Bacterial taxonomy and classification US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Bacterial taxonomy and classification. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Bacterial taxonomy and classification US Medical PG Question 1: A 50-year-old male presents to the emergency room complaining of fever, shortness of breath, and diarrhea. He returned from a spa in the Rocky Mountains five days prior. He reports that over the past two days, he developed a fever, cough, dyspnea, and multiple watery stools. His past medical history is notable for major depressive disorder and peptic ulcer disease. He takes omeprazole and paroxetine. He does not smoke and drinks alcohol on social occasions. His temperature is 102.8°F (39.3°C), blood pressure is 120/70 mmHg, pulse is 65/min, and respirations are 20/min. Physical examination reveals dry mucus membranes, delayed capillary refill, and rales at the bilateral lung bases. A basic metabolic panel is shown below:
Serum:
Na+: 126 mEq/L
Cl-: 100 mEq/L
K+: 4.1 mEq/L
HCO3-: 23 mEq/L
Ca2+: 10.1 mg/dL
Mg2+: 2.0 mEq/L
Urea nitrogen: 14 mg/dL
Glucose: 90 mg/dL
Creatinine: 1.1 mg/dL
Which of the following is the most appropriate growth medium to culture the pathogen responsible for this patient’s condition?
- A. Eaton’s agar
- B. Bordet-Gengou agar
- C. Thayer-Martin agar
- D. Charcoal yeast agar with iron and cysteine (Correct Answer)
- E. Sorbitol-MacConkey agar
Bacterial taxonomy and classification Explanation: ***Charcoal yeast agar with iron and cysteine***
- This patient's symptoms (fever, cough, dyspnea, diarrhea) after visiting a spa, combined with **hyponatremia** (Na+ 126 mEq/L), are highly characteristic of **Legionnaires' disease** caused by *Legionella pneumophila*.
- *Legionella* is a fastidious organism that requires specialized media for growth, specifically charcoal yeast extract (BCYE) agar supplemented with **L-cysteine** and **iron salts**.
*Eaton’s agar*
- Eaton's agar is a specialized medium used for the primary isolation of **Mycoplasma pneumoniae**.
- *Mycoplasma pneumoniae* typically causes **atypical pneumonia** but does not present with severe gastrointestinal symptoms or hyponatremia as seen in this patient.
*Bordet-Gengou agar*
- Bordet-Gengou agar, containing potato extract, glycerol, and blood, is the selective medium used for the isolation of **Bordetella pertussis**, the causative agent of whooping cough.
- The clinical presentation of **pertussis** involves paroxysmal coughing fits, often with a 'whoop,' and is distinct from the patient's symptoms.
*Thayer-Martin agar*
- Thayer-Martin agar is a selective medium primarily used for the isolation of **Neisseria gonorrhoeae** and *Neisseria meningitidis*.
- These bacteria cause gonorrhea and meningitis, respectively, and are not associated with the respiratory and gastrointestinal symptoms described.
*Sorbitol-MacConkey agar*
- Sorbitol-MacConkey agar is a differential and selective medium used to detect **enterohemorrhagic Escherichia coli O157:H7** in stool samples, which appears as colorless colonies because it cannot ferment sorbitol.
- While the patient has diarrhea, the predominant respiratory symptoms, hyponatremia, and exposure history point away from E. coli O157:H7 as the primary pathogen.
Bacterial taxonomy and classification US Medical PG Question 2: A 24-year-old woman presents to the ED with symptoms of pelvic inflammatory disease despite being previously treated with azithromycin for chlamydial infection. Based on your clinical understanding about the epidemiology of PID, you decide to obtain a gram stain which shows a gram-negative diplococci. What is the next step in order to confirm the identity of the organism described?
