Biofilms in endocarditis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Biofilms in endocarditis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Biofilms in endocarditis US Medical PG Question 1: A 34-year-old man comes to the physician because of fatigue and shortness of breath with moderate exertion for the past 2 months. Over the past 10 days, he has had low-grade fevers and night sweats. He has no history of serious illness except for a bicuspid aortic valve diagnosed 5 years ago. He has smoked one pack of cigarettes daily for 10 years and drinks 3–5 beers on social occasions. He does not use illicit drugs. The patient takes no medications. He appears weak. His temperature is 37.7°C (99.9°F), pulse is 70/min, and blood pressure is 128/64 mm Hg. The lungs are clear to auscultation. A grade 2/6 systolic murmur is heard best at the right sternal border and second intercostal space. There are several hemorrhages underneath his fingernails on both hands and multiple tender, red nodules on his fingers. Which of the following is the most likely causal organism?
- A. Candida albicans
- B. Streptococcus sanguinis (Correct Answer)
- C. Streptococcus pneumoniae
- D. Staphylococcus epidermidis
Biofilms in endocarditis Explanation: ***Streptococcus sanguinis***
- The patient's history of **bicuspid aortic valve** represents a predisposing cardiac lesion for **infective endocarditis**.
- **S. sanguinis** is part of the **viridans group streptococci**, common inhabitants of the oral flora, and is a frequent cause of subacute bacterial endocarditis, especially in individuals with damaged heart valves.
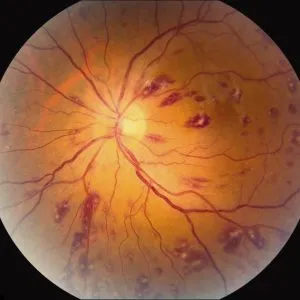
- The clinical presentation of **splinter hemorrhages** and **Osler nodes** (tender nodules on fingers) along with low-grade fever and constitutional symptoms is classic for subacute bacterial endocarditis.
*Candida albicans*
- While *Candida* can cause endocarditis, it is typically seen in specific risk groups such as **intravenous drug users**, immunocompromised patients, or after prosthetic valve surgery, none of which apply here.
- Fungal endocarditis often presents with larger **vegetations** and a more subacute course, but bacterial causes (especially viridans streptococci) are far more common in this clinical setting.
*Streptococcus pneumoniae*
- *S. pneumoniae* (pneumococcus) is a known cause of **pneumonia**, **meningitis**, and **otitis media**, but it is an uncommon cause of endocarditis.
- Pneumococcal endocarditis, when it occurs, typically presents with a more fulminant course and may be associated with other sites of pneumococcal infection.
*Staphylococcus epidermidis*
- *S. epidermidis* is a common cause of **prosthetic valve endocarditis** and infections related to foreign bodies or catheters.
- Given the patient's **native valve** issue and absence of prosthetic material or recent invasive procedures, it is less likely than **viridans streptococci**.
Biofilms in endocarditis US Medical PG Question 2: A 37-year-old man with a history of IV drug use presents to the ED with complaints of fevers, chills, and malaise for one week. He admits to recently using IV and intramuscular heroin. Vital signs are as follows: T 40.0 C, HR 120 bpm, BP 110/68 mmHg, RR 14, O2Sat 98%. Examination reveals a new systolic murmur that is loudest at the lower left sternal border. Initial management includes administration of which of the following regimens?
- A. IV Vancomycin, IV ceftriaxone, IV fluconazole
- B. IV Vancomycin, IV ceftriaxone (Correct Answer)
- C. IV Vancomycin, IV levofloxacin
- D. IV Vancomycin
- E. IV Vancomycin, IV gentamicin, PO rifampin
Biofilms in endocarditis Explanation: ***IV Vancomycin, IV ceftriaxone***
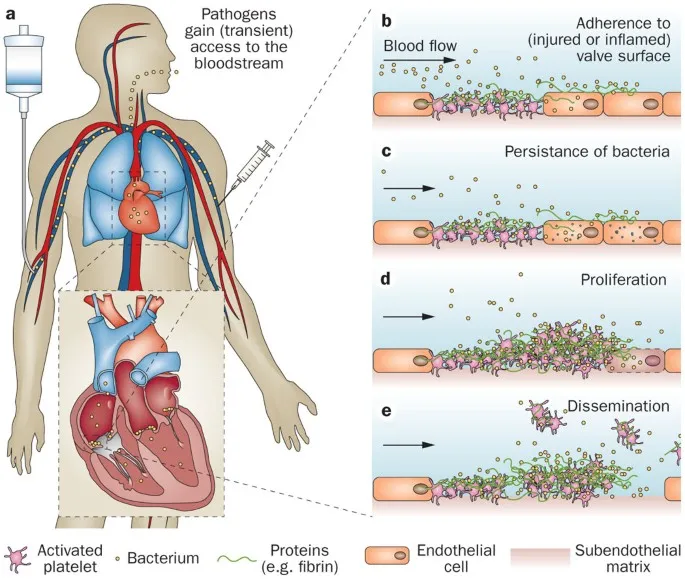
- The patient's history of **IV drug use**, fevers, chills, new systolic murmur, and likely **tricuspid valve involvement** (murmur loudest at the lower left sternal border) strongly suggest **infective endocarditis**.
