Exotoxins and endotoxins US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Exotoxins and endotoxins. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Exotoxins and endotoxins US Medical PG Question 1: A 30-year-old man returns to the hospital 3 weeks after open reduction and internal fixation of left tibia and fibula fractures from a motor vehicle accident. The patient complains that his surgical site has been draining pus for a few days, and his visiting nurse told him to go to the emergency room after he had a fever this morning. On exam, his temperature is 103.0°F (39.4°C), blood pressure is 85/50 mmHg, pulse is 115/min, and respirations are 14/min. The ED physician further documents that the patient is also starting to develop a diffuse, macular rash. The patient is started on broad spectrum antibiotics, and Gram stain demonstrates purple cocci in clusters. Which of the following toxins is likely to be the cause of this patient's condition?
- A. Pyogenic exotoxin A
- B. Alpha toxin
- C. Endotoxin
- D. Exfoliative toxin
- E. Toxic shock syndrome toxin 1 (Correct Answer)
Exotoxins and endotoxins Explanation: ***Toxic shock syndrome toxin 1***
- The patient presents with **fever**, **hypotension**, and a **diffuse macular rash** following a surgical procedure with a draining wound, consistent with **toxic shock syndrome**.
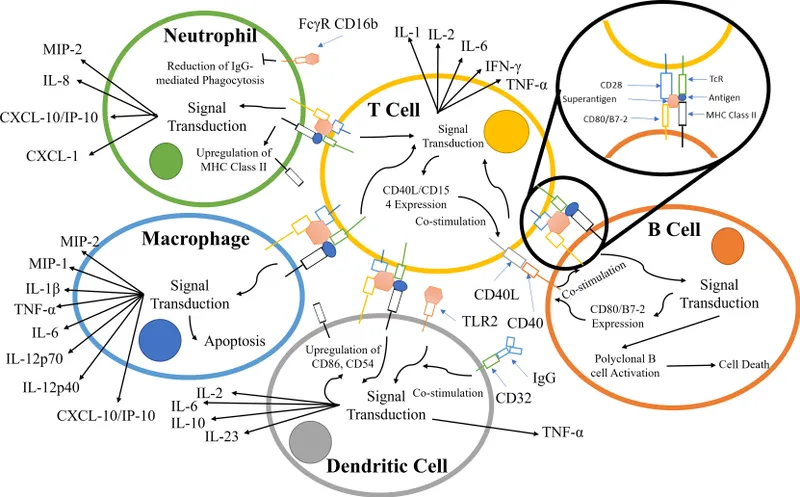
- **Gram-positive cocci in clusters** (consistent with *Staphylococcus aureus*) grown from a surgical site infection, coupled with symptoms of toxic shock, points to **TSST-1** as the likely causative toxin due to its superantigen activity.
*Pyogenic exotoxin A*
- This toxin, also known as **streptococcal pyrogenic exotoxin A (SpeA)**, is associated with **streptococcal toxic shock syndrome** and scarlet fever.
- While it causes a similar toxic shock picture, the **Gram stain showing cocci in clusters** points away from *Streptococcus* (which is typically in chains) and towards *Staphylococcus*.
*Alpha toxin*
- **Alpha toxin** is a pore-forming cytotoxin produced by *Staphylococcus aureus* that contributes to tissue damage and host cell lysis.
- While *S. aureus* is the causative agent, alpha toxin primarily causes **local tissue destruction** and hemolysis, not the systemic superantigen effects seen in toxic shock syndrome.
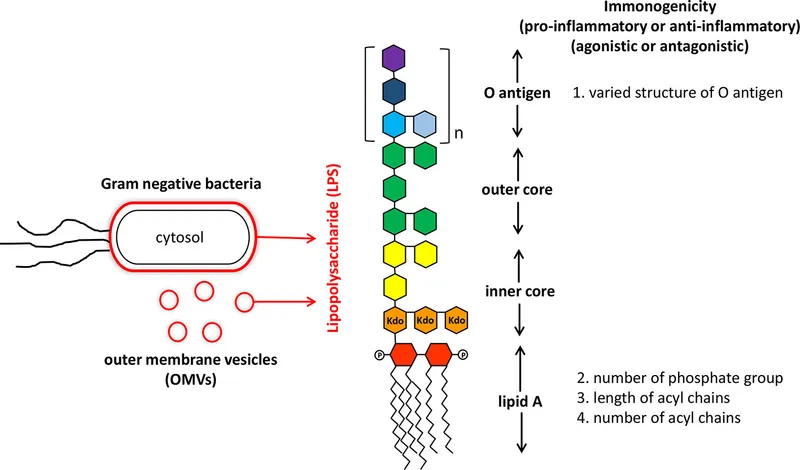
*Endotoxin*
- **Endotoxin** (lipopolysaccharide or LPS) is a component of the outer membrane of **Gram-negative bacteria** and is responsible for many symptoms of Gram-negative sepsis.
