Biofilms in chronic infections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Biofilms in chronic infections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Biofilms in chronic infections US Medical PG Question 1: An investigator is studying the growth of an organism in different media. The organism is inoculated on a petri dish that contains heated sheep blood, vancomycin, nystatin, trimethoprim, and colistin. The resulting growth medium is incubated at 37°C. Numerous small, white colonies are seen after incubation for 48 hours. This organism is most likely to cause which of the following conditions?
- A. Pontiac fever
- B. Pseudomembranous colitis
- C. Hemolytic uremic syndrome
- D. Oral thrush
- E. Gonorrhea (Correct Answer)
Biofilms in chronic infections Explanation: ***Gonorrhea***
- The growth medium described is **Thayer-Martin agar**, a selective medium containing **heated sheep blood** (supplies NAD+), **vancomycin** (inhibits Gram-positives), **colistin** (inhibits Gram-negatives), **nystatin** (inhibits fungi), and **trimethoprim** (inhibits Proteus). This medium is specifically designed for the isolation of *Neisseria gonorrhoeae* from polymicrobial samples.
- *Neisseria gonorrhoeae* typically grows as **small, translucent-to-white colonies** on selective media like Thayer-Martin agar, and incubation at 37°C in CO2 (not explicitly mentioned but often required) for 24-48 hours yields visible growth, causing **gonorrhea**.
*Pontiac fever*
- Pontiac fever is a mild, self-limiting form of **legionellosis**, caused by *Legionella pneumophila*.
- *Legionella* requires a specialized medium such as **buffered charcoal yeast extract (BCYE) agar** for growth, not Thayer-Martin agar.
*Pseudomembranous colitis*
- This condition is caused by **toxin-producing *Clostridioides difficile***, often after antibiotic use.
- *C. difficile* is an obligate anaerobe and requires **anaerobic conditions** and specific selective media (e.g., CCFA agar) for isolation, not Thayer-Martin agar under aerobic conditions.
*Hemolytic uremic syndrome*
- Hemolytic uremic syndrome (HUS) is often caused by **Shiga toxin-producing *Escherichia coli* (STEC)**, particularly O157:H7.
- STEC can be isolated on media like **sorbitol MacConkey agar (SMAC)**, where O157:H7 appears as non-sorbitol fermenting colonies, distinct from the growth seen on Thayer-Martin.
*Oral thrush*
- Oral thrush is caused by *Candida albicans*, a yeast.
- *Candida* would be inhibited by **nystatin** in the Thayer-Martin medium, which is an antifungal agent.
Biofilms in chronic infections US Medical PG Question 2: A team of intensivists working in a private intensive care unit (ICU) observe that the clinical efficacy of vancomycin is low, and proven nosocomial infections have increased progressively over the past year. A clinical microbiologist is invited to conduct a bacteriological audit of the ICU. He analyzes the microbiological reports of all patients treated with vancomycin over the last 2 years and takes relevant samples from the ICU for culture and antibiotic sensitivity analysis. The audit concludes that there is an increased incidence of vancomycin-resistant Enterococcus fecalis infections. Which of the following mechanisms best explains the changes that took place in the bacteria?
- A. Decreased number of porins in the bacterial cell wall leading to decreased intracellular entry of the antibiotic
- B. Production of an enzyme that hydrolyzes the antibiotic
- C. Protection of the antibiotic-binding site by Qnr protein
- D. Increased expression of efflux pumps which extrude the antibiotic from the bacterial cell
- E. Replacement of the terminal D-Ala in the cell wall peptidoglycan by D-lactate (Correct Answer)
Biofilms in chronic infections Explanation: ***Replacement of the terminal D-ala in the cell wall peptidoglycan by D-lactate***
- **Vancomycin** exerts its antibacterial effect by binding to the **D-Ala-D-Ala** terminus of the peptidoglycan precursor in the bacterial cell wall, preventing its incorporation.
- In **vancomycin-resistant Enterococcus (VRE)**, the D-Ala-D-Ala is replaced by **D-Ala-D-Lac**, which significantly reduces vancomycin's binding affinity, leading to resistance.
