Biofilms in cystic fibrosis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Biofilms in cystic fibrosis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Biofilms in cystic fibrosis US Medical PG Question 1: A 4-year-old boy is brought by his parents to his pediatrician’s office. His mother mentions that the child has been producing an increased number of foul stools recently. His mother says that over the past year, he has had 1 or 2 foul-smelling stools per month. Lately, however, the stools are looser, more frequent, and have a distinct odor. Over the past several years, he has been admitted 4 times with episodes of pneumonia. Genetic studies reveal a mutation on a specific chromosome that has led to a 3 base-pair deletion for the amino acid phenylalanine. Which of the following chromosomes is the defective gene responsible for this boy’s clinical condition?
- A. Chromosome 4
- B. Chromosome 7 (Correct Answer)
- C. Chromosome 22
- D. Chromosome 17
- E. Chromosome 15
Biofilms in cystic fibrosis Explanation: ***Chromosome 7***
- This patient's symptoms (recurrent pneumonia, foul-smelling stools/steatorrhea) are classic for **cystic fibrosis (CF)**. The most common mutation in CF is a **3-base pair deletion for phenylalanine** (ΔF508), located on the **CFTR gene** on **chromosome 7**.
- The cystic fibrosis transmembrane conductance regulator (CFTR) gene, which is defective in CF, is found on **the long arm (q) of chromosome 7** at position 31.2.
*Chromosome 4*
- **Chromosome 4** is associated with genetic disorders such as **Huntington's disease** and **Wolf-Hirschhorn syndrome**, which do not match the clinical presentation of recurrent pneumonia and steatorrhea.
- Huntington's disease involves trinucleotide repeats and primarily affects neurological function later in life.
*Chromosome 22*
- **Chromosome 22** is implicated in conditions like **DiGeorge syndrome** (22q11.2 deletion syndrome) and certain leukemias, none of which present with the described gastrointestinal and pulmonary symptoms.
- DiGeorge syndrome is characterized by cardiac defects, abnormal facies, thymic hypoplasia, cleft palate, and hypocalcemia.
*Chromosome 17*
- **Chromosome 17** is associated with diseases such as **Neurofibromatosis type 1** and **hereditary breast and ovarian cancer** (BRCA1 gene), which are inconsistent with the patient's symptoms.
- Neurofibromatosis type 1 primarily involves the skin, nervous system, and bones, with manifestations like café-au-lait spots and neurofibromas.
*Chromosome 15*
- **Chromosome 15** is linked to disorders like **Prader-Willi syndrome** and **Angelman syndrome**, which are distinct neurodevelopmental disorders not characterized by recurrent respiratory infections and malabsorption.
- These syndromes result from genomic imprinting defects and present with intellectual disability, developmental delay, and specific physical features.
Biofilms in cystic fibrosis US Medical PG Question 2: A 20-year-old woman presents for a follow-up visit with her physician. She has a history of cystic fibrosis and is currently under treatment. She has recently been struggling with recurrent bouts of cough and foul-smelling, mucopurulent sputum over the past year. Each episode lasts for about a week or so and then subsides. She does not have a fever or chills during these episodes. She has been hospitalized several times for pneumonia as a child and continues to struggle with diarrhea. Physically she appears to be underweight and in distress. Auscultation reveals reduced breath sounds on the lower lung fields with prominent rhonchi. Which of the following infectious agents is most likely associated with the recurrent symptoms this patient is experiencing?
