Zoonotic bacterial infections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Zoonotic bacterial infections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Zoonotic bacterial infections US Medical PG Question 1: A 50-year-old woman returns from a family trip to the Caribbean with three days of fever, watery diarrhea, and vomiting. She states that she tried to avoid uncooked food and unpeeled fruits on her vacation. Of note, her grandson had caught a cold from daycare prior to the trip, and she had been in close contact with the infant throughout the trip. She denies rhinorrhea or coughing. On exam, her temperature is 99.1°F (37.3°C), blood pressure is 110/68 mmHg, pulse is 113/min, and respirations are 12/min. Her stool culture is negative for bacteria. Which of the following describes the most likely cause?
- A. Linear dsRNA virus
- B. ssDNA virus
- C. Linear dsDNA virus
- D. (+) ssRNA virus (Correct Answer)
- E. (-) ssRNA virus
Zoonotic bacterial infections Explanation: ***(+) ssRNA virus***
- The symptoms of **fever, watery diarrhea, and vomiting** following a trip to the Caribbean, especially with contact with a child from daycare, are highly suggestive of a **norovirus infection**.
- **Norovirus** is a **non-enveloped positive-sense single-stranded RNA virus** (+ssRNA) that is a leading cause of acute gastroenteritis outbreaks worldwide.
*Linear dsRNA virus*
- **Rotavirus** is a common cause of gastroenteritis, particularly in children, and is a **segmented double-stranded RNA (dsRNA) virus**, not linear.
- However, the patient's exposure was more typical for **norovirus**, and rotavirus typically presents with more severe dehydration in young children.
*ssDNA virus*
- **Single-stranded DNA viruses (ssDNA)** like **parvovirus** cause various infections, but are not a common cause of acute gastroenteritis in this clinical context.
- **Parvovirus B19** causes Fifth disease, while other parvoviruses can cause canine or feline enteritis, but not typically human acute watery diarrhea.
*Linear dsDNA virus*
- **Double-stranded DNA (dsDNA) viruses**, such as **adenovirus**, can cause gastroenteritis, but it typically presents with more protracted diarrhea and often respiratory symptoms.
- The rapid onset of watery diarrhea and vomiting, along with the exposure history, is less classic for adenovirus.
*(-) ssRNA virus*
- **Negative-sense single-stranded RNA viruses ((-) ssRNA)** include viruses like **influenza virus** and **measles virus**, which cause respiratory infections or rashes, not primarily acute gastroenteritis with watery diarrhea.
- While some (-) ssRNA viruses like **Ebola** can cause gastrointestinal symptoms, the overall clinical picture and travel history do not align with such severe infections.
Zoonotic bacterial infections US Medical PG Question 2: A 65-year-old man presents to the emergency department with a complaint of intense pain in his right foot for the past month, along with fever and chills. He denies any traumatic injury to his foot in recent memory. He has a medical history of poorly-controlled type II diabetes and is a former smoker with extensive peripheral vascular disease. On physical exam, the area of his right foot around the hallux is swollen, erythematous, tender to light palpation, and reveals exposed bone. Labs are notable for elevated C-reactive protein and erythrocyte sedimentation rate. The physician obtains a biopsy for culture. What is the most likely causative organism for this patient’s condition?
- A. Pasteurella multocida
- B. Mycobacterium tuberculosis
- C. Staphylococcus aureus (Correct Answer)
- D. Pseudomonas aeruginosa
- E. Neisseria gonorrhoeae
Zoonotic bacterial infections Explanation: ***Staphylococcus aureus***
- This patient presents with signs of **osteomyelitis** (foot pain, fever, chills, exposed bone, elevated inflammatory markers) in the setting of **diabetes** and **peripheral vascular disease (PVD)**.
- **_S. aureus_** is the most common cause of osteomyelitis, especially in patients with diabetes and PVD where skin integrity is compromised or there's hematogenous spread.
*Pasteurella multocida*
- **_Pasteurella multocida_** is typically associated with infections following **animal bites**, specifically cat or dog bites.
- There is no history of animal bite in this patient, making this organism less likely.
*Mycobacterium tuberculosis*
- **_Mycobacterium tuberculosis_** can cause osteomyelitis, known as **Pott's disease** when affecting the spine, but it's typically a **chronic, granulomatous infection** often without acute purulence or the rapid progression seen here.