- The Gram stain in this case shows **Gram-positive cocci in clusters**, ruling out Gram-negative bacterial infection and endotoxin as the primary cause.
*Exfoliative toxin*
- **Exfoliative toxins A and B** are produced by *Staphylococcus aureus* and are responsible for **staphylococcal scalded skin syndrome (SSSS)**.
- SSSS is characterized by widespread **blistering and desquamation** of the epidermis, which is distinct from the **macular rash** and hemodynamic instability seen in toxic shock syndrome.
Exotoxins and endotoxins US Medical PG Question 2: A 62-year-old woman presents to the emergency department for evaluation of a spreading skin infection that began from an ulcer on her foot. The patient has type 2 diabetes mellitus that is poorly controlled. On examination, there is redness and erythema to the lower limb with skin breakdown along an extensive portion of the leg. The patient’s tissues separate readily from the fascial plane, prompting a diagnosis of necrotizing fasciitis. What is the exotoxin most likely associated with this patient’s presentation?
- A. Streptococcal pyogenic exotoxin A
- B. TSST-1
- C. Diphtheria toxin
- D. Exfoliative toxin
- E. Streptococcal pyogenic exotoxin B (Correct Answer)
Exotoxins and endotoxins Explanation: ***Streptococcal pyogenic exotoxin B***
- **Streptococcal pyogenic exotoxin B** is a **cysteine protease** that directly degrades tissue, including collagen and fibronectin, leading to the rapid tissue destruction characteristic of **necrotizing fasciitis**.
- This exotoxin is frequently associated with **Group A Streptococcus (GAS)** infections, a common cause of severe soft tissue infections, especially in immunocompromised individuals like diabetics.
*Streptococcal pyogenic exotoxin A*
- This exotoxin acts as a **superantigen**, primarily causing symptoms of **streptococcal toxic shock syndrome** (STSS), characterized by fever, rash, and organ failure.
- While GAS can cause necrotizing fasciitis, Exotoxin A is more closely linked to toxic shock phenomena rather than direct tissue destruction.
*TSST-1*
- **Toxic Shock Syndrome Toxin-1 (TSST-1)** is produced by **Staphylococcus aureus** and is a classic cause of **staphylococcal toxic shock syndrome**.
- It acts as a **superantigen** but is not directly responsible for the extensive tissue necrosis seen in necrotizing fasciitis caused by streptococci.
*Diphtheria toxin*
- **Diphtheria toxin**, produced by *Corynebacterium diphtheriae*, inhibits **protein synthesis** by inactivating elongation factor-2 (EF-2), leading to cell death.
- It causes diphtheria, characterized by a **pseudomembrane** in the throat and myocarditis, not necrotizing fasciitis.
*Exfoliative toxin*
- **Exfoliative toxins A and B** are produced by **Staphylococcus aureus** and are responsible for **Staphylococcal Scalded Skin Syndrome (SSSS)**.
- These toxins cause cleavage of desmoglein-1 in the epidermis, leading to widespread blistering and desquamation, not deep tissue necrosis.
Exotoxins and endotoxins US Medical PG Question 3: A 27-year-old man presents to the emergency department with unrelenting muscle spasms for the past several hours. The patient’s girlfriend states that he started having jaw spasms and soreness last night but now his neck, back, and arms are spasming. She also states that he stepped on a nail about 1 week ago. Past medical history is noncontributory. The patient's vaccination status is unknown at this time. Today, the vital signs include temperature 39.1°C (102.4°F), heart rate 115/min, blood pressure 145/110 mm Hg, and respiratory rate 10/min. On exam, the patient is in obvious discomfort, with a clenched jaw and extended neck. Labs are drawn and a basic metabolic panel comes back normal and the white blood cell (WBC) count is moderately elevated. Which of the following is the most likely etiology of this patient’s symptoms?