- A. Perform an RT-PCR
- B. Culture in TCBS agar
- C. Culture in Thayer-Martin media (Correct Answer)
- D. Obtain an acid fast stain
- E. Culture in Bordet-Gengou agar
Bacterial taxonomy and classification Explanation: ***Culture in Thayer-Martin media***
- The presence of **gram-negative diplococci** in a patient with PID symptoms strongly suggests *Neisseria gonorrhoeae*.
- **Thayer-Martin media** is a selective **agar** specifically designed for the isolation and identification of *Neisseria* species, including *N. gonorrhoeae*, by inhibiting the growth of most commensal bacteria and fungi.
*Perform an RT-PCR*
- While **RT-PCR** can detect *Neisseria gonorrhoeae* nucleic acids, it is primarily used for **molecular diagnosis** and not directly for confirming the identity of a cultured organism visualized on gram stain.
- **RT-PCR** is generally used for direct detection from clinical samples and is particularly useful in situations where culture is difficult or unavailable.
*Culture in TCBS agar*
- **TCBS (Thiosulfate Citrate Bile Salts Sucrose) agar** is a selective medium primarily used for the isolation of *Vibrio* species, which are not typically associated with pelvic inflammatory disease or characterized as gram-negative diplococci.
- This medium is designed to differentiate between different *Vibrio* species based on sucrose fermentation.
*Obtain an acid fast stain*
- An **acid-fast stain** (e.g., Ziehl-Neelsen stain) is used to identify bacteria with a **waxy cell wall**, such as *Mycobacterium* species (e.g., *Mycobacterium tuberculosis*).
- *Neisseria gonorrhoeae* is not acid-fast, and this stain would not be appropriate for its identification.
*Culture in Bordet-Gengou agar*
- **Bordet-Gengou agar** is a specialized culture medium used for the isolation of *Bordetella pertussis*, the causative agent of whooping cough.
- This medium is not suitable for the isolation of *Neisseria gonorrhoeae*.
Bacterial taxonomy and classification US Medical PG Question 3: A 27-year-old woman visits your office with a 3-day complaint of fever, malaise, myalgias, and headaches associated with vulvar itching, vulvar soreness, dysuria, and urethral discharge. The pain when urinating is so severe that she has attempted to avoid the use of the toilet. She just returned from a spring break in the tropics and explains that she had multiple unprotected sexual encounters with men and women. Upon physical examination, the temperature was 38.7°C (101.6°F) and the heart rate was 90/min. The pelvic examination revealed vulvar ulcers, vulvar excoriations, erythema, vaginal mucosa edema, and ulcerative cervicitis. Which of the following will best aid you in the identification of the specific organism causing the above symptoms?
- A. Location of the lesions
- B. Culture in Thayer-Martin agar
- C. Direct fluorescence antigen (Correct Answer)
- D. Serology
- E. Tzanck smear
Bacterial taxonomy and classification Explanation: ***Direct fluorescence antigen***
- A **direct fluorescence antigen (DFA)** test can rapidly identify viral antigens from the lesions, specifically for **Herpes Simplex Virus (HSV)**, which is highly suspected given the patient's symptoms (fever, malaise, myalgias, vulvar ulcers, dysuria, and recent unprotected sexual encounters).
- **HSV** is a common cause of genital ulcers, and DFA offers a quick, sensitive, and specific method for detection directly from clinical samples.
*Location of the lesions*
- While the **location of the lesions** (vulvar ulcers) is characteristic of several sexually transmitted infections (STIs), it is not specific enough to identify the *specific organism* without further laboratory testing.
- Conditions like syphilis, chancroid, and HSV all cause genital ulcers, making location alone insufficient for definitive diagnosis.
*Culture in Thayer-Martin agar*
- **Thayer-Martin agar** is selectively used for culturing **Neisseria gonorrhoeae**, which causes gonorrhea.
- Although the patient has urethral discharge and dysuria, the presence of **vulvar ulcers** and systemic symptoms like fever and myalgias point away from uncomplicated gonorrhea.
