Bacterial cell structure and physiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Bacterial cell structure and physiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Bacterial cell structure and physiology US Medical PG Question 1: The surgical equipment used during a craniectomy is sterilized using pressurized steam at 121°C for 15 minutes. Reuse of these instruments can cause transmission of which of the following pathogens?
- A. Non-enveloped viruses
- B. Sporulating bacteria
- C. Prions (Correct Answer)
- D. Enveloped viruses
- E. Yeasts
Bacterial cell structure and physiology Explanation: ***Prions***
- Prions are **abnormally folded proteins** that are highly resistant to standard sterilization methods like steam autoclaving at 121°C, making them a risk for transmission through reused surgical instruments.
- They cause transmissible spongiform encephalopathies (TSEs) like **Creutzfeldt-Jakob disease**, where even trace amounts can be highly infectious.
*Non-enveloped viruses*
- Non-enveloped viruses are generally **more resistant to heat and disinfectants** than enveloped viruses but are typically inactivated by recommended steam sterilization protocols.
- Standard autoclaving conditions are effective in destroying most non-enveloped viruses.
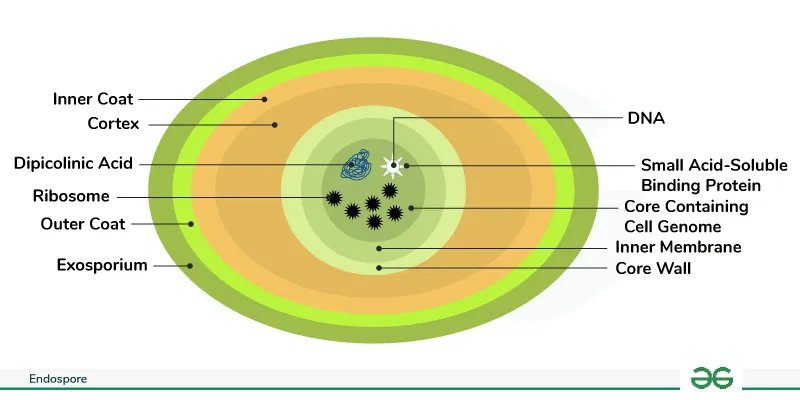
*Sporulating bacteria*
- **Bacterial spores**, such as those from *Clostridium* or *Bacillus*, are known for their high resistance to heat and chemicals, but are usually **inactivated by steam sterilization at 121°C** for 15 minutes.
- This method is specifically designed to kill bacterial spores effectively.
*Enveloped viruses*
- Enveloped viruses are the **least resistant to heat and chemical disinfectants** due to their lipid envelope.
- They are readily **inactivated by standard steam sterilization** at 121°C.
*Yeasts*
- **Yeasts** are eukaryotic microorganisms that are typically **susceptible to heat sterilization**.
- They are effectively killed by typical steam autoclaving conditions used for surgical instruments.
Bacterial cell structure and physiology US Medical PG Question 2: Part of the success of the Streptococcus pyogenes bacterium lies in its ability to evade phagocytosis. Which of the following helps in this evasion?
- A. Streptolysin S
- B. Streptolysin O
- C. Streptokinase
- D. M protein (Correct Answer)
- E. Pyrogenic toxin
Bacterial cell structure and physiology Explanation: ***M protein***
- The **M protein** is a major virulence factor of *Streptococcus pyogenes* that **inhibits phagocytosis** by binding to factor H, a host complement regulatory protein, preventing C3b deposition.
- It also helps the bacterium adhere to host cells and resist killing by neutrophils.
*Streptolysin S*
- **Streptolysin S** is a **hemolysin** that causes beta-hemolysis on blood agar and contributes to tissue damage by lysing cells.
- While contributing to virulence, its primary role is not direct inhibition of phagocytosis but rather cell lysis.
*Streptolysin O*
- **Streptolysin O (SLO)** is another **hemolysin** that produces pore-forming toxins, leading to cell lysis and tissue destruction.
- It is highly antigenic and often used as a diagnostic marker (ASO titer) for past *S. pyogenes* infections, but it does not directly prevent phagocytosis.
*Streptokinase*
- **Streptokinase** is an enzyme that activates plasminogen, leading to the breakdown of fibrin clots, which helps in the **spread of infection** within tissues.