- It usually occurs in patients with active tuberculosis elsewhere or those from endemic regions, and the clinical presentation is not as acute as described.
*Pseudomonas aeruginosa*
- **_Pseudomonas aeruginosa_** is a common cause of osteomyelitis in specific contexts, such as **puncture wounds** through footwear (especially in diabetic patients) or in **IV drug users**.
- While possible in diabetic foot infections, **_S. aureus_** remains overwhelmingly more common given the general presentation of osteomyelitis without a specific puncture wound history.
*Neisseria gonorrhoeae*
- **_Neisseria gonorrhoeae_** causes **gonococcal arthritis** or disseminated gonococcal infection, which can affect joints.
- However, it typically presents with migratory polyarthralgia, tenosynovitis, or dermatitis, rather than localized acute osteomyelitis with exposed bone in the foot as described.
Zoonotic bacterial infections US Medical PG Question 3: An investigator is studying the growth of an organism in different media. The organism is inoculated on a petri dish that contains heated sheep blood, vancomycin, nystatin, trimethoprim, and colistin. The resulting growth medium is incubated at 37°C. Numerous small, white colonies are seen after incubation for 48 hours. This organism is most likely to cause which of the following conditions?
- A. Pontiac fever
- B. Pseudomembranous colitis
- C. Hemolytic uremic syndrome
- D. Oral thrush
- E. Gonorrhea (Correct Answer)
Zoonotic bacterial infections Explanation: ***Gonorrhea***
- The growth medium described is **Thayer-Martin agar**, a selective medium containing **heated sheep blood** (supplies NAD+), **vancomycin** (inhibits Gram-positives), **colistin** (inhibits Gram-negatives), **nystatin** (inhibits fungi), and **trimethoprim** (inhibits Proteus). This medium is specifically designed for the isolation of *Neisseria gonorrhoeae* from polymicrobial samples.
- *Neisseria gonorrhoeae* typically grows as **small, translucent-to-white colonies** on selective media like Thayer-Martin agar, and incubation at 37°C in CO2 (not explicitly mentioned but often required) for 24-48 hours yields visible growth, causing **gonorrhea**.
*Pontiac fever*
- Pontiac fever is a mild, self-limiting form of **legionellosis**, caused by *Legionella pneumophila*.
- *Legionella* requires a specialized medium such as **buffered charcoal yeast extract (BCYE) agar** for growth, not Thayer-Martin agar.
*Pseudomembranous colitis*
- This condition is caused by **toxin-producing *Clostridioides difficile***, often after antibiotic use.
- *C. difficile* is an obligate anaerobe and requires **anaerobic conditions** and specific selective media (e.g., CCFA agar) for isolation, not Thayer-Martin agar under aerobic conditions.
*Hemolytic uremic syndrome*
- Hemolytic uremic syndrome (HUS) is often caused by **Shiga toxin-producing *Escherichia coli* (STEC)**, particularly O157:H7.
- STEC can be isolated on media like **sorbitol MacConkey agar (SMAC)**, where O157:H7 appears as non-sorbitol fermenting colonies, distinct from the growth seen on Thayer-Martin.
*Oral thrush*
- Oral thrush is caused by *Candida albicans*, a yeast.
- *Candida* would be inhibited by **nystatin** in the Thayer-Martin medium, which is an antifungal agent.
Zoonotic bacterial infections US Medical PG Question 4: A 21-year-old man comes to the physician's office due to a 3-week history of fatigue and a rash, along with the recent development of joint pain that has moved from his knee to his elbows. The patient reports going camping last month but denies having been bitten by a tick. His past medical history is significant for asthma treated with an albuterol inhaler. His pulse is 54/min and blood pressure is 110/72. Physical examination reveals multiple circular red rings with central clearings on the right arm and chest. There is a normal range of motion in all joints and 5/5 strength bilaterally in the upper and lower extremities. Without proper treatment, the patient is at highest risk for which of the following complications?
- A. Liver capsule inflammation
- B. Bone marrow failure
- C. Heart valve stenosis
- D. Glomerular damage
- E. Cranial nerve palsy (Correct Answer)
Zoonotic bacterial infections Explanation: ***Cranial nerve palsy***
- This patient presents with classic **Lyme disease** (caused by *Borrelia burgdorferi*), including camping exposure, fatigue, migratory arthralgia, and **erythema migrans** (multiple circular red rings with central clearings on the arm and chest).