*Serology*
- **Serology** detects antibodies to pathogens, indicating past or present infection, but is often less useful for identifying the *acute* causative organism in the initial stages of a symptomatic outbreak like this one.
- For instance, HSV serology can distinguish between HSV-1 and HSV-2 exposure but does not confirm active infection in the way direct antigen methods or PCR do.
*Tzanck smear*
- A **Tzanck smear** can reveal characteristic **multinucleated giant cells** and **intranuclear inclusions**, which are indicative of herpesvirus infections (HSV or VZV).
- However, it is less sensitive and specific than a direct fluorescence antigen test or PCR, and results can be variable depending on the quality of the smear and interpretation.
Bacterial taxonomy and classification US Medical PG Question 4: A 55-year-old woman with type 2 diabetes mellitus is admitted to the hospital because of a 2-day history of fever, breathlessness, and cough productive of large quantities of green sputum. She drinks 8 beers daily. Her temperature is 39°C (102.2°F), pulse is 110/min, respirations are 28/min, and blood pressure is 100/60 mm Hg. Blood and sputum cultures grow gram-negative, catalase-positive, capsulated bacilli. Which of the following components of the causal organism is the most likely cause of this patient's hypotension?
- A. Poly-D-glutamate
- B. Teichoic acid
- C. Lipid A (Correct Answer)
- D. Lecithinase
- E. Lipooligosaccharide
Bacterial taxonomy and classification Explanation: ***Lipid A***
- The patient's presentation with **fever**, **hypotension**, and gram-negative bacterial infection suggests **sepsis** and **septic shock**.
- **Lipid A** is the endotoxic component of **lipopolysaccharide (LPS)** found in the outer membrane of gram-negative bacteria, directly responsible for mediating the systemic inflammatory response and hypotension in septic shock.
- Lipid A is recognized by **TLR4** on immune cells, triggering the release of **TNF-α**, **IL-1**, and other cytokines that cause vasodilation, increased vascular permeability, and shock.
*Poly-D-glutamate*
- This is a component of the **capsule of *Bacillus anthracis***, which is a gram-positive rod, not the gram-negative, catalase-positive, capsulated organism described.
- While it contributes to virulence by inhibiting phagocytosis, it does not directly cause the profound hemodynamic changes seen in sepsis from gram-negative bacteria.
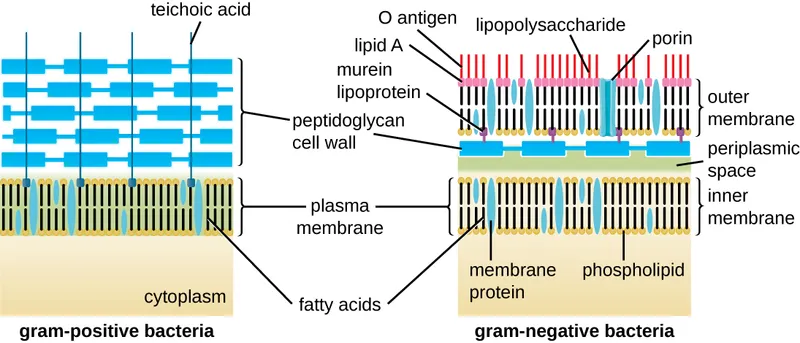
*Teichoic acid*
- **Teichoic acids** are components of the **cell wall of gram-positive bacteria** (e.g., *Staphylococcus*, *Streptococcus*) and are not found in gram-negative bacteria.
- While they can stimulate an inflammatory response, they are not the primary cause of septic shock in gram-negative infections.
*Lecithinase*
- **Lecithinase** (also known as **alpha-toxin** or **phospholipase C**) is an **exotoxin** produced by various bacteria, notably *Clostridium perfringens*.
- While it can cause tissue damage and contribute to virulence, it is not an integral structural component of the bacterial cell wall responsible for generalized vasodilation and hypotension in gram-negative sepsis.
