Biofilms in otitis media and sinusitis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Biofilms in otitis media and sinusitis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Biofilms in otitis media and sinusitis US Medical PG Question 1: An 8-year-old boy with asthma is brought to the physician because of a 2-week history of facial pain and congestion. His mother states that the nasal discharge was initially clear, but it has become thicker and more purulent over the last week. He has tried multiple over-the-counter oral decongestants and antihistamines, with minimal relief. Current medications include cetirizine, intranasal oxymetazoline, and albuterol. His temperature is 37.7°C (99.8°F), pulse is 100/min, respirations are 14/min, and blood pressure is 110/70 mm Hg. Examination shows congested nasal mucosa with purulent discharge from the nares bilaterally. There is tenderness to palpation over the cheeks, with no transillumination over the maxillary sinuses. Which of the following is the most likely predisposing factor for this patient's current condition?
- A. Nasal polyps
- B. Viral upper respiratory tract infection (Correct Answer)
- C. Recent use of antihistamines
- D. Foreign body
- E. Asthma
Biofilms in otitis media and sinusitis Explanation: ***Viral upper respiratory tract infection***
- **Acute bacterial rhinosinusitis** often develops as a complication of a **viral upper respiratory tract infection (URI)**, which causes inflammation and edema of the nasal mucosa, obstructing sinus drainage.
- The initial clear nasal discharge followed by purulent discharge and persistent symptoms for over 10 days (or worsening after 5-7 days) is highly suggestive of a progression from viral rhinitis to a bacterial infection.
*Nasal polyps*
- While nasal polyps can contribute to chronic sinusitis, they are less likely to be the initial predisposing factor for an acute bacterial infection in a child unless associated with conditions like **cystic fibrosis**.
- Polyps typically cause **nasal obstruction** and **anosmia**, but the scenario here points to an acute infectious process.
*Recent use of antihistamines*
- **Antihistamines** like cetirizine can dry out nasal secretions, but they are not a direct predisposing factor for developing bacterial sinusitis.
- Their effect on thickening mucus is not the primary cause of bacterial overgrowth in the sinuses.
*Foreign body*
- A **nasal foreign body** primarily causes unilateral symptoms, including foul-smelling unilateral nasal discharge.
- This patient presents with bilateral symptoms, making a foreign body less likely.
*Asthma*
- While asthma and allergic rhinitis are related conditions that can affect the respiratory tract, **asthma itself does not directly predispose** to acute bacterial rhinosinusitis.
- However, uncontrolled allergic inflammation could indirectly make a patient more susceptible to viral infections, which then could progress to sinusitis.
Biofilms in otitis media and sinusitis US Medical PG Question 2: An investigator is studying the growth of an organism in different media. The organism is inoculated on a petri dish that contains heated sheep blood, vancomycin, nystatin, trimethoprim, and colistin. The resulting growth medium is incubated at 37°C. Numerous small, white colonies are seen after incubation for 48 hours. This organism is most likely to cause which of the following conditions?
- A. Pontiac fever
- B. Pseudomembranous colitis
- C. Hemolytic uremic syndrome
- D. Oral thrush
- E. Gonorrhea (Correct Answer)
Biofilms in otitis media and sinusitis Explanation: ***Gonorrhea***
- The growth medium described is **Thayer-Martin agar**, a selective medium containing **heated sheep blood** (supplies NAD+), **vancomycin** (inhibits Gram-positives), **colistin** (inhibits Gram-negatives), **nystatin** (inhibits fungi), and **trimethoprim** (inhibits Proteus). This medium is specifically designed for the isolation of *Neisseria gonorrhoeae* from polymicrobial samples.
- *Neisseria gonorrhoeae* typically grows as **small, translucent-to-white colonies** on selective media like Thayer-Martin agar, and incubation at 37°C in CO2 (not explicitly mentioned but often required) for 24-48 hours yields visible growth, causing **gonorrhea**.
*Pontiac fever*
- Pontiac fever is a mild, self-limiting form of **legionellosis**, caused by *Legionella pneumophila*.