*Decreased number of porins in the bacterial cell wall leading to decreased intracellular entry of the antibiotic*
- This mechanism primarily affects **Gram-negative bacteria**, where porins are crucial for antibiotic entry through the outer membrane.
- **Enterococcus faecalis** is a **Gram-positive bacterium** and does not rely on porins in the same way for vancomycin uptake.
*Production of an enzyme that hydrolyzes the antibiotic*
- This mechanism is characteristic of resistance to **beta-lactam antibiotics** (e.g., penicillinases, cephalosporinases).
- Vancomycin is not a beta-lactam, and its resistance mechanism in Enterococcus does not typically involve enzymatic hydrolysis.
*Protection of the antibiotic-binding site by Qnr protein*
- **Qnr proteins** are associated with **quinolone resistance**, specifically by protecting DNA gyrase and topoisomerase IV from quinolone inhibition.
- This mechanism is irrelevant to vancomycin, which targets the bacterial cell wall.
*Increased expression of efflux pumps which extrude the antibiotic from the bacterial cell*
- Efflux pumps are a common mechanism of antibiotic resistance against a wide range of antibiotics, including **tetracyclines, macrolides, and fluoroquinolones**.
- While efflux pumps can contribute to some forms of resistance, they are not the primary or best-explained mechanism for **high-level vancomycin resistance in Enterococcus**.
Biofilms in chronic infections US Medical PG Question 3: A 67-year-old woman comes to the physician because of fever, chills, myalgias, and joint pain 1 month after undergoing aortic prosthetic valve replacement due to high-grade aortic stenosis. She does not drink alcohol or use illicit drugs. Her temperature is 39.3°C (102.8°F). She appears weak and lethargic. Physical examination shows crackles at both lung bases and a grade 2/6, blowing diastolic murmur over the right sternal border. Laboratory studies show leukocytosis and an elevated erythrocyte sedimentation rate. The causal organism is most likely to have which of the following characteristics?
- A. Beta hemolytic, bacitracin-sensitive cocci
- B. Alpha hemolytic, optochin-resistant cocci
- C. Catalase-negative cocci that grows in 6.5% saline
- D. Novobiocin-sensitive, coagulase-negative cocci (Correct Answer)
- E. Alpha hemolytic, optochin-sensitive diplococci
Biofilms in chronic infections Explanation: ***Novobiocin-sensitive, coagulase-negative cocci***
- The patient's symptoms (fever, chills, new murmur) and recent **prosthetic valve replacement** strongly suggest **nosocomial infective endocarditis**.
- **Staphylococcus epidermidis** is a common cause of prosthetic valve endocarditis, and it is a **coagulase-negative Staphylococcus** that is characteristically **novobiocin-sensitive**.
*Beta hemolytic, bacitracin-sensitive cocci*
- This describes **Group A Streptococcus (Streptococcus pyogenes)**, which causes pharyngitis, cellulitis, and toxic shock syndrome, but rarely infective endocarditis, particularly 1 month post-op.
- While it can cause rheumatic fever (leading to valve damage), it is not a common cause of prosthetic valve endocarditis in this specific context.
*Alpha hemolytic, optochin-resistant cocci*
- This describes **Viridans group streptococci (e.g., Streptococcus mitis, S. sanguinis)**, which are common causes of native valve endocarditis, often following dental procedures.
- However, they are typically **alpha-hemolytic** and **optochin-resistant**, not associated with prosthetic valve infections in the immediate post-operative period.
*Catalase-negative cocci that grows in 6.5% saline*
- This describes **Enterococci (e.g., Enterococcus faecalis, Enterococcus faecium)**. They are catalase-negative and can grow in 6.5% saline.
- While enterococci can cause endocarditis, particularly in patients with genitourinary or gastrointestinal procedures, they are not the most likely cause of prosthetic valve endocarditis 1 month after surgery.
*Alpha hemolytic, optochin-sensitive diplococci*
- This describes **Streptococcus pneumoniae**, a common cause of pneumonia, meningitis, and otitis media.
- While it can cause endocarditis, it is less common for prosthetic valve endocarditis in this setting and would typically present with more prominent respiratory symptoms.