- A. Mycobacterium avium
- B. Pseudomonas (Correct Answer)
- C. Histoplasma
- D. Pneumococcus
- E. Listeria
Biofilms in cystic fibrosis Explanation: ***Pseudomonas***
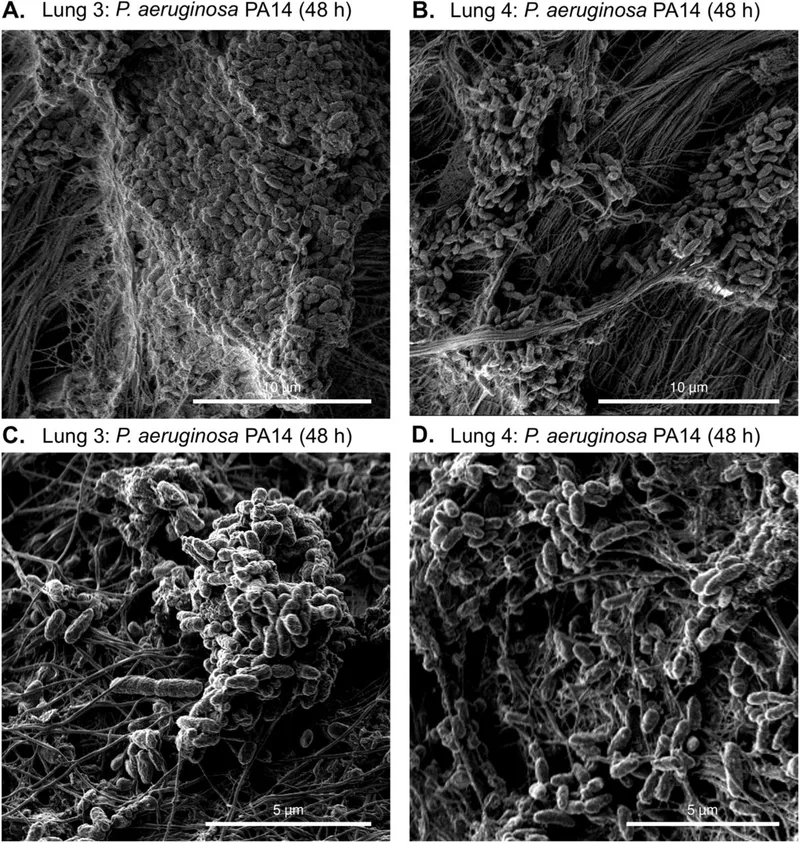
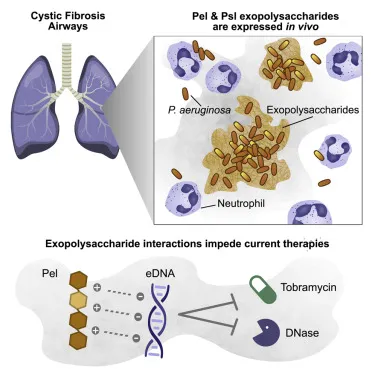
- **Pseudomonas aeruginosa** is a common and opportunistic pathogen in patients with **cystic fibrosis** due to altered mucus secretion and impaired mucociliary clearance.
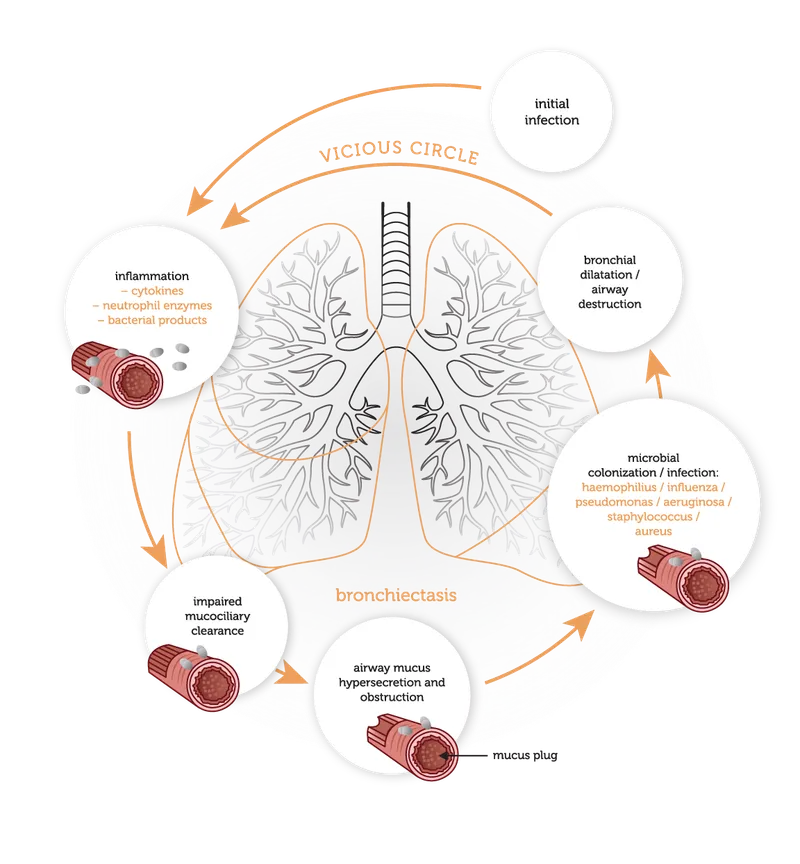
- Recurrent cough, foul-smelling, and **mucopurulent sputum** are classic symptoms of **Pseudomonas** lung infections in CF patients, often leading to chronic colonization and bronchiectasis.
