG Question 4: Three days after admission to the hospital following a motor vehicle accident, a 45-year-old woman develops a fever. A central venous catheter was placed on the day of admission for treatment of severe hypotension. Her temperature is 39.2°C (102.5°F). Examination shows erythema surrounding the catheter insertion site at the right internal jugular vein. Blood cultures show gram-positive, catalase-positive cocci that have a high minimum inhibitory concentration when exposed to novobiocin. Which of the following is the most appropriate pharmacotherapy?
- A. Clarithromycin
- B. Vancomycin (Correct Answer)
- C. Metronidazole
- D. Penicillin G
- E. Polymyxin B
Prevention of biofilm formation Explanation: ***Vancomycin***
- The description of **gram-positive, catalase-positive cocci** that are **novobiocin-resistant** (high MIC) strongly points to **Staphylococcus epidermidis** or other coagulase-negative staphylococci. *S. epidermidis* is the most common cause of **catheter-related bloodstream infections** and is often **methicillin-resistant**, making **vancomycin** the drug of choice.
- The presence of erythema at the catheter site and fever in a patient with a central venous catheter indicates a **central line-associated bloodstream infection (CLABSI)**, for which empiric coverage with vancomycin is standard until sensitivities are known.
- The novobiocin resistance test helps differentiate *S. epidermidis* (resistant) from *S. saprophyticus* (sensitive).
*Clarithromycin*
- **Clarithromycin** is a macrolide antibiotic primarily used for respiratory tract infections and *Mycobacterium avium complex*.
- It is **not effective** against methicillin-resistant staphylococci and would not be appropriate for a suspected CLABSI.
*Metronidazole*
- **Metronidazole** is an antibiotic mainly used for **anaerobic bacterial infections** and certain parasitic infections.
- It has **no activity** against gram-positive cocci like staphylococci.
*Penicillin G*
- **Penicillin G** is a narrow-spectrum penicillin effective against some gram-positive cocci, like **Streptococcus pyogenes**.
- However, virtually all staphylococci, especially those causing hospital-acquired infections, are **resistant to penicillin G** due to beta-lactamase (penicillinase) production.
*Polymyxin B*
- **Polymyxin B** is an antibiotic primarily effective against **gram-negative bacteria**, particularly those with multi-drug resistance such as **Pseudomonas aeruginosa** and **Acinetobacter baumannii**.
- It has **no significant activity** against gram-positive cocci like staphylococci.
Prevention of biofilm formation US Medical PG Question 5: A group of microbiological investigators is studying bacterial DNA replication in E. coli colonies. While the cells are actively proliferating, the investigators stop the bacterial cell cycle during S phase and isolate an enzyme involved in DNA replication. An assay of the enzyme's exonuclease activity determines that it is active on both intact and demethylated thymine nucleotides. Which of the following enzymes have the investigators most likely isolated?
- A. DNA ligase
- B. Telomerase
- C. Primase
- D. DNA topoisomerase
- E. DNA polymerase I (Correct Answer)
Prevention of biofilm formation Explanation: ***DNA polymerase I***
- **DNA polymerase I** possesses **5' to 3' exonuclease activity**, which is crucial for removing **RNA primers** (intact nucleotides) laid down by primase during DNA replication.
- This 5' to 3' exonuclease activity also allows it to excise damaged DNA, including DNA containing **demethylated thymine nucleotides**.
- It also has 3' to 5' exonuclease activity for proofreading.
- **Key distinction:** While DNA polymerase III (the main replicative enzyme) only has 3' to 5' exonuclease activity, DNA polymerase I has **both** 3' to 5' and 5' to 3' exonuclease activities, making it essential for primer removal and DNA repair.
*DNA ligase*
- **DNA ligase** functions to form a **phosphodiester bond** between adjacent nucleotides to seal nicks in the DNA backbone, but it does not have exonuclease activity.
- Its primary role is in joining Okazaki fragments and repairing single-strand breaks.
*Telomerase*
- **Telomerase** is a specialized reverse transcriptase that extends the telomeres at the ends of eukaryotic chromosomes, but is not present in prokaryotes like *E. coli*.