- *Legionella* requires a specialized medium such as **buffered charcoal yeast extract (BCYE) agar** for growth, not Thayer-Martin agar.
*Pseudomembranous colitis*
- This condition is caused by **toxin-producing *Clostridioides difficile***, often after antibiotic use.
- *C. difficile* is an obligate anaerobe and requires **anaerobic conditions** and specific selective media (e.g., CCFA agar) for isolation, not Thayer-Martin agar under aerobic conditions.
*Hemolytic uremic syndrome*
- Hemolytic uremic syndrome (HUS) is often caused by **Shiga toxin-producing *Escherichia coli* (STEC)**, particularly O157:H7.
- STEC can be isolated on media like **sorbitol MacConkey agar (SMAC)**, where O157:H7 appears as non-sorbitol fermenting colonies, distinct from the growth seen on Thayer-Martin.
*Oral thrush*
- Oral thrush is caused by *Candida albicans*, a yeast.
- *Candida* would be inhibited by **nystatin** in the Thayer-Martin medium, which is an antifungal agent.
Biofilms in otitis media and sinusitis US Medical PG Question 3: An 8-year-old female presents to her pediatrician with nasal congestion. Her mother reports that the patient has had nasal congestion and nighttime cough for almost two weeks. The patient’s 3-year-old brother had similar symptoms that began around the same time and have since resolved. The patient initially seemed to be improving, but four days ago she began developing worsening nasal discharge and fever to 102.6°F (39.2°C) at home. Her mother denies any change in appetite. The patient denies sore throat, ear pain, and headache. She is otherwise healthy. In the office, her temperature is 102.2°F (39.0°C), blood pressure is 96/71 mmHg, pulse is 128/min, and respirations are 18/min. On physical exam, the nasal turbinates are edematous and erythematous. She has a dry cough. Purulent mucous can be visualized dripping from the posterior nasopharynx. Her maxillary sinuses are tender to palpation.
Which of the following organisms is most likely to be causing this patient’s current condition?
- A. Moraxella catarrhalis (Correct Answer)
- B. Streptococcus pyogenes
- C. Adenovirus
- D. Streptococcus pneumoniae
- E. Haemophilus influenzae
Biofilms in otitis media and sinusitis Explanation: ***Moraxella catarrhalis***
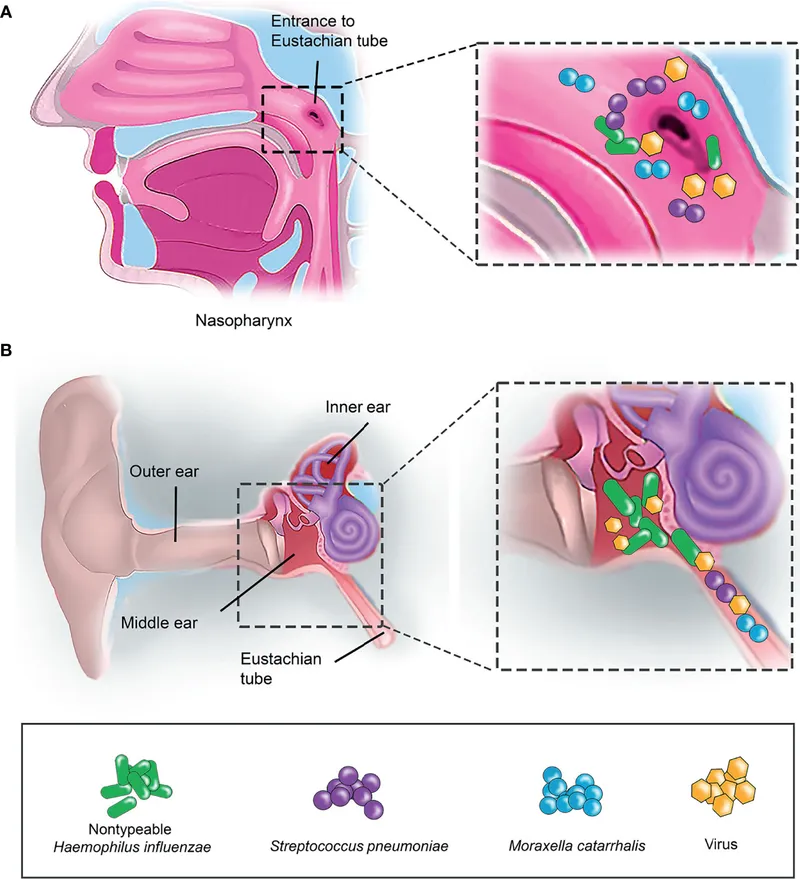
- This patient presents with **acute bacterial rhinosinusitis (ABRS)**, characterized by worsening nasal congestion, purulent discharge, high fever, and maxillary sinus tenderness after initial improvement from a viral illness (the classic **"double sickening"** pattern).