- The **bradycardia (pulse 54/min)** suggests early **Lyme carditis** with possible first-degree AV block, which typically resolves with treatment and rarely progresses to complete heart block in treated cases.
- Without proper antibiotic treatment, **cranial neuropathy** is one of the most common neurological complications in early disseminated Lyme disease, with **facial nerve palsy (Bell's palsy)** being the most frequent, occurring in up to 10% of untreated patients.
- Other neurological complications include meningitis, radiculoneuropathy, and peripheral neuropathy, making neurologic involvement a significant risk in untreated disease.
*Liver capsule inflammation*
- **Perihepatitis (Fitz-Hugh-Curtis syndrome)** is associated with **pelvic inflammatory disease (PID)** caused by *Chlamydia trachomatis* or *Neisseria gonorrhoeae*, not Lyme disease.
- This presents with right upper quadrant pain and "violin string" adhesions between the liver capsule and peritoneum.
*Bone marrow failure*
- **Bone marrow failure** (aplastic anemia) can be caused by parvovirus B19, certain medications, radiation, or idiopathic causes, but is **not a recognized complication of Lyme disease**.
- Lyme disease primarily affects the skin, joints, heart (conduction system), and nervous system, not hematopoietic function.
*Heart valve stenosis*
- **Lyme carditis** affects the **cardiac conduction system**, causing **AV blocks** (first, second, or third degree) and myocarditis, as suggested by this patient's bradycardia.
- Lyme does **not cause valvular stenosis or regurgitation**. Valvular disease is associated with rheumatic fever (post-streptococcal), endocarditis, or degenerative changes.
- The cardiac manifestations of Lyme typically resolve with appropriate antibiotic therapy and rarely cause permanent structural damage.
*Glomerular damage*
- **Glomerulonephritis** is not a typical complication of Lyme disease in humans (though "Lyme nephritis" occurs in dogs).
- Renal involvement in human Lyme disease is extremely rare and not a significant clinical concern compared to neurological, cardiac, or rheumatological manifestations.
Zoonotic bacterial infections US Medical PG Question 5: A 50-year-old farmer presents to a physician with painless, black, severely swollen pustules on the left hand. Examination reveals extensive swelling around the wound. Microscopy reveals gram-positive bacilli with a bamboo stick appearance. Culture shows large, gray, non-hemolytic colonies with irregular borders. Which of the following is the most likely diagnosis?
- A. Anthrax (Correct Answer)
- B. Tularemia
- C. Brucellosis
- D. Erysipeloid
- E. Listeriosis
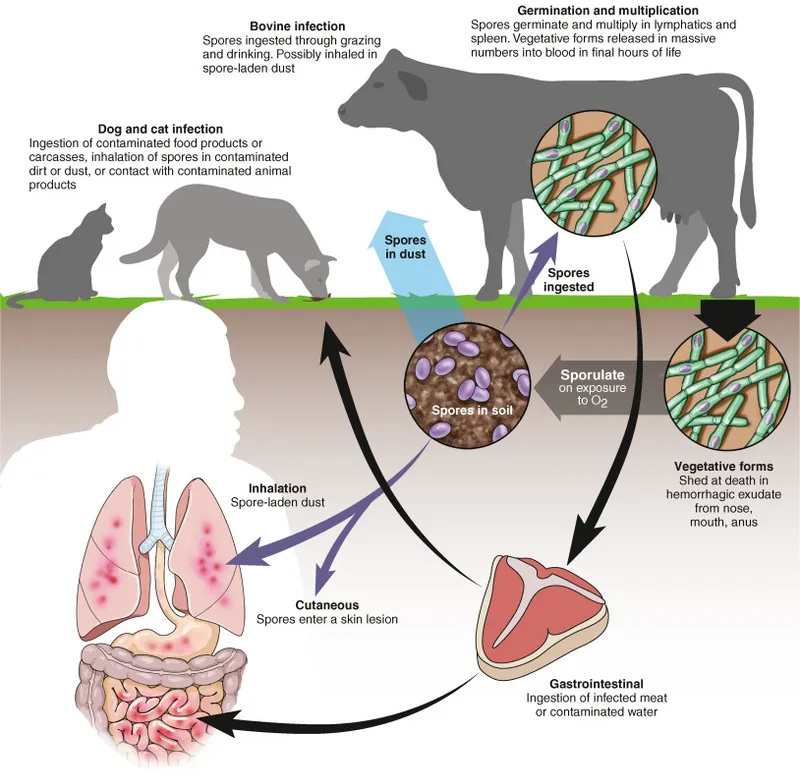
Zoonotic bacterial infections Explanation: ***Anthrax***
- The combination of **painless, black, severely swollen pustules** (eschar and edema) on the hand of a **farmer** is pathognomonic for **cutaneous anthrax**.