- It uses an RNA template to synthesize DNA, and it lacks exonuclease activity.
*Primase*
- **Primase** is an RNA polymerase that synthesizes short **RNA primers** on the DNA template, providing a starting point for DNA synthesis.
- It is involved in synthesizing primers, not in removing or excising nucleotides, and has no exonuclease activity.
*DNA topoisomerase*
- **DNA topoisomerases** relieve supercoiling in DNA during replication and transcription by cutting and rejoining DNA strands.
- While they act on DNA, their function is to manage topological stress, and they do not exhibit exonuclease activity on nucleotides.
Prevention of biofilm formation US Medical PG Question 6: A 67-year-old man is brought to the emergency department because of severe dyspnea and orthopnea for 6 hours. He has a history of congestive heart disease and an ejection fraction of 40%. The medical history is otherwise unremarkable. He appears confused. At the hospital, his blood pressure is 165/110 mm Hg, the pulse is 135/min, the respirations are 48/min, and the temperature is 36.2°C (97.2°F). Crackles are heard at both lung bases. There is pitting edema from the midtibia to the ankle bilaterally. The patient is intubated and admitted to the critical care unit for mechanical ventilation and treatment. Intravenous morphine, diuretics, and nitroglycerine are initiated. Which of the following is the most effective method to prevent nosocomial infection in this patient?
- A. Nasogastric tube insertion
- B. Suprapubic catheter insertion
- C. Daily oropharynx decontamination with antiseptic agent (Correct Answer)
- D. Daily urinary catheter irrigation with antimicrobial agent
- E. Condom catheter placement
Prevention of biofilm formation Explanation: ***Daily oropharynx decontamination with antiseptic agent***
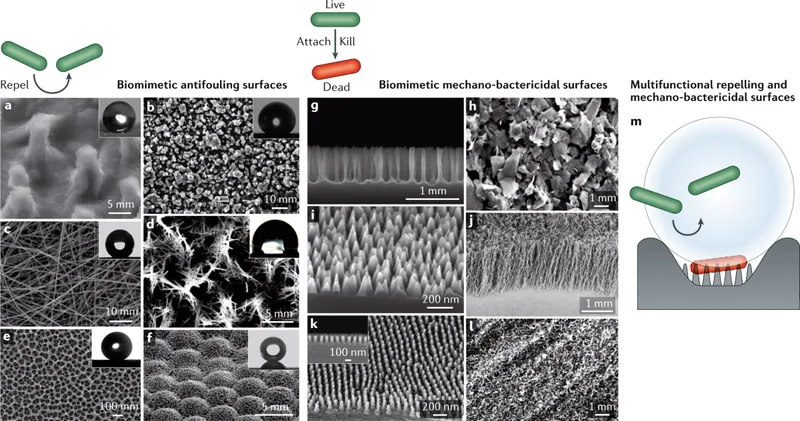
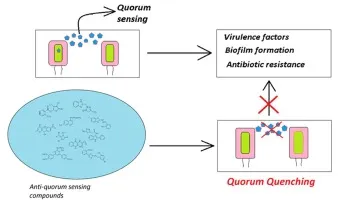
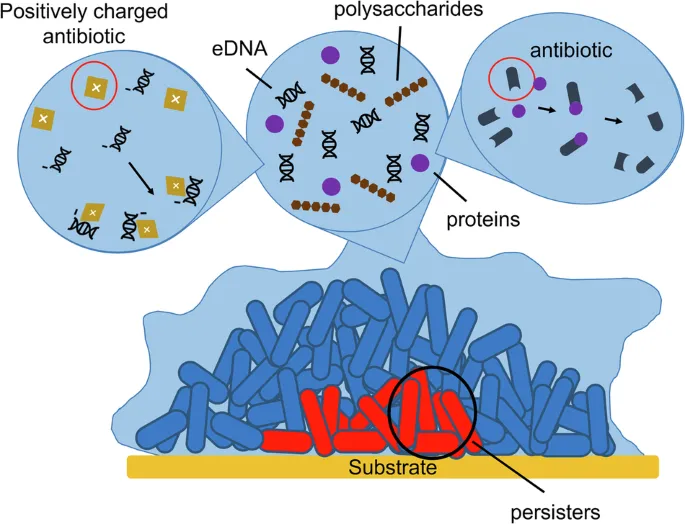
- **Oropharyngeal decontamination** helps reduce the bacterial load in the oral cavity, which is crucial for preventing **ventilator-associated pneumonia (VAP)** in intubated patients.
