Bacterial culture methods US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Bacterial culture methods. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Bacterial culture methods US Medical PG Question 1: A 42-year-old woman comes to her primary care physician with 2 days of fever and malaise. She also says that she has a painful red lesion on her left hand that she noticed after shucking oysters at a recent family reunion. Physical exam reveals a well-demarcated swollen, tender, warm, red lesion on her left hand. Pressing the lesion causes a small amount of purulent drainage. The material is cultured and the causative organism is identified. Which of the following characteristics describes the organism that is most associated with this patient's mechanism of infection?
- A. Gram-negative facultative anaerobe (Correct Answer)
- B. Gram-negative aerobe
- C. Gram-positive clusters
- D. Gram-positive chains
- E. Gram-negative anaerobe
Bacterial culture methods Explanation: ***Gram-negative facultative anaerobe***
- This clinical presentation, including oyster exposure and a painful, red hand lesion with purulent drainage, is highly suggestive of infection with **Vibrio vulnificus**.
- **Vibrio vulnificus** is a classic **Gram-negative facultative anaerobe** that thrives in warm, brackish water and is known to cause severe wound infections and sepsis, particularly in individuals who consume raw seafood or have open wounds exposed to contaminated water.
*Gram-negative aerobe*
- While some Gram-negative bacteria are aerobes, a purely aerobic organism would not fit the typical growth characteristics of **Vibrio vulnificus**, which is **facultative anaerobic**.
- No common obligate Gram-negative aerobes are primarily associated with the rapid, severe wound infection seen after oyster exposure.
*Gram-positive clusters*
- **Staphylococcus** species are Gram-positive bacteria that grow in clusters and can cause skin infections, but they are generally not associated with oyster exposure or the rapid progression described.
- The mechanism of infection via oyster shucking points away from typical staphylococcal wound infections.
*Gram-positive chains*
- **Streptococcus** species are Gram-positive bacteria that grow in chains and can cause various infections, including cellulitis, but they are not typically linked to seafood-related wound infections like **Vibrio vulnificus**.
- The clinical context strongly favors a different causative agent.
*Gram-negative anaerobe*
- While there are Gram-negative anaerobes, such as **Bacteroides**, they are primarily found in the gut flora and are less commonly implicated in acute wound infections acquired from environmental exposure like oysters.
- **Vibrio vulnificus** is a **facultative anaerobe**, meaning it can grow with or without oxygen, which is distinct from obligate anaerobes.
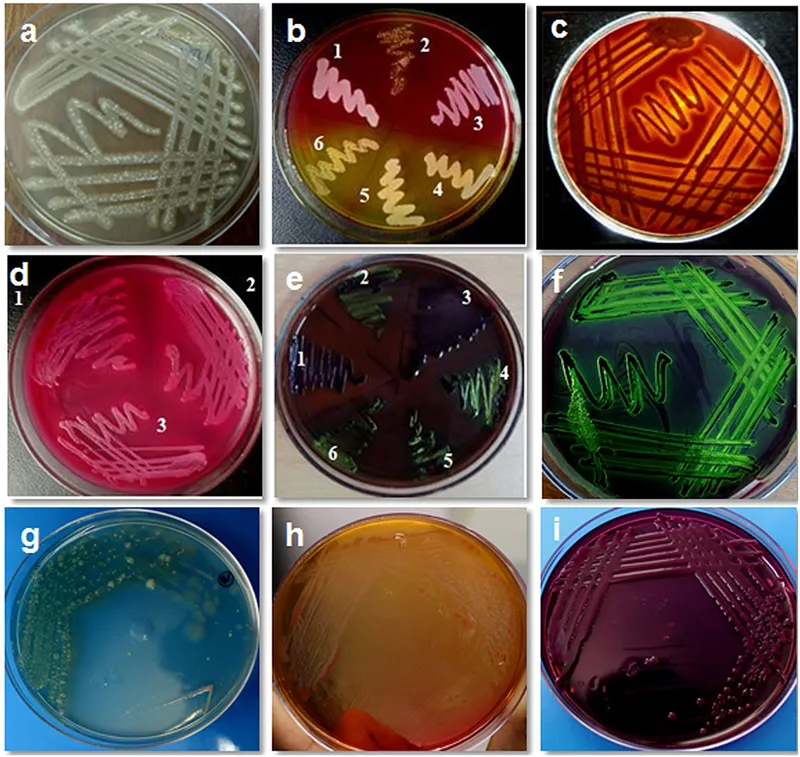
Bacterial culture methods US Medical PG Question 2: A 6-month old child is brought to the ER by parents for one day of fever, decreased feeding, and lethargy. They report that neither she nor her siblings are immunized due to their concerns about vaccinations. On exam, the infant is toxic-appearing. Antibiotics are started and lumbar puncture reveals bacterial meningitis caused by a gram-negative, encapsulated organism that requires chocolate agar and the two factors shown in Image A for growth. Which organism does this best describe?