- The empiric regimen for suspected endocarditis in an IV drug user should cover **methicillin-resistant _Staphylococcus aureus_ (MRSA)** with **vancomycin** and gram-negative organisms with a **third-generation cephalosporin** like **ceftriaxone**.
- This combination provides broad coverage for the most common pathogens in native valve endocarditis among IV drug users, including MRSA, streptococci, and many gram-negative organisms.
*IV Vancomycin, IV ceftriaxone, IV fluconazole*
- While vancomycin and ceftriaxone are appropriate, **fluconazole** is an antifungal and is generally not indicated for empiric treatment of bacterial endocarditis unless there's a strong suspicion of **fungal infection**.
- Fungal endocarditis is less common and usually requires prolonged treatment with specific antifungals, often alongside surgical intervention.
*IV Vancomycin, IV levofloxacin*
- **Levofloxacin** is a fluoroquinolone that covers a broad spectrum of bacteria but is not the preferred empiric agent for gram-negative coverage in suspected endocarditis in IV drug users due to concerns about resistance and lack of superior coverage compared to third-generation cephalosporins.
- **Ceftriaxone** provides better coverage for common gram-negative pathogens associated with endocarditis among IV drug users in this context.
*IV Vancomycin, IV gentamicin, PO rifampin*
- **Gentamicin** is an aminoglycoside that provides effective gram-negative coverage and is often used in combination therapy for endocarditis, but **rifampin** is typically reserved for prosthetic valve endocarditis or refractory cases due to its risk of drug interactions and resistance development.
- **Oral rifampin** may not be appropriate for initial aggressive treatment in an acutely ill patient with suspected acute endocarditis, where IV therapy is preferred.
*IV Vancomycin*
- While **vancomycin** is crucial for covering **MRSA** which is common in IV drug users, it alone does not provide adequate coverage for potential **gram-negative pathogens** that can also cause endocarditis in this population.
- **Multidrug empiric therapy** is essential to cover a broad range of likely pathogens causing endocarditis in IV drug users, especially with severe symptoms.
Biofilms in endocarditis US Medical PG Question 3: Part of the success of the Streptococcus pyogenes bacterium lies in its ability to evade phagocytosis. Which of the following helps in this evasion?
- A. Streptolysin S
- B. Streptolysin O
- C. Streptokinase
- D. M protein (Correct Answer)
- E. Pyrogenic toxin
Biofilms in endocarditis Explanation: ***M protein***
- The **M protein** is a major virulence factor of *Streptococcus pyogenes* that **inhibits phagocytosis** by binding to factor H, a host complement regulatory protein, preventing C3b deposition.
- It also helps the bacterium adhere to host cells and resist killing by neutrophils.
*Streptolysin S*
- **Streptolysin S** is a **hemolysin** that causes beta-hemolysis on blood agar and contributes to tissue damage by lysing cells.
- While contributing to virulence, its primary role is not direct inhibition of phagocytosis but rather cell lysis.
*Streptolysin O*
- **Streptolysin O (SLO)** is another **hemolysin** that produces pore-forming toxins, leading to cell lysis and tissue destruction.
- It is highly antigenic and often used as a diagnostic marker (ASO titer) for past *S. pyogenes* infections, but it does not directly prevent phagocytosis.
*Streptokinase*
- **Streptokinase** is an enzyme that activates plasminogen, leading to the breakdown of fibrin clots, which helps in the **spread of infection** within tissues.