- A. An exotoxin that causes ADP-ribosylation of EF-2
- B. An edema factor that functions as adenylate cyclase
- C. A heat-labile toxin that inhibits ACh release at the NMJ
- D. An exotoxin that cleaves SNARE proteins (Correct Answer)
- E. A toxin that disables the G-protein coupled receptor
Exotoxins and endotoxins Explanation: ***An exotoxin that cleaves SNARE proteins***
- The patient's presentation with **unrelenting muscle spasms**, jaw spasms (**trismus**), extended neck (**opisthotonus**), and a recent **puncture wound** are classic signs of **tetanus**.
- **Tetanospasmin**, the neurotoxin produced by *Clostridium tetani*, acts by cleaving **SNARE proteins**, which are essential for the release of **inhibitory neurotransmitters** (glycine and GABA) from spinal interneurons, leading to uncontrolled muscle contraction.
*An exotoxin that causes ADP-ribosylation of EF-2*
- This mechanism describes **diphtheria toxin**, which is produced by *Corynebacterium diphtheriae* and inhibits protein synthesis in eukaryotic cells.
- While *C. diphtheriae* can cause systemic effects, it primarily manifests as **upper respiratory tract infection** with pseudomembrane formation, lymphadenopathy, and myocarditis, not generalized muscle spasms.
*An edema factor that functions as adenylate cyclase*
- This describes the **edema factor** component of **anthrax toxin**, produced by *Bacillus anthracis*.
- Anthrax typically causes cutaneous, inhalational, or gastrointestinal infections, and its symptoms do not include the generalized muscle spasms seen in this patient.
*A heat-labile toxin that inhibits ACh release at the NMJ*
- This mechanism describes **botulinum toxin**, produced by *Clostridium botulinum*, which causes **flaccid paralysis** by preventing the release of acetylcholine at the neuromuscular junction.
- The patient exhibits muscle spasms and rigidity (**spastic paralysis**), which is directly opposite to the effects of botulinum toxin.
*A toxin that disables the G-protein coupled receptor*
- While various toxins can affect G-protein coupled receptors (e.g., cholera toxin or pertussis toxin), this general description does not specifically match the clinical presentation of tetanus.
- Toxins affecting G-protein coupled receptors typically lead to symptoms like **severe diarrhea** (cholera) or **whooping cough** (pertussis) rather than generalized muscle spasms.
Exotoxins and endotoxins US Medical PG Question 4: An otherwise healthy 7-year-old boy is brought to the emergency department because of a 1-day history of involuntary muscle contractions and pain in his back and neck. Two weeks ago, he fell while playing in the sandbox and scraped both his knees. He has not received any vaccinations since birth. His temperature is 38.5°C (101.3°F). He is diaphoretic. Examination shows inability to open his mouth beyond 1 cm. There is hyperextension of the lumbar spine and resistance to neck flexion. Administration of which of the following would most likely have prevented this patient's current condition?
- A. Chemically-inactivated virus
- B. Denatured bacterial product (Correct Answer)
- C. Viable but weakened microorganism
- D. Human immunoglobulin against a viral protein
- E. Capsular polysaccharides
Exotoxins and endotoxins Explanation: ***Denatured bacterial product***
- This describes a **toxoid vaccine**, specifically the **tetanus toxoid vaccine**, which is a denatured form of the bacterial toxin.
- The patient's symptoms (trismus, back and neck pain, muscle contractions, **opisthotonus**) are classic for **tetanus**, and his unvaccinated status and recent wound increase his risk.
*Chemically-inactivated virus*
- This refers to an **inactivated viral vaccine**, which is effective against viral infections, not bacterial toxins.
- Tetanus is caused by a bacterial toxin, not a virus, making this vaccine type irrelevant to preventing the described condition.
*Viable but weakened microorganism*
- This describes a **live-attenuated vaccine**, which typically induces a strong immune response against the live pathogen itself.
- Tetanus prevention targets the toxin produced by *Clostridium tetani*, not the microorganism directly via an attenuated form.
*Human immunoglobulin against a viral protein*
- This describes **passive immunization** using antibodies against a viral protein, usually for viral infections or post-exposure prophylaxis.