*Mycobacterium avium*
- While *Mycobacterium avium complex* (MAC) can infect patients with cystic fibrosis, it typically causes a **more indolent and chronic lung disease** rather than recurrent, self-limiting bouts of cough and sputum.
- MAC infections are often associated with **nodular or cavitary lesions** on imaging and may require prolonged multidrug therapy.
*Histoplasmosis*
- **Histoplasmosis** is a fungal infection endemic to certain geographic regions (e.g., Ohio and Mississippi River valleys) and is acquired by inhaling spores.
- It's **not a typical or recurrent pathogen** in cystic fibrosis patients in the way bacterial infections are, and its presentation often includes fever, chills, and disseminated disease in immunocompromised individuals.
*Pneumococcus*
- *Streptococcus pneumoniae* (**Pneumococcus**) is a common cause of **acute bacterial pneumonia** in the general population, including young children.
- While CF patients can get pneumococcal infections, the pattern of **recurrent bouts of foul-smelling mucopurulent sputum** without fever and the chronic nature of the lung disease point away from typical acute pneumococcal infection and more towards a chronic colonizer like *Pseudomonas*.
*Listeria*
- *Listeria monocytogenes* is primarily a cause of **foodborne illness**, leading to gastroenteritis, meningitis, or sepsis, particularly in immunocompromised individuals, pregnant women, and neonates.
- It is **not a common respiratory pathogen**, and its presentation does not align with the described recurrent pulmonary symptoms in a cystic fibrosis patient.
Biofilms in cystic fibrosis US Medical PG Question 3: A 55-year-old woman comes to the physician with a 6-month history of cough and dyspnea. She has smoked 1 pack of cigarettes daily for the past 30 years. Analysis of the sputum sample from bronchoalveolar lavage shows abnormal amounts of an isoform of elastase that is normally inhibited by alpha-1 antitrypsin. The cell responsible for secreting this elastase is most likely also responsible for which of the following functions?
- A. Phagocytosis of foreign material (Correct Answer)
- B. Production of lactoferrin
- C. Degradation of toxins
- D. Secretion of mucus
- E. Diffusion of gases
Biofilms in cystic fibrosis Explanation: ***Phagocytosis of foreign material***
- The abnormal elastase described is **neutrophil elastase**, which is normally inhibited by **alpha-1 antitrypsin**.
- **Neutrophils** are the primary cells responsible for secreting this elastase, and their main function is the **phagocytosis of foreign material** and pathogens.
*Production of lactoferrin*
- **Lactoferrin** is an iron-binding protein with antimicrobial properties, primarily produced by **neutrophils**, but it is not their defining or most unique function in the context of elastase secretion and lung pathology.
- While neutrophils do produce lactoferrin, the question asks for a function that aligns with the described cellular pathology following elastase release.
*Degradation of toxins*
- While certain immune cells and organs (e.g., liver) are involved in **detoxification**, it is not a primary or most characteristic function of **neutrophils** in the lung.
- Neutrophils are more focused on direct microbial killing and inflammation rather than broad toxin degradation.
*Secretion of mucus*
- **Mucus secretion** in the airways is primarily a function of **goblet cells** and submucosal glands, not neutrophils.
- Excessive mucus secretion is a feature of chronic bronchitis, which can coexist with emphysema, but neutrophils themselves do not secrete mucus.
*Diffusion of gases*
- **Gas diffusion** is the primary function of **type I pneumocytes** in the alveolar sacs, which form the thin barrier between air and blood.
- This function is entirely unrelated to the role of neutrophils or the secretion of elastase.
Biofilms in cystic fibrosis US Medical PG Question 4: A 14-year-old girl is brought to the emergency department because of a 3-day history of worsening confusion, high-grade fever, and a productive cough. She has had recurrent respiratory infections and bulky, foul-smelling, oily stools since infancy. She is at the 14th percentile for height and 8th percentile for weight. Despite appropriate care, the patient dies 2 days after admission. Autopsy of the lungs shows bronchial mucus plugging and bronchiectasis. Which of the following is the most likely underlying cause of this patient's condition?