- Its main function is not to evade phagocytosis but rather to facilitate invasion by dissolving blood clots that would typically wall off the infection.
*Pyrogenic toxin*
- **Pyrogenic toxins** (also known as erythrogenic toxins) are superantigens that cause symptoms like fever and rash (e.g., in scarlet fever) by stimulating a massive, non-specific T-cell activation.
- These toxins contribute to the systemic manifestations of infection but do not directly interfere with the process of phagocytosis.
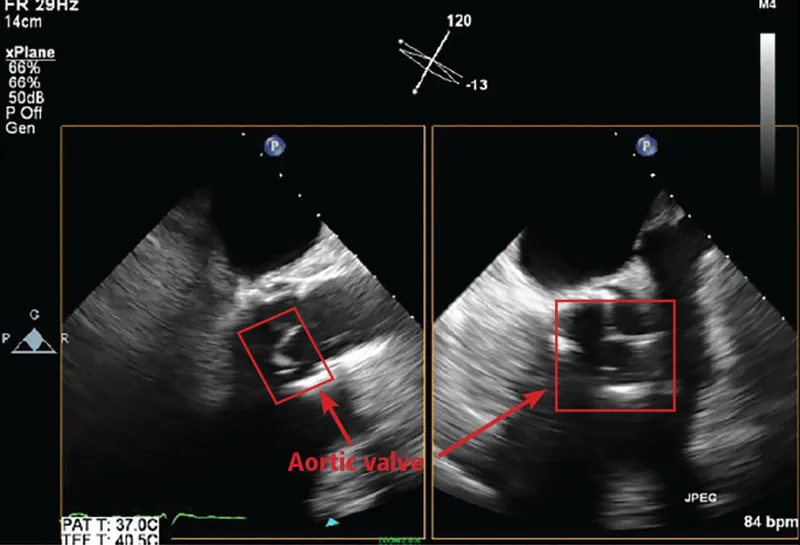
Biofilms in endocarditis US Medical PG Question 4: A 45-year-old man comes to the physician because of a 1-month history of fever and poor appetite. Five weeks ago, he underwent molar extraction for dental caries. His temperature is 38°C (100.4°F). Cardiac examination shows a grade 2/6 holosystolic murmur heard best at the apex. A blood culture shows gram-positive, catalase-negative cocci. Transesophageal echocardiography shows a small vegetation on the mitral valve with mild regurgitation. The causal organism most likely has which of the following characteristics?
- A. Production of dextrans (Correct Answer)
- B. Production of CAMP factor
- C. Conversion of fibrinogen to fibrin
- D. Formation of germ tubes at body temperature
- E. Replication in host macrophages
Biofilms in endocarditis Explanation: **Production of dextrans**
- The clinical picture of **fever**, **poor appetite**, a **holosystolic murmur**, and **mitral valve vegetation** following a dental procedure (molar extraction) strongly points to **infective endocarditis** caused by **Viridans streptococci**.
- **Viridans streptococci**, commonly found in the oral cavity, produce **dextrans**, which allow them to adhere to damaged heart valves and fibrin-platelet aggregates, initiating vegetation formation.
*Production of CAMP factor*
- **CAMP factor** is a characteristic of **Group B Streptococcus (Streptococcus agalactiae)**, which primarily causes infections in neonates and immunocompromised adults, not typically infective endocarditis post-dental procedure.
- *Streptococcus agalactiae* is also catalase-negative and gram-positive but is rarely associated with endocarditis arising from oral flora.
*Conversion of fibrinogen to fibrin*
- The ability to convert **fibrinogen to fibrin** is characteristic of **coagulase-positive organisms**, such as *Staphylococcus aureus*, which is a catalase-positive organism.
- The blood culture in this case specifically states **catalase-negative cocci**, ruling out *Staphylococcus aureus* as the causative agent.
*Formation of germ tubes at body temperature*
- **Germ tube formation** at body temperature is a distinguishing characteristic of *Candida albicans*, a **fungus**, not a gram-positive, catalase-negative coccus.
- While *Candida* can cause endocarditis, the microbiological findings described do not align with a fungal infection.
*Replication in host macrophages*
- **Intracellular replication in host macrophages** is characteristic of certain bacteria like *Mycobacterium tuberculosis*, *Listeria monocytogenes*, or *Salmonella typhi*, which typically cause systemic infections
- This characteristic is not associated with the gram-positive, catalase-negative cocci responsible for subacute bacterial endocarditis following dental procedures.