- While passive immunization with tetanus immune globulin can *treat* tetanus, a vaccine is needed for *prevention*, and the target here is a bacterial toxin, not a viral protein.
*Capsular polysaccharides*
- This describes a component of **polysaccharide vaccines** used against encapsulated bacteria (e.g., *Streptococcus pneumoniae*, *Haemophilus influenzae type b*).
- *Clostridium tetani* is not an encapsulated bacterium, and its pathogenicity stems from its toxin, not its capsule.
Exotoxins and endotoxins US Medical PG Question 5: A previously healthy 17-year-old boy is brought to the emergency department because of fever, nausea, and myalgia for the past day. His temperature is 39.5°C (103.1°F), pulse is 112/min, and blood pressure is 77/55 mm Hg. Physical examination shows scattered petechiae over the anterior chest and abdomen. Blood culture grows an organism on Thayer-Martin agar. Which of the following virulence factors of the causal organism is most likely responsible for the high mortality rate associated with it?
- A. Immunoglobulin A protease
- B. Lipooligosaccharide (Correct Answer)
- C. Toxic shock syndrome toxin-1
- D. Lipoteichoic acid
- E. Erythrogenic exotoxin A
Exotoxins and endotoxins Explanation: ***Lipooligosaccharide***
- The patient's presentation with **fever**, **hypotension**, and **petechiae**, along with a positive blood culture on Thayer-Martin agar, points to **meningococcemia** caused by *Neisseria meningitidis*.
- **Lipooligosaccharide (LOS)** acts as an **endotoxin**, triggering an excessive inflammatory response that leads to widespread vascular damage, **capillary leakage**, and **septic shock**, accounting for the high mortality.
*Immunoglobulin A protease*
- While *N. meningitidis* produces **IgA protease** to cleave secretory IgA and evade host defenses on mucosal surfaces, this factor is primarily involved in colonization and initial invasion rather than the systemic severity and mortality of septic shock.
- Its role is to help the bacteria **adhere and penetrate** host mucous membranes, but it does not directly cause the shock and petechiae seen in this severe presentation.
*Toxic shock syndrome toxin-1*
- **Toxic shock syndrome toxin-1 (TSST-1)** is a **superantigen** produced by *Staphylococcus aureus* that causes **toxic shock syndrome**, which can present with fever, rash, and hypotension.
- However, the organism grown on **Thayer-Martin agar** is characteristic of *Neisseria meningitidis*, not *Staphylococcus aureus*.
*Lipoteichoic acid*
- **Lipoteichoic acid** is a major component of the cell wall of **Gram-positive bacteria**, acting as a potent proinflammatory molecule and contributing to septic shock in those infections.
- *Neisseria meningitidis* is a **Gram-negative bacterium**, and therefore does not possess lipoteichoic acid.
*Erythrogenic exotoxin A*
- **Erythrogenic exotoxin A** is primarily produced by ***Streptococcus pyogenes*** and is responsible for the characteristic rash of **scarlet fever**.
- While *S. pyogenes* can cause invasive infections, the clinical picture and the specific growth on **Thayer-Martin agar** are not consistent with streptococcal infection.
Exotoxins and endotoxins US Medical PG Question 6: An investigator is studying bacterial toxins in a nonpathogenic bacterial monoculture that has been inoculated with specific bacteriophages. These phages were previously cultured in a toxin-producing bacterial culture. After inoculation, a new toxin is isolated from the culture. Genetic sequencing shows that the bacteria have incorporated viral genetic information, including the gene for this toxin, into their genome. The described process is most likely responsible for acquired pathogenicity in which of the following bacteria?
- A. Staphylococcus aureus
- B. Haemophilus influenzae
- C. Neisseria meningitidis
- D. Streptococcus pneumoniae
- E. Corynebacterium diphtheriae (Correct Answer)
Exotoxins and endotoxins Explanation: ***Corynebacterium diphtheriae***
- The process described, where a bacterium acquires new genetic information (e.g., a toxin gene) from a bacteriophage, is called **lysogenic conversion** or **phage conversion**. *Corynebacterium diphtheriae* is the **classic example** of this mechanism, acquiring its toxigenicity through phage-mediated transfer of the **diphtheria toxin gene (tox gene)** via bacteriophage β.