Biofilms in chronic infections US Medical PG Question 4: A 25-day-old male infant presents to the emergency department because his mother states that he has been acting irritable for the past 2 days and has now developed a fever. On exam, the infant appears uncomfortable and has a temperature of 39.1 C. IV access is immediately obtained and a complete blood count and blood cultures are drawn. Lumbar puncture demonstrates an elevated opening pressure, elevated polymorphonuclear neutrophil, elevated protein, and decreased glucose. Ampicillin and cefotaxime are immediately initiated and CSF culture eventually demonstrates infection with a Gram-negative rod. Which of the following properties of this organism was necessary for the infection of this infant?
- A. K capsule (Correct Answer)
- B. M protein
- C. Fimbriae
- D. IgA protease
- E. LPS endotoxin
Biofilms in chronic infections Explanation: ***K capsule***
- The K capsule (specifically **K1 antigen**) is a specific virulence factor found in **E. coli** strains, which are a common cause of neonatal meningitis.
- This capsule is **antiphagocytic** and helps the bacteria evade the immune system, allowing it to cross the **blood-brain barrier** and cause meningitis in neonates.
*M protein*
- **M protein** is a major virulence factor associated with **Streptococcus pyogenes** (Group A Strep), playing a role in attachment and immune evasion.
- While *S. pyogenes* can cause infections, it is not typically the Gram-negative rod responsible for **neonatal meningitis** and its M protein is not relevant here.
*Fimbriae*
- **Fimbriae** (pili) are important for bacterial **adhesion** to host cells, often in the initial stages of infection, particularly in urinary tract infections (UTIs).
- While gram-negative rods possess fimbriae, the specific virulence factor critical for **meningitis** caused by *E. coli* in neonates is the K1 capsule, not fimbriae which are more for initial colonization.
*IgA protease*
- **IgA protease** is an enzyme produced by some bacteria (e.g., *N. meningitidis, H. influenzae, S. pneumoniae*) that cleaves **IgA antibodies**, helping them colonize mucous membranes.
- This enzyme is not a primary virulence factor for the **Gram-negative rod** causing neonatal meningitis, where capsule formation is more critical for invasion.
*LPS endotoxin*
- **Lipopolysaccharide (LPS) endotoxin** is a component of the outer membrane of Gram-negative bacteria and is responsible for many symptoms of sepsis and **systemic inflammation**.
- While LPS contributes to the overall disease severity, it primarily mediates **inflammation and fever**, and is not the specific factor necessary for **invasion and survival within the central nervous system**, which is facilitated by the K capsule.
Biofilms in chronic infections US Medical PG Question 5: A 47-year-old woman comes to the physician because of a 6-week history of fatigue and low-grade fever. She has no history of serious illness except for a bicuspid aortic valve, diagnosed 10 years ago. She does not use illicit drugs. Her temperature is 37.7°C (99.9°F). Physical examination shows petechiae under the fingernails and multiple tender, red nodules on the fingers. A new grade 2/6 diastolic murmur is heard at the right second intercostal space. Which of the following is the most likely causal organism?
- A. Staphylococcus epidermidis
- B. Streptococcus pyogenes
- C. Streptococcus sanguinis (Correct Answer)
- D. Streptococcus pneumoniae
- E. Enterococcus faecalis
Biofilms in chronic infections Explanation: ***Streptococcus sanguinis***
- The patient's presentation with **fatigue, low-grade fever, petechiae, tender nodules (Osler nodes)**, and a **new diastolic murmur** in a patient with a **bicuspid aortic valve** is highly suggestive of **infective endocarditis**.
- **Streptococcus sanguinis** (and other viridans streptococci) are common causes of subacute bacterial endocarditis, often associated with **oral flora** and pre-existing valvular heart disease.
*Staphylococcus epidermidis*
- This organism is a common cause of **prosthetic valve endocarditis** and **nosocomial infections** but is less likely to cause endocarditis in a native valve without a history of recent surgery or intravenous lines.
- While it can cause endocarditis, the clinical features here, especially the lack of recent medical interventions, point away from *S. epidermidis* as the primary cause.
*Streptococcus pyogenes*
- **Streptococcus pyogenes** is primarily known for causing **strep throat, scarlet fever, and rheumatic fever**, which can lead to rheumatic heart disease but rarely causes acute or subacute infective endocarditis directly.
