Biofilm disruption strategies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Biofilm disruption strategies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Biofilm disruption strategies US Medical PG Question 1: A 54-year-old woman comes to the physician because of lower back pain, night sweats, and a 5-kg (11-lb) weight loss during the past 4 weeks. She has rheumatoid arthritis treated with adalimumab. Her temperature is 38°C (100.4°F). Physical examination shows tenderness over the T10 and L1 spinous processes. Passive extension of the right hip causes pain in the right lower quadrant. The patient's symptoms are most likely caused by an organism with which of the following virulence factors?
- A. Proteins that bind to the Fc region of immunoglobulin G
- B. Protease that cleaves immunoglobulin A
- C. Polysaccharide capsule that prevents phagocytosis
- D. Surface glycolipids that prevent phagolysosome fusion (Correct Answer)
- E. Polypeptides that inactivate elongation factor 2
Biofilm disruption strategies Explanation: ***Surface glycolipids that prevent phagolysosome fusion***
- The patient's symptoms (low back pain, night sweats, weight loss, fever, spinal tenderness, and hip pain) in a patient on **adalimumab** (a TNF-alpha inhibitor) suggest **disseminated tuberculosis** (Pott disease).
- *Mycobacterium tuberculosis* uses **mycolic acids** and other surface glycolipids to prevent phagolysosome fusion, allowing it to survive and replicate within macrophages.
*Proteins that bind to the Fc region of immunoglobulin G*
- This virulence factor is characteristic of bacteria like *Staphylococcus aureus* (Protein A) and *Streptococcus pyogenes* (Protein G), which is not consistent with the clinical picture.
- These proteins interfere with opsonization and antibody-mediated immunity, but are not the primary mechanism of *Mycobacterium tuberculosis* survival within macrophages.
*Protease that cleaves immunoglobulin A*
- **IgA protease** is a virulence factor for bacteria such as *Neisseria gonorrhoeae*, *Neisseria meningitidis*, and *Streptococcus pneumoniae*, which colonize mucosal surfaces.
- This mechanism helps these bacteria evade mucosal immunity, but it is not relevant to the pathogenesis of tuberculosis.
*Polysaccharide capsule that prevents phagocytosis*
- A polysaccharide capsule is a major virulence factor for many encapsulated bacteria (e.g., *Streptococcus pneumoniae*, *Haemophilus influenzae*, *Neisseria meningitidis*) that helps them evade phagocytosis.
- However, *Mycobacterium tuberculosis* is not primarily characterized by a polysaccharide capsule for immune evasion; its internal survival within macrophages is more critical.
*Polypeptides that inactivate elongation factor 2*
- Toxins that inactivate **elongation factor 2** are associated with *Corynebacterium diphtheriae* (**diphtheria toxin**) and *Pseudomonas aeruginosa* (**exotoxin A**), leading to inhibition of protein synthesis.
- This mechanism is not involved in the pathogenesis of *Mycobacterium tuberculosis* infection or its ability to cause disseminated disease.
Biofilm disruption strategies US Medical PG Question 2: A 68-year-old man comes to the physician because of headache, fatigue, and nonproductive cough for 1 week. He appears pale. Pulmonary examination shows no abnormalities. Laboratory studies show a hemoglobin concentration of 9.5 g/dL and an elevated serum lactate dehydrogenase concentration. A peripheral blood smear shows normal red blood cells that are clumped together. Results of cold agglutinin titer testing show a 4-fold elevation above normal. An x-ray of the chest shows diffuse, patchy infiltrates bilaterally. Treatment is begun with an antibiotic that is also used to promote gut motility. Which of the following is the primary mechanism of action of this drug?
- A. Inhibition of bacterial RNA polymerase
- B. Inhibition of folic acid synthesis
- C. Free radical creation within bacterial cells
- D. Inhibition of transpeptidase cross-linking at the cell wall
- E. Inhibition of peptide translocation at the 50S ribosomal subunit (Correct Answer)
Biofilm disruption strategies Explanation: ***Inhibition of peptide translocation at the 50S ribosomal subunit***
- This drug described is likely **erythromycin** or another **macrolide antibiotic**, which inhibits bacterial protein synthesis by binding to the **50S ribosomal subunit** and preventing translocation.