Biofilms in endocarditis US Medical PG Question 5: A 47-year-old woman comes to the physician because of a 6-week history of fatigue and low-grade fever. She has no history of serious illness except for a bicuspid aortic valve, diagnosed 10 years ago. She does not use illicit drugs. Her temperature is 37.7°C (99.9°F). Physical examination shows petechiae under the fingernails and multiple tender, red nodules on the fingers. A new grade 2/6 diastolic murmur is heard at the right second intercostal space. Which of the following is the most likely causal organism?
- A. Staphylococcus epidermidis
- B. Streptococcus pyogenes
- C. Streptococcus sanguinis (Correct Answer)
- D. Streptococcus pneumoniae
- E. Enterococcus faecalis
Biofilms in endocarditis Explanation: ***Streptococcus sanguinis***
- The patient's presentation with **fatigue, low-grade fever, petechiae, tender nodules (Osler nodes)**, and a **new diastolic murmur** in a patient with a **bicuspid aortic valve** is highly suggestive of **infective endocarditis**.
- **Streptococcus sanguinis** (and other viridans streptococci) are common causes of subacute bacterial endocarditis, often associated with **oral flora** and pre-existing valvular heart disease.
*Staphylococcus epidermidis*
- This organism is a common cause of **prosthetic valve endocarditis** and **nosocomial infections** but is less likely to cause endocarditis in a native valve without a history of recent surgery or intravenous lines.
- While it can cause endocarditis, the clinical features here, especially the lack of recent medical interventions, point away from *S. epidermidis* as the primary cause.
*Streptococcus pyogenes*
- **Streptococcus pyogenes** is primarily known for causing **strep throat, scarlet fever, and rheumatic fever**, which can lead to rheumatic heart disease but rarely causes acute or subacute infective endocarditis directly.
- It typically causes more acute and severe infections, which doesn't align with the 6-week history of low-grade fever and fatigue.
*Streptococcus pneumoniae*
- **Streptococcus pneumoniae** is a common cause of **pneumonia, meningitis, and otitis media** but is an uncommon cause of infective endocarditis, accounting for a very small percentage of cases.
- Endocarditis due to *S. pneumoniae* tends to be **acute and fulminant**, often associated with severe systemic illness, which is not fully consistent with the subacute presentation here.
*Enterococcus faecalis*
- **Enterococcus faecalis** is a common cause of **nosocomial urinary tract infections** and can cause endocarditis, especially in older patients or those with gastrointestinal or genitourinary procedures.
- While it's a possibility for endocarditis, the oral flora association with viridans streptococci (like *S. sanguinis*) in the context of a bicuspid aortic valve makes it a more direct fit.
Biofilms in endocarditis US Medical PG Question 6: A 63-year-old female recovering from a total shoulder arthroplasty completed 6 days ago presents complaining of joint pain in her repaired shoulder. Temperature is 39 degrees Celsius. Physical examination demonstrates erythema and significant tenderness around the incision site. Wound cultures reveal Gram-positive cocci that are resistant to nafcillin. Which of the following organisms is the most likely cause of this patient's condition?
- A. Streptococcus pyogenes
- B. Escherichia coli
- C. Streptococcus viridans
- D. Staphylococcus epidermidis
- E. Staphylococcus aureus (Correct Answer)
Biofilms in endocarditis Explanation: ***Staphylococcus aureus***
- The combination of **post-surgical infection**, **erythema**, and fever with **Gram-positive cocci** that are **nafcillin-resistant** is highly indicative of **Methicillin-Resistant Staphylococcus aureus (MRSA)**.
- *S. aureus* is a common cause of **surgical site infections**, and its resistance to nafcillin implies it is MRSA, a significant clinical concern for its difficulty in treatment.
*Streptococcus pyogenes*
- While *S. pyogenes* is a Gram-positive coccus that can cause skin and soft tissue infections, it is typically **susceptible to penicillin** and related antibiotics like nafcillin, unlike the organism described.
- It is more commonly associated with **streptococcal pharyngitis** or **cellulitis**, and while it can cause severe disease, its resistance profile doesn't match the clinical picture.
*Escherichia coli*
- *E. coli* is a **Gram-negative rod**, not a Gram-positive coccus.