- It typically causes more acute and severe infections, which doesn't align with the 6-week history of low-grade fever and fatigue.
*Streptococcus pneumoniae*
- **Streptococcus pneumoniae** is a common cause of **pneumonia, meningitis, and otitis media** but is an uncommon cause of infective endocarditis, accounting for a very small percentage of cases.
- Endocarditis due to *S. pneumoniae* tends to be **acute and fulminant**, often associated with severe systemic illness, which is not fully consistent with the subacute presentation here.
*Enterococcus faecalis*
- **Enterococcus faecalis** is a common cause of **nosocomial urinary tract infections** and can cause endocarditis, especially in older patients or those with gastrointestinal or genitourinary procedures.
- While it's a possibility for endocarditis, the oral flora association with viridans streptococci (like *S. sanguinis*) in the context of a bicuspid aortic valve makes it a more direct fit.
Biofilms in chronic infections US Medical PG Question 6: While testing various strains of Streptococcus pneumoniae, a researcher discovers that a certain strain of this bacteria is unable to cause disease in mice when deposited in their lungs. What physiological test would most likely deviate from normal in this strain of bacteria as opposed to a typical strain?
- A. Quellung reaction (Correct Answer)
- B. Hemolytic reaction when grown on sheep blood agar
- C. Bile solubility
- D. Optochin sensitivity
- E. Motility
Biofilms in chronic infections Explanation: ***Quellung reaction***
- The **Quellung reaction** tests for the presence of the **polysaccharide capsule**, which is the primary virulence factor of *S. pneumoniae*.
- An **avirulent strain** that cannot cause disease would most likely lack the capsule and show a **negative Quellung reaction** (no capsular swelling), deviating from the **positive reaction** seen in typical encapsulated pathogenic strains.
- The capsule enables *S. pneumoniae* to evade phagocytosis and complement-mediated killing, which is essential for establishing infection in the lungs.
*Hemolytic reaction when grown on sheep blood agar*
- Both virulent and avirulent strains of *S. pneumoniae* typically exhibit **alpha-hemolysis** (partial hemolysis, producing a greenish discoloration) on sheep blood agar due to the production of pneumolysin.
- This characteristic does not differentiate between pathogenic and non-pathogenic strains in terms of disease-causing ability.
*Bile solubility*
- *S. pneumoniae* is characteristically **bile-soluble** due to the presence of autolysin enzymes that are activated by bile salts, leading to cellular lysis.
- This property is a **species characteristic** present in both virulent and avirulent strains, thus it would not explain the inability to cause disease.
*Optochin sensitivity*
- *S. pneumoniae* is universally **sensitive to optochin**, a chemical agent that inhibits its growth and is used for laboratory identification.
- This characteristic is used for **species identification** but does not correlate with strain virulence or disease-causing ability.
*Motility*
- *Streptococcus pneumoniae* is a **non-motile** bacterium; it lacks flagella.
- This characteristic is consistent across all strains and is not a virulence factor for this species.
Biofilms in chronic infections US Medical PG Question 7: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Biofilms in chronic infections Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Biofilms in chronic infections US Medical PG Question 8: A 54-year-old man comes to the physician because of persistent right knee pain and swelling for 2 weeks. Six months ago, he had a total knee replacement because of osteoarthritis. His temperature is 38.5°C (101.3°F), pulse is 100/min, and blood pressure is 139/84 mm Hg. Examination shows warmth and erythema of the right knee; range of motion is limited by pain. His leukocyte count is 14,500/mm3, and erythrocyte sedimentation rate is 50 mm/hr. Blood cultures grow gram-positive, catalase-positive cocci. These bacteria grow on mannitol salt agar without color change. Production of which of the following is most important for the organism's virulence?