- The diphtheria toxin is an **AB toxin** that ADP-ribosylates and thereby inactivates **elongation factor 2 (EF-2)**, inhibiting host cell protein synthesis and leading to the characteristic symptoms of diphtheria.
- This is the **prototypical and most clinically significant example** of lysogenic conversion in medical microbiology.
*Staphylococcus aureus*
- While *Staphylococcus aureus* can acquire some virulence factors via bacteriophages (e.g., **Panton-Valentine leukocidin**, some enterotoxins), many of its toxins are encoded on **mobile genetic elements** such as plasmids, pathogenicity islands, or chromosomal genes.
- However, *S. aureus* is **not the classic example** of lysogenic conversion described in this scenario. *C. diphtheriae* better exemplifies the acquisition of a major toxin exclusively through phage conversion.
*Haemophilus influenzae*
- *Haemophilus influenzae* primarily causes disease through its **polysaccharide capsule** (especially type b) and is a common cause of respiratory infections and meningitis.
- Its major virulence factors are typically chromosomally encoded or acquired through **transformation** (uptake of naked DNA), not through phage conversion for a primary toxin.
*Neisseria meningitidis*
- *Neisseria meningitidis* causes meningococcal disease, primarily due to its **polysaccharide capsule** and **endotoxin (LPS)**.
- While genetic exchange can occur, the acquisition of a major toxin gene by phage conversion as described is not a primary mechanism for its key virulence factors.
*Streptococcus pneumoniae*
- *Streptococcus pneumoniae* is a leading cause of pneumonia, meningitis, and otitis media, with its main virulence factor being its **polysaccharide capsule**.
- It primarily acquires genetic material through **transformation** (competence-mediated uptake of naked DNA), which contributes to antibiotic resistance and capsule types, but lysogenic conversion with toxin acquisition is not typical for its major virulence factors.
Exotoxins and endotoxins US Medical PG Question 7: A 25-day-old male infant presents to the emergency department because his mother states that he has been acting irritable for the past 2 days and has now developed a fever. On exam, the infant appears uncomfortable and has a temperature of 39.1 C. IV access is immediately obtained and a complete blood count and blood cultures are drawn. Lumbar puncture demonstrates an elevated opening pressure, elevated polymorphonuclear neutrophil, elevated protein, and decreased glucose. Ampicillin and cefotaxime are immediately initiated and CSF culture eventually demonstrates infection with a Gram-negative rod. Which of the following properties of this organism was necessary for the infection of this infant?
- A. K capsule (Correct Answer)
- B. M protein
- C. Fimbriae
- D. IgA protease
- E. LPS endotoxin
Exotoxins and endotoxins Explanation: ***K capsule***
- The K capsule (specifically **K1 antigen**) is a specific virulence factor found in **E. coli** strains, which are a common cause of neonatal meningitis.
- This capsule is **antiphagocytic** and helps the bacteria evade the immune system, allowing it to cross the **blood-brain barrier** and cause meningitis in neonates.
*M protein*
- **M protein** is a major virulence factor associated with **Streptococcus pyogenes** (Group A Strep), playing a role in attachment and immune evasion.
- While *S. pyogenes* can cause infections, it is not typically the Gram-negative rod responsible for **neonatal meningitis** and its M protein is not relevant here.
*Fimbriae*
- **Fimbriae** (pili) are important for bacterial **adhesion** to host cells, often in the initial stages of infection, particularly in urinary tract infections (UTIs).
- While gram-negative rods possess fimbriae, the specific virulence factor critical for **meningitis** caused by *E. coli* in neonates is the K1 capsule, not fimbriae which are more for initial colonization.
*IgA protease*
- **IgA protease** is an enzyme produced by some bacteria (e.g., *N. meningitidis, H. influenzae, S. pneumoniae*) that cleaves **IgA antibodies**, helping them colonize mucous membranes.
- This enzyme is not a primary virulence factor for the **Gram-negative rod** causing neonatal meningitis, where capsule formation is more critical for invasion.
*LPS endotoxin*
- **Lipopolysaccharide (LPS) endotoxin** is a component of the outer membrane of Gram-negative bacteria and is responsible for many symptoms of sepsis and **systemic inflammation**.