- A. Mutation of DNAI1 gene on chromosome 9
- B. Deficiency in alpha-1 antitrypsin
- C. Deficiency in apolipoprotein B-48
- D. Deficiency in adenosine deaminase
- E. Deletion of phenylalanine codon on chromosome 7 (Correct Answer)
Biofilms in cystic fibrosis Explanation: ***Deletion of phenylalanine codon on chromosome 7***
- The patient's presentation of **recurrent respiratory infections**, **bronchial mucus plugging**, **bronchiectasis**, and **malabsorption** (foul-smelling, oily stools, failure to thrive) is classic for **cystic fibrosis**.
- **Cystic fibrosis** is most commonly caused by a **deletion of three base pairs** coding for phenylalanine at position 508 (**ΔF508**) on the **CFTR gene** located on **chromosome 7**.
*Mutation of DNAI1 gene on chromosome 9*
- A mutation in the **DNAI1 gene** on chromosome 9 is associated with **primary ciliary dyskinesia (PCD)**.
- While PCD can cause recurrent respiratory infections and bronchiectasis due to impaired mucociliary clearance, it typically **does not involve the pancreatic insufficiency** and malabsorption suggested by the oily stools and failure to thrive in this patient.
*Deficiency in alpha-1 antitrypsin*
- **Alpha-1 antitrypsin deficiency** primarily leads to early-onset **emphysema** and liver disease, not typically the severe pancreatic insufficiency and recurrent bacterial infections seen in cystic fibrosis.
- While it can cause lung damage, the absence of symptoms related to **pancreatic dysfunction** makes this less likely.
*Deficiency in apolipoprotein B-48*
- A deficiency in **apolipoprotein B-48** is associated with **abetalipoproteinemia**, a disorder characterized by the inability to synthesize chylomicrons, leading to severe malabsorption of dietary fats and fat-soluble vitamins.
- While it causes malabsorption and greasy stools, it **does not typically present with recurrent respiratory infections, mucus plugging, and bronchiectasis**, which are prominent features in this case.
*Deficiency in adenosine deaminase*
- A deficiency in **adenosine deaminase (ADA)** leads to **severe combined immunodeficiency (SCID)**, characterized by profound lymphopenia and recurrent infections (bacterial, viral, fungal).
- While SCID causes recurrent infections and failure to thrive, it typically **does not present with the specific pulmonary pathology of mucus plugging and bronchiectasis**, nor the **pancreatic exocrine insufficiency** suggested by the oily stools.
Biofilms in cystic fibrosis US Medical PG Question 5: A 51-year-old man with alcohol use disorder comes to the physician because of a fever and productive cough. An x-ray of the chest shows a right lower lobe consolidation and a diagnosis of aspiration pneumonia is made. The physician prescribes a drug that blocks peptide transfer by binding to the 50S ribosomal subunit. Which of the following drugs was most likely prescribed?
- A. Ceftriaxone
- B. Doxycycline
- C. Metronidazole
- D. Clindamycin (Correct Answer)
- E. Azithromycin
Biofilms in cystic fibrosis Explanation: ***Clindamycin***
- **Clindamycin** is a lincosamide antibiotic that **blocks peptide transfer** by binding to the **50S ribosomal subunit**, inhibiting bacterial protein synthesis.
- It is a highly effective treatment for **aspiration pneumonia** due to its excellent activity against the **anaerobic bacteria** commonly found in oral flora, which are the primary pathogens in this condition.
*Ceftriaxone*
- **Ceftriaxone** is a third-generation cephalosporin that inhibits bacterial cell wall synthesis by binding to **penicillin-binding proteins**, not the 50S ribosomal subunit.
- While it has broad-spectrum activity, it is typically used for community-acquired pneumonia and is less effective against the **anaerobic organisms** predominant in aspiration pneumonia.
*Doxycycline*
- **Doxycycline** is a tetracycline antibiotic that binds to the **30S ribosomal subunit**, preventing the attachment of aminoacyl-tRNA.
- While effective against some respiratory pathogens, it is not the first-line choice for **aspiration pneumonia** as its anaerobic coverage is insufficient.