- The three most common bacterial causes of ABRS in children are *Streptococcus pneumoniae* (most common, 30-40%), *Haemophilus influenzae* (20-30%), and ***Moraxella catarrhalis*** (10-20%).
- **Given the options provided, *Moraxella catarrhalis* is the correct answer** as it is a well-established cause of pediatric ABRS, particularly in children under 10 years of age, and is the only common ABRS pathogen listed among the choices.
*Pseudomonas aeruginosa*
- *Pseudomonas aeruginosa* is associated with **nosocomial infections**, **chronic sinusitis in cystic fibrosis patients**, immunocompromised states, or malignant otitis externa.
- It is not a typical cause of acute community-acquired bacterial rhinosinusitis in healthy, immunocompetent children.
*Streptococcus pyogenes*
- *Streptococcus pyogenes* (Group A Streptococcus) primarily causes **pharyngitis** with sore throat, tonsillar exudates, and cervical lymphadenopathy—none of which are present in this patient.
- **Note:** This should not be confused with ***Streptococcus pneumoniae***, which is actually the **most common cause** of bacterial rhinosinusitis in children but is not listed as an option in this question.
- *S. pyogenes* is not a recognized common cause of acute bacterial rhinosinusitis.
*Adenovirus*
- Adenovirus is a common viral cause of **upper respiratory tract infections** and likely caused this patient's initial illness.
- The **biphasic course** with worsening symptoms after day 10, persistent high fever (>102°F), and purulent discharge indicate **bacterial superinfection**, not ongoing viral illness.
- Viral URIs typically improve within 7-10 days without this pattern of clinical deterioration.
*Staphylococcus aureus*
- While *Staphylococcus aureus* can cause sinusitis, it is **not a common cause** of acute community-acquired bacterial rhinosinusitis in otherwise healthy children.
- *S. aureus* sinusitis is more commonly associated with **chronic sinusitis**, **nosocomial infections**, **post-surgical infections**, or complications such as orbital or intracranial extension.
Biofilms in otitis media and sinusitis US Medical PG Question 4: A 43-year-old type 1 diabetic woman who is poorly compliant with her diabetes medications presented to the emergency department with hemorrhage from her nose. On exam, you observe the findings shown in figure A. What is the most likely explanation for these findings?