- It is a common cause of **urinary tract infections** and **gastrointestinal infections**, making it an unlikely pathogen for a post-surgical joint infection unless contaminated from a visceral source.
*Streptococcus viridans*
- **Viridans streptococci** are Gram-positive cocci but are typically associated with **endocarditis** or dental infections, especially after poor dental hygiene or procedures.
- They are usually **susceptible to penicillin** and do not typically exhibit nafcillin resistance as the primary feature in a post-arthroplasty infection.
*Staphylococcus epidermidis*
- *S. epidermidis* is a **coagulase-negative Staphylococcus** known for forming **biofilms on prosthetic devices**, leading to chronic, low-grade infections.
- While it can be nafcillin-resistant, the **acute presentation** with fever and significant inflammation suggests a more virulent pathogen like *S. aureus*, as *S. epidermidis* infections are typically indolent.
Biofilms in endocarditis US Medical PG Question 7: A 42-year-old woman presents to a medical office with complaints of fatigue, weight loss, and low-grade fever for 1 week. She noticed bleeding spots on her feet this morning. The past medical history is significant for a recent dental appointment. She is a non-smoker and does not drink alcohol. She does not currently take any medications. On examination, the vital signs include temperature 37.8°C (100.0°F), blood pressure 138/90 mm Hg, respirations 21/min, and pulse 87/min. Cardiac auscultation reveals a pansystolic murmur in the mitral area with radiation to the left axilla. Laboratory studies show hemoglobin levels of 17.2 g/dL, erythrocyte sedimentation rate (ESR) of 25 mm/h, and a white blood cell (WBC) count of 12,000 cells/mm3. An echocardiogram reveals valvular vegetations on the mitral valve with mild regurgitation. Blood samples are sent for bacterial culture. Empiric antibiotic therapy is initiated with ceftriaxone and vancomycin. The blood cultures most likely will yield the growth of which of the following organisms?
- A. Actinomyces israelii
- B. Coxiella burnetii
- C. Group B Streptococcus
- D. Staphylococcus aureus
- E. Streptococcus viridans (Correct Answer)
Biofilms in endocarditis Explanation: ***Streptococcus viridans***
- The patient's recent **dental appointment**, the presence of an **oral organism**, and symptoms consistent with **subacute bacterial endocarditis** (fatigue, fever, weight loss, petechiae) strongly suggest *S. viridans* as the causative agent.
- *Streptococcus viridans* species are common inhabitants of the **oral flora** and are a leading cause of endocarditis following dental procedures, especially in individuals with pre-existing valvular abnormalities.
*Actinomyces israelii*
- While *Actinomyces israelii* is an oral commensal, it typically causes **actinomycosis**, a chronic, suppurative infection characterized by abscess formation and sinus tracts, often following dental procedures.
- It less commonly presents as acute or subacute endocarditis and would not typically cause the rapid progression of symptoms described.
*Coxiella burnetii*
- *Coxiella burnetii* causes **Q fever**, which can manifest as endocarditis, often associated with exposure to **farm animals** or their products.
- The patient's history lacks any such exposure, and the clinical presentation is more aligned with standard bacterial endocarditis from oral flora.
*Group B Streptococcus*
- **Group B Streptococcus** (*Streptococcus agalactiae*) is primarily known as a cause of **neonatal sepsis** and meningitis, and infections in immunocompromised adults or those with underlying conditions like diabetes.
- It is not typically associated with endocarditis following a dental procedure in an otherwise healthy adult.
*Staphylococcus aureus*
- **Staphylococcus aureus** can cause endocarditis, particularly in **intravenous drug users** or patients with prosthetic valves/indwelling lines, and often presents as a more **acute and aggressive disease**.
- While possible, the association with a recent dental procedure and the subacute course makes *Streptococcus viridans* a more likely culprit in this specific scenario.
Biofilms in endocarditis US Medical PG Question 8: Blood cultures are sent to the laboratory and empiric treatment with intravenous vancomycin is started. Blood cultures grow gram-negative bacilli identified as Cardiobacterium hominis. Which of the following is the most appropriate next step in management?
- A. Switch to intravenous gentamicin
- B. Switch to intravenous ampicillin
- C. Switch to intravenous ceftriaxone (Correct Answer)
- D. Switch to intravenous cefazolin
- E. Add intravenous rifampin
Biofilms in endocarditis Explanation: ***Switch to intravenous ceftriaxone***
- **Cardiobacterium hominis** is part of the **HACEK group** of bacteria, which are known for causing **endocarditis**.