- While LPS contributes to the overall disease severity, it primarily mediates **inflammation and fever**, and is not the specific factor necessary for **invasion and survival within the central nervous system**, which is facilitated by the K capsule.
Exotoxins and endotoxins US Medical PG Question 8: A 2-month-old girl is brought to the physician by her father for a routine well-child examination. She is given a vaccine that contains polyribosylribitol phosphate conjugated to a toxoid carrier. The vaccine is most likely to provide immunity against which of the following pathogens?
- A. Haemophilus influenzae (Correct Answer)
- B. Neisseria meningitidis
- C. Bordetella pertussis
- D. Streptococcus pneumoniae
- E. Corynebacterium diphtheriae
Exotoxins and endotoxins Explanation: **Haemophilus influenzae**
- The vaccine described, containing **polyribosylribitol phosphate (PRP)** conjugated to a toxoid carrier, is characteristic of the **Haemophilus influenzae type b (Hib) vaccine**.
- PRP is the **polysaccharide capsule** of *H. influenzae* type b, and conjugating it to a protein (toxoid carrier) allows for T-cell dependent immunity, effective in infants.
*Neisseria meningitidis*
- While *N. meningitidis* also has a **polysaccharide capsule** and vaccines are available, their capsular components differ (e.g., serogroups A, C, Y, W-135, or B outer membrane protein).
- The description of **polyribosylribitol phosphate** is specific to *H. influenzae* type b.
*Bordetella pertussis*
- Vaccines against *Bordetella pertussis* are typically **acellular pertussis vaccines (aP)**, which contain purified components like pertussis toxoid, filamentous hemagglutinin, and pertactin, not a PRP conjugate.
- These vaccines target bacterial toxins and adhesins, not a polysaccharide capsule unique to PRP.
*Streptococcus pneumoniae*
- Vaccines for *S. pneumoniae* (pneumococcal vaccines) use **capsular polysaccharides** from various serotypes, often conjugated to a protein carrier (e.g., diphtheria toxoid), but the specific polysaccharide is not PRP.
- The structure and serotypes of pneumococcal capsular polysaccharides are distinct from PRP.
*Corynebacterium diphtheriae*
- The vaccine for *C. diphtheriae* is the **diphtheria toxoid**, which is an inactivated form of the diphtheria toxin, not a polysaccharide conjugate.
- It provides immunity by inducing antibodies against the toxin, preventing its harmful effects.
Exotoxins and endotoxins US Medical PG Question 9: A 3-year-old boy presents to the emergency department with a fever and a rash. This morning the patient was irritable and had a fever which gradually worsened throughout the day. He also developed a rash prior to presentation. He was previously healthy and is not currently taking any medications. His temperature is 102.0°F (38.9°C), blood pressure is 90/50 mmHg, pulse is 160/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam is notable for a scarlatiniform rash with flaccid blisters that rupture easily, covering more than 60% of the patient’s body surface. The lesions surround the mouth but do not affect the mucosa, and palpation of the rash is painful. Which of the following is the most likely diagnosis?
- A. Staphylococcal scalded skin syndrome (Correct Answer)
- B. Toxic epidermal necrolysis
- C. Toxic shock syndrome
- D. Urticaria
- E. Stevens Johnson syndrome
Exotoxins and endotoxins Explanation: ***Staphylococcal scalded skin syndrome***
- The presentation of a **fever**, **irritability**, and a **scarlatiniform rash with flaccid blisters** that rupture easily, especially with painful lesions and perioral involvement without mucosal lesions, is highly characteristic of **Staphylococcal scalded skin syndrome (SSSS)**.
- SSSS is caused by **exfoliative toxins** produced by *Staphylococcus aureus*, which target **desmoglein-1** in the skin, leading to widespread superficial blistering and epidermal sloughing.
*Toxic epidermal necrolysis*
- **Toxic epidermal necrolysis (TEN)** is a severe mucocutaneous reaction often triggered by **medications**, characterized by widespread **epidermal detachment (>30% BSA)** and **mucosal involvement**.
- TEN typically presents with full-thickness epidermal necrosis and severe systemic symptoms, often after drug exposure, which is not noted in this previously healthy, non-medicated child.
*Toxic shock syndrome*
- **Toxic shock syndrome (TSS)** is characterized by **fever**, **hypotension**, **diffuse erythematous rash**, and **multisystem organ dysfunction**.