- A. Cryptococcal infection
- B. Sporotrichosis
- C. Gram negative bacterial infection
- D. Candida infection
- E. Rhizopus infection (Correct Answer)
Biofilms in otitis media and sinusitis Explanation: ***Rhizopus infection***
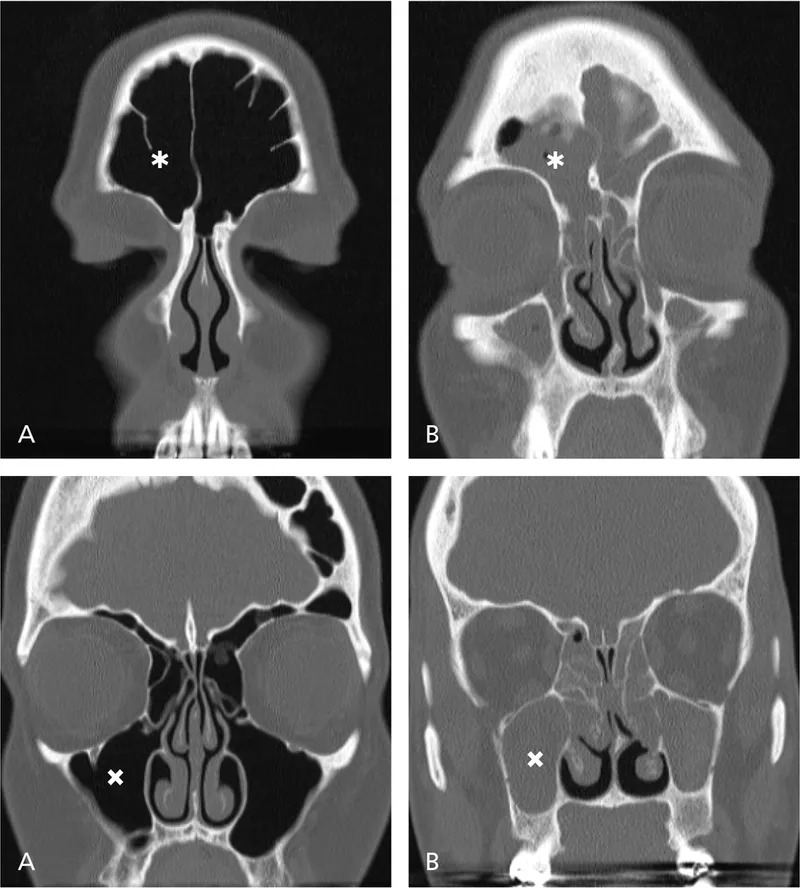
- The image likely depicts findings consistent with **mucormycosis**, an aggressive fungal infection caused by organisms like *Rhizopus*, characterized by **black necrotic eschars** and rapid tissue destruction.
- **Type 1 diabetes mellitus** with poor compliance (leading to **diabetic ketoacidosis**) is a major risk factor for mucormycosis due to impaired immune function and acidic environment.
*Cryptococcal infection*
- Primarily causes **meningitis** or **pulmonary disease**, especially in immunocompromised individuals, and less commonly presents as rhinocerebral mucormycosis-like lesions.
- Skin lesions can occur but are usually **papules**, **nodules**, or **ulcers**, not typically widespread necrotizing eschars of the nasal region.
*Sporothricosis*
- Typically presents as **subcutaneous nodules** that slowly enlarge and may ulcerate, often following trauma with contaminated plant material.
- It does not usually cause the rapid, aggressive, and necrotizing sinonasal infection seen in the context of uncontrolled diabetes.
*Gram negative bacterial infection*
- While gram-negative bacteria can cause severe infections, they typically present with **purulent discharge**, **cellulitis**, or **abscess formation**, rather than the characteristic black necrotic eschar of mucormycosis.
- Although immunosuppression increases risk, the specific clinical findings point away from a primary gram-negative bacterial infection.
*Candida infection*
- Commonly causes **oral thrush**, **esophagitis**, or **vaginitis**, or disseminated candidiasis in severely immunocompromised patients.
- While it can cause invasive sinusitis, it rarely produces the aggressive **necrotic eschar** seen in mucormycosis, and is generally less common in this specific presentation.
Biofilms in otitis media and sinusitis US Medical PG Question 5: A 24-year-old man presents with low-grade fever and shortness of breath for the last 3 weeks. Past medical history is significant for severe mitral regurgitation status post mitral valve replacement five years ago. His temperature is 38.3°C (101.0°F) and respiratory rate is 18/min. Physical examination reveals vertical hemorrhages under his nails, multiple painless erythematous lesions on his palms, and two tender, raised nodules on his fingers. Cardiac auscultation reveals a new-onset 2/6 holosystolic murmur loudest at the apex with the patient in the left lateral decubitus position. A transesophageal echocardiogram reveals vegetations on the prosthetic valve. Blood cultures reveal catalase-positive, gram-positive cocci. Which of the following characteristics is associated with the organism most likely responsible for this patient’s condition?