- A. Group B Streptococcus
- B. Haemophilus influenzae (Correct Answer)
- C. Moraxella catarrhalis
- D. Streptococcus pneumoniae
- E. Listeria monocytogenes
Bacterial culture methods Explanation: **Haemophilus influenzae**
- This organism is a **gram-negative, encapsulated coccobacillus** that requires **chocolate agar** and **factors X (hemin) and V (NAD+)** for growth, which perfectly matches the description.
- In unvaccinated children, *H. influenzae* type b (Hib) is a significant cause of **bacterial meningitis**, epiglottitis, and other invasive infections, especially considering the family's anti-vaccination stance.
*Group B Streptococcus*
- **Group B Streptococcus (GBS)** is a **gram-positive coccus** and a common cause of early-onset neonatal sepsis and meningitis, typically in infants less than 3 months old.
- It does not require chocolate agar or specific growth factors X and V, and is **gram-positive**, not gram-negative.
*Moraxella catarrhalis*
- *Moraxella catarrhalis* is a **gram-negative diplococcus** and a common cause of otitis media, sinusitis, and bronchitis, but it is a rare cause of meningitis.
- While it is a gram-negative organism, it does not typically require chocolate agar or specific growth factors X and V for isolation, usually growing on standard blood agar.
*Streptococcus pneumoniae*
- *Streptococcus pneumoniae* is a **gram-positive coccus** that is a leading cause of bacterial meningitis in children and adults.
- It is **gram-positive**, not gram-negative, and grows on blood agar, not specifically requiring chocolate agar or factors X and V.
*Listeria monocytogenes*
- *Listeria monocytogenes* is a **gram-positive rod** and a cause of meningitis in neonates, immunocompromised individuals, and the elderly.
- It is a **gram-positive rod**, contrary to the gram-negative, encapsulated organism described, and does not require chocolate agar or factors X and V for growth.
Bacterial culture methods US Medical PG Question 3: An investigator is studying a strain of bacteria that retains a blue color after crystal violet dye and acetone are applied. The bacteria are inoculated in a petri dish containing hypotonic saline. After the addition of an antibiotic, the bacteria swell and rupture. This antibiotic most likely belongs to which of the following classes?
- A. Macrolide
- B. Cephalosporin (Correct Answer)
- C. Sulfonamide
- D. Fluoroquinolone
- E. Tetracycline
Bacterial culture methods Explanation: ***Cephalosporin***
- This scenario describes a **Gram-positive bacterium** (retains blue color) which, after antibiotic treatment, swells and lyses in a hypotonic solution. This indicates a defect in the **peptidoglycan cell wall**.
- **Cephalosporins** are **β-lactam antibiotics** that inhibit bacterial cell wall synthesis by interfering with **peptidoglycan cross-linking**, leading to osmotic lysis in hypotonic environments.
*Macrolide*
- Macrolides like **azithromycin** and **erythromycin** inhibit bacterial **protein synthesis** by binding to the 50S ribosomal subunit.