- A. Vi capsule
- B. Exotoxin A
- C. Cord factor
- D. Exopolysaccharides (Correct Answer)
- E. Protein A
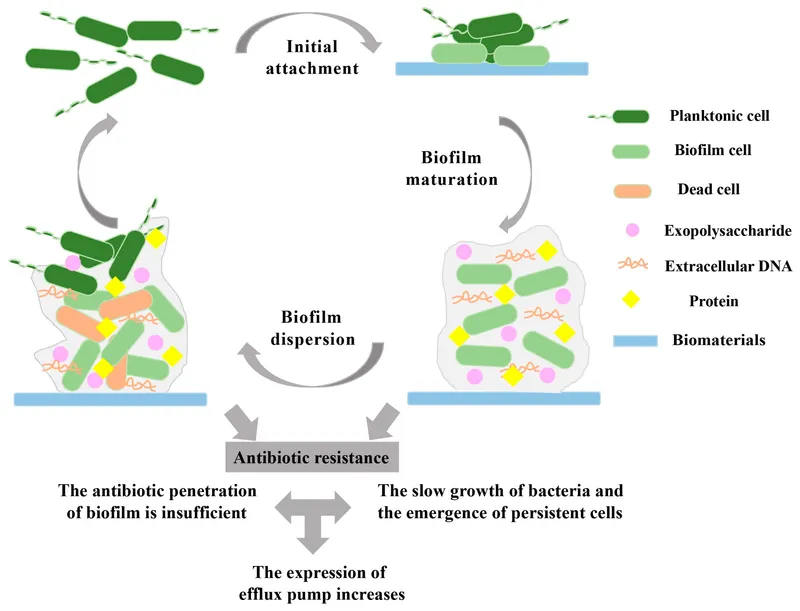
Biofilms in chronic infections Explanation: ***Exopolysaccharides***
- The patient presents with **fever**, **joint pain and swelling**, elevated **leukocyte count** and **ESR**, and a history of **total knee replacement**, all indicative of a **prosthetic joint infection**.
- The pathogen is described as **gram-positive**, **catalase-positive cocci** that grow on mannitol salt agar without a color change, suggesting **Staphylococcus epidermidis** or a similar coagulase-negative Staphylococcus species. These pathogens are known for forming **biofilms (exopolysaccharides)** on foreign bodies, making treatment difficult.
*Vi capsule*
- The **Vi capsule** is a virulence factor primarily associated with **Salmonella typhi**, which causes typhoid fever.
- The clinical presentation and microbiological findings (gram-positive cocci) do not match **Salmonella typhi** infection.
*Exotoxin A*
- **Exotoxin A** is a potent virulence factor produced by **Pseudomonas aeruginosa**, a gram-negative rod.
- The bacterial description in the stem (gram-positive, catalase-positive cocci) is inconsistent with **Pseudomonas aeruginosa**.
*Cord factor*
- **Cord factor** is a mycolic acid-containing glycolipid found in the cell wall of **Mycobacterium tuberculosis** and other mycobacteria.
- The pathogen in this case is described as **gram-positive cocci**, which rules out a mycobacterial infection.
*Protein A*
- **Protein A** is a cell wall component of **Staphylococcus aureus** that binds to the Fc region of IgG, inhibiting opsonization and phagocytosis.
- While *Staphylococcus aureus* is a gram-positive, catalase-positive cocci, its typical growth on mannitol salt agar involves **yellowing (fermentation of mannitol)** due to acid production, which is not described here ("without color change").
Biofilms in chronic infections US Medical PG Question 9: A 65-year-old man is brought to the emergency department after coughing up copious amounts of blood-tinged sputum at his nursing home. He recently had an upper respiratory tract infection that was treated with antibiotics. He has a long-standing history of productive cough that has worsened since he had a stroke 3 years ago. He smoked a pack of cigarettes daily for 40 years until the stroke, after which he quit. The patient appears distressed and short of breath. His temperature is 38°C (100.4°F), pulse is 92/min, and blood pressure is 145/85 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 92%. Physical examination shows digital clubbing and cyanosis of the lips. Coarse crackles are heard in the thorax. An x-ray of the chest shows increased translucency and tram-track opacities in the right lower lung field. Which of the following is the most likely diagnosis?
- A. Aspiration pneumonia
- B. Pulmonary embolism
- C. Lung cancer
- D. Bronchiectasis (Correct Answer)
- E. Emphysema
Biofilms in chronic infections Explanation: ***Bronchiectasis***
- The patient's history of **chronic productive cough**, **hemoptysis** (blood-tinged sputum), **digital clubbing**, and recent respiratory infection suggests bronchiectasis. The chest X-ray finding of **tram-track opacities** is highly characteristic of this condition, indicating bronchial wall thickening and dilation. The history of stroke placing him at risk for aspiration, and prior smoking also contribute to the risk of chronic lung damage.