- Regular cleaning with an antiseptic agent disrupts the formation of **biofilms** and the aspiration of pathogenic bacteria into the lower respiratory tract.
*Nasogastric tube insertion*
- While a nasogastric tube can be important for nutrition and medication delivery, it does not directly prevent **nosocomial infections** and can even be a source of infection if not properly managed.
- It does not address the primary risk of pneumonia or other infections related to intubation and critical illness.
*Suprapubic catheter insertion*
- A suprapubic catheter is used for drainage of the bladder, but it is an invasive procedure with its own risks of **urinary tract infections (UTIs)** and is not indicated for preventing nosocomial infections in this patient's primary presentation.
- It is not a standard method to prevent the most common nosocomial infections in an intubated patient in the ICU.
*Daily urinary catheter irrigation with antimicrobial agent*
- Irrigating a urinary catheter daily with an antimicrobial agent is **not recommended** as a routine practice to prevent **catheter-associated urinary tract infections (CAUTIs)**.
- Such irrigation can disrupt the natural flora and potentially lead to **antimicrobial resistance** or further infection by promoting the growth of resistant organisms.
*Condom catheter placement*
- A condom catheter is a non-invasive external device used for urinary incontinence in males, but it's generally **less effective** than indwelling catheters for critical care patients requiring precise fluid output monitoring.
- It does not address the risk of **VAP**, which is a major concern for intubated patients, and may not be feasible or adequate for all bedridden patients in the ICU.
Prevention of biofilm formation US Medical PG Question 7: An investigator is studying a strain of bacteria that retains a blue color after crystal violet dye and acetone are applied. The bacteria are inoculated in a petri dish containing hypotonic saline. After the addition of an antibiotic, the bacteria swell and rupture. This antibiotic most likely belongs to which of the following classes?
- A. Macrolide
- B. Cephalosporin (Correct Answer)
- C. Sulfonamide
- D. Fluoroquinolone
- E. Tetracycline
Prevention of biofilm formation Explanation: ***Cephalosporin***
- This scenario describes a **Gram-positive bacterium** (retains blue color) which, after antibiotic treatment, swells and lyses in a hypotonic solution. This indicates a defect in the **peptidoglycan cell wall**.
- **Cephalosporins** are **β-lactam antibiotics** that inhibit bacterial cell wall synthesis by interfering with **peptidoglycan cross-linking**, leading to osmotic lysis in hypotonic environments.
*Macrolide*
- Macrolides like **azithromycin** and **erythromycin** inhibit bacterial **protein synthesis** by binding to the 50S ribosomal subunit.
- They do not directly target the cell wall, so they would not cause immediate osmotic lysis in this manner.
*Sulfonamide*
- Sulfonamides inhibit bacterial **folic acid synthesis** by acting as a competitive inhibitor of dihydropteroate synthase, disrupting DNA and RNA production.
- Their mechanism of action does not involve direct cell wall disruption or osmotic lysis.
*Fluoroquinolone*
- Fluoroquinolones interfere with bacterial **DNA replication and transcription** by inhibiting **DNA gyrase** and **topoisomerase IV**.
- This class of antibiotics does not primarily target the cell wall, and therefore would not lead to prompt osmotic swelling and rupture.
*Tetracycline*
- Tetracyclines inhibit bacterial **protein synthesis** by binding to the 30S ribosomal subunit, preventing the attachment of aminoacyl-tRNA.
- They do not affect the cell wall, so they would not cause the observed osmotic lysis.