- A. Coagulase positive
- B. DNAse positive
- C. Hemolysis
- D. Novobiocin sensitive (Correct Answer)
- E. Optochin sensitive
Biofilms in otitis media and sinusitis Explanation: ***Novobiocin sensitive***
- The patient has **prosthetic valve endocarditis** caused by a **catalase-positive, gram-positive coccus**, which is most likely **_Staphylococcus epidermidis_** due to its association with foreign bodies and prosthetic devices.
- _Staphylococcus epidermidis_ is a **coagulase-negative staphylococcus** that is **novobiocin sensitive**, helping to differentiate it from other coagulase-negative staphylococci like **_Staphylococcus saprophyticus_** (novobiocin resistant).
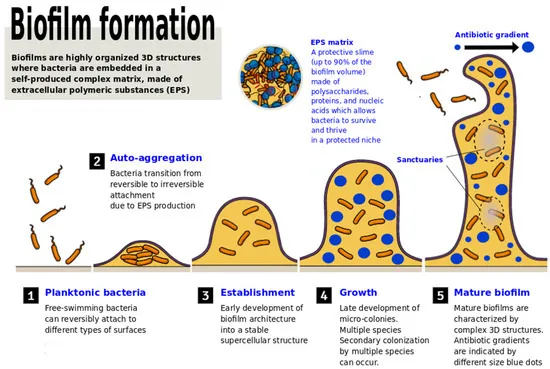
- Although this is late prosthetic valve endocarditis (5 years post-surgery), _S. epidermidis_ remains a common pathogen due to biofilm formation on prosthetic materials.
*Coagulase positive*
- **Coagulase-positive** gram-positive cocci, such as **_Staphylococcus aureus_**, are a common cause of endocarditis, especially in intravenous drug users and can also cause prosthetic valve endocarditis.
- However, the correct answer requires identifying the characteristic that differentiates the most likely organism, and **coagulase-negative** staphylococci like _S. epidermidis_ are more characteristically associated with prosthetic device infections due to their biofilm-forming capabilities.
- A positive coagulase test differentiates _S. aureus_ from coagulase-negative staphylococci.
*DNAse positive*
- **DNAse positivity** is characteristic of **_Staphylococcus aureus_** and group A beta-hemolytic streptococci (_Streptococcus pyogenes_).
- While _S. aureus_ can cause prosthetic valve endocarditis, the question asks for the characteristic most associated with the likely organism, which in the context of prosthetic devices is typically **_S. epidermidis_** (DNAse negative).
*Hemolysis*
- **Hemolysis patterns** are primarily used to differentiate **streptococcal species**, not staphylococci. For example, **beta-hemolytic streptococci** cause complete hemolysis.
- While some staphylococci can show hemolytic activity, it is not a primary characteristic used to differentiate between the most likely staphylococcal causes of prosthetic valve endocarditis.
*Optochin sensitive*
- **Optochin sensitivity** is a key characteristic used to identify **_Streptococcus pneumoniae_**.
- _S. pneumoniae_ is **catalase-negative**, while the described organism is **catalase-positive**, ruling out _S. pneumoniae_ as the causative agent.
Biofilms in otitis media and sinusitis US Medical PG Question 6: A 65-year-old woman undergoes an abdominal hysterectomy. She develops pain and discharge at the incision site on the fourth postoperative day. The past medical history is significant for diabetes of 12 years duration, which is well-controlled on insulin. Pus from the incision site is sent for culture on MacConkey agar, which shows white-colorless colonies. On blood agar, the colonies were green. Biochemical tests reveal an oxidase-positive organism. Which of the following is the most likely pathogen?
- A. Staphylococcus aureus
- B. Enterococcus faecalis
- C. Streptococcus pyogenes
- D. Pseudomonas aeruginosa (Correct Answer)
- E. Staphylococcus epidermidis
Biofilms in otitis media and sinusitis Explanation: ***Pseudomonas aeruginosa***
- The combination of **white, colorless colonies on MacConkey agar** (indicating a non-lactose fermenter), **green colonies on blood agar** (due to pigment production), and a **positive oxidase test** is highly characteristic of *Pseudomonas aeruginosa*.
