Treponema pallidum US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Treponema pallidum. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Treponema pallidum US Medical PG Question 1: A 45-year-old man presents with a long history of ulcers on the bottom of his feet. He recalls having a similar looking ulcer on the side of his penis when he was 19 years old for which he never sought treatment. The patient denies any fever, chills, or constitutional symptoms. He reports multiple sexual partners and a very promiscuous sexual history. He has also traveled extensively as a writer since he was 19. The patient is afebrile, and his vital signs are within normal limits. A rapid plasma reagin (RPR) test is positive, and the result of a Treponema pallidum particle agglutination (TP-PA) is pending. Which of the following findings would most likely be present in this patient?
- A. Hyperreflexia
- B. Memory loss
- C. Wide-based gait with a low step
- D. Positive Romberg's sign (Correct Answer)
- E. Agraphesthesia
Treponema pallidum Explanation: ***Positive Romberg's sign***
- The patient's history of untreated penile ulcers at age 19, extensive sexual history, and positive RPR strongly suggest **late-stage syphilis** [3].
- A positive Romberg's sign indicates **sensory ataxia**, which is a classic finding in **tabes dorsalis**, a manifestation of neurosyphilis involving degeneration of the dorsal columns and dorsal roots of the spinal cord [1].
*Hyperreflexia*
- **Hyperreflexia** is typically seen in **upper motor neuron lesions**, while tabes dorsalis primarily affects the **sensory pathways** (dorsal columns), leading to sensory deficits rather than motor spasticity.
- In some neurosyphilis cases, **hyporeflexia or areflexia** may be observed due to damage to the dorsal roots.
*Memory loss*
- **Memory loss** can occur in neurosyphilis, particularly in conditions like **general paresis**, which is a form of neurosyphilis affecting the cerebral cortex [3].
- However, the symptom of **foot ulcers** points more directly to sensory neuropathy, making **ataxia** (and thus Romberg's sign) a more likely direct neurological finding.
*Wide-based gait with a low step*
- A **wide-based gait with a high stepping (steppage) gait** is characteristic of **foot drop** or **motor neuropathy**, which is less typical for tabes dorsalis.
- A **wide-based gait** can occur in tabes dorsalis due to **sensory ataxia** [2], but the "low step" component is less specific compared to the clear indication of sensory loss by Romberg's sign.
*Agraphesthesia*
- **Agraphesthesia** (inability to recognize writing on the skin) is a sign of **parietal lobe dysfunction** or severe sensory pathway damage.
- While neurosyphilis can affect various parts of the CNS, **tabes dorsalis** primarily causes problems with proprioception and vibratory sense, leading to ataxia and a positive Romberg's sign.
Treponema pallidum US Medical PG Question 2: A 26-year-old immigrant from Mexico presents to your clinic for a physical. He tells you that several weeks ago, he noticed a lesion on his penis which went away after several weeks. It was nontender and did not bother him. He currently does not have any complaints. His temperature is 97.9°F (36.6°C), blood pressure is 139/91 mmHg, pulse is 87/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam is unremarkable and shows no evidence of any rash. A VDRL and FTA-ABS test are both positive. What is the most appropriate management of this patient?