- Its main function is not to evade phagocytosis but rather to facilitate invasion by dissolving blood clots that would typically wall off the infection.
*Pyrogenic toxin*
- **Pyrogenic toxins** (also known as erythrogenic toxins) are superantigens that cause symptoms like fever and rash (e.g., in scarlet fever) by stimulating a massive, non-specific T-cell activation.
- These toxins contribute to the systemic manifestations of infection but do not directly interfere with the process of phagocytosis.
Bacterial cell structure and physiology US Medical PG Question 3: An investigator is studying the growth of an organism in different media. The organism is inoculated on a petri dish that contains heated sheep blood, vancomycin, nystatin, trimethoprim, and colistin. The resulting growth medium is incubated at 37°C. Numerous small, white colonies are seen after incubation for 48 hours. This organism is most likely to cause which of the following conditions?
- A. Pontiac fever
- B. Pseudomembranous colitis
- C. Hemolytic uremic syndrome
- D. Oral thrush
- E. Gonorrhea (Correct Answer)
Bacterial cell structure and physiology Explanation: ***Gonorrhea***
- The growth medium described is **Thayer-Martin agar**, a selective medium containing **heated sheep blood** (supplies NAD+), **vancomycin** (inhibits Gram-positives), **colistin** (inhibits Gram-negatives), **nystatin** (inhibits fungi), and **trimethoprim** (inhibits Proteus). This medium is specifically designed for the isolation of *Neisseria gonorrhoeae* from polymicrobial samples.
- *Neisseria gonorrhoeae* typically grows as **small, translucent-to-white colonies** on selective media like Thayer-Martin agar, and incubation at 37°C in CO2 (not explicitly mentioned but often required) for 24-48 hours yields visible growth, causing **gonorrhea**.
*Pontiac fever*
- Pontiac fever is a mild, self-limiting form of **legionellosis**, caused by *Legionella pneumophila*.
- *Legionella* requires a specialized medium such as **buffered charcoal yeast extract (BCYE) agar** for growth, not Thayer-Martin agar.
*Pseudomembranous colitis*
- This condition is caused by **toxin-producing *Clostridioides difficile***, often after antibiotic use.
- *C. difficile* is an obligate anaerobe and requires **anaerobic conditions** and specific selective media (e.g., CCFA agar) for isolation, not Thayer-Martin agar under aerobic conditions.
*Hemolytic uremic syndrome*
- Hemolytic uremic syndrome (HUS) is often caused by **Shiga toxin-producing *Escherichia coli* (STEC)**, particularly O157:H7.
- STEC can be isolated on media like **sorbitol MacConkey agar (SMAC)**, where O157:H7 appears as non-sorbitol fermenting colonies, distinct from the growth seen on Thayer-Martin.
*Oral thrush*
- Oral thrush is caused by *Candida albicans*, a yeast.
- *Candida* would be inhibited by **nystatin** in the Thayer-Martin medium, which is an antifungal agent.
Bacterial cell structure and physiology US Medical PG Question 4: An 18-year-old college student seeks evaluation at an emergency department with complaints of fevers with chills, fatigue, diarrhea, and loss of appetite, which have lasted for 1 week. He says that his symptoms are progressively getting worse. He was taking over-the-counter acetaminophen, but it was ineffective. The past medical history is insignificant. His temperature is 38.8°C (101.9°F) and his blood pressure is 100/65 mm Hg. The physical examination is within normal limits, except that the patient appears ill. Eventually, a diagnosis of typhoid fever was established and he is started on appropriate antibiotics. Which of the following cellular components is most likely to be responsible for the toxic symptoms in this patient?