*Lipooligosaccharide*
- **Lipooligosaccharide (LOS)** is a structural variant of LPS found in certain gram-negative bacteria (particularly **Neisseriaceae** like *N. meningitidis* and *N. gonorrhoeae*), consisting of **Lipid A** plus a short oligosaccharide core without the O-antigen repeats.
- While **Lipid A within LOS** is endotoxic, the question asks for the specific **component** causing hypotension, which is **Lipid A itself**, not the larger LOS molecule.
- The likely pathogen here (*Klebsiella pneumoniae* given clinical context) contains **LPS**, not LOS, making Lipid A the most precise answer.
Bacterial taxonomy and classification US Medical PG Question 5: A 22-year-old woman at 30 weeks gestation presents to the obstetrician with the sudden onset of fever, headache, anorexia, fatigue, and malaise. She mentioned that she had eaten ice cream 3 days ago. Blood cultures show gram-positive rods that are catalase-positive and display distinctive tumbling motility in liquid medium. What is the most likely diagnosis?
- A. Tularaemia
- B. Brucellosis
- C. Legionnaires' disease
- D. Influenza
- E. Listeriosis (Correct Answer)
Bacterial taxonomy and classification Explanation: ***Listeriosis***
- The patient's symptoms (fever, headache, anorexia, fatigue, malaise), pregnancy status (30 weeks gestation), recent consumption of **ice cream** (a potential source of **Listeria monocytogenes**), and blood culture findings of **gram-positive rods** that are **catalase-positive** with **tumbling motility** are all classic indicators of listeriosis.
- **Listeria monocytogenes** is known to cause severe illness in pregnant women and has a characteristic **tumbling motility** due to flagella and can grow at refrigerator temperatures, making contaminated dairy products a common source.
*Tularaemia*
- Tularaemia is caused by **Francisella tularensis**, which is a **gram-negative coccobacillus**, not a gram-positive rod, and typically transmitted through contact with infected animals or insect bites.
- It usually presents with a papule that ulcerates, lymphadenopathy, and systemic symptoms, which are not described here.
*Brucellosis*
- Brucellosis is caused by bacteria of the genus **Brucella**, which are **gram-negative coccobacillary rods**, not gram-positive, and typically transmitted from unpasteurized dairy products or contact with infected animals.
- While it can present with fever and malaise, the gram stain and motility characteristics in the blood culture rule it out.
*Legionnaires' disease*
- Legionnaires' disease is caused by **Legionella pneumophila**, a **gram-negative rod** that is difficult to culture and often diagnosed via urine antigen test for Legionella serogroup 1.
- It primarily causes pneumonia and does not typically present with the described blood culture findings.
*Influenza*
- Influenza is a **viral infection** and would not show **gram-positive rods** or any bacterial growth on blood cultures.
- While it presents with fever, headache, and fatigue, the microbiological findings are inconsistent with a viral etiology.
Bacterial taxonomy and classification US Medical PG Question 6: A 10-year-old girl is brought to the emergency department because of a 2-day history of bloody diarrhea and abdominal pain. Four days ago, she visited a petting zoo with her family. Her temperature is 39.4°C (102.9°F). Abdominal examination shows tenderness to palpation of the right lower quadrant. Stool cultures at 42°C grow colonies that turn black after adding phenylenediamine. Which of the following best describes the most likely causal organism?
- A. Gram-positive, anaerobic, rod-shaped bacteria that form spores
- B. Gram-positive, aerobic, rod-shaped bacteria that produce catalase
- C. Gram-negative, non-flagellated bacteria that do not ferment lactose
- D. Gram-negative, flagellated bacteria that do not ferment lactose (Correct Answer)
- E. Gram-negative, non-flagellated bacteria that ferment lactose
Bacterial taxonomy and classification Explanation: ***Gram-negative, flagellated bacteria that do not ferment lactose***
- The clinical presentation of **bloody diarrhea**, **abdominal pain**, and fever, along with a history of **petting zoo exposure**, strongly suggests a *Campylobacter* infection, which is a **gram-negative, flagellated, curved rod** that does not ferment lactose.