Prevention of biofilm formation US Medical PG Question 8: A 20-year-old woman presents for a follow-up visit with her physician. She has a history of cystic fibrosis and is currently under treatment. She has recently been struggling with recurrent bouts of cough and foul-smelling, mucopurulent sputum over the past year. Each episode lasts for about a week or so and then subsides. She does not have a fever or chills during these episodes. She has been hospitalized several times for pneumonia as a child and continues to struggle with diarrhea. Physically she appears to be underweight and in distress. Auscultation reveals reduced breath sounds on the lower lung fields with prominent rhonchi. Which of the following infectious agents is most likely associated with the recurrent symptoms this patient is experiencing?
- A. Mycobacterium avium
- B. Pseudomonas (Correct Answer)
- C. Histoplasma
- D. Pneumococcus
- E. Listeria
Prevention of biofilm formation Explanation: ***Pseudomonas***
- **Pseudomonas aeruginosa** is a common and opportunistic pathogen in patients with **cystic fibrosis** due to altered mucus secretion and impaired mucociliary clearance.
- Recurrent cough, foul-smelling, and **mucopurulent sputum** are classic symptoms of **Pseudomonas** lung infections in CF patients, often leading to chronic colonization and bronchiectasis.
*Mycobacterium avium*
- While *Mycobacterium avium complex* (MAC) can infect patients with cystic fibrosis, it typically causes a **more indolent and chronic lung disease** rather than recurrent, self-limiting bouts of cough and sputum.
- MAC infections are often associated with **nodular or cavitary lesions** on imaging and may require prolonged multidrug therapy.
*Histoplasmosis*
- **Histoplasmosis** is a fungal infection endemic to certain geographic regions (e.g., Ohio and Mississippi River valleys) and is acquired by inhaling spores.
- It's **not a typical or recurrent pathogen** in cystic fibrosis patients in the way bacterial infections are, and its presentation often includes fever, chills, and disseminated disease in immunocompromised individuals.
*Pneumococcus*
- *Streptococcus pneumoniae* (**Pneumococcus**) is a common cause of **acute bacterial pneumonia** in the general population, including young children.
- While CF patients can get pneumococcal infections, the pattern of **recurrent bouts of foul-smelling mucopurulent sputum** without fever and the chronic nature of the lung disease point away from typical acute pneumococcal infection and more towards a chronic colonizer like *Pseudomonas*.
*Listeria*
- *Listeria monocytogenes* is primarily a cause of **foodborne illness**, leading to gastroenteritis, meningitis, or sepsis, particularly in immunocompromised individuals, pregnant women, and neonates.
- It is **not a common respiratory pathogen**, and its presentation does not align with the described recurrent pulmonary symptoms in a cystic fibrosis patient.
Prevention of biofilm formation US Medical PG Question 9: A 7-year-old boy with a history of cystic fibrosis is brought to the physician for evaluation of recurrent episodes of productive cough, wheezing, and shortness of breath over the past month. Physical examination shows coarse crackles and expiratory wheezing over both lung fields. Serum studies show elevated levels of IgE and eosinophilia. A CT scan of the lungs shows centrally dilated bronchi with thickened walls and peripheral airspace consolidation. Antibiotic therapy is initiated. One week later, the patient continues to show deterioration in lung function. A sputum culture is most likely to grow which of the following?
- A. Monomorphic, septate hyphae that branch at acute angles (Correct Answer)
- B. Monomorphic, broad, nonseptate hyphae that branch at wide angles
- C. Dimorphic, broad-based budding yeast
- D. Dimorphic, cigar-shaped budding yeast
- E. Monomorphic, narrow budding encapsulated yeast
Prevention of biofilm formation Explanation: **Monomorphic, septate hyphae that branch at acute angles**
- The patient's presentation with **cystic fibrosis (CF)**, recurrent respiratory symptoms, CT findings of **central bronchiectasis**, elevated **IgE**, and **eosinophilia** strongly points towards **allergic bronchopulmonary aspergillosis (ABPA)**.
- *Aspergillus fumigatus*, the causative agent of ABPA, is characterized microscopically by **monomorphic, septate hyphae that branch at acute angles**.