- Macrolides are used to treat **atypical pneumonia** caused by *Mycoplasma pneumoniae*, which is indicated by the patient's symptoms (headache, fatigue, nonproductive cough, bilateral patchy infiltrates) and **cold agglutinin disease**.
*Inhibition of bacterial RNA polymerase*
- This is the mechanism of action of **rifampin**, which is primarily used for **tuberculosis** and **meningitis prophylaxis**, not for atypical pneumonia.
- Rifampin's side effects and spectrum of activity do not align with the implied clinical scenario, especially the gut motility promotion.
*Inhibition of folic acid synthesis*
- This is the mechanism for **sulfonamides** and **trimethoprim**, which are bacteriostatic and target different pathogens than those causing cold agglutinin positive pneumonia.
- These drugs are not known for promoting gut motility.
*Free radical creation within bacterial cells*
- This mechanism is characteristic of **metronidazole**, an antibiotic used for anaerobic bacterial and parasitic infections.
- Metronidazole does not fit the clinical context of atypical pneumonia with cold agglutinins, nor is it a macrolide that promotes gut motility.
*Inhibition of transpeptidase cross-linking at the cell wall*
- This describes the mechanism of **beta-lactam antibiotics** (e.g., penicillins, cephalosporins), which are ineffective against **atypical pneumonia** because *Mycoplasma* lacks a cell wall.
- Beta-lactams do not typically promote gut motility.
Biofilm disruption strategies US Medical PG Question 3: An investigator is studying the chemical structure of antibiotics and its effect on bacterial growth. He has synthesized a simple beta-lactam antibiotic and has added a bulky side chain to the molecule that inhibits the access of bacterial enzymes to the beta-lactam ring. The synthesized drug will most likely be appropriate for the treatment of which of the following conditions?
- A. Folliculitis (Correct Answer)
- B. Nocardiosis
- C. Atypical pneumonia
- D. Erythema migrans
- E. Otitis media
Biofilm disruption strategies Explanation: ***Folliculitis***
- The bulky side chain provides **steric hindrance** that prevents **staphylococcal beta-lactamases** from accessing and degrading the **beta-lactam ring**.
- This modification creates an **anti-staphylococcal penicillin** (similar to methicillin, nafcillin, or oxacillin), which is effective against **methicillin-sensitive *Staphylococcus aureus* (MSSA)**.
- **Folliculitis** is most commonly caused by *S. aureus*, making this modified beta-lactam an appropriate treatment choice for MSSA-related folliculitis.
- The bulky side chain specifically protects against the **penicillinase** (beta-lactamase) produced by staphylococci.
*Otitis media*
- Otitis media is commonly caused by beta-lactamase-producing organisms like *Haemophilus influenzae* and *Moraxella catarrhalis*.
- However, the beta-lactamases produced by these gram-negative organisms are **not inhibited by bulky side chains** alone.
- Treatment of beta-lactamase-producing *H. influenzae* and *M. catarrhalis* requires **beta-lactamase inhibitors** (such as clavulanic acid combined with amoxicillin), not steric hindrance.
- The mechanism of protection differs: beta-lactamase inhibitors **suicide inhibitors** that bind to the enzyme, whereas bulky side chains provide **physical blocking**.
*Nocardiosis*
- Nocardiosis is caused by *Nocardia* species, which are **aerobic actinomycetes**.
- These bacteria are typically treated with **sulfonamides** (trimethoprim-sulfamethoxazole) for prolonged periods.
- Beta-lactam antibiotics are generally not first-line treatment, as *Nocardia* species often show intrinsic resistance or require specific antibiotic combinations.
*Atypical pneumonia*
- Atypical pneumonia is caused by organisms like *Mycoplasma pneumoniae*, *Chlamydophila pneumoniae*, and *Legionella pneumophila*.
- These organisms lack a **peptidoglycan cell wall**, which is the target of all **beta-lactam antibiotics**.
- Beta-lactams (regardless of modifications) are completely ineffective against atypical pneumonia pathogens.
- Treatment requires **macrolides** (azithromycin), **tetracyclines** (doxycycline), or **fluoroquinolones**.