- This organism is a common cause of **nosocomial infections**, particularly in immunocompromised patients (like those with diabetes) and in postoperative wound infections.
*Staphylococcus aureus*
- This bacterium would typically produce **golden-yellow colonies** on blood agar and **no growth on MacConkey agar**.
- It is **oxidase-negative** and a common cause of surgical site infections, but its colonial morphology and biochemical tests do not match the description.
*Enterococcus faecalis*
- This organism is a **Gram-positive coccus** that would not grow well on MacConkey agar and would not produce green colonies on blood agar or be oxidase-positive.
- It is a common cause of urinary tract and wound infections, especially in hospitalized patients.
*Streptococcus pyogenes*
- This is a **beta-hemolytic Streptococcus** that typically produces small, clear colonies with a zone of complete hemolysis on blood agar and would not grow on MacConkey agar.
- It is also **oxidase-negative**, making it inconsistent with the findings.
*Staphylococcus epidermidis*
- This organism forms **white colonies** on blood agar and would not grow on MacConkey agar or produce green pigment.
- It is **coagulase-negative** and **oxidase-negative**, and while it can cause surgical site infections, its colonial characteristics differ.
Biofilms in otitis media and sinusitis US Medical PG Question 7: Blood cultures are sent to the laboratory. Intravenous antibiotic therapy is started. Transesophageal echocardiography shows a large, oscillating vegetation attached to the tricuspid valve. There are multiple small vegetations attached to tips of the tricuspid valve leaflets. There is moderate tricuspid regurgitation. The left side of the heart and the ejection fraction are normal. Which of the following is the most likely causal organism of this patient's condition?
- A. Streptococcus sanguinis
- B. Staphylococcus aureus (Correct Answer)
- C. Enterococcus faecalis
- D. Neisseria gonorrhoeae
- E. Staphylococcus epidermidis
Biofilms in otitis media and sinusitis Explanation: ***Staphylococcus aureus***
- **_Staphylococcus aureus_** is the most common cause of **acute infective endocarditis**, particularly in intravenous drug users, which often affects the **tricuspid valve**.
- The presence of large, oscillating vegetations and **multiple small vegetations** on the tricuspid valve strongly suggests an aggressive infection, typical of _S. aureus_.
*Streptococcus sanguinis*
- _Streptococcus sanguinis_ is a common cause of **subacute infective endocarditis** in patients with pre-existing valvular disease but rarely causes acute, aggressive right-sided endocarditis.
- It's typically associated with **dental procedures** and usually affects the left side of the heart.
*Enterococcus faecalis*
- _Enterococcus faecalis_ can cause endocarditis, often associated with **genitourinary or gastrointestinal procedures**, and typically affects older men.
- While it can cause virulent endocarditis, it is less commonly associated with acute right-sided disease in this demographic compared to _S. aureus_.
*Neisseria gonorrhoeae*
- **_Neisseria gonorrhoeae_** is a rare cause of endocarditis, usually seen in younger, sexually active individuals, and often involves the aortic valve.
- While it can be acute, it is an extremely uncommon cause of **tricuspid valve endocarditis**.
*Staphylococcus epidermidis*
- **_Staphylococcus epidermidis_** is primarily associated with **prosthetic valve endocarditis** or foreign bodies, often presenting as a subacute infection.
- It rarely causes natural valve endocarditis, especially acute right-sided disease in this context.