- These organisms are typically susceptible to **beta-lactam antibiotics**, with **third-generation cephalosporins** like ceftriaxone being the drug of choice due to their excellent activity and good penetration.
*Switch to intravenous gentamicin*
- While **aminoglycosides** like gentamicin can be used in combination regimens for serious infections, they are generally **not monotherapy** for HACEK endocarditis and are associated with **nephrotoxicity** and **ototoxicity**.
- The primary treatment for HACEK endocarditis is a **beta-lactam antibiotic**, not an aminoglycoside alone.
*Switch to intravenous ampicillin*
- **Ampicillin** is a beta-lactam, but it may not consistently provide optimal coverage for all HACEK organisms, and some strains may have reduced susceptibility.
- **Third-generation cephalosporins** are preferred due to their broader and more consistent activity against this group.
*Switch to intravenous cefazolin*
- **Cefazolin** is a first-generation cephalosporin and typically has **limited activity** against gram-negative bacilli, especially those like Cardiobacterium hominis which require broader-spectrum beta-lactams.
- Its spectrum of activity is primarily against **gram-positive bacteria** and some **gram-negative cocci**.
*Add intravenous rifampin*
- **Rifampin** is primarily used for **mycobacterial infections** and in combination regimens for specific bacterial infections (e.g., bone and joint infections, prosthetic device infections) often due to resistant staphylococci.
- It is **not a first-line agent** for Cardiobacterium hominis infections and there's no indication for its use here with an organism susceptible to ceftriaxone.
Biofilms in endocarditis US Medical PG Question 9: A 24-year-old man presents with low-grade fever and shortness of breath for the last 3 weeks. Past medical history is significant for severe mitral regurgitation status post mitral valve replacement five years ago. His temperature is 38.3°C (101.0°F) and respiratory rate is 18/min. Physical examination reveals vertical hemorrhages under his nails, multiple painless erythematous lesions on his palms, and two tender, raised nodules on his fingers. Cardiac auscultation reveals a new-onset 2/6 holosystolic murmur loudest at the apex with the patient in the left lateral decubitus position. A transesophageal echocardiogram reveals vegetations on the prosthetic valve. Blood cultures reveal catalase-positive, gram-positive cocci. Which of the following characteristics is associated with the organism most likely responsible for this patient’s condition?
- A. Coagulase positive
- B. DNAse positive
- C. Hemolysis
- D. Novobiocin sensitive (Correct Answer)
- E. Optochin sensitive
Biofilms in endocarditis Explanation: ***Novobiocin sensitive***
- The patient has **prosthetic valve endocarditis** caused by a **catalase-positive, gram-positive coccus**, which is most likely **_Staphylococcus epidermidis_** due to its association with foreign bodies and prosthetic devices.
- _Staphylococcus epidermidis_ is a **coagulase-negative staphylococcus** that is **novobiocin sensitive**, helping to differentiate it from other coagulase-negative staphylococci like **_Staphylococcus saprophyticus_** (novobiocin resistant).
- Although this is late prosthetic valve endocarditis (5 years post-surgery), _S. epidermidis_ remains a common pathogen due to biofilm formation on prosthetic materials.
*Coagulase positive*
- **Coagulase-positive** gram-positive cocci, such as **_Staphylococcus aureus_**, are a common cause of endocarditis, especially in intravenous drug users and can also cause prosthetic valve endocarditis.
- However, the correct answer requires identifying the characteristic that differentiates the most likely organism, and **coagulase-negative** staphylococci like _S. epidermidis_ are more characteristically associated with prosthetic device infections due to their biofilm-forming capabilities.
- A positive coagulase test differentiates _S. aureus_ from coagulase-negative staphylococci.
*DNAse positive*
- **DNAse positivity** is characteristic of **_Staphylococcus aureus_** and group A beta-hemolytic streptococci (_Streptococcus pyogenes_).
- While _S. aureus_ can cause prosthetic valve endocarditis, the question asks for the characteristic most associated with the likely organism, which in the context of prosthetic devices is typically **_S. epidermidis_** (DNAse negative).
*Hemolysis*
- **Hemolysis patterns** are primarily used to differentiate **streptococcal species**, not staphylococci. For example, **beta-hemolytic streptococci** cause complete hemolysis.