- The growth at **42°C (thermophilic)** and a **positive oxidase test** (indicated by colonies turning black after adding phenylenediamine, an oxidase reagent) are characteristic features of *Campylobacter spp*.
*Gram-positive, anaerobic, rod-shaped bacteria that form spores*
- This description typically refers to organisms like *Clostridium difficile* or *Clostridium perfringens*, which can cause diarrhea.
- However, they are **anaerobic** and would not grow well in typical stool culture conditions without specific anaerobic techniques, nor would they produce a positive oxidase test.
*Gram-positive, aerobic, rod-shaped bacteria that produce catalase*
- This describes organisms like *Listeria monocytogenes* or *Bacillus cereus*.
- While *Listeria* can cause gastrointestinal symptoms, it's less commonly associated with the acute, bloody diarrhea and petting zoo exposure seen here, and *Bacillus cereus* typically causes food poisoning with vomiting.
*Gram-negative, non-flagellated bacteria that do not ferment lactose*
- This description commonly applies to *Shigella spp.*
- While *Shigella* causes **bloody diarrhea** and **abdominal pain**, it is typically **non-motile** (non-flagellated), whereas *Campylobacter* is motile due to its flagella.
*Gram-negative, non-flagellated bacteria that ferment lactose*
- This description would fit organisms like enteropathogenic *E. coli* (EPEC) or enterotoxigenic *E. coli* (ETEC).
- However, the specific growth conditions (thermophilic) and positive oxidase test pointed to by phenylenediamine reactivity are not characteristic of these organisms.
Bacterial taxonomy and classification US Medical PG Question 7: A 2-year-old boy has a history of recurrent bacterial infections, especially of his skin. When he has an infection, pus does not form. His mother reports that, when he was born, his umbilical cord took 5 weeks to detach. He is ultimately diagnosed with a defect in a molecule in the pathway that results in neutrophil extravasation. Which of the following correctly pairs the defective molecule with the step of extravasation that molecule affects?
- A. E-selectin; transmigration
- B. LFA-1 (integrin); tight adhesion (Correct Answer)
- C. ICAM-1; margination
- D. E-selectin; tight adhesion
- E. PECAM-1; transmigration
Bacterial taxonomy and classification Explanation: ***LFA-1 (integrin); tight adhesion***
- This patient's symptoms (recurrent bacterial infections, lack of pus formation, and delayed umbilical cord separation) are classic for **Leukocyte Adhesion Deficiency type 1 (LAD-1)**.
- **LAD-1** is caused by a defect in the **CD18 subunit** of **β2 integrins**, including **LFA-1** and **Mac-1**, which are crucial for the **tight adhesion** of neutrophils to endothelial cells.
*E-selectin; transmigration*
- **E-selectin** mediates the initial **rolling** of leukocytes along the endothelial surface, not transmigration.
- A defect in E-selectin would impair rolling, but the primary defect in LAD-1 is in tight adhesion.
*ICAM-1; margination*
- **ICAM-1** (Intercellular Adhesion Molecule-1) is an endothelial ligand that binds to integrins on leukocytes, facilitating **tight adhesion** and transmigration, not margination.
- **Margination** refers to the movement of leukocytes to the periphery of the blood vessel lumen.
*E-selectin; tight adhesion*
- **E-selectin** is involved in the initial **rolling** phase of extravasation by binding to sialyl Lewis X on leukocytes.
- It does not primarily mediate **tight adhesion**, which is facilitated by integrins binding to ICAM-1.
*PECAM-1; transmigration*
- **PECAM-1** (Platelet Endothelial Cell Adhesion Molecule-1) is primarily involved in **transmigration** (diapedesis), where leukocytes pass between endothelial cells.