*Erythema migrans*
- Erythema migrans is the characteristic rash of early **Lyme disease**, caused by *Borrelia burgdorferi*.
- While *Borrelia* is sensitive to certain beta-lactam antibiotics (amoxicillin, ceftriaxone), it does **not produce beta-lactamases**.
- The bulky side chain modification is unnecessary for treating *Borreria* infections, as there is no beta-lactamase to protect against.
- Standard treatment uses doxycycline, amoxicillin, or ceftriaxone—not anti-staphylococcal penicillins.
Biofilm disruption strategies US Medical PG Question 4: A scientist is studying the mechanisms by which bacteria become resistant to antibiotics. She begins by obtaining a culture of vancomycin-resistant Enterococcus faecalis and conducts replicate plating experiments. In these experiments, colonies are inoculated onto a membrane and smeared on 2 separate plates, 1 containing vancomycin and the other with no antibiotics. She finds that all of the bacterial colonies are vancomycin resistant because they grow on both plates. She then maintains the bacteria in liquid culture without vancomycin while she performs her other studies. Fifteen generations of bacteria later, she conducts replicate plating experiments again and finds that 20% of the colonies are now sensitive to vancomycin. Which of the following mechanisms is the most likely explanation for why these colonies have become vancomycin sensitive?
- A. Point mutation
- B. Gain of function mutation
- C. Viral infection
- D. Plasmid loss (Correct Answer)
- E. Loss of function mutation
Biofilm disruption strategies Explanation: ***Plasmid loss***
- The initial **vancomycin resistance** in *Enterococcus faecalis* is often mediated by genes located on **plasmids**, which are extrachromosomal DNA.
- In the absence of selective pressure (vancomycin), bacteria that lose the plasmid (and thus the resistance genes) have a **growth advantage** over those that retain the energetically costly plasmid, leading to an increase in sensitive colonies over generations.
*Point mutation*
- A **point mutation** typically involves a change in a single nucleotide and could lead to loss of resistance if it occurred in a gene conferring resistance.
- However, since there was no selective pressure for loss of resistance, it is less likely that 20% of the population would acquire such a specific point mutation to revert resistance.
*Gain of function mutation*
- A **gain of function mutation** would imply that the bacteria acquired a *new* advantageous trait, not the *loss* of resistance.
- This type of mutation would not explain why some colonies became sensitive to vancomycin after the drug was removed.
*Viral infection*
- **Viral infection** (bacteriophages) can transfer genes through transduction or cause bacterial lysis, but it's not the primary mechanism for a widespread reversion of resistance in the absence of antibiotic pressure.
- It would not explain the observed increase in vancomycin-sensitive colonies due to evolutionary pressure.
*Loss of function mutation*
- While a **loss of function mutation** in a gene conferring resistance could lead to sensitivity, it's generally less likely to explain a 20% shift without selective pressure than **plasmid loss**.
- Plasmids are often unstable and are easily lost in the absence of selection, whereas a specific gene mutation causing loss of function would need to arise and become prevalent in the population.
Biofilm disruption strategies US Medical PG Question 5: A 65-year-old woman undergoes an abdominal hysterectomy. She develops pain and discharge at the incision site on the fourth postoperative day. The past medical history is significant for diabetes of 12 years duration, which is well-controlled on insulin. Pus from the incision site is sent for culture on MacConkey agar, which shows white-colorless colonies. On blood agar, the colonies were green. Biochemical tests reveal an oxidase-positive organism. Which of the following is the most likely pathogen?
- A. Staphylococcus aureus
- B. Enterococcus faecalis
- C. Streptococcus pyogenes
- D. Pseudomonas aeruginosa (Correct Answer)
- E. Staphylococcus epidermidis
Biofilm disruption strategies Explanation: ***Pseudomonas aeruginosa***
- The combination of **white, colorless colonies on MacConkey agar** (indicating a non-lactose fermenter), **green colonies on blood agar** (due to pigment production), and a **positive oxidase test** is highly characteristic of *Pseudomonas aeruginosa*.
- This organism is a common cause of **nosocomial infections**, particularly in immunocompromised patients (like those with diabetes) and in postoperative wound infections.