- A. Pili on the bacterial cell surface
- B. Lipid A - a toxic component present in the bacterial cell wall (Correct Answer)
- C. Flagella
- D. Toxins secreted by the bacteria
- E. Outer capsule
Bacterial cell structure and physiology Explanation: ***Lipid A - a toxic component present in the bacterial cell wall***
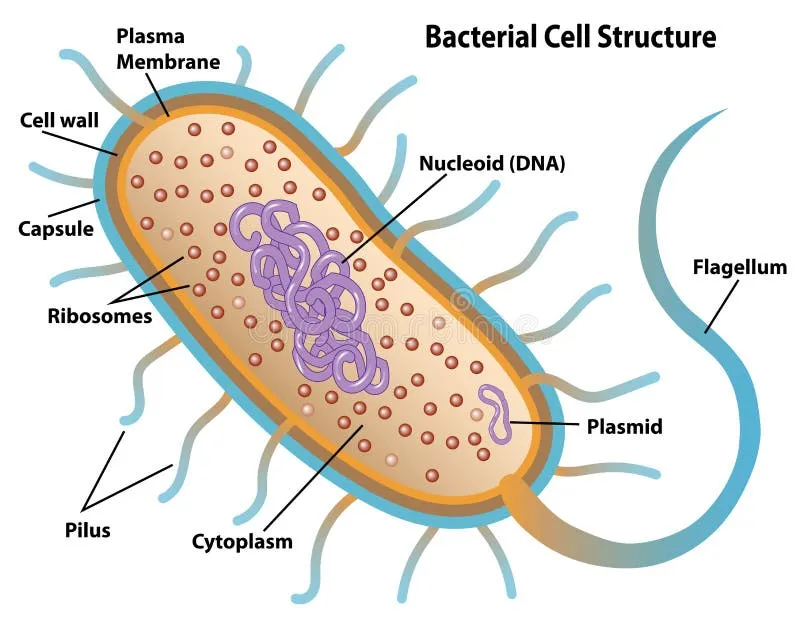
- The toxic symptoms of typhoid fever, caused by *Salmonella Typhi*, are primarily due to **endotoxins**. **Lipid A** is the toxic component of **lipopolysaccharide (LPS)**, which is an endotoxin found in the outer membrane of Gram-negative bacteria like *Salmonella*.
- When bacteria are lysed, LPS is released, triggering a strong immune response that leads to fever, chills, hypotension, and systemic inflammation characteristic of **septic shock** or severe infections.
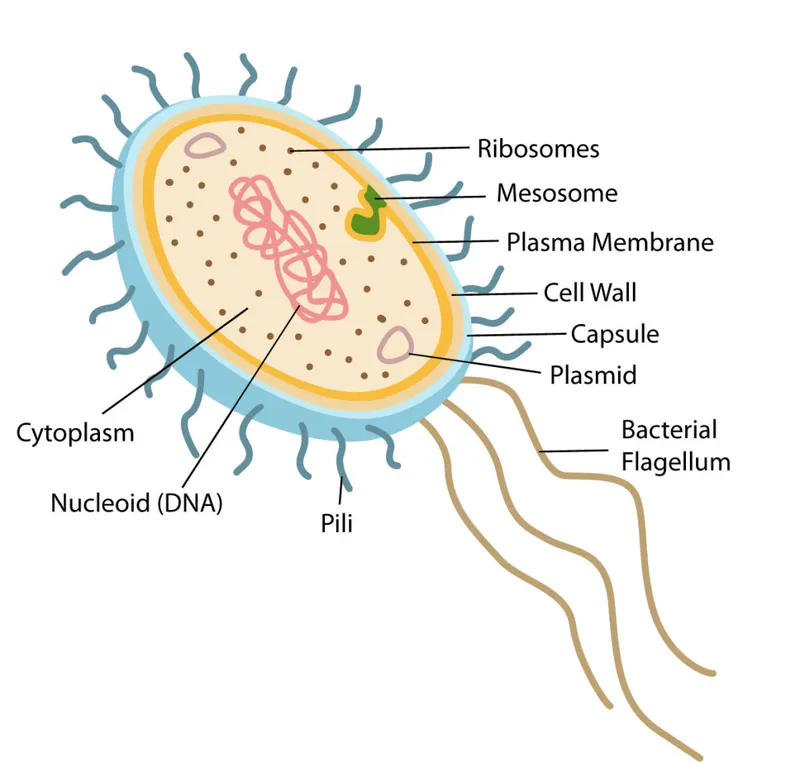
*Pili on the bacterial cell surface*
- **Pili** (fimbriae) are hair-like appendages responsible for **bacterial adherence** to host cells and surfaces, facilitating colonization.