- They do not directly target the cell wall, so they would not cause immediate osmotic lysis in this manner.
*Sulfonamide*
- Sulfonamides inhibit bacterial **folic acid synthesis** by acting as a competitive inhibitor of dihydropteroate synthase, disrupting DNA and RNA production.
- Their mechanism of action does not involve direct cell wall disruption or osmotic lysis.
*Fluoroquinolone*
- Fluoroquinolones interfere with bacterial **DNA replication and transcription** by inhibiting **DNA gyrase** and **topoisomerase IV**.
- This class of antibiotics does not primarily target the cell wall, and therefore would not lead to prompt osmotic swelling and rupture.
*Tetracycline*
- Tetracyclines inhibit bacterial **protein synthesis** by binding to the 30S ribosomal subunit, preventing the attachment of aminoacyl-tRNA.
- They do not affect the cell wall, so they would not cause the observed osmotic lysis.
Bacterial culture methods US Medical PG Question 4: On the 4th day of hospital admission due to pneumonia, a 69-year-old woman develops non-bloody diarrhea and abdominal pain. She is currently treated with ceftriaxone. Despite the resolution of fever after the first 2 days of admission, her temperature is now 38.5°C (101.3°F). On physical examination, she has mild generalized abdominal tenderness without abdominal guarding or rebound tenderness. Laboratory studies show re-elevation of leukocyte counts. Ceftriaxone is discontinued. Given the most likely diagnosis in this patient, which of the following is the most sensitive test?
- A. Nucleic acid amplification test (Correct Answer)
- B. Stool culture for bacterial isolation and toxin presence
- C. Enzyme immunoassay glutamate dehydrogenase
- D. Gram stain of stool sample
- E. Endoscopy
Bacterial culture methods Explanation: ***Nucleic acid amplification test***
- **NAAT** (PCR) for *C. difficile* toxin genes is the most **sensitive** and specific test for routine clinical diagnosis of *C. difficile* infection.
- It detects the **DNA** of toxin-producing *C. difficile* (tcdB gene) and is highly reliable even with low bacterial loads.
- NAAT has become the **gold standard** in most clinical settings due to its rapid turnaround time (hours) and excellent sensitivity (~90-95%) and specificity (~95%).
*Enzyme immunoassay glutamate dehydrogenase*
- **EIA GDH** detects an antigen common to all *C. difficile* strains (both toxin-producing and non-toxin-producing).
- While it has **high sensitivity** (~85-95%), it has **low specificity** and requires confirmation with a toxin test or NAAT, as it cannot distinguish between toxigenic and non-toxigenic strains.
- Often used as part of a **two-step algorithm** for screening.
*Gram stain of stool sample*
- A **Gram stain** of stool is generally not helpful for diagnosing *C. difficile* infection.
- It would show a mix of **gut flora** and would not specifically identify *C. difficile* or its toxins.
*Stool culture for bacterial isolation and toxin presence*
- **Stool culture** for *C. difficile* is technically the most sensitive method (~95-100%) but does not differentiate toxin-producing from non-toxin-producing strains without subsequent **toxin testing**.
- It is also **time-consuming** (2-3 days) and labor-intensive, making it impractical for routine clinical diagnosis.
- Primarily used for **research** or **epidemiological typing**.
*Endoscopy*
- **Endoscopy** with visualization of **pseudomembranes** is highly specific for severe *C. difficile* infection.
- However, it is an **invasive procedure**, not sensitive for mild-to-moderate disease, and is usually reserved for cases where diagnosis is unclear or severe complications (toxic megacolon, fulminant colitis) are suspected.