- A. Penicillin (Correct Answer)
- B. Doxycycline
- C. No treatment indicated
- D. Acyclovir
- E. Azithromycin and ceftriaxone
Treponema pallidum Explanation: ***Penicillin***
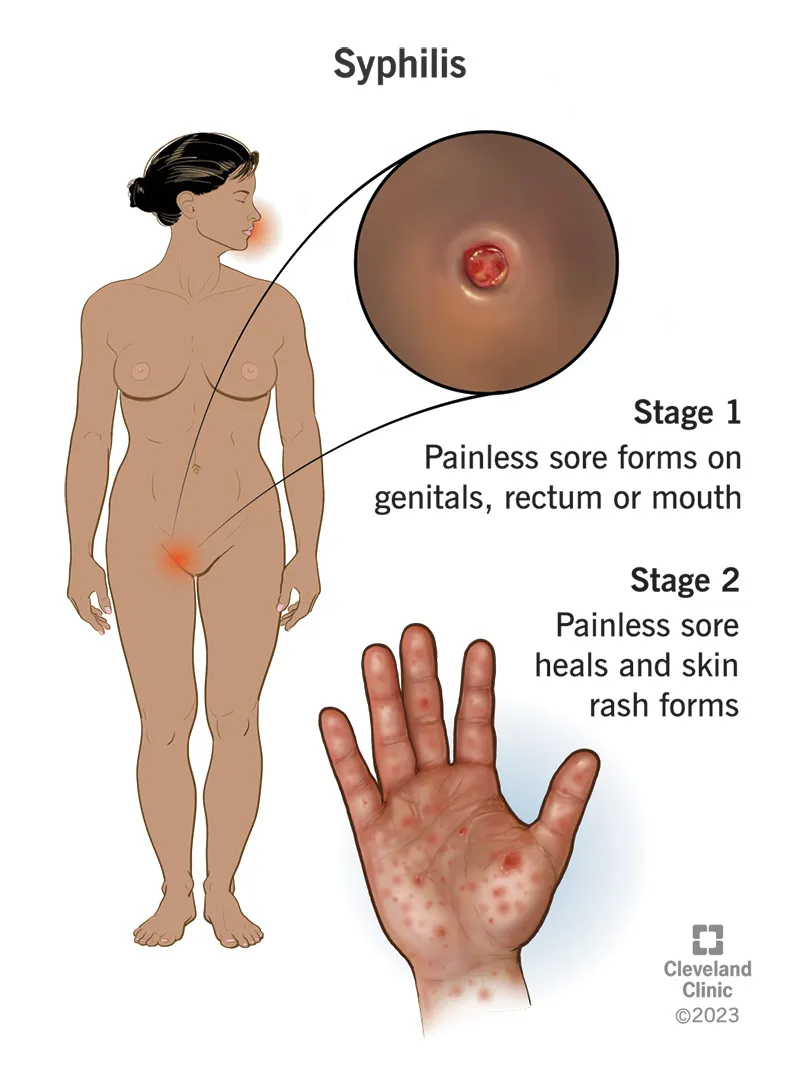
- The patient's history of a **painless genital ulcer** that resolved spontaneously, followed by positive VDRL and FTA-ABS tests, is classic for **syphilis**. Given the VDRL and FTA-ABS are both positive, this indicates a current or treated syphilis infection.
- **Penicillin G** is the drug of choice for all stages of syphilis; the specific formulation (e.g., benzathine penicillin G) and duration depend on the stage of infection.
*Doxycycline*
- **Doxycycline** can be used as an alternative treatment for syphilis in patients with a **penicillin allergy**.
- However, it is not the first-line treatment and there is no indication of a penicillin allergy in this patient.
*No treatment indicated*
- The positive VDRL and FTA-ABS tests definitively confirm an active or recently treated syphilis infection, requiring **treatment**.
- Leaving syphilis untreated can lead to severe complications, including **neurosyphilis** and **cardiovascular syphilis**.
*Acyclovir*
- **Acyclovir** is an antiviral medication used to treat **herpes simplex virus (HSV)** infections, which cause painful genital ulcers, not the painless chancre seen in syphilis.
- It has no efficacy against the bacterial pathogen *Treponema pallidum* that causes syphilis.
*Azithromycin and ceftriaxone*
- The combination of **azithromycin and ceftriaxone** is typically used to treat uncomplicated **gonorrhea** and **chlamydia** simultaneously.
- While these are common sexually transmitted infections, they do not cause the painless chancre or result in the serological findings (positive VDRL and FTA-ABS) characteristic of syphilis.
Treponema pallidum US Medical PG Question 3: A previously healthy 25-year-old man comes to the physician because of a 1-week history of fever and fluid release from painful lumps in his right groin. He had an atraumatic ulceration of his penis about 1 month ago that was not painful and resolved on its own within 1 week. He works at an animal shelter for abandoned pets. He is sexually active with multiple male partners and does not use condoms. His temperature is 38.5°C (101.3°F). Examination of the groin shows numerous tender nodules with purulent discharge. The remainder of the examination shows no abnormalities. Which of the following is the most likely causal pathogen?