- While important for establishing infection, pili themselves are not directly responsible for the **toxic systemic symptoms** like fever and hypotension.
*Flagella*
- **Flagella** are whip-like structures primarily involved in **bacterial motility**, allowing the bacteria to move through fluids.
- They are essential for bacterial dissemination within the host but do not directly cause the **toxic effects** associated with severe systemic infections.
*Toxins secreted by the bacteria*
- While some bacteria secrete exotoxins that cause disease, the primary toxic component in **Gram-negative infections** like typhoid fever is the **endotoxin (LPS)**, which is part of the cell wall and released upon bacterial lysis, not actively secreted from living bacteria.
- *Salmonella Typhi* does not produce potent exotoxins that cause the main systemic manifestations observed in typhoid fever.
*Outer capsule*
- The **outer capsule** is a protective layer that helps bacteria evade phagocytosis and contributes to **virulence** by offering immune evasion.
- While critical for bacterial survival and pathogenicity, the capsule itself is not directly responsible for triggering the **toxic inflammatory response** that causes the symptoms of septic shock.
Bacterial cell structure and physiology US Medical PG Question 5: A previously healthy 17-year-old boy is brought to the emergency department because of fever, nausea, and myalgia for the past day. His temperature is 39.5°C (103.1°F), pulse is 112/min, and blood pressure is 77/55 mm Hg. Physical examination shows scattered petechiae over the anterior chest and abdomen. Blood culture grows an organism on Thayer-Martin agar. Which of the following virulence factors of the causal organism is most likely responsible for the high mortality rate associated with it?
- A. Immunoglobulin A protease
- B. Lipooligosaccharide (Correct Answer)
- C. Toxic shock syndrome toxin-1
- D. Lipoteichoic acid
- E. Erythrogenic exotoxin A
Bacterial cell structure and physiology Explanation: ***Lipooligosaccharide***
- The patient's presentation with **fever**, **hypotension**, and **petechiae**, along with a positive blood culture on Thayer-Martin agar, points to **meningococcemia** caused by *Neisseria meningitidis*.
- **Lipooligosaccharide (LOS)** acts as an **endotoxin**, triggering an excessive inflammatory response that leads to widespread vascular damage, **capillary leakage**, and **septic shock**, accounting for the high mortality.
*Immunoglobulin A protease*
- While *N. meningitidis* produces **IgA protease** to cleave secretory IgA and evade host defenses on mucosal surfaces, this factor is primarily involved in colonization and initial invasion rather than the systemic severity and mortality of septic shock.
- Its role is to help the bacteria **adhere and penetrate** host mucous membranes, but it does not directly cause the shock and petechiae seen in this severe presentation.
*Toxic shock syndrome toxin-1*
- **Toxic shock syndrome toxin-1 (TSST-1)** is a **superantigen** produced by *Staphylococcus aureus* that causes **toxic shock syndrome**, which can present with fever, rash, and hypotension.
- However, the organism grown on **Thayer-Martin agar** is characteristic of *Neisseria meningitidis*, not *Staphylococcus aureus*.
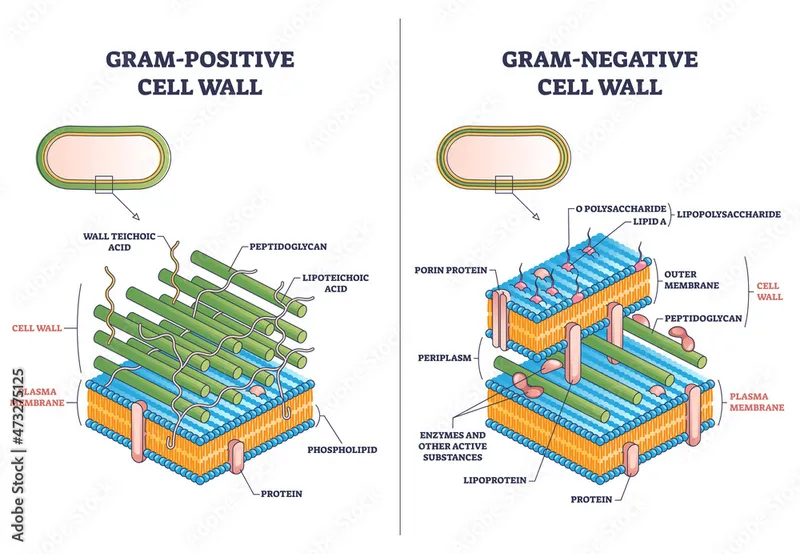
*Lipoteichoic acid*
- **Lipoteichoic acid** is a major component of the cell wall of **Gram-positive bacteria**, acting as a potent proinflammatory molecule and contributing to septic shock in those infections.