Bacterial culture methods US Medical PG Question 5: A 12-year-old boy admitted to the intensive care unit 1 day ago for severe pneumonia suddenly develops hypotension. He was started on empiric antibiotics and his blood culture reports are pending. According to the nurse, the patient was doing fine until his blood pressure suddenly dropped. Vital signs include: blood pressure is 88/58 mm Hg, temperature is 39.4°C (103.0°F), pulse is 120/min, and respiratory rate is 24/min. His limbs feel warm. The resident physician decides to start him on intravenous vasopressors, as the blood pressure is not responding to intravenous fluids. The on-call intensivist suspects shock due to a bacterial toxin. What is the primary mechanism responsible for the pathogenesis of this patient's condition?
- A. Inactivation of elongation factor (EF) 2
- B. Inhibition of GABA and glycine
- C. Inhibition of acetylcholine release
- D. Release of tumor necrosis factor (TNF) (Correct Answer)
- E. Degradation of lecithin in cell membranes
Bacterial culture methods Explanation: ***Release of tumor necrosis factor (TNF)***
- The patient's presentation with **warm limbs** and **hypotension** despite fluid resuscitation in the setting of severe pneumonia is highly suggestive of **septic shock**.
- **Bacterial toxins**, particularly **endotoxins** from gram-negative bacteria or **exotoxins** like superantigens, trigger a massive **inflammatory response** by stimulating immune cells to release pro-inflammatory cytokines such as **TNF-α**, IL-1, and IL-6, leading to systemic vasodilation and capillary leak.
*Inactivation of elongation factor (EF) 2*
- This is the mechanism of action of **diphtheria toxin** and **exotoxin A** from *Pseudomonas aeruginosa*.
- While these toxins can cause severe systemic illness, their primary role is not typically the induction of septic shock characterized by widespread vasodilation and warm extremities.
*Inhibition of GABA and glycine*
- This mechanism is characteristic of **tetanus toxin**, which prevents the release of inhibitory neurotransmitters and leads to spastic paralysis.
- This is not consistent with the patient's presentation of septic shock.
*Inhibition of acetylcholine release*
- This is the mechanism of action of **botulinum toxin**, which causes flaccid paralysis by blocking acetylcholine release at the neuromuscular junction.
- This effect is not associated with the pathogenesis of septic shock.
*Degradation of lecithin in cell membranes*
- This mechanism is associated with **alpha toxin** of *Clostridium perfringens* (lecithinase), which causes gas gangrene and hemolysis.
- While this toxin contributes to tissue damage in certain infections, it is not the primary mechanism behind the systemic inflammatory response and vasodilation seen in septic shock.
Bacterial culture methods US Medical PG Question 6: A 42-year-old woman presents to a medical office with complaints of fatigue, weight loss, and low-grade fever for 1 week. She noticed bleeding spots on her feet this morning. The past medical history is significant for a recent dental appointment. She is a non-smoker and does not drink alcohol. She does not currently take any medications. On examination, the vital signs include temperature 37.8°C (100.0°F), blood pressure 138/90 mm Hg, respirations 21/min, and pulse 87/min. Cardiac auscultation reveals a pansystolic murmur in the mitral area with radiation to the left axilla. Laboratory studies show hemoglobin levels of 17.2 g/dL, erythrocyte sedimentation rate (ESR) of 25 mm/h, and a white blood cell (WBC) count of 12,000 cells/mm3. An echocardiogram reveals valvular vegetations on the mitral valve with mild regurgitation. Blood samples are sent for bacterial culture. Empiric antibiotic therapy is initiated with ceftriaxone and vancomycin. The blood cultures most likely will yield the growth of which of the following organisms?
- A. Actinomyces israelii
- B. Coxiella burnetii
- C. Group B Streptococcus
- D. Staphylococcus aureus
- E. Streptococcus viridans (Correct Answer)
Bacterial culture methods Explanation: ***Streptococcus viridans***
- The patient's recent **dental appointment**, the presence of an **oral organism**, and symptoms consistent with **subacute bacterial endocarditis** (fatigue, fever, weight loss, petechiae) strongly suggest *S. viridans* as the causative agent.