*Metronidazole*
- **Metronidazole** acts by forming **cytotoxic compounds** that damage bacterial DNA after reduction by anaerobic enzymes, rather than binding to ribosomal subunits.
- While effective against many **anaerobes**, it is often used in combination with other antibiotics for aspiration pneumonia, and its mechanism of action is distinct from that described.
*Azithromycin*
- **Azithromycin** is a macrolide antibiotic that also binds to the **50S ribosomal subunit**, but it **inhibits translocation** of the growing peptide chain, not primarily peptide transfer.
- While used for community-acquired pneumonia, its coverage for **oropharyngeal anaerobes** can be inconsistent, making clindamycin a more reliable choice for aspiration pneumonia.
Biofilms in cystic fibrosis US Medical PG Question 6: An 11-year-old boy who recently emigrated from Ukraine is brought to the physician for the evaluation of failure to thrive. Genetic analysis shows the deletion of the 508th codon in a gene on chromosome 7. The deletion results in defective post-translational folding of a protein and retention of the misfolded protein in the rough endoplasmic reticulum. The activity of which of the following channels is most likely to be increased as a result of the defect?
- A. Calcium channels of distal tubular cells
- B. ATP-sensitive potassium channels of pancreatic beta cells
- C. Bicarbonate channels of pancreatic ductal cells
- D. Chloride channels of epithelial cells in sweat glands
- E. Sodium channels of respiratory epithelial cells (Correct Answer)
Biofilms in cystic fibrosis Explanation: ***Sodium channels of respiratory epithelial cells***
- The patient's presentation with **failure to thrive**, genetic defect (deletion of codon 508 on chromosome 7), and **defective protein folding** are classic for **cystic fibrosis (CF)**.
- In CF, the defective **CFTR protein** (a chloride channel) leads to reduced chloride secretion and increased **sodium absorption** in respiratory epithelial cells, causing thickened mucus.
*Calcium channels of distal tubular cells*
- Dysfunction of **calcium channels** in the distal tubules is not a primary feature of cystic fibrosis.
- Renal calcium handling issues are typically associated with conditions like **Dent's disease** or various types of **renal tubular acidosis**, not CF.
*ATP-sensitive potassium channels of pancreatic beta cells*
- While CF can lead to pancreatic insufficiency and **CF-related diabetes**, the primary defect is not in the **ATP-sensitive potassium channels** of beta cells.
- The insulin deficiency in CF diabetes is due to destruction of pancreatic islets secondary to duct obstruction and inflammation.
*Bicarbonate channels of pancreatic ductal cells*
- In cystic fibrosis, the **CFTR protein** is a chloride channel that also facilitates bicarbonate transport, and its dysfunction does impair **bicarbonate secretion** in pancreatic ductal cells.
- However, the question specifically asks about an *increase* in channel activity, and bicarbonate channel activity is *decreased* in CF.
*Chloride channels of epithelial cells in sweat glands*
- The **CFTR protein** is indeed a **chloride channel** in sweat glands, and in CF, its *activity is decreased*, leading to reduced chloride reabsorption and high sweat chloride (the basis for the sweat test).
- The question asks for an *increased* channel activity, which is seen with sodium channels due to the linked transport mechanisms.
Biofilms in cystic fibrosis US Medical PG Question 7: A 9-year-old boy with cystic fibrosis (CF) presents to the clinic with fever, increased sputum production, and cough. The vital signs include: temperature 38.0°C (100.4°F), blood pressure 126/74 mm Hg, heart rate 103/min, and respiratory rate 22/min. His physical examination is significant for short stature, thin body frame, decreased breath sounds bilateral, and a 2/6 holosystolic murmur heard best on the upper right sternal border. His pulmonary function tests are at his baseline, and his sputum cultures reveal Pseudomonas aeruginosa. What is the best treatment option for this patient?
- A. Dornase alfa 2.5 mg as a single-use
- B. Oral cephalexin for 14 days
- C. Inhaled tobramycin for 28 days (Correct Answer)
- D. Minocycline for 28 days
- E. Sulfamethoxazole and trimethoprim for 14 days
Biofilms in cystic fibrosis Explanation: ***Inhaled tobramycin for 28 days***
- This patient presents with a **mild pulmonary exacerbation** of **cystic fibrosis (CF)**, characterized by fever, increased sputum production, and the isolation of **Pseudomonas aeruginosa** from sputum cultures.