- A. Haemophilus ducreyi
- B. Klebsiella granulomatis
- C. Treponema pallidum
- D. Bartonella henselae
- E. Chlamydia trachomatis (Correct Answer)
Treponema pallidum Explanation: ***Chlamydia trachomatis***
- The presentation of a **painless penile ulcer** followed by **painful inguinal lymphadenopathy** (buboes) with **purulent discharge** is classic for **lymphogranuloma venereum (LGV)**, caused by specific serovars (L1, L2, L3) of **Chlamydia trachomatis**.
- **Sexual activity with multiple male partners** and **lack of condom use** are risk factors for sexually transmitted infections, including LGV.
*Haemophilus ducreyi*
- This pathogen causes **chancroid**, which typically presents with **multiple, painful genital ulcers** and often painful inguinal lymphadenopathy, but the initial ulcer described here was painless.
- The initial lesion in chancroid is usually soft and ragged, distinguishing it from the firm, painless chancre of syphilis.
*Klebsiella granulomatis*
- This bacterium causes **granuloma inguinale (donovanosis)**, characterized by **painless, progressively enlarging ulcerative lesions** in the anogenital area that are highly vascular and bleed easily.
- It does not typically present with the dramatic inguinal lymphadenopathy and purulent discharge seen in LGV, although pseudobuboes can occur.
*Treponema pallidum*
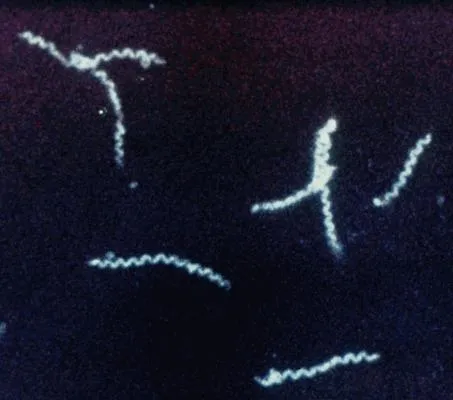
- This spirochete causes **syphilis**. The primary lesion of syphilis is a **painless chancre**, similar to the initial penile ulcer described.
- However, the subsequent **inguinal lymphadenopathy** in primary syphilis is typically **non-tender, bilateral**, and firm, unlike the painful, suppurative nodes observed here.
*Bartonella henselae*
- This bacterium is the causative agent of **cat scratch disease**, which typically presents with a **papule or pustule at the site of a cat scratch** followed by regional lymphadenopathy.
- The patient's job at an animal shelter might suggest exposure, but the presentation of a penile ulcer followed by suppurative inguinal lymphadenitis is not characteristic of cat scratch disease.
Treponema pallidum US Medical PG Question 4: A 45-year-old man presents with a 2-month history of painless testicular swelling. He reports being treated for syphilis 20 years ago. Examination reveals bilateral, non-tender testicular enlargement. Which of the following is the most likely diagnosis?
- A. Hydrocele
- B. Tuberculosis orchitis
- C. Epididymitis
- D. Testicular cancer
- E. Gummatous orchitis (Correct Answer)
Treponema pallidum Explanation: ***Gummatous orchitis***
- This diagnosis is strongly suggested by the history of treated **syphilis 20 years ago** and the presentation of **painless, bilateral, non-tender testicular enlargement**. Gummatous orchitis is a manifestation of **tertiary syphilis** [1].
- **Gumma** formation is a characteristic lesion of tertiary syphilis, leading to chronic, inflammatory, and often painless infiltrates in various organs, including the testes [1].
*Hydrocele*
- While hydroceles cause painless testicular swelling, they are typically **transilluminable** and feel like a fluid-filled sac separate from the testis. The clinical description of "non-tender testicular enlargement" implies involvement of the testicular tissue itself, not just fluid accumulation around it.
- Hydroceles are usually not associated with a remote history of syphilis in this manner and would not explain the **bilateral** and **solid-feeling** enlargement expected with gummatous orchitis.
*Tuberculosis orchitis*
- Tuberculosis orchitis usually presents with a more **indurated** or **nodular** feel and is often associated with symptoms of systemic tuberculosis (e.g., fever, weight loss, night sweats) or other genitourinary TB manifestations [2].
- While it can be painless, the specific history of syphilis points away from TB as the most likely cause without other supporting evidence.