- **Bronchiectasis** is defined by **permanent dilation of the bronchi** due to chronic inflammation and infection, leading to impaired mucociliary clearance and recurrent infections. The description perfectly fits the clinical and radiological picture.
*Aspiration pneumonia*
- While the patient's history of **stroke** increases his risk for **aspiration**, the chronic nature of his symptoms (long-standing productive cough worsening since stroke) and the presence of **digital clubbing** are less consistent with acute aspiration pneumonia.
- **Aspiration pneumonia** typically presents as an acute illness with fever and cough, and while it could explain some symptoms, it doesn't fully account for the chronic changes (clubbing, tram-track opacities).
*Pulmonary embolism*
- **Pulmonary embolism** usually presents with **acute onset dyspnea** and **pleuritic chest pain**, often without a history of chronic productive cough or digital clubbing. Hemoptysis can occur but is not typically copious and is associated with infarction.
- The chest X-ray findings of **increased translucency** and **tram-track opacities** are not characteristic of pulmonary embolism, which might show an area of opacification (Westermark sign, Hampton hump) or be normal.
*Lung cancer*
- While **lung cancer** can cause cough, hemoptysis, and shortness of breath, and the patient's smoking history is a risk factor, the description of **tram-track opacities** on chest X-ray is not characteristic of lung cancer. **Digital clubbing** can be seen, but the chronic productive cough for years is more indicative of a chronic inflammatory process.
- The typical X-ray findings for lung cancer would be a **mass lesion**, nodule, or atelectasis, not diffuse bronchial wall thickening.
*Emphysema*
- **Emphysema** is characterized by **shortness of breath** and a **chronic cough**, often related to a smoking history, and the X-ray might show **increased translucency** due to hyperinflation. However, copious **blood-tinged sputum** and **digital clubbing** are not typical features of emphysema.
- The classic X-ray finding for emphysema is **hyperinflation** with flattened diaphragms, and while increased translucency is mentioned, **tram-track opacities** are not seen; these indicate bronchial wall thickening, not alveolar destruction.
Biofilms in chronic infections US Medical PG Question 10: A 46-year-old Caucasian female presents with cold intolerance, weight gain, and constipation. She has also noticed that her nails have become thinner recently but denies any fever or neck pain. Which of the following is NOT an expected histological finding in the thyroid?
- A. Hurthle cells
- B. Lymphocytic infiltration
- C. Multinucleate giant cells (Correct Answer)
- D. Several germinal centers
- E. Fibrosis
Biofilms in chronic infections Explanation: ***Multinucleate giant cells***
- The patient's symptoms (cold intolerance, weight gain, constipation, thin nails) are highly suggestive of **hypothyroidism**, most commonly caused by **Hashimoto's thyroiditis**.
- **Multinucleate giant cells** are typically associated with **subacute granulomatous (de Quervain's) thyroiditis**, which presents with painful thyroid enlargement and a biphasic course (transient hyperthyroidism followed by hypothyroidism).
*Hurthle cells*
- These are **eosinophilic, granular follicular cells** that represent metaplastic changes within the thyroid.
- They are a common histological finding in **Hashimoto's thyroiditis**, often seen alongside chronic inflammation.
*Lymphocytic infiltration*
- This is a hallmark feature of **Hashimoto's thyroiditis**, characterized by extensive infiltration of the thyroid parenchyma by **lymphocytes**, plasma cells, and macrophages.
- The immune response targets thyroid peroxidases and thyroglobulin, leading to gradual destruction of thyroid follicles.
*Several germinal centers*
- The presence of **germinal centers** within the thyroid is a characteristic histopathological feature of **Hashimoto's thyroiditis**.
- These centers indicate active B-cell proliferation and are part of the autoimmune process in the gland.
*Fibrosis*
- Over time, chronic inflammation in **Hashimoto's thyroiditis** often leads to **fibrosis** within the thyroid gland.
- Extensive fibrosis can result in a firm, enlarged thyroid and contribute to impaired thyroid function.
More Biofilms in chronic infections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.