Biofilms in otitis media and sinusitis US Medical PG Question 8: A 9-year-old boy is brought to the pediatrician by his parents with a fever, cough, and cold symptoms that began 7 days ago. He has been complaining of right ear pain for the last 2 days. He is otherwise a completely healthy child with no known medical conditions. On physical examination, the temperature is 39.0°C (102.2°F), the pulse is 114 /min, the blood pressure is 106/74 mm Hg, and the respiratory rate is 26/min. On chest auscultation, rales are heard over the right subscapular region accompanied by bronchial breathing in the same region. Examination of the right external auditory canal reveals an erythematous, bulging tympanic membrane. The results of a complete blood count are as follows:
Hemoglobin % 11 g/dL
WBC count 12,000/mm3
Neutrophils 88%
Lymphocytes 10%
Monocytes 2%
Platelet count 200,000/mm3
A chest radiograph shows a focal homogenous opacity in the right lung suggestive of consolidation. Bacteriologic cultures of the blood, nasopharynx, and sputum grew Moraxella catarrhalis. Which of the following is the antibiotic of choice?
- A. Azithromycin
- B. Amoxicillin-clavulanate (Correct Answer)
- C. Amoxicillin
- D. Cefuroxime
- E. Erythromycin
Biofilms in otitis media and sinusitis Explanation: ***Correct Option: Amoxicillin-clavulanate***
- The patient has **community-acquired pneumonia** and **acute otitis media** caused by *Moraxella catarrhalis*, confirmed by cultures.
- **>90% of *Moraxella catarrhalis* isolates produce beta-lactamase**, making them **resistant to amoxicillin alone**.
- **Amoxicillin-clavulanate** is the **first-line treatment** as clavulanate inhibits beta-lactamase, restoring activity against this organism.
- This combination provides **appropriate coverage** for both the pneumonia and otitis media in this pediatric patient.
*Incorrect Option: Amoxicillin*
- While amoxicillin is first-line for many respiratory infections, it is **ineffective against beta-lactamase-producing *M. catarrhalis***.
- Using amoxicillin alone would likely result in **treatment failure** given the high prevalence of beta-lactamase production in this organism.
- The presence of **documented *M. catarrhalis*** on culture makes beta-lactamase coverage essential.
*Incorrect Option: Azithromycin*
- This **macrolide antibiotic** is effective against *M. catarrhalis* and could be used as an alternative.
- However, it is **not first-line** when *M. catarrhalis* is documented, especially in a patient with concurrent pneumonia and otitis media where broader coverage is preferred.
- **Increasing macrolide resistance** in respiratory pathogens makes beta-lactam combinations more reliable for documented bacterial infections.
*Incorrect Option: Cefuroxime*
- This **second-generation cephalosporin** is **beta-lactamase stable** and effective against *M. catarrhalis*.
- While it would be an acceptable alternative, **amoxicillin-clavulanate is preferred** as first-line therapy for community-acquired respiratory infections in children per IDSA guidelines.
- Cefuroxime is typically reserved for **penicillin allergy** or **treatment failure** with first-line agents.
*Incorrect Option: Erythromycin*
- This older **macrolide antibiotic** has activity against *M. catarrhalis* but is **less preferred** than newer macrolides or beta-lactam combinations.
- It has **more gastrointestinal side effects** than azithromycin and **increasing resistance** among respiratory pathogens.
- Not considered first-line therapy for documented *M. catarrhalis* infections in current practice.
Biofilms in otitis media and sinusitis US Medical PG Question 9: An 81-year-old man comes to the emergency department with severe left ear pain and drainage for 3 days. He has a history of poorly-controlled type 2 diabetes mellitus. He appears uncomfortable. Physical examination of the ear shows marked periauricular erythema, exquisite tenderness on palpation, and granulation tissue in the external auditory canal. The most likely causal pathogen produces an exotoxin that acts by a mechanism most similar to a toxin produced by which of the following organisms?
- A. Corynebacterium diphtheriae (Correct Answer)
- B. Bacillus anthracis
- C. Staphylococcus aureus
- D. Bordetella pertussis
- E. Shigella dysenteriae
Biofilms in otitis media and sinusitis Explanation: ***Corynebacterium diphtheriae***
- The clinical picture describes **malignant otitis externa** (MOE), likely caused by *Pseudomonas aeruginosa*, particularly in an elderly diabetic patient. Both *Pseudomonas aeruginosa* exotoxin A and *Corynebacterium diphtheriae* diphtheria toxin **inhibit protein synthesis by ADP-ribosylation of elongation factor-2 (EF-2)**.