*Epididymitis*
- Epididymitis is typically characterized by **pain and tenderness** of the epididymis, often accompanied by fever and dysuria, especially in acute cases. Even chronic epididymitis usually involves some degree of tenderness.
- The presented case describes a **painless** condition primarily affecting the testis, not the epididymis, making epididymitis less likely.
*Testicular cancer*
- Testicular cancer typically presents as a **unilateral, painless mass or enlargement** of the testis. While it can be painless, the **bilateral involvement** seen in this patient makes testicular cancer less likely as a primary diagnosis.
- Although it's a differential for painless testicular swelling, the strong history of syphilis is a powerful indicator for an infectious cause like gummatous orchitis.
Treponema pallidum US Medical PG Question 5: A 24-year-old man presents with a painless genital ulcer for the past 2 weeks. He reports that he recently has been having unprotected sex with multiple partners. Past medical history is unremarkable. On physical examination, a single ulcer is present on the dorsal shaft of the penis which is circumscribed, indurated, and partially healed. There is moderate inguinal lymphadenopathy but no buboes. Which of the following tests would confirm the most likely diagnosis in this patient?
- A. Perform a darkfield microscopic examination of a swab from the chancre (Correct Answer)
- B. Swab the chancre and perform a saline wet mount
- C. Fluorescent treponemal antibody absorption (FTA-ABS) test
- D. Frei test
- E. Venereal Disease Research Laboratory (VDRL) test
Treponema pallidum Explanation: ***Perform a darkfield microscopic examination of a swab from the chancre***
- This patient's presentation with a **painless, indurated genital ulcer** (chancre) and regional lymphadenopathy is highly suggestive of **primary syphilis**.
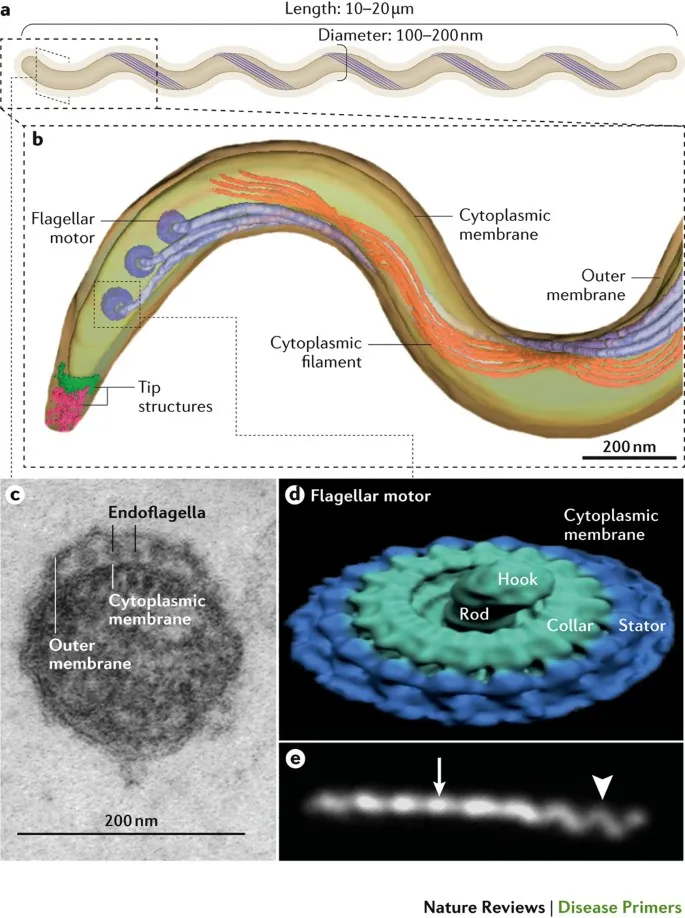
- **Darkfield microscopy** directly visualizes the spirochetes (**_Treponema pallidum_**) from the chancre, providing a definitive and rapid diagnosis.
*Swab the chancre and perform a saline wet mount*
- A **saline wet mount** is used to identify mobile organisms like **_Trichomonas vaginalis_** or clue cells suggestive of **bacterial vaginosis**, neither of which are associated with this type of ulcer.