*Staphylococcus aureus*
- This bacterium would typically produce **golden-yellow colonies** on blood agar and **no growth on MacConkey agar**.
- It is **oxidase-negative** and a common cause of surgical site infections, but its colonial morphology and biochemical tests do not match the description.
*Enterococcus faecalis*
- This organism is a **Gram-positive coccus** that would not grow well on MacConkey agar and would not produce green colonies on blood agar or be oxidase-positive.
- It is a common cause of urinary tract and wound infections, especially in hospitalized patients.
*Streptococcus pyogenes*
- This is a **beta-hemolytic Streptococcus** that typically produces small, clear colonies with a zone of complete hemolysis on blood agar and would not grow on MacConkey agar.
- It is also **oxidase-negative**, making it inconsistent with the findings.
*Staphylococcus epidermidis*
- This organism forms **white colonies** on blood agar and would not grow on MacConkey agar or produce green pigment.
- It is **coagulase-negative** and **oxidase-negative**, and while it can cause surgical site infections, its colonial characteristics differ.
Biofilm disruption strategies US Medical PG Question 6: While testing various strains of Streptococcus pneumoniae, a researcher discovers that a certain strain of this bacteria is unable to cause disease in mice when deposited in their lungs. What physiological test would most likely deviate from normal in this strain of bacteria as opposed to a typical strain?
- A. Quellung reaction (Correct Answer)
- B. Hemolytic reaction when grown on sheep blood agar
- C. Bile solubility
- D. Optochin sensitivity
- E. Motility
Biofilm disruption strategies Explanation: ***Quellung reaction***
- The **Quellung reaction** tests for the presence of the **polysaccharide capsule**, which is the primary virulence factor of *S. pneumoniae*.
- An **avirulent strain** that cannot cause disease would most likely lack the capsule and show a **negative Quellung reaction** (no capsular swelling), deviating from the **positive reaction** seen in typical encapsulated pathogenic strains.
- The capsule enables *S. pneumoniae* to evade phagocytosis and complement-mediated killing, which is essential for establishing infection in the lungs.
*Hemolytic reaction when grown on sheep blood agar*
- Both virulent and avirulent strains of *S. pneumoniae* typically exhibit **alpha-hemolysis** (partial hemolysis, producing a greenish discoloration) on sheep blood agar due to the production of pneumolysin.
- This characteristic does not differentiate between pathogenic and non-pathogenic strains in terms of disease-causing ability.
*Bile solubility*
- *S. pneumoniae* is characteristically **bile-soluble** due to the presence of autolysin enzymes that are activated by bile salts, leading to cellular lysis.
- This property is a **species characteristic** present in both virulent and avirulent strains, thus it would not explain the inability to cause disease.
*Optochin sensitivity*
- *S. pneumoniae* is universally **sensitive to optochin**, a chemical agent that inhibits its growth and is used for laboratory identification.
- This characteristic is used for **species identification** but does not correlate with strain virulence or disease-causing ability.
*Motility*
- *Streptococcus pneumoniae* is a **non-motile** bacterium; it lacks flagella.
- This characteristic is consistent across all strains and is not a virulence factor for this species.
Biofilm disruption strategies US Medical PG Question 7: An investigator is studying a strain of bacteria that retains a blue color after crystal violet dye and acetone are applied. The bacteria are inoculated in a petri dish containing hypotonic saline. After the addition of an antibiotic, the bacteria swell and rupture. This antibiotic most likely belongs to which of the following classes?
- A. Macrolide
- B. Cephalosporin (Correct Answer)
- C. Sulfonamide
- D. Fluoroquinolone
- E. Tetracycline
Biofilm disruption strategies Explanation: ***Cephalosporin***
- This scenario describes a **Gram-positive bacterium** (retains blue color) which, after antibiotic treatment, swells and lyses in a hypotonic solution. This indicates a defect in the **peptidoglycan cell wall**.
- **Cephalosporins** are **β-lactam antibiotics** that inhibit bacterial cell wall synthesis by interfering with **peptidoglycan cross-linking**, leading to osmotic lysis in hypotonic environments.
*Macrolide*
- Macrolides like **azithromycin** and **erythromycin** inhibit bacterial **protein synthesis** by binding to the 50S ribosomal subunit.