- While a rash and fever are present, the hallmark **flaccid blistering** and **skin peeling** seen in SSSS is not typical for TSS; TSS rash is more often a blanching erythroderma.
*Urticaria*
- **Urticaria (hives)** presents as **pruritic, transient, raised erythematous wheals** that blanch with pressure.
- The rash in this patient is described as **scarlatiniform with flaccid blisters** and is painful, which is inconsistent with the typical appearance and symptoms of urticaria.
*Stevens Johnson syndrome*
- **Stevens-Johnson syndrome (SJS)** is a severe adverse drug reaction, similar to TEN but with less extensive skin involvement (**<10% BSA**), and is characterized by **erythematous macules**, **targetoid lesions**, and **mucosal involvement**.
- While blistering can occur, the widespread, painful, easily rupturing flaccid blisters without specific target lesions and prominent perioral involvement (without mucosal affection) point more strongly to SSSS over SJS.
Exotoxins and endotoxins US Medical PG Question 10: A group of medical students is studying bacteria and their pathogenesis. They have identified that a substantial number of bacteria cause human disease by producing exotoxins. Exotoxins are typically proteins, but they have different mechanisms of action and act at different sites. The following is a list of exotoxins together with mechanisms of action. Which of the following pairs is correctly matched?
- A. Tetanospasmin - binds 60S ribosome subunit and inhibits protein synthesis
- B. Cholera toxin - ADP-ribosylates Gs, keeping adenylate cyclase active and ↑ [cAMP] (Correct Answer)
- C. Diphtheria toxin - cleaves synaptobrevin, blocking vesicle formation and the release of acetylcholine
- D. Botulinum toxin - cleaves synaptobrevin, blocking vesicle formation and the release of the inhibitory neurotransmitters GABA and glycine
- E. Anthrax toxin - ADP-ribosylates elongation factor - 2 (EF-2) and inhibits protein synthesis
Exotoxins and endotoxins Explanation: ***Cholera toxin - ADP-ribosylates Gs, keeping adenylate cyclase active and ↑ [cAMP]***
- **Cholera toxin** works by irrevocably activating **adenylate cyclase** via **ADP-ribosylation** of the **alpha subunit of Gs protein**.
- This leads to a persistent increase in intracellular **cyclic AMP (cAMP)**, resulting in excessive secretion of water and electrolytes into the intestinal lumen, causing characteristic **rice-water diarrhea**.
*Tetanospasmin - binds 60S ribosome subunit and inhibits protein synthesis*
- **Tetanospasmin (tetanus toxin)** acts by cleaving **synaptobrevin**, a SNARE protein, which inhibits the release of **inhibitory neurotransmitters (GABA and glycine)** from Renhaw cells in the spinal cord.
- This blockade of inhibitory signals leads to uncontrolled muscle contractions and **spastic paralysis**.
*Diphtheria toxin - cleaves synaptobrevin, blocking vesicle formation and the release of acetylcholine*
- **Diphtheria toxin** works by **ADP-ribosylating elongation factor-2 (EF-2)**, which is crucial for protein synthesis.
- The inactivation of **EF-2** leads to the arrest of protein synthesis and ultimately **cell death**.
*Botulinum toxin - cleaves synaptobrevin, blocking vesicle formation and the release of the inhibitory neurotransmitters GABA and glycine*
- **Botulinum toxin** cleaves **SNARE proteins** (including synaptobrevin) at the **neuromuscular junction**, specifically blocking the release of **acetylcholine**.
- This inhibition of neurotransmitter release at the presynaptic terminal leads to **flaccid paralysis**.
*Anthrax toxin - ADP-ribosylates elongation factor - 2 (EF-2) and inhibits protein synthesis*
- **Anthrax toxin** consists of three proteins: Protective Antigen (PA), Edema Factor (EF), and Lethal Factor (LF). The **Edema Factor (EF)** is a **calmodulin-dependent adenylate cyclase** that increases intracellular **cAMP**, and the **Lethal Factor (LF)** is a **metalloprotease** that targets MAPK pathways.
- **Anthrax toxin** does not work by ADP-ribosylating EF-2; that mechanism is characteristic of **diphtheria toxin**.
More Exotoxins and endotoxins US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.