- *Neisseria meningitidis* is a **Gram-negative bacterium**, and therefore does not possess lipoteichoic acid.
*Erythrogenic exotoxin A*
- **Erythrogenic exotoxin A** is primarily produced by ***Streptococcus pyogenes*** and is responsible for the characteristic rash of **scarlet fever**.
- While *S. pyogenes* can cause invasive infections, the clinical picture and the specific growth on **Thayer-Martin agar** are not consistent with streptococcal infection.
Bacterial cell structure and physiology US Medical PG Question 6: While testing various strains of Streptococcus pneumoniae, a researcher discovers that a certain strain of this bacteria is unable to cause disease in mice when deposited in their lungs. What physiological test would most likely deviate from normal in this strain of bacteria as opposed to a typical strain?
- A. Quellung reaction (Correct Answer)
- B. Hemolytic reaction when grown on sheep blood agar
- C. Bile solubility
- D. Optochin sensitivity
- E. Motility
Bacterial cell structure and physiology Explanation: ***Quellung reaction***
- The **Quellung reaction** tests for the presence of the **polysaccharide capsule**, which is the primary virulence factor of *S. pneumoniae*.
- An **avirulent strain** that cannot cause disease would most likely lack the capsule and show a **negative Quellung reaction** (no capsular swelling), deviating from the **positive reaction** seen in typical encapsulated pathogenic strains.
- The capsule enables *S. pneumoniae* to evade phagocytosis and complement-mediated killing, which is essential for establishing infection in the lungs.
*Hemolytic reaction when grown on sheep blood agar*
- Both virulent and avirulent strains of *S. pneumoniae* typically exhibit **alpha-hemolysis** (partial hemolysis, producing a greenish discoloration) on sheep blood agar due to the production of pneumolysin.
- This characteristic does not differentiate between pathogenic and non-pathogenic strains in terms of disease-causing ability.
*Bile solubility*
- *S. pneumoniae* is characteristically **bile-soluble** due to the presence of autolysin enzymes that are activated by bile salts, leading to cellular lysis.
- This property is a **species characteristic** present in both virulent and avirulent strains, thus it would not explain the inability to cause disease.
*Optochin sensitivity*
- *S. pneumoniae* is universally **sensitive to optochin**, a chemical agent that inhibits its growth and is used for laboratory identification.
- This characteristic is used for **species identification** but does not correlate with strain virulence or disease-causing ability.
*Motility*
- *Streptococcus pneumoniae* is a **non-motile** bacterium; it lacks flagella.
- This characteristic is consistent across all strains and is not a virulence factor for this species.
Bacterial cell structure and physiology US Medical PG Question 7: An investigator is studying a strain of bacteria that retains a blue color after crystal violet dye and acetone are applied. The bacteria are inoculated in a petri dish containing hypotonic saline. After the addition of an antibiotic, the bacteria swell and rupture. This antibiotic most likely belongs to which of the following classes?
- A. Macrolide
- B. Cephalosporin (Correct Answer)
- C. Sulfonamide
- D. Fluoroquinolone
- E. Tetracycline
Bacterial cell structure and physiology Explanation: ***Cephalosporin***
- This scenario describes a **Gram-positive bacterium** (retains blue color) which, after antibiotic treatment, swells and lyses in a hypotonic solution. This indicates a defect in the **peptidoglycan cell wall**.
- **Cephalosporins** are **β-lactam antibiotics** that inhibit bacterial cell wall synthesis by interfering with **peptidoglycan cross-linking**, leading to osmotic lysis in hypotonic environments.
*Macrolide*
- Macrolides like **azithromycin** and **erythromycin** inhibit bacterial **protein synthesis** by binding to the 50S ribosomal subunit.
- They do not directly target the cell wall, so they would not cause immediate osmotic lysis in this manner.