- They do not directly target the cell wall, so they would not cause immediate osmotic lysis in this manner.
*Sulfonamide*
- Sulfonamides inhibit bacterial **folic acid synthesis** by acting as a competitive inhibitor of dihydropteroate synthase, disrupting DNA and RNA production.
- Their mechanism of action does not involve direct cell wall disruption or osmotic lysis.
*Fluoroquinolone*
- Fluoroquinolones interfere with bacterial **DNA replication and transcription** by inhibiting **DNA gyrase** and **topoisomerase IV**.
- This class of antibiotics does not primarily target the cell wall, and therefore would not lead to prompt osmotic swelling and rupture.
*Tetracycline*
- Tetracyclines inhibit bacterial **protein synthesis** by binding to the 30S ribosomal subunit, preventing the attachment of aminoacyl-tRNA.
- They do not affect the cell wall, so they would not cause the observed osmotic lysis.
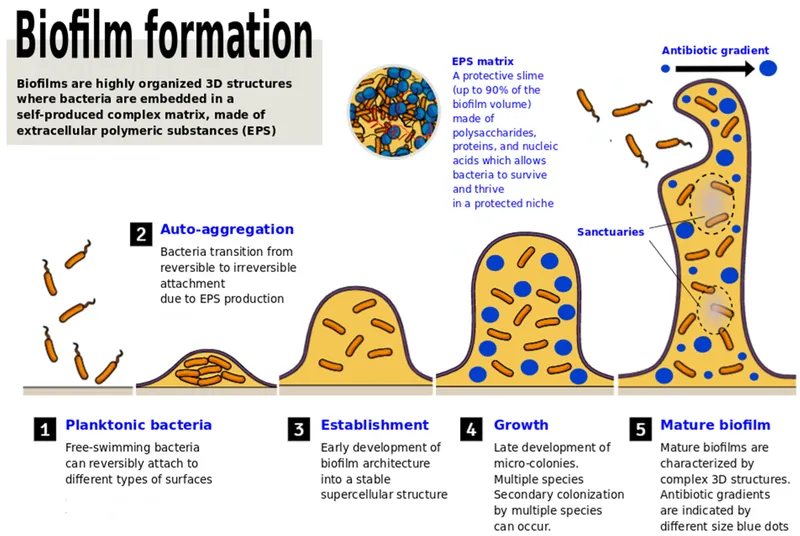
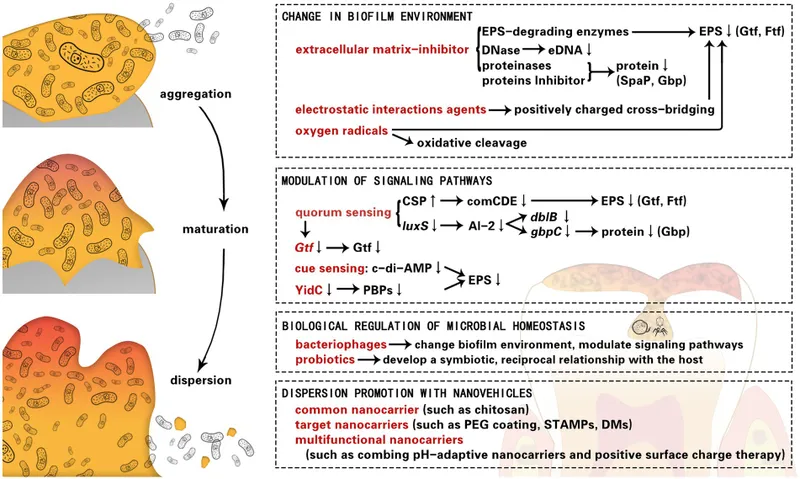
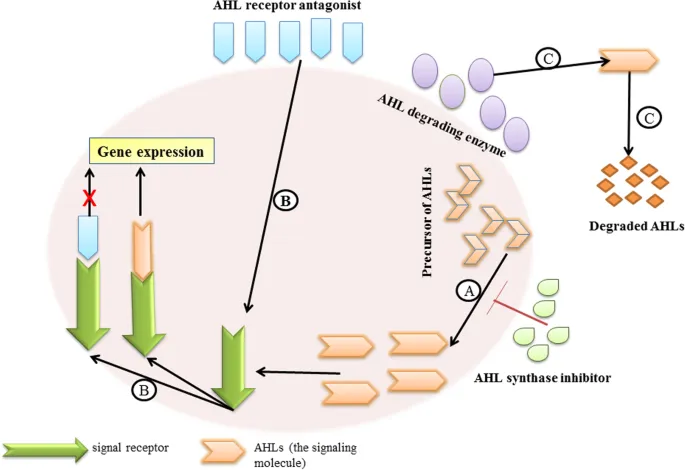
Biofilm disruption strategies US Medical PG Question 8: A hospital implements silver-coated central venous catheters to reduce catheter-related bloodstream infections. Initial results show 60% reduction in infections at 1 week, but this benefit decreases to 20% reduction by 4 weeks. Electron microscopy of explanted catheters shows biofilm formation with embedded bacteria despite the silver coating. What mechanism best explains the loss of antimicrobial efficacy over time?