- This test would not reveal the spirochetes responsible for syphilis and is not appropriate for diagnosing a genital ulcer.
*Fluorescent treponemal antibody absorption (FTA-ABS) test*
- The **FTA-ABS test** is a **treponemal-specific serological test** used to confirm a syphilis diagnosis, particularly in later stages or when non-treponemal tests are reactive.
- While sensitive for syphilis, it's typically reactive later in the disease course and cannot directly visualize the bacteria from the ulcer, making darkfield microscopy a more immediate and direct diagnostic tool for primary syphilis.
*Frei test*
- The **Frei test** is an obsolete intradermal skin test used to diagnose **lymphogranuloma venereum (LGV)**, which typically presents with a transient, unnoticed lesion followed by severe lymphadenopathy and buboes.
- It is not used for the diagnosis of syphilis and would not be helpful for this patient's presentation.
*Viral and rickettsial disease research laboratory (VDRL) test*
- The **VDRL test** is a **non-treponemal serological test** for syphilis that detects antibodies against cardiolipin, a lipid released from damaged host cells.
- While used for screening and monitoring treatment response, it can be **negative in early primary syphilis** (before seroconversion) and may not be positive at the time of presentation with a fresh chancre.
Treponema pallidum US Medical PG Question 6: A 25-year-old man presents with painless penile ulcer for 2 weeks. Physical examination reveals a firm, non-tender, clean-based ulcer with rolled edges. Dark-field microscopy of the lesion shows spirochetes. VDRL test is positive at 1:32 dilution. Which of the following is the most appropriate treatment?
- A. Azithromycin 1g orally single dose
- B. Three weekly doses of benzathine penicillin G 2.4 million units IM
- C. Single dose of benzathine penicillin G 2.4 million units IM (Correct Answer)
- D. Doxycycline 100 mg orally twice daily for 14 days
- E. Ceftriaxone 250 mg IM single dose
Treponema pallidum Explanation: ***Single dose of benzathine penicillin G 2.4 million units IM***
- This is the recommended treatment for **primary syphilis**, characterized by a **painless chancre** and **positive dark-field microscopy** and VDRL [1].
- The single dose is effective because primary syphilis is an early stage of the infection [1].
*Azithromycin 1g orally single dose*
- This regimen is primarily used for the treatment of **Chlamydia trachomatis** infections.
- It is not effective against **Treponema pallidum**, the causative agent of syphilis.
*Three weekly doses of benzathine penicillin G 2.4 million units IM*
- This multi-dose regimen is indicated for **late latent syphilis** or **syphilis of unknown duration**, not primary syphilis.
- While penicillin is the correct drug, the duration of therapy is too long for an early-stage infection.
*Doxycycline 100 mg orally twice daily for 14 days*
- Doxycycline is an alternative treatment for **early syphilis** (primary, secondary, or early latent) in patients who are allergic to penicillin.
- Given that penicillin is not contraindicated here, it is not the primary choice, and treatment with penicillin is more effective.
*Ceftriaxone 250 mg IM single dose*
- Ceftriaxone is a treatment for **gonorrhea**, not syphilis.
- While it has some activity against *Treponema pallidum*, it is not the recommended first-line treatment for syphilis.
Treponema pallidum US Medical PG Question 7: An investigator studying patients with symptoms of arthritis detects a nonenveloped virus with a single-stranded DNA genome in the serum of a pregnant patient. Fetal infection with this pathogen is most likely to cause which of the following manifestations?
- A. Hydrops fetalis (Correct Answer)
- B. Notched teeth
- C. Microcephaly
- D. Chorioretinitis
- E. Vesicular rash
Treponema pallidum Explanation: ***Hydrops fetalis***
- The description of a nonenveloped virus with a **single-stranded DNA genome** is characteristic of **Parvovirus B19**. This virus commonly causes hydrops fetalis due to **fetal anemia** and subsequent heart failure.
- Parvovirus B19 infection in pregnant women can lead to severe complications for the fetus, primarily due to tropism for **erythroid progenitor cells**, resulting in anemia.
*Notched teeth*
- **Hutchinson's teeth**, characterized by notches, are a classic manifestation of **congenital syphilis**, caused by the bacterium *Treponema pallidum*, not a virus.