- *Streptococcus viridans* species are common inhabitants of the **oral flora** and are a leading cause of endocarditis following dental procedures, especially in individuals with pre-existing valvular abnormalities.
*Actinomyces israelii*
- While *Actinomyces israelii* is an oral commensal, it typically causes **actinomycosis**, a chronic, suppurative infection characterized by abscess formation and sinus tracts, often following dental procedures.
- It less commonly presents as acute or subacute endocarditis and would not typically cause the rapid progression of symptoms described.
*Coxiella burnetii*
- *Coxiella burnetii* causes **Q fever**, which can manifest as endocarditis, often associated with exposure to **farm animals** or their products.
- The patient's history lacks any such exposure, and the clinical presentation is more aligned with standard bacterial endocarditis from oral flora.
*Group B Streptococcus*
- **Group B Streptococcus** (*Streptococcus agalactiae*) is primarily known as a cause of **neonatal sepsis** and meningitis, and infections in immunocompromised adults or those with underlying conditions like diabetes.
- It is not typically associated with endocarditis following a dental procedure in an otherwise healthy adult.
*Staphylococcus aureus*
- **Staphylococcus aureus** can cause endocarditis, particularly in **intravenous drug users** or patients with prosthetic valves/indwelling lines, and often presents as a more **acute and aggressive disease**.
- While possible, the association with a recent dental procedure and the subacute course makes *Streptococcus viridans* a more likely culprit in this specific scenario.
Bacterial culture methods US Medical PG Question 7: A group of microbiological investigators is studying bacterial DNA replication in E. coli colonies. While the cells are actively proliferating, the investigators stop the bacterial cell cycle during S phase and isolate an enzyme involved in DNA replication. An assay of the enzyme's exonuclease activity determines that it is active on both intact and demethylated thymine nucleotides. Which of the following enzymes have the investigators most likely isolated?
- A. DNA ligase
- B. Telomerase
- C. Primase
- D. DNA topoisomerase
- E. DNA polymerase I (Correct Answer)
Bacterial culture methods Explanation: ***DNA polymerase I***
- **DNA polymerase I** possesses **5' to 3' exonuclease activity**, which is crucial for removing **RNA primers** (intact nucleotides) laid down by primase during DNA replication.
- This 5' to 3' exonuclease activity also allows it to excise damaged DNA, including DNA containing **demethylated thymine nucleotides**.
- It also has 3' to 5' exonuclease activity for proofreading.
- **Key distinction:** While DNA polymerase III (the main replicative enzyme) only has 3' to 5' exonuclease activity, DNA polymerase I has **both** 3' to 5' and 5' to 3' exonuclease activities, making it essential for primer removal and DNA repair.
*DNA ligase*
- **DNA ligase** functions to form a **phosphodiester bond** between adjacent nucleotides to seal nicks in the DNA backbone, but it does not have exonuclease activity.
- Its primary role is in joining Okazaki fragments and repairing single-strand breaks.
*Telomerase*
- **Telomerase** is a specialized reverse transcriptase that extends the telomeres at the ends of eukaryotic chromosomes, but is not present in prokaryotes like *E. coli*.
- It uses an RNA template to synthesize DNA, and it lacks exonuclease activity.
*Primase*
- **Primase** is an RNA polymerase that synthesizes short **RNA primers** on the DNA template, providing a starting point for DNA synthesis.
- It is involved in synthesizing primers, not in removing or excising nucleotides, and has no exonuclease activity.
*DNA topoisomerase*
- **DNA topoisomerases** relieve supercoiling in DNA during replication and transcription by cutting and rejoining DNA strands.
- While they act on DNA, their function is to manage topological stress, and they do not exhibit exonuclease activity on nucleotides.