- The **pulmonary function tests (PFTs) at baseline** indicate this is a **mild exacerbation** that can be managed in the **outpatient setting**.
- **Inhaled tobramycin** is the appropriate first-line treatment for **mild-to-moderate exacerbations** and for **chronic suppressive therapy** of **Pseudomonas aeruginosa** infections in CF patients.
- It is effective in improving lung function, reducing bacterial load, and decreasing exacerbation frequency with minimal systemic toxicity.
- More severe exacerbations (significant PFT decline, respiratory distress) would require **IV antipseudomonal antibiotics**.
*Dornase alfa 2.5 mg as a single-use*
- **Dornase alfa** (DNase) is a mucolytic agent used in CF to reduce sputum viscosity and improve airway clearance by breaking down extracellular DNA in mucus.
- While beneficial for **chronic airway clearance therapy**, it is not an antibiotic and does not directly treat the **bacterial infection** causing the current exacerbation.
*Oral cephalexin for 14 days*
- **Cephalexin** is a first-generation cephalosporin that primarily targets **gram-positive bacteria** (such as Staphylococcus aureus) and some **gram-negative bacteria**.
- It is **completely ineffective against Pseudomonas aeruginosa**, which is intrinsically resistant to first-generation cephalosporins.
*Minocycline for 28 days*
- **Minocycline** is a **tetracycline antibiotic** with activity against many bacteria, including some **atypical pathogens** and **Staphylococcus aureus**.
- However, it is **not effective against Pseudomonas aeruginosa**, which is intrinsically resistant to tetracyclines and is a common and aggressive pathogen in CF patients.
*Sulfamethoxazole and trimethoprim for 14 days*
- **Sulfamethoxazole and trimethoprim** (TMP-SMX, Bactrim) is an antibiotic combination effective against various bacteria, including some **gram-negative organisms** and **Staphylococcus aureus**.
- It does **not provide adequate coverage for Pseudomonas aeruginosa**, making it an inappropriate choice for this patient's documented infection.
Biofilms in cystic fibrosis US Medical PG Question 8: A 7-year-old boy with a history of cystic fibrosis is brought to the physician for evaluation of recurrent episodes of productive cough, wheezing, and shortness of breath over the past month. Physical examination shows coarse crackles and expiratory wheezing over both lung fields. Serum studies show elevated levels of IgE and eosinophilia. A CT scan of the lungs shows centrally dilated bronchi with thickened walls and peripheral airspace consolidation. Antibiotic therapy is initiated. One week later, the patient continues to show deterioration in lung function. A sputum culture is most likely to grow which of the following?
- A. Monomorphic, septate hyphae that branch at acute angles (Correct Answer)
- B. Monomorphic, broad, nonseptate hyphae that branch at wide angles
- C. Dimorphic, broad-based budding yeast
- D. Dimorphic, cigar-shaped budding yeast
- E. Monomorphic, narrow budding encapsulated yeast
Biofilms in cystic fibrosis Explanation: **Monomorphic, septate hyphae that branch at acute angles**
- The patient's presentation with **cystic fibrosis (CF)**, recurrent respiratory symptoms, CT findings of **central bronchiectasis**, elevated **IgE**, and **eosinophilia** strongly points towards **allergic bronchopulmonary aspergillosis (ABPA)**.
- *Aspergillus fumigatus*, the causative agent of ABPA, is characterized microscopically by **monomorphic, septate hyphae that branch at acute angles**.
*Monomorphic, broad, nonseptate hyphae that branch at wide angles*
- This describes organisms like *Rhizopus* or *Mucor*, which cause **mucormycosis**.
- Mucormycosis typically affects immunocompromised individuals (e.g., diabetics, neutropenic patients) and presents as aggressive rhinocerebral or pulmonary infections, not ABPA.
*Dimorphic, broad-based budding yeast*
- This morphology is characteristic of *Blastomyces dermatitidis*, which causes **blastomycosis**.
- Blastomycosis is an endemic fungal infection often presenting with pulmonary symptoms, but it does not cause central bronchiectasis, elevated IgE, or eosinophilia in the context of CF.
*Dimorphic, cigar-shaped budding yeast*
- This morphology describes *Sporothrix schenckii*, which causes **sporotrichosis**.
- Sporotrichosis typically presents as a chronic ulcerative skin disease (rose gardener's disease) or, less commonly, pulmonary disease, but is not associated with ABPA.