- Syphilis is a spirochete and not a single-stranded DNA virus.
*Microcephaly*
- **Microcephaly** is a severe neurological abnormality often associated with congenital infections like **Zika virus** or **cytomegalovirus (CMV)**, which are RNA and double-stranded DNA viruses, respectively.
- While viral infections can cause microcephaly, Parvovirus B19 is primarily known for causing fetal anemia and hydrops, not typically microcephaly.
*Chorioretinitis*
- **Chorioretinitis** is a common ocular manifestation of congenital infections such as **toxoplasmosis**, **CMV**, and **rubella**, but it is not a hallmark of Parvovirus B19 infection.
- These pathogens have different genomic structures and disease presentations.
*Vesicular rash*
- A **vesicular rash** is characteristic of infections caused by **herpesviruses**, such as **varicella-zoster virus (VZV)** or herpes simplex virus.
- These are **double-stranded DNA viruses**, not single-stranded DNA viruses like Parvovirus B19.
Treponema pallidum US Medical PG Question 8: A 28-year-old woman comes to the emergency department for a rash that began 3 days ago. She has low-grade fever and muscle aches. She has no history of serious illness and takes no medications. She has had 5 male sexual partners over the past year and uses condoms inconsistently. Her temperature is 38.1°C (100.6° F), pulse is 85/min, and blood pressure is 126/89 mm Hg. Examination shows a diffuse maculopapular rash that includes the palms and soles. The remainder of the examination shows no abnormalities. A venereal disease research laboratory (VDRL) test is positive. Which of the following is the next appropriate step in management?
- A. Intravenous penicillin G
- B. Dark field microscopy
- C. Treponemal culture
- D. Oral doxycycline
- E. Fluorescent treponemal antibody absorption test (Correct Answer)
Treponema pallidum Explanation: ***Fluorescent treponemal antibody absorption test***
- A positive **VDRL** (a non-treponemal test) should be confirmed with a **treponemal-specific test** like the **fluorescent treponemal antibody absorption (FTA-ABS)** test or **Treponema pallidum particle agglutination (TPPA)** assay to definitively diagnose syphilis.
- This confirmatory step helps differentiate true syphilis from false-positive VDRL results, which can occur in autoimmune diseases (SLE, antiphospholipid syndrome), other infections (malaria, mononucleosis), pregnancy, or recent vaccination.
- While this patient's presentation is highly suggestive of **secondary syphilis** (diffuse maculopapular rash involving palms and soles, fever, myalgias, positive VDRL), confirmatory testing is the standard next step before initiating treatment.
- Note: In some clinical settings with classic secondary syphilis, immediate treatment may be initiated, but confirmatory testing remains the most appropriate next diagnostic step.
*Intravenous penicillin G*
- IV aqueous penicillin G is the treatment for **neurosyphilis**, not uncomplicated secondary syphilis.
- **Secondary syphilis** is treated with **intramuscular benzathine penicillin G 2.4 million units** as a single dose.
- Treatment should follow confirmed diagnosis with treponemal-specific testing.
*Dark field microscopy*
- This technique visualizes spirochetes directly from **primary lesions** (chancres) or moist secondary lesions (condyloma lata, mucous patches).
- It is not practical for this patient who has a diffuse maculopapular rash without obvious mucosal or genital lesions.
- Dark-field microscopy requires specialized equipment and expertise not readily available in most emergency departments.
*Treponemal culture*
- **Treponema pallidum** cannot be cultured on artificial media because it is an **obligate pathogen** that requires living host cells.
- Culture is not a diagnostic option for syphilis.
*Oral doxycycline*
- **Doxycycline 100 mg twice daily for 14 days** is an alternative treatment for early syphilis in **penicillin-allergic patients**.
- Treatment should only be initiated after diagnosis is confirmed with treponemal-specific testing.
- This is not the next appropriate step; confirmatory testing comes first.
Treponema pallidum US Medical PG Question 9: A 3000-g (6.6-lb) female newborn is delivered at term to a 23-year-old primigravid woman. The mother has had no prenatal care. Immunization records are not available. Cardiac examination shows a continuous heart murmur. There are several bluish macules on the skin that do not blanch with pressure. Slit lamp examination shows cloudy lenses in both eyes. The newborn does not pass his auditory screening tests. Which of the following is the most likely diagnosis?