Bacterial culture methods US Medical PG Question 8: A 69-year-old man is brought to the emergency department by his wife because of fever, cough, diarrhea, and confusion for 2 days. He recently returned from a cruise to the Caribbean. He has a history of chronic obstructive pulmonary disease. He has smoked one pack of cigarettes daily for 40 years. His temperature is 39.1°C (102.4°F), pulse is 83/min, and blood pressure is 111/65 mm Hg. He is confused and oriented only to person. Physical examination shows coarse crackles throughout both lung fields. His serum sodium concentration is 125 mEq/L. Culture of the most likely causal organism would require which of the following mediums?
- A. Charcoal yeast extract agar (Correct Answer)
- B. Eosin-methylene blue agar
- C. Mannitol salt agar
- D. Chocolate agar
- E. Eaton agar
Bacterial culture methods Explanation: ***Charcoal yeast extract agar***
- The patient's symptoms (fever, cough, diarrhea, confusion, hyponatremia) and risk factors (COPD, smoking history, recent cruise travel) are highly suggestive of **Legionnaires' disease** caused by *Legionella pneumophila*.
- *Legionella* is a fastidious organism that requires **cysteine** and **iron salts** for growth, which are provided in **buffered charcoal yeast extract (BCYE) agar**.
*Eosin-methylene blue agar*
- This is a **selective and differential medium** used for the isolation and differentiation of **Gram-negative enteric bacteria**, particularly useful for identifying coliforms like *E. coli*.
- It contains dyes that inhibit Gram-positive bacteria and differentiate lactose fermenters, which is not relevant for *Legionella*.
*Mannitol salt agar*
- This is a **selective and differential medium** primarily used for the isolation and identification of **staphylococci**, especially *Staphylococcus aureus*.
- It contains a high salt concentration to inhibit most bacteria and mannitol to differentiate *S. aureus* (which ferments mannitol) from other staphylococci.
*Chocolate agar*
- This enriched medium is used for the isolation of fastidious bacteria such as **Haemophilus influenzae** and **Neisseria species**, which require factors like **hemin (X factor)** and **NAD (V factor)**.
- While it supports the growth of many pathogenic bacteria, it does not provide the specific growth requirements for *Legionella*.
*Eaton agar*
- This specialized medium is primarily used for the isolation and cultivation of **Mycoplasma pneumoniae**, a common cause of "walking pneumonia."
- *Mycoplasma pneumoniae* is a bacterium that lacks a cell wall and has unique growth requirements, distinct from *Legionella*.
Bacterial culture methods US Medical PG Question 9: A 27-year-old woman presents to the clinic with severe pain in her left knee of 1-day duration. Physical examination reveals a red, swollen, warm, and tender left knee with a decreased range of motion. The patient affirms that she has been sexually active with several partners over the last year and that 1 of her partners has complained of dysuria and yellow urethral discharge. An arthrocentesis was performed and showed a WBC count of 60,000/µL, with 90% polymorphonuclear leukocytes. Visualization of the patient's synovial fluid is provided in the image. Which of the following is a characteristic feature of the organism causing this condition?
- A. It causes the Jarisch-Herxheimer reaction when treated with penicillin
- B. It produces a heat-labile toxin that prevents protein synthesis
- C. It selectively grows on Thayer-Martin medium (Correct Answer)
- D. It is a gram-positive diplococcus
- E. It ferments maltose
Bacterial culture methods Explanation: ***It selectively grows on Thayer-Martin medium***
- The patient's presentation with **septic arthritis**, a history of multiple sexual partners, and a partner with symptoms of **urethritis** suggests **gonococcal arthritis** caused by *Neisseria gonorrhoeae*.
- *Neisseria gonorrhoeae* is a fastidious organism that requires an enriched selective medium like **Thayer-Martin agar** for optimal growth, which contains antimicrobial agents to inhibit commensal flora.
*It causes the Jarisch-Herxheimer reaction when treated with penicillin*
- The **Jarisch-Herxheimer reaction** is typically associated with treatment of **spirochetal diseases** like **syphilis** (caused by *Treponema pallidum)* or **Lyme disease** (caused by *Borrelia burgdorferi*) with penicillin.