*Monomorphic, narrow budding encapsulated yeast*
- This morphology is characteristic of *Cryptococcus neoformans*, which causes **cryptococcosis**.
- Cryptococcosis commonly affects immunocompromised individuals, causing meningoencephalitis or pulmonary disease, but its presentation is distinct from ABPA, lacking the allergic and bronchiectatic features described.
Biofilms in cystic fibrosis US Medical PG Question 9: What is the chance of a child having cystic fibrosis if both parents are carriers of the disease?
- A. 75%
- B. 25% (Correct Answer)
- C. 50%
- D. 0%
- E. 100%
Biofilms in cystic fibrosis Explanation: ***50%***
- If one parent is affected by cystic fibrosis (CF), they are **homozygous for the CFTR mutation**, while the normal parent is likely **homozygous for the normal allele**.
- Each child has a **50% chance** of inheriting the **mutated allele** from the affected parent, resulting in an **autosomal recessive** inheritance pattern [1].
*70%*
- This percentage does not reflect the inheritance probabilities associated with **autosomal recessive traits** [1], such as cystic fibrosis.
- In heterozygous and normal arrangements, the calculation does not support a **70%** inheritance chance of the disease.
*80%*
- Similarly, an **80% chance** is inaccurate as cystic fibrosis requires two mutated alleles for the disease to manifest [1].
- The inheritance pattern does not allow for a higher than **50% chance** when one parent is normal.
*25%*
- A **25% chance** applies if both parents were carriers of the CFTR mutation [1]. However, with only one affected parent, this percentage does not apply.
- The maximum **chance of inheritance** from one affected and one normal parent is accurately stated as **50%**.
**References:**
[1] Cross SS. Underwood's Pathology: A Clinical Approach. 6th ed. (Basic Pathology) introduces the student to key general principles of pathology, both as a medical science and as a clinical activity with a vital role in patient care. Part 2 (Disease Mechanisms) provides fundamental knowledge about the cellular and molecular processes involved in diseases, providing the rationale for their treatment. Part 3 (Systematic Pathology) deals in detail with specific diseases, with emphasis on the clinically important aspects., pp. 53-54.
Biofilms in cystic fibrosis US Medical PG Question 10: An 8-year-old girl is brought to the pediatrician because she is significantly shorter than her classmates. Her mother notes that she has had thick, oral secretions for the past several months, along with a chronic cough. Her exam is notable for clubbed fingernails. Her pediatrician sends a genetic test for a transmembrane channel mutation, which shows a normal DNA sequence, except for the deletion of three nucleotides that code for a phenylalanine at position 508. What type of mutation has caused her presentation?
- A. Triplet expansion
- B. Nonsense mutation
- C. Frameshift mutation
- D. In-frame mutation (Correct Answer)
- E. Silent mutation
Biofilms in cystic fibrosis Explanation: ***In-frame mutation***
- The deletion of three nucleotides, which together code for a single amino acid (phenylalanine), results in an **in-frame mutation** because the reading frame of the mRNA is maintained.
- This specific mutation is **ΔF508**, the most common mutation in **cystic fibrosis (CF)**, consistent with the patient's symptoms of growth failure, thick secretions, chronic cough, and clubbed fingernails.
*Triplet expansion*
- This involves the **increase in the number of repeats of a trinucleotide sequence**, such as in Huntington's disease or fragile X syndrome.
- The patient's mutation is a **deletion**, not an expansion of a trinucleotide repeat.
*Nonsense mutation*
- A nonsense mutation involves a **point mutation** that results in a **premature stop codon**, leading to a truncated protein.
- The patient's mutation is a **deletion of an entire codon**, not a single base change leading to a stop codon.
*Frameshift mutation*
- A frameshift mutation occurs when the deletion or insertion of nucleotides is **not a multiple of three**, leading to a shift in the reading frame and alteration of all downstream amino acids.
- In this case, the deletion of **three nucleotides** maintains the reading frame, so it is not a frameshift.
*Silent mutation*
- A silent mutation is a **point mutation** where a change in a single nucleotide does not alter the amino acid sequence due to the degeneracy of the genetic code.
- Here, the **deletion of a codon** results in the loss of an amino acid, clearly altering the protein product, hence it is not silent.
More Biofilms in cystic fibrosis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.