*Sulfonamide*
- Sulfonamides inhibit bacterial **folic acid synthesis** by acting as a competitive inhibitor of dihydropteroate synthase, disrupting DNA and RNA production.
- Their mechanism of action does not involve direct cell wall disruption or osmotic lysis.
*Fluoroquinolone*
- Fluoroquinolones interfere with bacterial **DNA replication and transcription** by inhibiting **DNA gyrase** and **topoisomerase IV**.
- This class of antibiotics does not primarily target the cell wall, and therefore would not lead to prompt osmotic swelling and rupture.
*Tetracycline*
- Tetracyclines inhibit bacterial **protein synthesis** by binding to the 30S ribosomal subunit, preventing the attachment of aminoacyl-tRNA.
- They do not affect the cell wall, so they would not cause the observed osmotic lysis.
Bacterial cell structure and physiology US Medical PG Question 8: A group of scientists studied the effects of cytokines on effector cells, including leukocytes. They observed that interleukin-12 (IL-12) is secreted by antigen-presenting cells (APCs) in response to bacterial lipopolysaccharide. When a CD4+ T cell is exposed to this interleukin, which of the following responses will it have?
- A. Responds to extracellular pathogens
- B. Cell-mediated immune responses (Correct Answer)
- C. Releases granzymes
- D. Activate B cells
- E. Secrete IL-4
Bacterial cell structure and physiology Explanation: ***Cell-mediated immune responses***
- **IL-12** from antigen-presenting cells promotes the differentiation of **naïve CD4+ T cells** into **Th1 cells**.
- **Th1 cells** are the primary drivers of **cell-mediated immunity**, producing cytokines like **IFN-γ** that activate macrophages and cytotoxic T cells to combat intracellular pathogens.
*Responds to extracellular pathogens*
- Responses to extracellular pathogens are primarily mediated by **Th2 cells** and **humoral immunity**.
- **Th2 cells** are induced by cytokines like **IL-4** and are involved in allergic reactions and antiparasitic responses.
*Releases granzymes*
- **Granzymes** are released by **cytotoxic T lymphocytes (CTLs)** and **natural killer (NK) cells** to induce apoptosis in infected or cancerous cells.
- While Th1 cells help activate CTLs, they do not directly release granzymes themselves.
*Activate B cells*
- **B cell activation** and antibody production are primarily driven by **Th2 cells** and **follicular helper T (Tfh) cells**.
- Th1 cells are more involved in responses against intracellular pathogens, which typically do not involve direct B cell activation.
*Secrete IL-4*
- **IL-4** is the signature cytokine of **Th2 cells**, which are primarily involved in humoral immunity and allergic responses.
- **IL-12** inhibits Th2 differentiation and promotes Th1 differentiation, so a CD4+ T cell exposed to IL-12 would not secrete IL-4.
Bacterial cell structure and physiology US Medical PG Question 9: A scientist is studying the process of thymus-dependent B cell activation in humans. He observes that, after bacterial infections, the germinal centers of secondary lymphoid organs become highly metabolically active. After subsequent reinfection with the same pathogen, the organism is able to produce immunoglobulins at a much faster pace. Which of the following processes is likely taking place in the germinal centers at the beginning of an infection?
- A. T cell positive selection
- B. T cell negative selection
- C. Development of early pro-B cells
- D. Development of immature B cells
- E. Affinity maturation (Correct Answer)
Bacterial cell structure and physiology Explanation: ***Affinity maturation***
- This process involves **somatic hypermutation** in the germinal centers, leading to B cells with receptors having higher affinity for the antigen.
- Coupled with **clonal selection**, this ensures that subsequent immune responses are faster and more effective due to the improved binding of antibodies to the pathogen.
*T cell positive selection*
- This process occurs in the **thymic cortex** and selects T cells capable of recognizing self-MHC molecules.
- It is crucial for the development of the T cell repertoire and does not occur in germinal centers during B cell activation.
*T cell negative selection*
- This process takes place primarily in the **thymic medulla** and eliminates T cells that bind too strongly to self-peptide/MHC complexes, preventing autoimmunity.
- It is a central tolerance mechanism and is not related to B cell responses in germinal centers.