- **Gram-positive bacilli with a bamboo stick appearance** and **large, gray, non-hemolytic colonies with irregular borders** on culture are characteristic features of *Bacillus anthracis*.
*Tularemia*
- While tularemia can present with an **ulceroglandular lesion** at the site of inoculation, it is typically accompanied by **highly painful regional lymphadenopathy**.
- The causative agent, *Francisella tularensis*, is a **small, gram-negative coccobacillus**, not a large gram-positive bacillus.
*Brucellosis*
- This zoonotic infection is primarily associated with **fever, sweats, malaise**, and **arthralgia**, often linked to consumption of unpasteurized dairy or contact with infected animals.
- It does not present with characteristic skin lesions like the **black pustules** described, and **Brucella species** are **gram-negative coccobacilli**.
*Erysipeloid*
- Erysipeloid is a skin infection caused by *Erysipelothrix rhusiopathiae*, characterized by a **reddish-purple, elevated migratory lesion with sharply defined borders**, often on the hands or fingers.
- It does not produce **black pustules** or the specific microscopic and cultural features described for *Bacillus anthracis*.
*Listeriosis*
- Listeriosis, caused by *Listeria monocytogenes*, typically presents as **meningitis, sepsis**, or **gastroenteritis**, particularly in immunocompromised individuals, pregnant women, and neonates.
- While *Listeria* is a **gram-positive rod**, it does not cause the distinct skin lesions seen in the patient, nor does it form large, non-hemolytic colonies with irregular borders.
Zoonotic bacterial infections US Medical PG Question 6: Blood cultures are sent to the laboratory and empiric treatment with intravenous vancomycin is started. Blood cultures grow gram-negative bacilli identified as Cardiobacterium hominis. Which of the following is the most appropriate next step in management?
- A. Switch to intravenous gentamicin
- B. Switch to intravenous ampicillin
- C. Switch to intravenous ceftriaxone (Correct Answer)
- D. Switch to intravenous cefazolin
- E. Add intravenous rifampin
Zoonotic bacterial infections Explanation: ***Switch to intravenous ceftriaxone***
- **Cardiobacterium hominis** is part of the **HACEK group** of bacteria, which are known for causing **endocarditis**.
- These organisms are typically susceptible to **beta-lactam antibiotics**, with **third-generation cephalosporins** like ceftriaxone being the drug of choice due to their excellent activity and good penetration.
*Switch to intravenous gentamicin*
- While **aminoglycosides** like gentamicin can be used in combination regimens for serious infections, they are generally **not monotherapy** for HACEK endocarditis and are associated with **nephrotoxicity** and **ototoxicity**.
- The primary treatment for HACEK endocarditis is a **beta-lactam antibiotic**, not an aminoglycoside alone.
*Switch to intravenous ampicillin*
- **Ampicillin** is a beta-lactam, but it may not consistently provide optimal coverage for all HACEK organisms, and some strains may have reduced susceptibility.
- **Third-generation cephalosporins** are preferred due to their broader and more consistent activity against this group.
*Switch to intravenous cefazolin*
- **Cefazolin** is a first-generation cephalosporin and typically has **limited activity** against gram-negative bacilli, especially those like Cardiobacterium hominis which require broader-spectrum beta-lactams.
- Its spectrum of activity is primarily against **gram-positive bacteria** and some **gram-negative cocci**.
*Add intravenous rifampin*
- **Rifampin** is primarily used for **mycobacterial infections** and in combination regimens for specific bacterial infections (e.g., bone and joint infections, prosthetic device infections) often due to resistant staphylococci.
- It is **not a first-line agent** for Cardiobacterium hominis infections and there's no indication for its use here with an organism susceptible to ceftriaxone.
Zoonotic bacterial infections US Medical PG Question 7: A child is brought into the emergency room by her mother. Her mother states that the 7-year-old child was playing with their dog, who is up to date on his vaccinations. When the dog started playing more aggressively, the child suffered a bite on the hand with two puncture wounds from the dog's canines. The child is up-to-date on her vaccinations and has no medical history. Her vitals are within normal limits. If this bite becomes infected, what is the most likely organism to be the cause of infection?