*Monomorphic, broad, nonseptate hyphae that branch at wide angles*
- This describes organisms like *Rhizopus* or *Mucor*, which cause **mucormycosis**.
- Mucormycosis typically affects immunocompromised individuals (e.g., diabetics, neutropenic patients) and presents as aggressive rhinocerebral or pulmonary infections, not ABPA.
*Dimorphic, broad-based budding yeast*
- This morphology is characteristic of *Blastomyces dermatitidis*, which causes **blastomycosis**.
- Blastomycosis is an endemic fungal infection often presenting with pulmonary symptoms, but it does not cause central bronchiectasis, elevated IgE, or eosinophilia in the context of CF.
*Dimorphic, cigar-shaped budding yeast*
- This morphology describes *Sporothrix schenckii*, which causes **sporotrichosis**.
- Sporotrichosis typically presents as a chronic ulcerative skin disease (rose gardener's disease) or, less commonly, pulmonary disease, but is not associated with ABPA.
*Monomorphic, narrow budding encapsulated yeast*
- This morphology is characteristic of *Cryptococcus neoformans*, which causes **cryptococcosis**.
- Cryptococcosis commonly affects immunocompromised individuals, causing meningoencephalitis or pulmonary disease, but its presentation is distinct from ABPA, lacking the allergic and bronchiectatic features described.
Prevention of biofilm formation US Medical PG Question 10: A 47-year-old man presents to the emergency department with jaundice and extreme fatigue for the past 4 days. He also noticed that his stool is very pale and urine is dark. Past medical history is unremarkable. The review of systems is significant for a 23 kg (50 lb) weight loss over the last 3 months which he says is due to decreased appetite. He is afebrile and the vital signs are within normal limits. A contrast computed tomography (CT) scan of the abdomen reveals a mass in the pancreatic head. A blood test for carbohydrate antigen (CA19-9) is positive. The patient is admitted to the intensive care unit (ICU) and undergoes surgical decompression of the biliary tract. He is placed on total parenteral nutrition (TPN). On day 4 after admission, his intravenous access site is found to be erythematous and edematous. Which of the following microorganisms is most likely responsible for this patient’s intravenous (IV) site infection?
- A. Candida parapsilosis (Correct Answer)
- B. E. coli
- C. Hepatitis B virus
- D. Pseudomonas aeruginosa
- E. Malassezia furfur
Prevention of biofilm formation Explanation: ***Candida parapsilosis***
- This yeast is a common cause of **catheter-related bloodstream infections** in patients receiving **total parenteral nutrition (TPN)**, as it can readily grow on lipid emulsions.
- The patient's presentation with an erythematous and edematous intravenous access site, coupled with a history of TPN, strongly points towards a fungal infection, with *C. parapsilosis* being a primary suspect due to its affinity for TPN.
*E. coli*
- While *E. coli* is a common cause of **urinary tract infections** and can cause **bloodstream infections**, it is not a typical cause of IV site infections specifically associated with TPN.
- Its presence at an IV site would usually indicate a more generalized sepsis or contamination, rather than the specific affinity *C. parapsilosis* has for TPN lines.
*Hepatitis B virus*
- **Hepatitis B virus** causes **viral hepatitis** and liver damage, but it does not directly cause localized IV site infections with erythema and edema.
- It is typically spread through blood and body fluids and its clinical manifestations are systemic, primarily involving the liver, rather than local skin signs at an IV access site.
*Pseudomonas aeruginosa*
- **Pseudomonas aeruginosa** is a common opportunistic pathogen, particularly in **immunocompromised patients** and those with medical devices, but it is typically associated with infections in burn wounds, cystic fibrosis, or ventilator-associated pneumonia.
- While it can cause catheter-related infections, it is not as uniquely linked to TPN-associated IV site infections as *Candida parapsilosis*.
*Malassezia furfur*
- *Malassezia furfur* is known to cause **catheter-related infections** in patients receiving **lipid emulsions** via central lines, similar to *C. parapsilosis*.
- However, *C. parapsilosis* is statistically a more common cause of TPN-associated fungemia and IV site infections than *M. furfur*.
More Prevention of biofilm formation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.