*Development of early pro-B cells*
- The development of pro-B cells, and indeed all early stages of B cell development (pro-B, pre-B, immature B), occurs primarily in the **bone marrow**.
- These are early developmental stages, distinct from the antigen-driven processes occurring in secondary lymphoid organs during an infection.
*Development of immature B cells*
- Immature B cells develop from pre-B cells in the **bone marrow** and then migrate to secondary lymphoid organs to complete maturation.
- This step occurs prior to encountering an antigen in the germinal centers and is part of initial B cell development rather than the refinement of the immune response to an infection.
Bacterial cell structure and physiology US Medical PG Question 10: A 3-year-old boy is brought to the physician for evaluation of a generalized, pruritic rash. The rash began during infancy and did not resolve despite initiating treatment with topical corticosteroids. Three months ago, he was treated for several asymptomatic soft tissue abscesses on his legs. He has been admitted to the hospital three times during the past two years for pneumonia. Physical examination shows a prominent forehead and a wide nasal bridge. Examination of the skin shows a diffuse eczematous rash and white plaques on the face, scalp, and shoulders. Laboratory studies show a leukocyte count of 6,000/mm3 with 25% eosinophils and a serum IgE concentration of 2,300 IU/mL (N = 0–380). Flow cytometry shows a deficiency of T helper 17 cells. The patient’s increased susceptibility to infection is most likely due to which of the following?
- A. Impaired Ig class-switching in lymphocytes
- B. Impaired DNA repair in lymphocytes
- C. Impaired actin assembly in lymphocytes
- D. Impaired chemotaxis of neutrophils
- E. Impaired IL-17 secretion by Th17 cells (Correct Answer)
Bacterial cell structure and physiology Explanation: ***Impaired IL-17 secretion by Th17 cells***
- The combination of **eczematous rash**, recurrent **skin abscesses**, recurrent **pneumonia**, **eosinophilia**, high **IgE levels**, and **dysmorphic facial features** (prominent forehead, wide nasal bridge) is characteristic of **hyper-IgE syndrome (Job's syndrome)**.
- The question explicitly states **deficiency of T helper 17 cells** on flow cytometry, which directly explains the mechanism of infection susceptibility.
- Hyper-IgE syndrome is caused by a defect in the **STAT3 signaling pathway**, which leads to **impaired Th17 cell differentiation and function**, resulting in reduced production of **IL-17** and **IL-22**, crucial cytokines for antifungal and antibacterial immunity, particularly against **Staphylococcus aureus** and **Candida**.
*Impaired Ig class-switching in lymphocytes*
- This is characteristic of **Hyper-IgM Syndrome**, where patients typically have normal or elevated IgM but very low levels of IgG, IgA, and IgE due to defects in **CD40-CD40L interaction** or AID enzyme.
- While patients with Hyper-IgM syndrome also suffer from recurrent infections, their primary issue is usually with **opportunistic infections** and they don't typically present with the specific dermatological and facial features seen here.
*Impaired DNA repair in lymphocytes*
- This refers to conditions like **Ataxia-telangiectasia**, which involves defects in DNA repair mechanisms and leads to immunodeficiency, **ataxia**, and **telangiectasias**.
- The clinical presentation of severe eczema, recurrent abscesses, and elevated IgE is not typical of **Ataxia-telangiectasia**.
*Impaired actin assembly in lymphocytes*
- This is characteristic of **Wiskott-Aldrich Syndrome**, which results from a defect in the **WASp gene** leading to impaired actin polymerization and cell motility.
- Patients typically present with **thrombocytopenia** (leading to bleeding issues), **eczema**, and recurrent infections; however, the elevated IgE and specific infections (abscesses, pneumonia) are more suggestive of hyper-IgE syndrome than the general immunodeficiency of Wiskott-Aldrich.
*Impaired chemotaxis of neutrophils*
- This is a feature of **Leukocyte Adhesion Deficiency (LAD)** or **Chediak-Higashi syndrome**.
- In LAD, neutrophils cannot extravasate to infection sites, leading to recurrent infections without pus formation and **delayed umbilical cord separation**, which is not described. In Chediak-Higashi, there are also giant lysosomes and partial albinism.
More Bacterial cell structure and physiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.