- A. Clostridium tetani
- B. Fusobacterium
- C. Pasteurella multocida (Correct Answer)
- D. Clostridium perfringens
- E. Pseudomonas aeruginosa
Zoonotic bacterial infections Explanation: ***Pasteurella multocida***
- This bacterium is a **common commensal** in the oral cavity of cats and dogs and is the **most frequent cause** of wound infections following animal bites.
- Infections with *Pasteurella multocida* typically present rapidly within **24 hours** with **erythema, swelling, tenderness, and purulent discharge** at the bite site.
*Clostridium tetani*
- This organism causes **tetanus**, characterized by **muscle spasms and lockjaw**, not focal wound infection, and is typically associated with penetrating injuries contaminated with soil.
- The child is stated to be **up-to-date on vaccinations**, making tetanus highly unlikely.
*Fusobacterium*
- *Fusobacterium* species are anaerobic bacteria often found in the oral cavity and can cause polymicrobial infections, but they are **not the primary or most likely organism** in dog bite infections.
- They are more commonly associated with **periodontal disease** and certain severe, invasive infections like Lemierre's syndrome.
*Clostridium perfringens*
- This bacterium is a significant cause of **gas gangrene** (clostridial myonecrosis), which is characterized by rapid tissue necrosis and gas production.
- While it can be associated with contaminated wounds, it is **not the most common pathogen** in dog bites and presents with a more severe, systemic picture.
*Pseudomonas aeruginosa*
- *Pseudomonas aeruginosa* is an opportunistic pathogen often associated with **water contamination**, **hospital-acquired infections**, or infections in immunocompromised individuals.
- It is **not a primary pathogen** in the oral flora of dogs and therefore uncommonly causes dog bite infections.
Zoonotic bacterial infections US Medical PG Question 8: A 24-year-old newly immigrated mother arrives to the clinic to discuss breastfeeding options for her newborn child. Her medical history is unclear as she has recently arrived from Sub-Saharan Africa. You tell her that unfortunately she will not be able to breastfeed until further testing is performed. Which of the following infections is an absolute contraindication to breastfeeding?
- A. Human Immunodeficiency Virus (HIV) (Correct Answer)
- B. Latent tuberculosis
- C. Hepatitis B
- D. Hepatitis C
- E. All of the options
Zoonotic bacterial infections Explanation: ***Human Immunodeficiency Virus (HIV)***
- In developed countries where safe alternatives are available, **HIV-positive mothers** are advised against breastfeeding due to the risk of **vertical transmission** through breast milk.
- This is considered an **absolute contraindication** in settings where formula feeding is accessible and safe.
*Latent tuberculosis*
- **Latent tuberculosis** is not a contraindication to breastfeeding; mothers can breastfeed while receiving treatment.
- Active, untreated tuberculosis, however, generally requires temporary separation of mother and child until the mother is no longer infectious, but pumping and feeding expressed milk is often still an option.
*Hepatitis B*
- **Hepatitis B** infection in the mother is not a contraindication to breastfeeding, especially if the infant receives **hepatitis B vaccine** and **Hepatitis B Immune Globulin (HBIG)** at birth.
- Breastfeeding is considered safe and does not increase the risk of transmission to the infant.
*Hepatitis C*
- **Hepatitis C** is generally **not a contraindication** to breastfeeding, as studies have shown a very low risk of transmission through breast milk.
- Breastfeeding is supported unless the mother has **cracked or bleeding nipples**, which could potentially allow viral transmission.
*All of the options*
- This option is incorrect because **only HIV** is considered an absolute contraindication to breastfeeding in settings where safe alternatives are available.
- Latent TB, Hepatitis B, and Hepatitis C alone do not preclude breastfeeding.
Zoonotic bacterial infections US Medical PG Question 9: A 3-year-old boy is brought to the physician for the evaluation of recurrent skin lesions. The episodes of lesions started at the age of 3 months. He has also had several episodes of respiratory tract infections, enlarged lymph nodes, and recurrent fevers since birth. The boy attends daycare. The patient's immunizations are up-to-date. He is at the 5th percentile for length and 10th percentile for weight. He appears ill. Temperature is 38°C (100.4°F). Examination shows several raised, erythematous lesions of different sizes over the face, neck, groin, and extremities; some are purulent. Bilateral cervical and axillary lymphadenopathy are present. What is the most likely underlying mechanism of this patient's symptoms?