- A. Depletion of silver ions from the catheter surface through diffusion
- B. Matrix proteins binding silver ions and reducing bioavailability
- C. Development of silver-tolerant persister cell populations
- D. Bacterial mutation conferring genetic resistance to silver ions
- E. Host protein deposition creating a conditioning film blocking silver release (Correct Answer)
Biofilm disruption strategies Explanation: ***Host protein deposition creating a conditioning film blocking silver release***
- Rapid adsorption of host proteins like **fibrinogen, fibronectin, and albumin** creates a **conditioning film** that physically masks the antimicrobial surface.
- This protein layer acts as a barrier to **ion release** and provides a scaffold for **bacterial adhesion**, facilitating the transition to a long-term **biofilm** state.
*Depletion of silver ions from the catheter surface through diffusion*
- Modern antimicrobial catheters are designed for **sustained release**, and the presence of silver on explanted microscopy suggests the reservoir is not yet empty.
- If diffusion were the only factor, efficacy would decline linearly rather than being linked to the physical observation of **biofilm formation** over the coating.
*Matrix proteins binding silver ions and reducing bioavailability*
- While some binding may occur, this is not the primary mechanism of clinical failure; the principal issue is the physical **obstruction of the surface**.
- This theory does not account for how bacteria are able to initially colonize and survive in **close physical contact** with the coated surface.
*Development of silver-tolerant persister cell populations*
- **Persister cells** are phenotypically dormant and survive antibiotics, but they do not typically cause the gradual, large-scale reduction in antimicrobial device efficacy seen here.
- The microscopy findings emphasize **structural biofilm layers** rather than a specific metabolic state of individual bacteria.
*Bacterial mutation conferring genetic resistance to silver ions*
- True **genetic resistance** to silver (via sil operons) is clinically rare and usually occurs through **efflux pumps**, not biofilm-mediated shielding.
- The scenario describes a loss of efficacy common across multiple hospital settings, whereas **mutational resistance** would be more sporadic or localized.
Biofilm disruption strategies US Medical PG Question 9: A 28-year-old woman with cystic fibrosis undergoes lung transplantation. Pre-transplant sputum cultures show mucoid Pseudomonas aeruginosa. Post-transplant, she receives immunosuppression and antibiotic prophylaxis. Six months later, she develops pneumonia, and cultures grow non-mucoid P. aeruginosa with identical genetic fingerprint to pre-transplant isolates. What evolutionary adaptation most likely explains this phenotypic reversion?
- A. Horizontal gene transfer from colonizing respiratory flora
- B. Decreased selective pressure for biofilm formation in absence of mucus obstruction (Correct Answer)
- C. Selection pressure favoring planktonic phenotype in immunosuppressed state
- D. Loss of mucA mutations due to genetic reversion in new host environment
- E. Antibiotic prophylaxis eliminating mucoid variants selectively
Biofilm disruption strategies Explanation: ***Decreased selective pressure for biofilm formation in absence of mucus obstruction***
- In the **Cystic Fibrosis (CF)** lung, the presence of thick **mucus plugs** and chronic inflammation exerts selective pressure that favors the **mucoid phenotype** (alginate production) for survival.