- This shared mechanism of action makes *Corynebacterium diphtheriae* the most appropriate comparative organism based on the question's premise of exotoxin mechanism.
*Bacillus anthracis*
- Produces **anthrax toxin**, which consists of Protective Antigen (PA), Edema Factor (EF), and Lethal Factor (LF). LF is a **zinc-dependent metalloprotease** that cleaves mitogen-activated protein kinase kinase (MAPKK) family proteins.
- This mechanism is distinct from the ADP-ribosylation of EF-2.
*Staphylococcus aureus*
- Produces several toxins, including **toxic shock syndrome toxin-1 (TSST-1)** and **exfoliatin**, which act as **superantigens** or **proteases** respectively.
- These mechanisms differ from the ADP-ribosylation of EF-2.
*Bordetella pertussis*
- Produces **pertussis toxin**, which **ADP-ribosylates Gi proteins**, leading to increased cAMP levels by disinhibiting adenylate cyclase.
- This is a different target and mechanism compared to the ADP-ribosylation of EF-2.
*Shigella dysenteriae*
- Produces **Shiga toxin**, which is an **N-glycosidase** that cleaves the adenine residue from the 28S rRNA of the 60S ribosomal subunit, thereby **inhibiting protein synthesis**.
- While it inhibits protein synthesis, the specific mechanism is different from ADP-ribosylation of EF-2.
Biofilms in otitis media and sinusitis US Medical PG Question 10: An 11-month-old boy is brought to the physician for the evaluation of recurrent otitis media since birth. The patient’s immunizations are up-to-date. He is at the 5th percentile for height and weight. Physical examination shows multiple petechiae and several eczematous lesions over the scalp and extremities. The remainder of the examination reveals no abnormalities. Laboratory studies show a leukocyte count of 9,600/mm3 (61% neutrophils and 24% lymphocytes), a platelet count of 29,000/mm3, and an increased serum IgE concentration. Which of the following is the most likely diagnosis?
- A. Chédiak-Higashi syndrome
- B. Chronic granulomatous disease
- C. Wiskott-Aldrich syndrome (Correct Answer)
- D. Severe combined immunodeficiency
- E. Hyper-IgE syndrome
Biofilms in otitis media and sinusitis Explanation: ***Wiskott-Aldrich syndrome***
- This syndrome is characterized by the classic triad of **thrombocytopenia** (platelet count 29,000/mm³), **eczema** (eczematous lesions), and **recurrent infections** (recurrent otitis media since birth).
- Patients also typically present with **petechiae** due to low platelet counts and **small platelet size**, which is a key diagnostic feature, along with elevated IgE levels.
*Chédiak-Higashi syndrome*
- This syndrome presents with **recurrent pyogenic infections**, **oculocutaneous albinism**, and **neurological abnormalities**, which are not described in this patient.
- While it features immune dysfunction, the specific triad of thrombocytopenia, eczema, and otitis media with elevated IgE is not characteristic.
*Chronic granulomatous disease*
- This condition is characterized by the inability of phagocytes to produce a **respiratory burst**, leading to recurrent infections with **catalase-positive organisms** and **granuloma formation**.
- It does not typically present with the severe thrombocytopenia or eczema seen in this patient.
*Severe combined immunodeficiency*
- SCID is characterized by profound defects in **T-cell and B-cell function**, leading to severe, life-threatening infections and **failure to thrive**.
- While recurrent infections are present, the specific features of thrombocytopenia, eczema, and elevated IgE levels are not typical presentations of SCID.
*Hyper-IgE syndrome*
- Also known as Job's syndrome, it is characterized by extremely high serum **IgE levels**, **eczema**, and recurrent **staphylococcal skin abscesses** and **pneumonia**.
- While eczema and elevated IgE are present, thrombocytopenia and petechiae are not characteristic features of Hyper-IgE syndrome.
More Biofilms in otitis media and sinusitis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.