- While important for extravasation, the characteristic findings of LAD-1 point to a defect earlier in the pathway, specifically tight adhesion.
Bacterial taxonomy and classification US Medical PG Question 8: An 8-year-old child is brought to the emergency department because of profuse diarrhea and vomiting that have lasted for 2 days. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. Past medical history is noncontributory. The family recently made a trip to India to visit relatives. Today, his heart rate is 100/min, respiratory rate is 22/min, blood pressure is 105/65 mm Hg, and temperature is 37.2ºC (99.0°F). On physical examination, he appears unwell with poor skin turgor and dry oral mucosa. His heart has a regular rate and rhythm and his lungs are clear to auscultation bilaterally. His abdomen is sensitive to shallow and deep palpation. A gross examination of the stool reveals a 'rice water' appearance. Diagnostic microbiology results are pending. Which of the following is the best diagnostic test to aid in the identification of this patient's condition?
- A. Methylene blue wet mount
- B. Gram stain of stool sample
- C. Dark-field microscopy
- D. Rapid diagnostic test for cholera toxin
- E. Stool culture on TCBS agar (Correct Answer)
Bacterial taxonomy and classification Explanation: ***Stool culture on TCBS agar***
- The patient's symptoms (profuse watery diarrhea, vomiting, dehydration, history of travel to India) strongly suggest **cholera**, caused by *Vibrio cholerae*.
- **Thiosulfate-citrate-bile salts-sucrose (TCBS) agar** is a highly selective medium specifically used for isolating *Vibrio* species.
*Methylene blue wet mount*
- This test is primarily used to identify **white blood cells (leukocytes)** in stool, which indicate an inflammatory process, such as in *Shigella* or *Salmonella* infections.
- Cholera is a **non-inflammatory** diarrhea, so a methylene blue wet mount would likely be negative for leukocytes and therefore not helpful for diagnosis.
*Gram stain of stool sample*
- While Gram stain can classify bacteria, it is generally **not useful for diagnosing diarrheal diseases** caused by specific enteric pathogens, as stool contains a vast array of Gram-negative and Gram-positive bacteria.
- It would be difficult to identify *Vibrio cholerae* among the normal flora using this method alone.
*Dark-field microscopy*
- This technique is typically used to visualize **spirochetes**, such as *Treponema pallidum* (syphilis), due to their characteristic motility and morphology.
- While *Vibrio cholerae* are motile rods, dark-field microscopy is **not the standard or most sensitive method** for its identification in a stool sample, especially compared to selective cultures.
*Rapid diagnostic test for cholera toxin*
- While such tests exist and can be useful in epidemic settings for quick screening, they generally have **lower sensitivity and specificity** compared to culture-based methods.
- **Culture remains the gold standard** for definitive diagnosis, especially for guiding treatment and epidemiological surveillance.
Bacterial taxonomy and classification US Medical PG Question 9: A scientist is studying the process of thymus-dependent B cell activation in humans. He observes that, after bacterial infections, the germinal centers of secondary lymphoid organs become highly metabolically active. After subsequent reinfection with the same pathogen, the organism is able to produce immunoglobulins at a much faster pace. Which of the following processes is likely taking place in the germinal centers at the beginning of an infection?
- A. T cell positive selection
- B. T cell negative selection
- C. Development of early pro-B cells
- D. Development of immature B cells
- E. Affinity maturation (Correct Answer)
Bacterial taxonomy and classification Explanation: ***Affinity maturation***
- This process involves **somatic hypermutation** in the germinal centers, leading to B cells with receptors having higher affinity for the antigen.
- Coupled with **clonal selection**, this ensures that subsequent immune responses are faster and more effective due to the improved binding of antibodies to the pathogen.
*T cell positive selection*
- This process occurs in the **thymic cortex** and selects T cells capable of recognizing self-MHC molecules.