- Following **lung transplantation**, the new lungs lack the original CF environment, causing the bacteria to revert to a **non-mucoid** state which is more energetically efficient for **planktonic growth** and rapid replication.
*Horizontal gene transfer from colonizing respiratory flora*
- Genetic identity via **fingerprinting** confirms the post-transplant isolate is a direct descendant of the original strain, not a result of **recombination** with other flora.
- The change in phenotype is an **adaptive response** to environmental shifts rather than the acquisition of new genetic material from the host microbiome.
*Selection pressure favoring planktonic phenotype in immunosuppressed state*
- While **immunosuppression** affects the host's ability to clear infections, it is the **structural change** (removal of mucus) that primarily influences the bacterial transition from biofilm to planktonic form.
- Biofilms are generally more resistant to the host immune system; thus, a lack of immunity would not logically drive the bacteria *away* from a protective **biofilm phenotype**.
*Loss of mucA mutations due to genetic reversion in new host environment*
- The **mucoid phenotype** in CF is often caused by **mucA mutations**, but spontaneous **back-mutations** (genetic reversion) are extremely rare in large bacterial populations.
- Phenotypic changes are more likely due to **compensatory mutations** or changes in **gene expression** rather than a literal restoration of the wild-type DNA sequence.
*Antibiotic prophylaxis eliminating mucoid variants selectively*
- **Mucoid variants** and their associated **biofilms** typically show *increased* resistance to antibiotics compared to non-mucoid forms.
- Therefore, **antibiotic prophylaxis** would be expected to select *for* mucoid variants rather than eliminating them to favor non-mucoid ones.
Biofilm disruption strategies US Medical PG Question 10: A clinical trial evaluates a new combination therapy for prosthetic joint infections: standard antibiotics plus an agent that degrades extracellular DNA (DNase). The DNase group shows 40% better cure rates without device removal compared to antibiotics alone. What is the most likely mechanism by which extracellular DNA contributes to biofilm antibiotic resistance?
- A. eDNA activates horizontal gene transfer of resistance plasmids
- B. eDNA triggers host inflammatory responses that damage surrounding tissue
- C. eDNA chelates magnesium ions required for antibiotic activity
- D. eDNA serves as a nutrient source sustaining bacterial metabolism during stress
- E. eDNA binds aminoglycosides through electrostatic interactions, sequestering antibiotics (Correct Answer)
Biofilm disruption strategies Explanation: ***eDNA binds aminoglycosides through electrostatic interactions, sequestering antibiotics***
- **Extracellular DNA (eDNA)** has a negatively charged **phosphate backbone** that binds to and sequesters **positively charged** antibiotics like **aminoglycosides**.
- This physical sequestration effectively reduces the concentration of active drug reaching the bacterial cells within the **biofilm matrix**.
*eDNA activates horizontal gene transfer of resistance plasmids*
- While eDNA can facilitate **transformation**, the primary mechanism of immediate **biofilm resistance** in clinical settings is structural sequestration rather than new gene acquisition.
- **Plasmids** are typically transferred via **conjugation**, which relies on cell-to-cell contact rather than free eDNA in the matrix.
*eDNA triggers host inflammatory responses that damage surrounding tissue*
- Host damage from inflammation contributes to **chronic infection**, but it does not directly explain why **DNase** improves antibiotic efficacy against the bacteria.
- DNA can act as a **DAMP** (Damage Associated Molecular Pattern), but this mechanism does not account for the **antibiotic resistance** observed in biofilms.
*eDNA chelates magnesium ions required for antibiotic activity*
- Although eDNA can bind **divalent cations**, there is no major antibiotic class used for prosthetic joint infections that requires **magnesium** for its intrinsic bactericidal activity.
- **Chelation** of ions primarily influences biofilm **structural stability** or membrane integrity rather than direct antibiotic neutralization.
*eDNA serves as a nutrient source sustaining bacterial metabolism during stress*
- Bacteria can utilize nucleotides, but the **structural and protective** role of eDNA in the **extracellular polymeric substance (EPS)** outweighs its role as a carbon source.
- Reducing nutrient availability would likely slow growth rather than dramatically increasing **antibiotic susceptibility** in the short term.
More Biofilm disruption strategies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.