- This reaction results from the rapid lysis of spirochetes and the release of endotoxins, which is not characteristic of gonococcal infection or its treatment.
*It produces a heat-labile toxin that prevents protein synthesis*
- This description is characteristic of toxins produced by organisms like **diphtheria toxin** (*Corynebacterium diphtheriae*) or **Shiga toxin** (*Shigella dysenteriae* and enterohemorrhagic *E. coli*), which inhibit protein synthesis but are not associated with *Neisseria gonorrhoeae*.
- *Neisseria gonorrhoeae* possesses virulence factors like pili, Opa proteins, and LOS, but its primary pathogenicity mechanism does not involve a heat-labile toxin that prevents protein synthesis.
*It is a gram-positive diplococcus*
- The image clearly shows **gram-negative diplococci** within phagocytes (neutrophils), which is a classic microscopic finding for *Neisseria gonorrhoeae*.
- *Neisseria gonorrhoeae* is specifically a **Gram-negative organism**, not Gram-positive.
*It ferments maltose*
- *Neisseria gonorrhoeae* metabolizes **glucose only** and does not ferment maltose, which helps differentiate it from *Neisseria meningitidis* (which ferments both glucose and maltose).
- This metabolic characteristic is a key biochemical test used in the laboratory for the identification of *Neisseria* species.
Bacterial culture methods US Medical PG Question 10: A 45-year-old man is brought to the emergency department after being found down outside of a bar. He does not have any identifying information and is difficult to arouse. On presentation, his temperature is 101.2°F (38.4°C), blood pressure is 109/72 mmHg, pulse is 102/min, and respirations are 18/min. Physical exam reveals an ill-appearing and disheveled man with labored breathing and coughing productive of viscous red sputum. Lung auscultation demonstrates consolidation of the left upper lobe of the patient. Given these findings, cultures are obtained and broad spectrum antibiotics are administered. Which of the following agar types should be used to culture the most likely organism in this case?
- A. Charcoal yeast extract agar
- B. Blood agar
- C. MacConkey agar (Correct Answer)
- D. Eaton agar
- E. Löwenstein-Jensen agar
Bacterial culture methods Explanation: ***MacConkey agar***
- The patient's presentation with **viscous red "currant jelly" sputum**, **upper lobe consolidation**, and history of **alcohol use** is classic for pneumonia caused by ***Klebsiella pneumoniae***.
- **MacConkey agar** is a selective and differential medium used to isolate **gram-negative bacteria** such as *Klebsiella pneumoniae*, which appears as mucoid, lactose-fermenting (pink) colonies.
- The "currant jelly sputum" is pathognomonic for *Klebsiella* and distinguishes it from other pneumonias.
*Blood agar*
- While blood agar is a rich, non-selective medium that supports growth of many organisms including *Streptococcus pneumoniae*, it is not the most appropriate choice for this case.
- *Streptococcus pneumoniae* typically causes **rust-colored sputum**, not the viscous red sputum described here.
- Though *Klebsiella* can grow on blood agar, **MacConkey agar** is more specific for identifying gram-negative organisms like *Klebsiella*.
*Charcoal yeast extract agar*
- This medium is specifically designed for the isolation of **Legionella species**, which are fastidious gram-negative rods.
- *Legionella* pneumonia typically presents with relative bradycardia, hyponatremia, and diarrhea, not the viscous red sputum characteristic of *Klebsiella*.
*Löwenstein-Jensen agar*
- This specialized medium is used for the isolation of **mycobacteria**, particularly *Mycobacterium tuberculosis*.
- TB typically presents with chronic symptoms (weeks to months), night sweats, and hemoptysis, not the acute presentation with viscous red sputum seen here.
*Eaton agar*
- This specialized medium is used for the isolation of **Mycoplasma pneumoniae**, which causes "walking pneumonia."
- *Mycoplasma* pneumonia is typically mild with dry cough and patchy infiltrates, not the severe lobar consolidation and viscous red sputum seen in this case.
More Bacterial culture methods US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.