- A. Congenital parvovirus infection
- B. Congenital cytomegalovirus infection
- C. Congenital rubella infection (Correct Answer)
- D. Congenital syphilis
- E. Congenital toxoplasmosis
Treponema pallidum Explanation: ***Congenital rubella infection***
- The classic triad of congenital rubella includes **sensorineural hearing loss**, **ocular abnormalities** (e.g., cataracts, glaucoma), and **cardiac defects** (e.g., patent ductus arteriosus, pulmonary artery stenosis), all of which are present in this case.
- The **blueberry muffin rash** (bluish macules) is also a characteristic, although non-specific, finding due to **extramedullary hematopoiesis**.
*Congenital parvovirus infection*
- Primarily causes **hydrops fetalis**, severe **anemia**, and fetal demise, often without the specific cardiac, ocular, and auditory defects described.
- While it can cause skin lesions, the constellation of findings strongly points away from parvovirus.
*Congenital cytomegalovirus infection*
- Can cause **sensorineural hearing loss** and central nervous system abnormalities (e.g., **periventricular calcifications**, microcephaly), but **cardiac defects** and **cataracts** are less common than with rubella.
- The typical skin lesions are often petechiae or purpura, not the distinct bluish macules seen here.
*Congenital syphilis*
- Presents with a wide range of manifestations, including **hepatosplenomegaly**, **rash** (often maculopapular or desquamating), **saddle nose deformity**, and bone abnormalities.
- While it can cause some ocular (e.g., interstitial keratitis) and auditory issues, the specific combination of **cataracts**, **patent ductus arteriosus**, and **sensorineural deafness** is not its hallmark.
*Congenital toxoplasmosis*
- Characterized by the classic triad of **chorioretinitis**, **hydrocephalus**, and **intracranial calcifications**.
- While it can cause hearing loss and some skin manifestations, the cardiac defect and cataracts described are not typical features.
Treponema pallidum US Medical PG Question 10: A 28-year-old man presents with painless anal ulcer. Dark-field microscopy shows spirochetes. He is allergic to penicillin with history of anaphylaxis. Which of the following is the most appropriate treatment?
- A. Erythromycin 500 mg four times daily for 14 days
- B. Penicillin desensitization followed by benzathine penicillin
- C. Doxycycline 100 mg orally twice daily for 14 days (Correct Answer)
- D. Azithromycin 2 g orally once
- E. Ceftriaxone 250 mg IM
Treponema pallidum Explanation: **Doxycycline 100 mg orally twice daily for 14 days**
- **Doxycycline** is the recommended alternative for treating **primary syphilis** in patients with a **penicillin allergy**, especially with a history of anaphylaxis.
- The 14-day duration for doxycycline is appropriate for treating early syphilis, including primary syphilis.
*Erythromycin 500 mg four times daily for 14 days*
- While erythromycin is an alternative, its efficacy for syphilis is **lower than doxycycline**, and it requires a longer duration of treatment.
- It is generally considered a less preferred option than doxycycline for penicillin-allergic patients due to adherence issues and potential for gastrointestinal side effects.
*Penicillin desensitization followed by benzathine penicillin*
- **Penicillin desensitization** is typically reserved for situations where penicillin is the **only truly effective treatment** and alternatives are not suitable, such as in neurosyphilis or syphilis in pregnancy.
- For primary syphilis in a non-pregnant patient with a clear anaphylactic allergy, an effective alternative like doxycycline is preferred over the risks associated with desensitization.
*Azithromycin 2 g orally once*
- **Azithromycin** resistance in *Treponema pallidum* is increasingly prevalent, making it an unreliable treatment for syphilis.
- A single dose is insufficient for effective treatment and carries a higher risk of treatment failure.
*Ceftriaxone 250 mg IM*
- **Ceftriaxone** is an alternative in some cases of syphilis, but the recommended dose for primary syphilis is typically higher and given for a longer duration (e.g., 1-2 g IM or IV daily for 10-14 days).
- A single 250 mg IM dose is insufficient for the treatment of syphilis and is more commonly used for gonorrhea.
More Treponema pallidum US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.