- While some staphylococci can show hemolytic activity, it is not a primary characteristic used to differentiate between the most likely staphylococcal causes of prosthetic valve endocarditis.
*Optochin sensitive*
- **Optochin sensitivity** is a key characteristic used to identify **_Streptococcus pneumoniae_**.
- _S. pneumoniae_ is **catalase-negative**, while the described organism is **catalase-positive**, ruling out _S. pneumoniae_ as the causative agent.
Biofilms in endocarditis US Medical PG Question 10: A hospital implements silver-coated central venous catheters to reduce catheter-related bloodstream infections. Initial results show 60% reduction in infections at 1 week, but this benefit decreases to 20% reduction by 4 weeks. Electron microscopy of explanted catheters shows biofilm formation with embedded bacteria despite the silver coating. What mechanism best explains the loss of antimicrobial efficacy over time?
- A. Depletion of silver ions from the catheter surface through diffusion
- B. Matrix proteins binding silver ions and reducing bioavailability
- C. Development of silver-tolerant persister cell populations
- D. Bacterial mutation conferring genetic resistance to silver ions
- E. Host protein deposition creating a conditioning film blocking silver release (Correct Answer)
Biofilms in endocarditis Explanation: ***Host protein deposition creating a conditioning film blocking silver release***
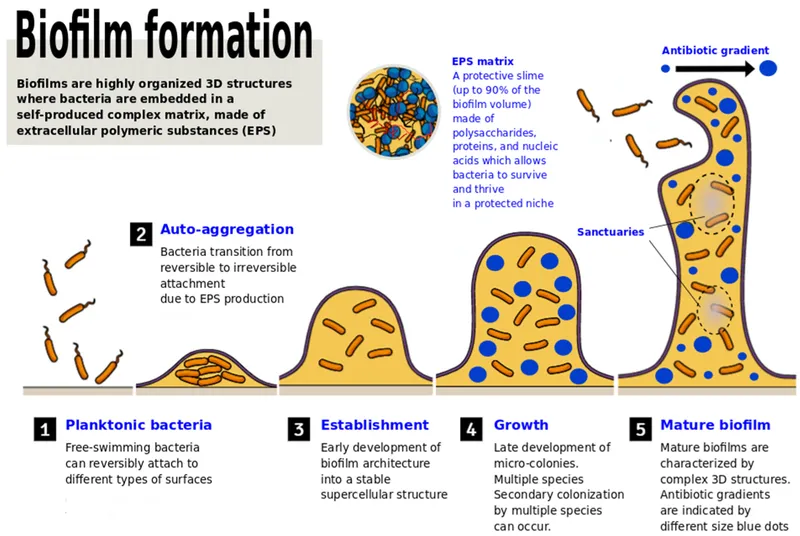
- Rapid adsorption of host proteins like **fibrinogen, fibronectin, and albumin** creates a **conditioning film** that physically masks the antimicrobial surface.
- This protein layer acts as a barrier to **ion release** and provides a scaffold for **bacterial adhesion**, facilitating the transition to a long-term **biofilm** state.
*Depletion of silver ions from the catheter surface through diffusion*
- Modern antimicrobial catheters are designed for **sustained release**, and the presence of silver on explanted microscopy suggests the reservoir is not yet empty.
- If diffusion were the only factor, efficacy would decline linearly rather than being linked to the physical observation of **biofilm formation** over the coating.
*Matrix proteins binding silver ions and reducing bioavailability*
- While some binding may occur, this is not the primary mechanism of clinical failure; the principal issue is the physical **obstruction of the surface**.
- This theory does not account for how bacteria are able to initially colonize and survive in **close physical contact** with the coated surface.
*Development of silver-tolerant persister cell populations*
- **Persister cells** are phenotypically dormant and survive antibiotics, but they do not typically cause the gradual, large-scale reduction in antimicrobial device efficacy seen here.
- The microscopy findings emphasize **structural biofilm layers** rather than a specific metabolic state of individual bacteria.
*Bacterial mutation conferring genetic resistance to silver ions*
- True **genetic resistance** to silver (via sil operons) is clinically rare and usually occurs through **efflux pumps**, not biofilm-mediated shielding.
- The scenario describes a loss of efficacy common across multiple hospital settings, whereas **mutational resistance** would be more sporadic or localized.
More Biofilms in endocarditis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.