- It is crucial for the development of the T cell repertoire and does not occur in germinal centers during B cell activation.
*T cell negative selection*
- This process takes place primarily in the **thymic medulla** and eliminates T cells that bind too strongly to self-peptide/MHC complexes, preventing autoimmunity.
- It is a central tolerance mechanism and is not related to B cell responses in germinal centers.
*Development of early pro-B cells*
- The development of pro-B cells, and indeed all early stages of B cell development (pro-B, pre-B, immature B), occurs primarily in the **bone marrow**.
- These are early developmental stages, distinct from the antigen-driven processes occurring in secondary lymphoid organs during an infection.
*Development of immature B cells*
- Immature B cells develop from pre-B cells in the **bone marrow** and then migrate to secondary lymphoid organs to complete maturation.
- This step occurs prior to encountering an antigen in the germinal centers and is part of initial B cell development rather than the refinement of the immune response to an infection.
Bacterial taxonomy and classification US Medical PG Question 10: A 42-year-old woman presents to a medical office with complaints of fatigue, weight loss, and low-grade fever for 1 week. She noticed bleeding spots on her feet this morning. The past medical history is significant for a recent dental appointment. She is a non-smoker and does not drink alcohol. She does not currently take any medications. On examination, the vital signs include temperature 37.8°C (100.0°F), blood pressure 138/90 mm Hg, respirations 21/min, and pulse 87/min. Cardiac auscultation reveals a pansystolic murmur in the mitral area with radiation to the left axilla. Laboratory studies show hemoglobin levels of 17.2 g/dL, erythrocyte sedimentation rate (ESR) of 25 mm/h, and a white blood cell (WBC) count of 12,000 cells/mm3. An echocardiogram reveals valvular vegetations on the mitral valve with mild regurgitation. Blood samples are sent for bacterial culture. Empiric antibiotic therapy is initiated with ceftriaxone and vancomycin. The blood cultures most likely will yield the growth of which of the following organisms?
- A. Actinomyces israelii
- B. Coxiella burnetii
- C. Group B Streptococcus
- D. Staphylococcus aureus
- E. Streptococcus viridans (Correct Answer)
Bacterial taxonomy and classification Explanation: ***Streptococcus viridans***
- The patient's recent **dental appointment**, the presence of an **oral organism**, and symptoms consistent with **subacute bacterial endocarditis** (fatigue, fever, weight loss, petechiae) strongly suggest *S. viridans* as the causative agent.
- *Streptococcus viridans* species are common inhabitants of the **oral flora** and are a leading cause of endocarditis following dental procedures, especially in individuals with pre-existing valvular abnormalities.
*Actinomyces israelii*
- While *Actinomyces israelii* is an oral commensal, it typically causes **actinomycosis**, a chronic, suppurative infection characterized by abscess formation and sinus tracts, often following dental procedures.
- It less commonly presents as acute or subacute endocarditis and would not typically cause the rapid progression of symptoms described.
*Coxiella burnetii*
- *Coxiella burnetii* causes **Q fever**, which can manifest as endocarditis, often associated with exposure to **farm animals** or their products.
- The patient's history lacks any such exposure, and the clinical presentation is more aligned with standard bacterial endocarditis from oral flora.
*Group B Streptococcus*
- **Group B Streptococcus** (*Streptococcus agalactiae*) is primarily known as a cause of **neonatal sepsis** and meningitis, and infections in immunocompromised adults or those with underlying conditions like diabetes.
- It is not typically associated with endocarditis following a dental procedure in an otherwise healthy adult.
*Staphylococcus aureus*
- **Staphylococcus aureus** can cause endocarditis, particularly in **intravenous drug users** or patients with prosthetic valves/indwelling lines, and often presents as a more **acute and aggressive disease**.
- While possible, the association with a recent dental procedure and the subacute course makes *Streptococcus viridans* a more likely culprit in this specific scenario.
More Bacterial taxonomy and classification US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.