- A. Defective cytoplasmic tyrosine kinase
- B. NADPH oxidase deficiency (Correct Answer)
- C. Impaired signaling to actin cytoskeleton reorganization
- D. Defective neutrophil chemotaxis
- E. Impaired repair of double-strand DNA breaks
Zoonotic bacterial infections Explanation: ***NADPH oxidase deficiency***
- The recurrent skin abscesses (purulent lesions), respiratory tract infections, lymphadenopathy, and fevers point to chronic granulomatous disease (CGD), which is caused by a deficiency in **NADPH oxidase**.
- **NADPH oxidase** is essential for the production of reactive oxygen species (ROS) in phagocytes, which are critical for killing catalase-positive bacteria and fungi.
*Defective cytoplasmic tyrosine kinase*
- This mechanism is associated with **X-linked agammaglobulinemia (Bruton's agammaglobulinemia)**, which primarily causes recurrent bacterial infections due to a lack of B cells and antibodies.
- While recurrent infections occur, the typical presentation involves encapsulated bacteria and lacks the widespread purulent skin lesions and lymphadenopathy seen in CGD.
*Impaired signaling to actin cytoskeleton reorganization*
- This defect is characteristic of **Wiskott-Aldrich syndrome**, leading to thrombocytopenia, eczema, and recurrent infections, particularly by encapsulated bacteria.
- The clinical picture of recurrent widespread skin abscesses and granuloma formation is not typical for Wiskott-Aldrich syndrome.
*Defective neutrophil chemotaxis*
- This can be seen in conditions like **leukocyte adhesion deficiency (LAD)** or **Chédiak-Higashi syndrome**.
- LAD presents with recurrent bacterial infections, impaired wound healing, and delayed umbilical cord separation, while Chédiak-Higashi involves partial oculocutaneous albinism and recurrent pyogenic infections, distinct from this patient's symptoms.
*Impaired repair of double-strand DNA breaks*
- This defect is associated with conditions like **ataxia-telangiectasia**, which involves cerebellar ataxia, telangiectasias, and immunodeficiency (T-cell and IgA deficiency).
- The patient's symptoms of recurrent purulent skin lesions and infections are not characteristic of the DNA repair defects seen in ataxia-telangiectasia.
Zoonotic bacterial infections US Medical PG Question 10: A scientist is studying the process of thymus-dependent B cell activation in humans. He observes that, after bacterial infections, the germinal centers of secondary lymphoid organs become highly metabolically active. After subsequent reinfection with the same pathogen, the organism is able to produce immunoglobulins at a much faster pace. Which of the following processes is likely taking place in the germinal centers at the beginning of an infection?
- A. T cell positive selection
- B. T cell negative selection
- C. Development of early pro-B cells
- D. Development of immature B cells
- E. Affinity maturation (Correct Answer)
Zoonotic bacterial infections Explanation: ***Affinity maturation***
- This process involves **somatic hypermutation** in the germinal centers, leading to B cells with receptors having higher affinity for the antigen.
- Coupled with **clonal selection**, this ensures that subsequent immune responses are faster and more effective due to the improved binding of antibodies to the pathogen.
*T cell positive selection*
- This process occurs in the **thymic cortex** and selects T cells capable of recognizing self-MHC molecules.
- It is crucial for the development of the T cell repertoire and does not occur in germinal centers during B cell activation.
*T cell negative selection*
- This process takes place primarily in the **thymic medulla** and eliminates T cells that bind too strongly to self-peptide/MHC complexes, preventing autoimmunity.
- It is a central tolerance mechanism and is not related to B cell responses in germinal centers.
*Development of early pro-B cells*
- The development of pro-B cells, and indeed all early stages of B cell development (pro-B, pre-B, immature B), occurs primarily in the **bone marrow**.
- These are early developmental stages, distinct from the antigen-driven processes occurring in secondary lymphoid organs during an infection.
*Development of immature B cells*
- Immature B cells develop from pre-B cells in the **bone marrow** and then migrate to secondary lymphoid organs to complete maturation.
- This step occurs prior to encountering an antigen in the germinal centers and is part of initial B cell development rather than the refinement of the immune response to an infection.
More Zoonotic bacterial infections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.